Abstract
Purpose
To evaluate clinical efficacy of combined sulphur hexafluoride (SF6) gas tamponade and laser photocoagulation for optic disc pit maculopathy (ODPM).
Methods
Eleven eyes of nine patients with optic disc pit maculopathy were treated with intravitreal injection of 0.6 ml 100% sulphur hexafluoride (SF6) combined with laser photocoagulation treatment. Patients were followed up for a mean of 28.54 months (range of 14–57 months) after treatment. The anatomical success was shown by optical coherence tomography (OCT) and the functional outcome was judged by best corrected visual acuity.
Results
Treatment with SF6 gas tamponade followed by laser photocoagulation in OPDM patients resulted in resolution of subretinal fluid (SRF) in 82% of eyes after single injection. Repeated injection was needed in two eyes to achieve resolution of SRF. Visual acuity improved significantly from a mean of 0.83 ± 0.14 logMAR preoperatively to a mean of 0.26 ± 0.11 logMAR postoperatively. Visual acuity stayed stable throughout the follow-up period.
Conclusions
SF6 gas tamponade combined with laser photocoagulation represents simple, effective, minimally invasive treatment option for ODPM without vitreomacular traction. Repeated injection was required in some patients.
Similar content being viewed by others
Introduction
Optic disc pit (ODP) remains a rare congenital abnormality that typically appears as a unilateral, oval, hypo-pigmented grey–white excavation of the optic disc at the temporal or inferotemporal segment. Although rarely, 15% of ODP were found to be bilateral [1]. Fluid tracking into the macula typically produces characteristic alterations with inner retinal cystic changes resembling macular retinoschisis followed by serous retinal detachment [2]. Some researchers proposed a probable passageway of fluid in ODPM that it first trickles into the outer layer of the retina and then affects other layers [3].
The exact pathogenic background behind the development of optic disc pit maculopathy (ODPM) stays controversial [4]. Because of the rarity of this disease, it is extremely arduous to properly conduct a randomised controlled clinical trial and thus, a number of surgical techniques are used [5]. Several studies suggested the presence of vitreous abnormalities [6] and recently, the most widely accepted treatment for such patients seems to be a surgical approach involving pars plana vitrectomy. Internal limiting membrane (ILM) peeling and endo-laser photocoagulation and gas endo-tamponade can be done with PPV [7]. Combined treatment with gas tamponade and laser without vitrectomy has been formerly reported with success rate of 75% [8].
The aim of this study was to determine long-term safety and efficacy of gas tamponade by means of sulphur hexafluoride (SF6) combined with laser photocoagulation in patients with ODPM.
Patients and method
This case series was conducted in Benha University and Asiut University Hospitals, Egypt. This work was approved by Benha University research ethics committee. All procedures were done in accordance with the Declaration of Helsinki and its updates. A written informed consent was got from every participant. Eleven eyes of nine patients with ODPM confirmed with optical coherence tomography (OCT) were included in the study. OCT and BCVA were obtained preoperatively and postoperatively in each patient.
Imaging
OCT images of the eyes were obtained using OCT 4000 Cirrus (Carl Zeiss Meditec, Inc, Dublin, CA) or (Topcon 3D OCT-2000 FA, Japan, version 8.30). The presence of a double-layer detachment, consisting of both a retinal schisis and a neurosensory detachment, was confirmed by OCT before surgery. The macular thickness profile was calculated. A comprehensive evaluation of the vitreoretinal interface regarding any vitreomacular or vitreo-papillary traction was done.
Gas injection
Intravitreal gas injection procedure was undertaken under topical anaesthesia. Paracentesis of the anterior chamber was followed by injection of 0.6 ml of 100% SF6 gas intravitreally. After this procedure the patients were instructed to adapt a facedown position for 2 weeks.
Laser
After subretinal fluid (SRF) absorption or fluid displacement away from the macula, 2–3 weeks following gas injection, laser photocoagulation was performed using a 532 nm wavelength laser. Two to three rows of 100 mm spot size burns were placed temporal and adjacent to the optic nerve to span the juxta papillary border of the retinal detachment. Exposures of 0.1 s were used, and the power adjusted to cause Grade I–II grey burn at the level of the retinal pigment epithelium. All the patients were followed up monthly postoperatively.
Outcome
The main outcome measures included BCVA and the status of retinal anatomic features (OCT). Patients were offered repeated treatment if maculopathy like serous detachment or schisis still existed.
Statistical analysis
Data management and statistical analysis were done using SPSS vs.25. Numerical data were summarised as means and standard deviations. All P values were two sided. P value < 0.05 was considered significant.
