Abstract
Background
To describe the clinical presentation, burden and antimicrobial resistance of Methicillin-Resistant Staphylococcus aureus (MRSA) eye infections and to recommend a streamlined protocol for the management of ocular MRSA colonisation detected by pre-operative screening.
Methods
A retrospective review of all ocular samples which resulted in the isolation of MRSA between 1st of January 2013 and 31st of December 2019 at the Royal Victoria Eye and Ear Hospital.
Results
A total of 185 samples taken from the ocular surface were MRSA positive. The majority were MRSA colonisation of the ocular surface obtained as part of an MRSA screen (139/6955 patients screened; 2%). Forty-six represented MRSA infections (46/7904 eye samples; 0.58%), most occurring in older patients the majority of whom had known local or systemic risk factors for colonisation. The most common presentation was conjunctivitis (n = 24), followed by pre-septal cellulitis (n = 9). MRSA infections with the poorest clinical outcomes and the longest inpatient stay, were keratitis (n = 6) and post-operative endophthalmitis (n = 2). Our study demonstrated over 60% resistance to azithromycin, fusidic acid and ciprofloxacin, although resistance to chloramphenicol was uncommon.
Conclusion
This study demonstrates that MRSA infections of the eye most commonly manifest as a mild infection, typically conjunctivitis, and are generally non-sight threatening. The majority of presentations occur in the context of known MRSA risk factors and in an older populous. Resistance to chloramphenicol is rare, thus it remains an excellent first line treatment. Its use to eradicate MRSA from the ocular surface is proposed to streamline the delivery of surgical eye care.
Similar content being viewed by others
Introduction
In an era of increasing drug resistant bacteria, Methicillin Resistant Staphylococcus aureus (MRSA) is endemic in many healthcare facilities. This has led to growing concern amongst healthcare workers, patients and governments alike. From an ophthalmology stand point, Staphylococcus aureus (SA) is a pertinent cause of common presentations to eye departments, including that of conjunctivitis and bacterial keratitis [1] and thus monitoring and reducing the incidence of MRSA is prudent to clinical practice.
In Ireland there is a national policy for the prevention and management of MRSA [2]. The rates of resistance differ across health service networks, although this could be explained by the capacity of different hospitals to implement such policies [2, 3]. On the whole, MRSA infections in the Royal Victoria Eye and Ear Hospital (RVEEH) ophthalmology department are uncommon. This may be for a number of reasons; most patients do not have prolonged hospital stays and are discharged on the day of surgery, there are robust protocols on the prevention, diagnosis and management of MRSA colonisation and infection, and the innate immunity of the ocular surface strongly inhibits bacterial population of the eye. The low incidence of MRSA-related eye infection at RVEEH is in keeping with other ophthalmic centres, with one study conducted by the Manchester Eye Hospital over a 44-month period showing that only 3% of SA infections were due to MRSA [4]. Nevertheless, MRSA eye infections still occur and reports are emerging of rising rates of antimicrobial resistance leading to concern and a need for ongoing vigilance amongst all clinicians [5].
The aim of this study was to describe the clinical manifestations, departmental burden and antimicrobial resistance patterns of MRSA eye infections and ocular carriage of MRSA in RVEEH, a large tertiary eye hospital in Ireland.
Methods
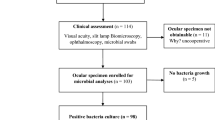
We conducted a retrospective review of all the MRSA positive ocular samples taken over a 7-year period, from 1st January 2013 to 31st December 2019, at RVEEH, the national tertiary referral hospital in Ireland for eye diseases. Cases were identified by reviewing the hospital microbiology laboratory information system. The site that the sample was taken from and the antibiotic sensitivity results were documented. The patient records were reviewed and information regarding patient demographics, clinical presentation, diagnosis, treatment and outcome was obtained where possible.
In keeping with the National guidelines for the prevention and control of MRSA, at-risk patients were screened for MRSA prior to admission for elective surgery [3]. In this instance, ophthalmic patients had the conjunctiva of both eyes swabbed for MRSA, as well as the nose, throat and groin. A positive ocular swab in a patient lacking clinical signs or symptoms of infection confirmed colonisation with MRSA. Patients who screen positive for MRSA undergo a decolonisation procedure preoperatively (Chlorhexidine washes, Mupiricin nasal ointment and ocular Chloramphenicol), as per the centre’s guidelines. Furthermore, in light of the early findings of this review, patient’s whose MRSA status is known preoperatively receive a dose of intracameral vancomycin surgical antibiotic prophylaxis at cataract surgery to prevent MRSA-associated endophthalmitis. Patients with clinical signs of ocular infection had diagnostic samples taken as clinically indicated, such as corneal scrapings and conjunctival swabs.
