Abstract
Objectives
To determine the patient-related factors that contribute to intraoperative corticocapsular adhesions (CCA) during phacoemulsification cataract extraction (PCE).
Methods
Prospective, single surgeon, multi-year study of consecutive patients undergoing PCE was performed. At the conclusion of each procedure, the surgeon recorded the CCA and perceived surgeon stress score. Patient variables included gender, age, diabetes mellitus, intake of oral alpha blockers, floppy iris, laterality, pseudo-exfoliation, and intraocular lens power.
Results
During the 10-year study, 1097 eyes underwent surgery and CCA was diagnosed intraoperatively in 41 eyes. On multi-variable analysis, the following patient characteristics were associated with intraoperative CCA: diabetes mellitus (p = 0.002), age >80 years (p = 0.002), presence of posterior capsular cataract (p = 0.046), severe nuclear sclerosis (p = 0.004), and absence of pseudo-exfoliation (p = 0.043).
Conclusion
Diabetes mellitus, advanced age and posterior subcapsular cataract are associated with CCA necessitating generous repetitive hydrodissection.
Similar content being viewed by others
Introduction
Hydrodissection is a major step during phacoemulsification. Cortical-cleaving hydrodissection was described in extracapsular cataract extraction by Faust [1] in 1984 and in phacoemulsification by several researchers [2,3,4,5] in early 1990. It involves separation of any corticocapsular adhesion (CCA) by injection of balanced salt solution with a blunt cannula by tenting the rim of the anterior capsule and this technique can include several variants such as single [6] or multilamellar [2] or multiquadrant [6]. Despite good cortical-cleaving hydrodissection, it may be very difficult or quite impossible to rotate the nucleus. In these cases, one should consider the presence of intraoperative CCA defined as the presence of adhesions between the capsule and cortex. The entity is detected intraoperatively, yet preoperative signs of possible CCA can be recognized by the presence of subcapsular furs [7,8,9]. Although the existence of intraoperative CCA is well recognized by phacoemulsification surgeons, we found few references dealing with the subject [7,8,9,10,11].
Methods
The Institutional Review Board of Rafic Hariri University Hospital, Beirut, Lebanon, approved this study. Prior to enrolment, each patient provided informed written consent in accordance with the Declaration of Helsinki. Data were anonymized to maintain patient confidentiality.
This is a prospective study of phacoemulsification cataract extraction (PCE) surgeries focusing on self-reported presence of intraoperative CCA and its correlation with patient-related ocular and systemic variables. Consecutive patients undergoing PCE under topical anaesthesia by one surgeon (AMM) between January 2010 and August 2019 were eligible for enrolment. Inclusion criteria were visually significant cataracts.
Baseline distance corrected Snellen visual acuity was measured by the surgeon. Each patient underwent slit lamp and dilated fundus examinations. Nuclear sclerosis was graded by slit lamp examination according to the Emery-Little classification system (very soft, soft, medium-hard, hard, and extremely hard). Topical xylocaine 2% or 3.5% gel was administered before surgery.
Surgical technique
A 2.7 mm bevelled limbal incision was made along with two side port incisions. A fairly rapid tiny injection of BSS is done with a 25-gauge flat hydrodissection cannula by tenting the rim of the anterior capsule on each side of the phacoemulsification incision twice followed by gentle decompression by pressing the nucleus downward to vent the fluid out. If the nucleus does not rotate using the flat cannula, CCA is diagnosed. Hydrodissection manoeuvre is then repeated twice in four quadrants and focally on the area of CCA that appears as ‘white cement’. When these manoeuvres fail, multilamellar hydrodissection into multiple lamellae of the lens, cleaving it into a small nucleus and multiple layers of cortex. If the nucleus does not rotate, the nucleus is divided into many segments that are emulsified. Forceful rotation of an adherent nucleus is not attempted for fear of zonular dialysis.