Results
The clinical characteristics of the nine patients are demonstrated in Table 1. All patients reported a history of decreased vision, metamorphopsia or scotoma for several months. The average duration of symptoms was 12.36 ± 4.12 months (range of 7–21). This study included six male and three female patients with a mean age of 22.0 ± 4.93 years (range 15–31). Two patients suffered bilateral disease, and the site of the pit was located temporally in nine eyes and inferior temporal in two eyes. The fluid was confined to the macula in seven eyes while it extended outside the arcades in four eyes.
Preoperative OCT findings are shown in the Table 2. No preoperative vitreomacular or vitreo-papillary traction was found in all subjects. PVD was detected in no case preoperatively and in one case postoperatively. The fluid distribution was SRF only in two eyes, SRF combined with outer layer fluid (OLF) in six eyes and SRF combined with multiple layer fluid (MLF) in three eyes. The mean preoperative average retinal thickness measured from the RPE to the ILM was 383 ± 34.82 μm. It improved at the last follow-up visit to a mean of 233.09 ± 20.48 μm (P value of <0.0001).
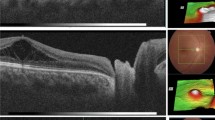
Combined retinal schisis and neurosensory macular detachment were displayed in Fig. 1 and the sole finding of macular neurosensory detachment was presented in Fig. 2. Complete retinal attachment was achieved in all patients with single intravitreal gas injection in nine eyes and with two injections in two eyes. Figure 3 shows serial images of a patient number 2 from presentation till complete resolution.
a Preoperative OCT scan shows multiple layer fluid (MLF) in the form of subretinal fluid (SRF), outer retinal layer fluid (OLF) and inner layer fluid (ILF). b OCT scan 2 weeks after the procedure shows subretinal fluid (SRF) and outer retinal layer fluid (OLF). c OCT scan a month later shows smaller amount of subretinal fluid (SRF) and outer retinal layer fluid (OLF). d OCT scan 6 months after the procedure shows complete resolution.
The mean preoperative logMAR BCVA was 0.83 ± 0.14 that improved to a mean postoperative logMAR BCVA of 0.26 ± 0.11 (P value of <0.0001). No significant intraoperative or postoperative complications were noted in all patients. There was no recurrence of macular detachment or intraretinal schisis in any patient after reaching complete reattachment during the follow-up period.
Discussion
Although ODPM represents a rare disease, visual deterioration is the result especially in the first 6 months of follow-up without treatment [9]. No definite ODPM treatment that is universally accepted, since none have been shown to be clearly better than the others. This is partially owed to the rarity of this clinical entity, and somewhat due to the challenging nature of the retinal detachment [10].
PPV has been the preferred method for surgical treatment of ODPM with the creation of PVD and gas tamponade. Laser photocoagulation of the peripapillary retina and ILM peeling can be added [11, 12]. The onset of ODPM commonly occurs in the 3rd and 4th decades of life which is the age of initial vitreous liquefaction [13, 14].
In our work we probed the usefulness of SF6 gas tamponade combined with laser photocoagulation for ODPM in eleven eyes of nine patients. We had younger patients with congenital ODPM. We had a mean age at presentation of ODPM 22.0 ± 4.93 years which was lower compared to Hirakata et al. (32.3 years) [15]. Ooto et al. had average age of 48.2 with an interquartile range of 35.5 to 63 years [16]. Avci et al. had cases with a mean age of 35.15 ± 16.38 years [17]. Our suggestion is that the relatively younger patient in our case series resulted in high success rate for gas and laser.
The fluid distribution in our cases was; subretinal fluid SRF only in two eyes, SRF and OLF in six eyes and SRF and MLF in three eyes. This typically goes in line with the proposed pathway of fluid in ODPM by Roy R and his associates. It first trickles into the outer retinal layer and then affects the other layers [3]. In our study no vitreomacular traction was observed by preoperative OCT examination. This indicates either absence of vitreomacular traction with a strong adhesive posterior hyaloid or a total PVD without traction. Various researches demonstrated the absence of vitreous abnormalities associated with ODP. ODPM in paediatric patients had strong vitreous adhesions compared to adults [18]. Moreover, number of OCT studies have revealed lack of evidence of vitreous traction on ODPs [19, 20]. Furthermore, ODPM can recur even after PPV with induction of posterior hyaloid detachment suggesting that traction may be unrequired for its formation [12].