Swabs were transported to the laboratory in Amies transport medium. All diagnostic eye swabs are inoculated onto Columbia blood agar and chocolate agar. Agar plates are incubated at 35 °C in 5% CO2 for 40–48 h. Corneal scrapings were taken using a 21 gauge needle or scalpel. The anaesthetised cornea was scraped and the sample was smeared in a C shape directly onto blood, chocolate and sabouraud’s dextrose agar. MRSA screening swabs were inoculated onto Brilliance MRSA II chromagar and incubated aerobically at 35 °C for 18–20 h. Following incubation, agar plates are examined daily for potential pathogens. Potential MRSA are identified to species level and antibiotic susceptibility testing is performed using VITEK® 2 (BioMerieux), according to European Committee on Antimicrobial Susceptibility Testing (EUCAST) standards. MRSA are confirmed using penicillin binding protein 2a latex agglutination and cefoxitin disc diffusion testing. The laboratory is accredited to ISO 15189 standards.
Statistical analysis was carried out using Microsoft Excel.
Results
During the 7-year period a total of 185 ocular samples tested positive for MRSA. These samples were taken as part of (a) pre-operative MRSA screening (139; 75.14%) or (b) diagnostic evaluation of patients with symptoms of eye infection (46; 24.86%). They were derived from conjunctival swabs (n = 160), corneal scrapings (n = 5), corneal swabs (n = 5), ocular fluid (n = 2), a contact lens (n = 1), and in 12 cases of screens the ocular sampling site was not specified. Table 1 illustrates the annual frequency of ocular MRSA colonisation detected from pre-operative MRSA screening.
The number of patients screened for MRSA increased from 2013 to 2019 in line with the increase in cataract surgery activity at the hospital and especially following the opening of a dedicated cataract operating theatre in 2016.
During the study period eye swabs, corneal scrapings and ocular fluids were obtained for diagnosis of infection. Forty-six MRSA infections were identified. See Table 2 for the occurrence of ocular MRSA infections during the review period.
Twenty-nine (63%) of the ocular MRSA infections occurred in patients over the age of 65 years. 54.3% (n = 25) had one or more local risk factors for MRSA and 65.2% (n = 30) had one or more systemic risk factors for MRSA (see Supplementary Tables 1 and 2).
Clinical presentation of MRSA ocular infections
Conjunctivitis
There were 24 cases (52.2% of MRSA infections) of conjunctivitis identified over the 7-year period, making conjunctivitis the most common ocular manifestation of MRSA at this centre. Of those, two cases were a polymicrobial infection; one with Moraxella and one with Neisseria gonorrhoea. The mean age of presentation was 66 years (standard deviation SD 22.53).
On initial presentation, the most commonly prescribed topical treatment was Chloramphenicol (CPL, n = 13), seven as a monotherapy regime (one drop QDS) and six in conjunction with topical azithromycin (one drop BD). The remainder of the patients were commenced on an alternative topical first line single agent; azithromycin (n = 2), fusidic acid (one drop BD) (n = 1) and acyclovir (one drop five times a day) (n = 1). All four of these patients were changed to topical CPL once MRSA infection was confirmed. One patient who had started CPL, was unable to tolerate the treatment due to ocular pain side effects and was subsequently changed to fusidic acid. Two cases were presumed non-infectious on presentation, but were commenced on treatment once microbiology results returned, one with fusidic acid and another with vancomycin. All of the infections resolved fully with treatment.
Pre-septal cellulitis
The second most common MRSA infection was pre-septal cellulitis (n = 9, 19.6%). The mean age of presentation was 61 years (standard deviation 23.9). Two patients required hospital admission for IV antibiotics, with an 8- and 4-day length of hospital stay, respectively. The most commonly prescribed systemic antibiotic for pre-septal cellulitis was oral Co-amoxiclav (n = 6) and all resolved on this treatment. Although MRSA may well have caused the preseptal cellulitis and responded to Co-Amoxiclav, it may also be true that the positive MRSA culture was due to colonisation and possibly another pathogen caused the cellulitis. All patients except for one were prescribed concurrent CPL drops (one drop QDS). No treatment changes were recorded following the availability of microbiology results. Only one case occurred without any predisposing local or systemic MRSA risk factors.