Hydrodissection was not attempted in eyes with hypermature cataracts. Phacoemulsification was performed with moderate infusion pressure (low infusion pressure), moderate aspiration pressure, and low ultrasound energy. At the completion of each surgery, the surgeon recorded the occurrence of CCA, the duration of surgery and the level of perceived stress on a scale from 0 to 2. The stress score was based on simplification of the Imperial Stress Assessment Tool [12] and consisted of summing up four items with each item worth one half a point (‘I felt the situation being out of control’; ‘I felt tense’; ‘I felt upset’; ‘I felt worried’).
Statistical analysis
Statistical analyses were performed using SPSS version 22 (IBM, Chicago, IL). The Chi-square test was used to test the difference between independent binary variables and the t-test was used to test the difference between the independent continuous variables. Linear regression analyses were performed with two-tailed Pearson and Spearman Chi-square tests. Multivariate analysis (when the dependent categorical variable was defined as ‘yes’ and ‘no’) was performed as a simple discriminant analysis using ANOVA, and confirmed by cross tabulation and Pearson Chi-square test. Spearman rank analysis was used to assess the correlation between continuous variables. Statistical significance was assumed when P values were less than 0.05.
Results
Seven hundred fifteen patients (mean age: 74 years) were enrolled in this study and 387 of them underwent bilateral cataract removal. Surgeries were performed on 1097 eyes (599 right eyes and 498 left eyes) and were nearly equally distributed among men (509) and women (588). Systemic and ocular co-morbidities included: diabetes mellitus (257 eyes in subjects with mean diabetes duration of 15.3 years; range 1–51 years), morbid obesity (body mass index ≥45 kg/m2) (36 eyes), pseudo-exfoliation (79 eyes), floppy iris syndrome (92 eyes), and use of oral alpha blockers for benign prostate hypertrophy (108 eyes). Grading of the nuclear sclerosis was as follows: 0 (soft) in 112 eyes, 1 (soft) in 53 eyes, 2 (semi-soft) in 163 eyes, 3 (medium-hard) in 425 eyes, 4 (hard) in 243 eyes, and 5 (rock-hard) in 101 eyes. Posterior subcapsular cataracts were present in 326 eyes.
LogMAR spectacle-corrected visual acuity (mean ± SD) improved from the preoperative visit (1.03 ± 0.63; Snellen equivalent of 20/209) to the last follow-up (0.20 ± 0.37; Snellen equivalent of 20/32; P < 0.001), which took place at a mean of 22.9 ± 31.0 months. The mean ± SD power of the implanted intraocular lens was 19.8 ± 1.6 D (range −3 to +31 D). The Rayner C-flex 570C monofocal intraocular lens (The Ridley Innovation Centre, Worthing, West Sussex, UK) was implanted in 694 eyes and the Alcon SA60AT intraocular lens (Alcon, Fort Worth, Texas, USA) was implanted in 389 eyes. CCA was diagnosed in 41 eyes (Fig. 1). In patients with bilateral surgery, CCA was unilateral in 15 patients and bilateral in 5 patients.
Univariate analysis using Chi-square revealed association with diabetes mellitus (p < 0.001), perceived surgeon stress (p < 0.001), duration of surgery (p < 0.001), age 80 and above vs. less than 80 (p = 0.001), posterior subcapsular cataract (p = 0.008), nuclear cataract grade (p = 0.037), right vs. left eye (p = 0.18), male vs. female (0.077), oral intake of alpha agonists (p = 0.38), pseudo-exfoliation (p = 0.42), lens power (15D to 25D vs. less than 15 D and more than 25D) (p = 0.45), floppy iris (p = 0.54), and morbid obesity (p = 0.61).
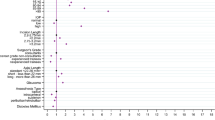
Regression analysis yielded a value F = 4.35 (p < 0.001) with significant associations being: advanced age (p = 0.002), presence of diabetes mellitus (p = 0.002), severe nuclear cataract (p = 0.004), longer duration of surgery (p = 0.007), higher surgeon stress score (p = 0.0027), presence of posterior subcapsular cataract (p = 0.046), and absence of pseudo-exfoliation (p = 0.043) (Table 1).