Finally, PPV was ineffective in eyes with preoperative total PVD and it has been suggested that PPV allows reattachment of the macula by releasing preexisting vitreous traction. Therefore, the preoperative condition of the posterior hyaloid membrane seems to be an important factor in predicting the outcome of PPV. In eyes with preoperative PVD, the ODP-associated maculopathy may have derived from a source independent of vitreous traction, like cerebrospinal fluid or vascular leakage [21]. Various clinical studies evaluated the presence of some vitreous abnormalities by OCT. Changes ranged from vitreomacular traction [5] or broad-based vitreous adhesion [22], vitreo-papillary traction [23] or a membrane over the ODP [24, 25]. Vitreomacular traction is linked to ODP strands or strands alone [5]. Broad-based vitreous adhesion may lead to sub ILM fluid accumulation and more than one level of intraretinal fluid [22]. Doyle et al. demonstrated fenestrations in the membrane over the ODP in the four patients of their case series without evidence of PVD [26]. The success of treatment of ODPM with PPV and PVD induction also suggest reduction of vitreous traction that lead to resolution of ODPM [15, 19]. The injection of intravitreal gas as a treatment option for OPDM was based on the concept that pneumatic displacement can cause reattachment of the macula and improve VA [27]. This technique was used by several researchers and resulted in visual improvement.
In our study retinal attachment was achieved in all patients, with single injection in nine eyes, and the rest needed two injections. These results may be because we have only four from 11 eyes with fluid extend beyond the arcades and three from 11 eyes with SRF and MLF. The existence of SRF and MLF and the presence of macular fluid extending beyond the vascular arcades represented negative prognostic factors for visual and anatomical success. This was reported by Steel et al. [28].
Lei et al. also employed a combination of intravitreal gas injection and 532 nm laser photocoagulation temporal to the disc. They reported visual improvement and reduction in fluid in all subjects with complete resolution of intraretinal and subretinal fluids in 75% of eyes [8]. In their trial a single intravitreal perfluoropropane (C3F8) was injected. We decided to use SF6 in our study as it is of lesser incidence of complications [29]. We used the same laser as in Lei and associates work (532 nm laser). Brief exposures and low power were applied merely to produce grade I–II grey burn at the level of the pigment epithelium. We believe that modification of the parameters can decrease the effect of laser on inner retinal layers.
Akiyama et al. used the same gas (SF6) only without any laser treatment. However, they more than one injection in four out of the eight patients. They suggested the laser treatment reduced the number of injections needed for retinal reattachment [7]. It should be carefully noted that, after the complete reattachment by gas tamponade, none of these cases had any recurrences during the follow-up period. It has been suggested that pneumo-retinopexy with the facedown position enables the absorption of SRF and intraretinal fluid. Photocoagulation block the abnormal communication between the pit and the adjacent inner retinal layers by the adhesion of the retina and choroid at the optic disc border [8].
Conclusion
Gas tamponade with SF6 combined with laser photocoagulation was proved to represent an effective method for ODPM treatment. High success rate can be achieved in relatively young patients and also in those with no vitreomacular or vitreo-papillary traction.
Summary
What was known before
-
Pars plana vitrectomy is the treatment of choice for cases with ODPM
What this study adds
-
SF6 gas tamponade combined with laser photocoagulation represents simple, effective, minimally invasive treatment option for ODPM without vitreomacular traction.
References
Chatziralli Theodossiadis P, Theodossiadis GP. Optic disk pit maculopathy: current management strategies. Clin Ophthalmol. 2018;10:1417–22.
Todorich B, Sharma S, Vajzovic L. Successful repair of recurrent optic disk pit maculopathy with autologous platelet rich plasma: report of a surgical technique. Retinal Cases Brief Rep. 2017;11:15–7.
Roy R, Waanbah AD, Mathur G, Raman R, Sharma T. Optical coherence tomography characteristics in eyes with optic pit maculopathy. Retina. 2013;33:771–5.
Moisseiev E1, Moisseiev J, Loewenstein A. Optic disc pit maculopathy: when and how to treat? A review of the pathogenesis and treatment options. Int J Retin Vitreous. 2015;1:13.
Nawrocki J1, Bonińska K, Michalewska Z. Managing Optic Pit. The right Stuff! Retina. 2016;36:2430–2.
Theodossiadis PG, Grigoropoulos VG, Emfietzoglou J, Theodossiadis GP. Vitreous findings in optic disc pit maculopathy based on optical coherence tomography. Graefes Arch Clin Exp Ophthalmol. 2007;245:1311–8.
Akiyama H, Shimoda Y, Fukuchi M, Kashima T, Mayuzumi H, Shinohara Y. et al. Intravitreal gas injection without vitrectomy for macular detachment associated with an optic disk pit. Retina. 2014;34:222–7.
Lei L, Li T, Ding X, Ma W, Zhu X, Atik A, et al. Gas tamponade combined with laser photocoagulation therapy for congenital optic disc pit maculopathy. Eye. 2015;1:106–14.
Sobol WM, Blodi CF, Folk JC, Weingeist TA. Long-term visual outcome in patients with optic nerve pit and serous retinal detachment of the macula. Ophthalmology 1990;97:1539–42.