Keratitis
Six (13%) cases of keratitis were recorded during the study period. Of note, one patient was positive for MRSA on a corneal swab. In the other five patients, MRSA was detected from the corneal scraping. All patients had multiple systemic and local co-morbidities. The mean age of presentation was 75 years (SD 18.81). All patients were treated empirically with topical vancomycin (one drop hourly) and ceftazidime (one drop hourly) and intravenous vancomycin was administered to one patient. Five patients required hospital admission for a period ranging from 4 days to 4 weeks. Resolution of the infection was achieved with topical therapy in 3 of the patients. Three of the patients underwent tarsarrhaphy. One patient required an enucleation for a persistent hypopyon and corneal abscess in a blind eye. In the remaining patients the final visual acuity was 6/6, 6/9, 6/20, and counting fingers (CF) in two patients.
Postoperative endophthalmitis
There were two cases of post-operative endophthalmitis caused by MRSA. The affected patients were elderly and presented within the first few days’ post uneventful phacoemulsification surgery. Both patients were treated with intravitreal and intensive topical vancomycin (one drop hourly) and ceftazidime (one drop hourly). One received oral moxifloxacin and the other intravenous ciprofloxacin and vancomycin. The duration of in-patient care was 9 and 13 days, respectively. The final visual acuity was CF in both patients.
Orbital cellulitis
There was one case of polymicrobial orbital cellulitis. MRSA and Pseudomonas aeruginosa grew on culture from a conjunctival swab. It occurred in an elderly patient following a split thickness skin graft following evisceration for squamous cell carcinoma. They had multiple systemic comorbidities including local and systemic risk factors for MRSA colonisation. Resolution of the infection occurred rapidly in response to systemic ciprofloxacin and topical chloramphenicol (one drop QDS).
Blepharitis
Three patients presenting with blepharitis symptoms and signs tested positive for MRSA on conjunctival swab. The mean age of presentation was 77 (SD 18.8) years. Two of the patients were treated with a course of fusidic acid drops (one drop BD) and the other with CPL ointment (QDS). All three infections resolved fully with treatment.
Canaliculitis
There was one case of canaliculitis. This occurred in a patient with no local or systemic risk factors for MRSA. It resolved with a course of oral Co-amoxiclav combined with topical CPL (one drop QDS) and dexamethasone ointment. Systemic MRSA antibiotics were not required.
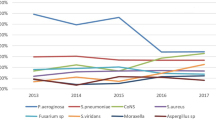
Antibiotic sensitivity analysis
MRSA positive samples from the eye were tested for antimicrobial resistance. Data was available from 2016 and 124 samples in total were analysed. The available results over the study period are shown in Table 3. MRSA detected from diagnostic samples and MRSA screens were included in the antibiotic analysis.
MRSA isolates from the eye were found to have a very low resistance to chloramphenicol and high resistance rates to fusidic acid and azithromycin, which are commonly used to treat conjunctivitis. Ciprofloxacin had the highest rates of resistance.
Discussion
In this 7-year review of MRSA eye infections and MRSA colonisation of the ocular surface detected at routine pre-operative screening at a specialist eye hospital, we have observed: (1) MRSA ocular infections do not represent a significant disease burden; and (2) pre-operative MRSA colonisation of the ocular surface is uncommonly detected in patients deemed to be at high risk of MRSA colonisation based on their medical and social history.
MRSA is a significant burden within many healthcare settings and is clinically significant. The Irish Health Protection Surveillance Centre reports that MRSA as a proportion of all S. aureus blood stream infection in Irish acute hospitals were 19.9% in 2013, 19.3% in 2014, 18.1% in 2015, 14.4% in 2016, 16.1% in 2017 and 12.4% in 2018 [6]. When contrasted to an ophthalmic setting, we demonstrate that MRSA positive eye swabs remained relatively low highlighting that MRSA in the eye is of less clinical significance than other healthcare settings. These low rates are in line with other single centre studies that have investigated the incidence of MRSA in ophthalmology departments [7].