Discussion
We found the following positive associations between CCA and the following: diabetes mellitus, advanced age, advanced nuclear cataract, and posterior subcapsular cataract while a negative association existed with pseudo-exfoliation. These findings partly confirm previous associations found by Vasavada et al. [7,8,9]. CCA was detected in 20% in this Indian series (5 times more than in the Lebanese series), and this high rate of CCA was attributed to advanced age and severity of cataract. Over a period of 8 months, Vasavada et al. [9] operated on 189 patients with CCA (mean age 64.7) and 391 patients without CCA (mean age of 64.7). Multivariate logistic regression yielded the following: (1) females had 83% higher risk (P = 0.027); (2) CCA increased with advanced age from 22% (n = 59) in the 45-49 years group to 70% (n = 110) in the 70-79 years group; (3) anterior cortical cataract increased the odds of CCA by 9.5 times, and posterior cortical cataract by 3.3 times (P = 0.001); (4) increase in axial length by 1 mm reduced the odds of CCA by 12% (P = 0.029); (5) diabetes mellitus showed a nonsignificant weak positive association with CCA.
CCA acts as a snag to nucleus rotation with the tight adhesion of cortex to the capsule resulting from the presence of abnormal collagen bonds from fibrous metaplasia, and forceful nuclear rotation or forceful aspiration may lead to zonular dehiscence [10]. Intraoperative confirmation of CCA can be anticipated by visualization of a furry surface of cortex or better by noticing CCA on the slit lamp in the preoperative period. The presence of some form of CCA may be more common than reported here, but the current paper measured only the ease of rotation of the nucleus following two repeated sideway hydrodissection attempts. Therefore, the incidence will vary in different studies depending upon how the CCA is diagnosed, the technique of hydrodissection used (speed, volume and number of repeat attempts). CCA literature is meagre with a few papers mainly from India and it is possible that it is uncommon in the industrialized countries as PCE to remove age-related cataracts is done at a relatively early stage [7,8,9]. CCA results from fibrosis of the subcapsular region. Previous investigations [13, 14] showed that trans-differentiation of lens epithelial cells in subcapsular cataract allows the excessive production of extracellular matrix proteins (collagen I, III and fibronectin), a general characteristic of fibrosis. Capsular plaque formation seems to an extreme form of fibrosis when lens epithelial cells undergo proliferation and fibrous metaplasia (epithelial to mesenchymal transition), while CCA is a milder form of this form of fibrous metaplasia of lens epithelial cells[15, 16].
According to Vasavada et al. [7], the nucleus rotation failure rate after thorough hydrodissection was 20% of 180 cataract cases, while it was detected in 39.7% of 58 diabetic cataract cases [10]. Li et al. [17] did a systematic meta-analysis of eight studies totalling 20,837 patients and found twice the risk of cataract in diabetic vs. non-diabetic subjects: posterior cortical cataract (odds ratio 1.68; P < 0.001) and posterior subcapsular cataract (odds ratio 1.55; P < 0.001.
Hydrodissection was more easily performed on the pseudo-exfoliation patients than on the controls in the current study. Sorkou et al. [11] compared two groups matched for age, gender, the biomicroscopic type of cataract, and the presence of diabetes mellitus in 115 consecutive patients with age-related cataract and including 42 with pseudo-exfoliation. Easy hydrodissection was easy in 39 of the 42 exfoliation patients (92.8%) vs. 47 out of 73 (64.3%) in the control group (p = 0.001). This finding could be related to the extensive ultrastructural subepithelial alterations of the anterior lens capsule in pseudo-exfoliation [11].
CCA was associated with diabetes mellitus and advanced age and was accompanied by longer operating room time and higher perceived stress by the cataract surgeon. Part of the extra time in CCA eyes was due to repeated hydrodissection attempts, and more so to PCE without hydrodissection [18] (such as the division of the nonrotating nucleus into small pies and emulsification of the central piece with special attention at aspirating the equatorial part of the nucleus).
Summary
What was known before
-
Corticocapsular adhesion is common in India and quite uncommon in the industrialized world.
What this study adds
-
Corticocapsular adhesion is associated with diabetes mellitus and advanced age Corticocapsular adhesion is associated with longer duration of surgery and increased perceived stress by the operating surgeon Corticocapsular adhesion is negatively associated with the presence of pseudo-exfoliation.