Georgalas I, Ladas I, Georgopoulos G, Petrou P. Optic disc pit: a review. Graefes Arch Clin Exp Ophthalmol. 2011;249:1113–22.
Abouammoh MA, Alsulaiman SM, Gupta VS, Mousa A, Hirakata A, Berrocal MH, et al. Pars plana vitrectomy with juxtapapillary laser photocoagulation versus vitrectomy without juxtapapillary laser photocoagulation for the treatment of optic disc pit maculopathy: the results of the KKESH International Collaborative Retina Study Group. Br J Ophthalmol. 2015;100:478–83.
Avci R, Kapran Z, Ozdek Ş, Teke MY, Oz O, Guven D, et al. Multicenter study of pars plana vitrectomy for optic disc pit maculopathy: MACPIT study. Eye. 2017;31:1266–73.
Brodsky MC. Congenital optic disc anomalies. Surv Ophthalmol 1994;39:89–112.
Brockhurst RJ. Optic pits and posterior retinal detachment. Trans Am Ophthalmol Soc 1975;73:264–91.
Hirakata A, Inoue M, Hiraoka T, McCuen BW. Vitrectomy without laser treatment or gas tamponade for macular detachment associated with an optic disc pit. Ophthalmology. 2012;119:810–8.
Ooto S, Mittra RA, Ridley ME, Spaide RF. Vitrectomy with inner retinal fenestration for optic disc pit maculopathy. Ophthalmology. 2014;121:1727–33.
Avci R, Yilmaz S, Inan UU, Kaderli B, Kurt M, Yalcinbayir O, et al. Long-term outcomes of pars plana vitrectomy without internal limiting peeling for optic disc pit maculopathy. Eye. 2013;27:1359–67.
Rii T, Hirakata A, Inoue M. Comparative findings in childhood-onset versus adult-onset optic disc pit maculopathy. Acta Ophthalmol. 2013;91:429–33.
Hirakata A, Okada AA, Hida T. Long-term results of vitrectomy without laser treatment for macular detachment with an optic disc pit. Ophthalmology. 2005;112:1430–5.
Karacorlu SA, Karacorlu M, Ozdemir H, Burumcek E, Esgin H. Optical coherence tomography in optic pit maculopathy. Int Ophthalmol 2007;27:293–7.
Haruta M, Kamada R, Umeno Y, Yamakawa R. Vitrectomy for optic disc pit-associated maculopathy with or without preoperative posterior vitreous detachment. Clin Ophthalmol 2012;6:1361–4.
Imamura Y, Zweifel SA, Fujiwara T, Freund KB, Spaide RF. High-resolution optical coherence tomography findings in optic pit maculopathy. Retina. 2010;30:1104–12.
Maertz J, Kolb JP, Klein T, Mohler KJ, Eibl M, Wieser W, et al. Combined in-depth, 3D, en face imaging of the optic disc, optic disc pits and optic disc pit maculopathy using swept-source megahertz OCT at 1050 nm. Graefes Arch Clin Exp Ophthalmol. 2018;256:289–98.
Michalewski J, Michalewska Z, Nawrocki J. Spectral domain optical coherence tomography morphology in optic disc pit associated maculopathy. Indian J Ophthalmol. 2014;62:777–81.
Christoforidis JB, Terrell W, Davidorf FH. Histopathology of optic nerve pit-associated maculopathy. Clin Ophthalmol. 2012;6:1169–74.
Doyle E, Trivedi D, Good P, Scott RA, Kirkby GR. High-resolution optical coherence tomography demonstration of membranes spanning optic disc pits and colobomas. Br J Ophthalmol. 2009;93:360–5.
Lincoff H1, Kreissig I. Optical coherence tomography of pneumatic displacement of optic disc pit maculopathy. Br J Ophthalmol. 1998;82:367–72.
Steel DH, Williamson TH, Laidlaw DA, Sharma P, Matthews C, Rees J, et al. Extent and location of intraretinal and subretinal fluid as prognostic factors for the outcome of patients with optic disk pit maculopathy. Retina. 2016;36:110–8.
Modi A, Giridhar A, Gopalakrishnan M. Sulfurhexafluoride (SF6) versus perfluoropropane (C3F8) gas as tamponade in macular hole surgery. Retina. 2017;37:283–90.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Elmohamady, M.N., Khalil, M.T.I., Bayoumy, A.S.M. et al. Sulphur hexafluoride (SF6) intravitreal injection combined with argon laser photocoagulation for treatment of optic disc pit maculopathy. Eye 35, 441–447 (2021). https://doi.org/10.1038/s41433-020-0867-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0867-3
This article is cited by
-
The outcomes of intravitreal C3F8 gas tamponade combined with laser photocoagulation treatment for optic disc pit maculopathy
International Ophthalmology (2022)