We have shown that a majority of cases had a mild clinical presentation and had a favourable response to first line agents. Over a seven-year period there was a total of 46 cases of infection-related MRSA samples, with conjunctivitis being the most prevalent, as expected [4, 8, 9]. These eye infections predominantly presented with a modest clinical picture and were not sight threatening, in keeping with other published reports [8, 10]. MRSA keratitis and post-operative endophthalmitis were clear exceptions to this in our series owing to the poor visual outcomes in affected patients. One anomaly we have noted in our series was within the category of patients with reported MRSA involving pre-septal cellulitis infection. Six of these cases were successfully treated with a course of oral Co-amoxiclav. This would suggest that these swabs may have represented co-colonisation of MRSA within the context of another infection, possibly lowering furthermore the true toll of MRSA infection in eye departments.
MRSA infections frequently responded well to treatment, as first-line chloramphenicol cited in the hospital’s guidelines have maintained its efficacy, in line with other studies [11]. However, high level of resistance was identified with fusidic acid, azithromycin and fluoroquinolones. Hospital acquired MRSA is more common than community acquired MRSA and is usually associated with a broader spectrum of antibiotic resistance [12]. As older patients tend to be exposed to the healthcare environment more frequently, they are the cohort group most likely to contract MRSA. This was in keeping with our results with most affected patients being over the age of 65 years and having associated risk factors. The local and systemic risk factors identified in this study support current knowledge that MRSA tends to be present in high-risk groups. The ability to identify a patient being at high risk of MRSA can help guide antimicrobial management of the presentation. Moreover, it is likely that the majority of patients attending eye departments for elective surgical procedures are within a MRSA high-risk cohort because of the age-related nature of cataract surgery.
National guidelines require patients who test positive for MRSA to undergo decolonisation and subsequently have three negative screens prior to elective procedures. This places a burden on nursing staff and employees who process swab results, as well as extending wait times for procedures. These findings are of particular importance during the COVID-19 pandemic as wait times for many procedures have been extended. From an epidemiological standpoint, it is important that screening for patients with MRSA in healthcare environments continues. In doing so, decolonisation of patients attending for elective surgery can be completed prior to their admission, thus reducing transmission and risk of MRSA-related infection [13, 14]. It is also imperative to identify these patients in the context of ocular surgery, as being MRSA positive alters recommendations on antimicrobial prophylaxis practice given intraoperatively. Instead of receiving intracameral cefuroxime, colonised patients should instead receive vancomycin as standard practice [15]. The dismal visual outcomes associated with MRSA related endophthalmitis versus methicillin sensitive SA reported in the literature [16], and in the two cases described in our series, stresses the importance of robust and ongoing surveillance programs and appropriate antibiotic stewardship in the context of intraocular surgery. However, ensuring three negative screens prior to surgery places a burden on the delivery of care. It is our opinion that a course of pre-operative Chloramphenicol drops combined with MRSA decolonisation immediately pre-operatively and the use of intracameral vancomycin in patients with proven MRSA colonisation of the ocular surface would provide sufficient prophylaxis against the development of MRSA post-operative endophthalmitis. We are in the process of implementing this change in practice in our hospital and will continue to audit the clinical outcomes of our MRSA policy.
This study is limited by its retrospective nature. The time to heal, dosage of antibiotics and definition of clinical resolution were limited by the retrospective nature of the study.
Secondly, this is a single centre study with overall small numbers of MRSA which results in a limited generalisability. Finally, hospital and community acquired MRSA often present differently with different antimicrobial resistance patterns. PVL typing was not done on our patient cohort and we used exposure to a healthcare environment alone as a determinate of hospital-acquired MRSA.
Conclusion
There are no national guidelines for the management of MRSA specifically in eye care settings. Our series demonstrates that MRSA infections of the eye are generally mild and non-sight threatening. However, keratitis and endophthalmitis MRSA infections have significant morbidity. The majority of presentations of MRSA eye infections occur in the context of a known MRSA risk factor. Resistance to chloramphenicol is rare as borne out by both antibiotic sensitivity results and clinical response to treatment. Topical chloramphenicol is an excellent first line choice of therapy for suspected or proven MRSA eye infections and for eradicating MRSA from the eye pre-operatively. The findings of this study support the continued pre-operative screening of patients for MRSA and the use of prophylactic topical chloramphenicol and intracameral vancomycin but also supports eliminating the need for repeated MRSA negative conjunctival swabs prior to proceeding with surgery.
Summary
What was known before
-
MRSA is endemic to many healthcare facilities but it’s burden on eye departments is not known. There is a need to characterise ocular MRSA clinical manifestations so that antimicrobial guidelines are appropriate to ophthalmology.
What this study adds
-
This study demonstrates that MRSA infections of the eye most commonly manifest as a mild infection and are generally non-sight threatening. The majority of presentations occur in the context of known MRSA risk factors and in an older populous.