References
Faust KJ. Hydrodissection of soft nuclei. J Am Intraocul Implant Soc. 1984;10:75–7.
Koch DD, Liu JF. Multilamellar hydrodissection in phacoemulsification and planned extracapsular surgery. J Cataract Refract Surg. 1990;16:559–62.
Fine IH. Cortical cleaving hydrodissection. J Cataract Refract Surg. 1992;18:508–12.
Blumenthal M, Ashkenazi I, Assia E, Cahane M. Small-incision manual extracapsular cataract extraction using selective hydrodissection. Ophthalmic Surg. 1992;23:699–701.
Gimbel HV. Hydrodissection and hydrodelineation. Int Ophthalmol Clin. 1994;34:73–90.
Joshi RS. Multiquadrant versus single quadrant cortical cleaving hydrodissection during phacoemulsification of age related cataract. Saudi J Ophthalmol. 2019;33:347–52.
Vasavada AR, Goyal D, Shastri L, Singh R. Corticocapsular adhesions and their effect during cataract surgery. J Cataract Refract Surg. 2003;29:309–14.
Vasavada AR, Singh R, Apple DJ, Trivedi RH, Pandey SK, Werner L. Effect of hydrodissection on intraoperative performance: randomized study. J Cataract Refract Surg. 2002;28:1623–8.
Vasavada VA, Vasavada VA. The probable associations for corticocapsular adhesions in patients undergoing cataract surgery: a clinic-based observational study. Indian J Ophthalmol. 2008;56:103–8.
Khokhar S, Pangtey MS. Surgical peculiarities in type II diabetic cataracts during phacoemulsification. Ophthalmic surgery, lasers and imaging. Retina. 2003;34:100–3.
Sorkou K, Tsinopoulos IT, Tsaousis KT, Karamitsos A, Meditskou S, Ziakas N, et al. Ease of hydrodissection during phacoemulsification: A comparison between patients with and those without exfoliation syndrome. Ophthalmic Res. 2020;63:497–500.
Arora S, Tierney T, Sevdalis N, Aggarwal R, Nestel D, Woloshynowych M, et al. The imperial stress assessment tool (ISAT): a feasible, reliable and valid approach to measuring stress in the operating room. World J Surg. 2010;34:1756–63.
Eldred JA, Dawes LJ, Wormstone IM. The lens as a model for fibrotic disease. Philos Trans R Soc Lond B Biol Sci. 2011;366:1301–19.
Lee EH, Joo CK. Role of tranforming growth factor-beta in transdifferentiation and fibrosis of lens epithelial cells. Invest Ophthalmol Vis Sci. 1999;40:2025–32.
Peng Q, Hennig A, Vasavada AR, Apple DJ. Posterior capsular plaque: a common feature of cataract surgery in the developing World. Am J Ophthalmol. 1998;125:621–6.
Vasavada AR, Chauhan H, Shah G. Incidence of posterior capsular plaque in cataract surgery. J Cataract Refract Surg. 1997;23:798–802.
Li L, Wan X, Zhao G. Meta-analysis of the risk of cataract in type 2 diabetes. BMC Ophthalmol. 2014;14:94.
Soda M, Yaguchi S. Phacoemulsification without hydrodissection: semi-crater and split technique. J Cataract Refract Surg. 2015;41:1132–6.
Acknowledgements
We thank Abhay Vasavada, MS, FRCS for reviewing the manuscript.
Author information
Authors and Affiliations
Contributions
AMM contributed to design of the study, data analysis, manuscript draft; IIKA contributed to design of the study and manuscript draft; KMEJ and HAM carried data collection and manuscript revision; ARC contributed to the statistical analysis and manuscript revision; All authors approved the final version
Corresponding author
Ethics declarations
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Mansour, A.M., Ahmed, I.I.K., Charbaji, A.R. et al. Associations in corticocapsular adhesions. Eye 36, 193–197 (2022). https://doi.org/10.1038/s41433-021-01482-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-021-01482-5