References
Sadaka A, Durand ML, Sisk R, Gilmore MS. Staphylococcus aureus and its bearing on ophthalmic disease. Ocul Immunol Inflamm. 2017;25:111–21.
Committee NCE Prevention and control methicillin-resistant staphylococcus aureus (MRSA) national clinical guideline No. 2. 2013.
Fitzpatrick F, Roche F, Cunney R, Humphreys H. Challenges of implementing national guidelines for the control and prevention of methicillin-resistant Staphylococcus aureus colonization or infection in acute care hospitals in the Republic of Ireland. Infect Control Hosp Epidemiol. 2009;30:277–81.
Shanmuganathan VA, Armstrong M, Buller A, Tullo AB. External ocular infections due to methicillin-resistant Staphylococcus aureus (MRSA). Eye. 2005;19:284–91.
Lalitha P, Manoharan G, Karpagam R, Prajna NV, Srinivasan M, Mascarenhas J, et al. Trends in antibiotic resistance in bacterial keratitis isolates from South India. Br J Ophthalmol. 2017;101:108–13.
HPSC Data on MRSA [Internet]. 2018 [cited 11/11/2019]. Available from: https://www.hpsc.ie/a-z/microbiologyantimicrobialresistance/europeanantimicrobialresistancesurveillancesystemearss/referenceandeducationalresourcematerial/saureusmrsa/latestsaureusmrsadata/.
Wong ES, Chow CW, Luk WK, Fung KS, Li KK. A 10-year review of ocular methicillin-resistant Staphylococcus aureus infections: epidemiology, clinical features, and treatment. Cornea 2017;36:92–7.
Amato M, Pershing S, Walvick M, Tanaka S. Trends in ophthalmic manifestations of methicillin-resistant Staphylococcus aureus (MRSA) in a northern California pediatric population. J AAPOS. 2013;17:243–7.
Walvick MD, Amato M. Ophthalmic methicillin-resistant Staphylococcus aureus infections: sensitivity and resistance profiles of 234 isolates 2011. p. 1024-6
Freidlin J, Acharya N, Lietman TM, Cevallos V, Whitcher JP, Margolis TP. Spectrum of eye disease caused by methicillin-resistant Staphylococcus aureus. Am J Ophthalmol. 2007;144:313–5.
Fukuda M, Ohashi H, Matsumoto C, Mishima S, Shimomura Y. Methicillin-resistant Staphylococcus aureus and methicillin-resistant coagulase-negative Staphylococcus ocular surface infection: efficacy of chloramphenicol eye drops. Cornea 2002;21:S86–S9.
Kang YC, Hsiao CH, Yeh LK, Ma DH, Chen PY, Lin HC, et al. Methicillin-resistant Staphylococcus aureus ocular infection in Taiwan: clinical features, genotying, and antibiotic susceptibility. Medicine 2015;94:e1620.
Sai N, Laurent C, Strale H, Denis O, Byl B. Efficacy of the decolonization of methicillin-resistant Staphylococcus aureus carriers in clinical practice. Antimicrob Resistance Infect Control. 2015;4:56.
Garvey MI, Winfield J, Wiley C, Reid M, Cooper M. Reduction in methicillin-resistant Staphylococcus aureus colonisation: impact of a screening and decolonisation programme. J Infect Prev 2016;17:294–7.
Porter LF, Khan RU, Hannan A, Kelly SP. MRSA and cataract surgery - reflections for practice. Clin Ophthalmol. 2010;4:1223–7.
Major JC Jr., Engelbert M, Flynn HW Jr., Miller D, Smiddy WE, Davis JL. Staphylococcus aureus endophthalmitis: antibiotic susceptibilities, methicillin resistance, and clinical outcomes. Am J Ophthalmol. 2010;149:278–83. e1
Funding
No funding was received for this study.
Author information
Authors and Affiliations
Contributions
C.C.M. conceived of this research topic. D.A.H. collected and analysed the data. E.G. and S.F. assisted in data analysis. S.J.K. and C.C.M. verified the analytical methods and supervised findings. D.A.H., E.G., S.J.K. and C.C.M. contributed to writing of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Harford, D.A., Greenan, E., Knowles, S.J. et al. The burden of methicillin-resistant Staphylococcus aureus in the delivery of eye care. Eye 36, 1368–1372 (2022). https://doi.org/10.1038/s41433-021-01643-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01643-6