Abstract
In this paper, an overview of advanced robotic surgical systems in ophthalmology is provided. The systems are introduced as representative examples of the degree of human vs. robotic control during surgical procedures. The details are presented on each system and the latest advancements of each are described. Future potential applications for surgical robotics in ophthalmology are discussed in detail, with representative examples provided alongside recent progress.
摘要
本文总结了先进的眼科机器人手术系统。文中通过具有代表性的眼科机器人系统介绍了在眼科手术中人类与机器人控制的程度。本文展现了每个系统的细节, 且描述了其最新进展。文章也详细讨论了手术机器人在眼科领域潜在的应用前景, 并提供了代表性例子及最新进展。
Similar content being viewed by others
Introduction
The integration of robotic surgical systems into operating rooms has become common across numerous surgical fields due to their increased precision, higher manoeuvrability, and improved visualisation over manually performed surgical procedures. In the past two decades, the da Vinci Surgical System (Intuitive Surgical, Inc.) has become the most prevalent robotic surgical system with an installed base of over 4000 units worldwide [1]. This market share has been used to perform more than 1.5 million surgical procedures in the fields of gynaecology, urology, and general surgery [1]. The da Vinci Surgical System is a commercially available surgical robotic system with FDA approval, but their initial intellectual property patents soon expire and competing systems such as Telelap Alf-X and Revo-I are undergoing clinical testing and getting closer to entering the market [2]. Despite this rapid progress, the implementation of surgical robotic systems into eye surgery has trailed behind their adoption into other surgical areas.
The delayed transition of intraocular surgical robotic systems from laboratory research prototypes to routine clinical practice can be attributed to the unique advantages of intraocular surgery, which may lessen the beneficial impacts of a robotic system over the traditional role of a human surgeon. For example, compared with other surgical fields such as laparoscopy, intraocular surgery benefits from relatively unobstructed, high-magnification views of the surgical field. In addition, the minimally invasive nature of intraocular instrumentation and the high manoeuvrability and range of manually controlled surgical instruments present advantages to the eye surgeon.
Despite these advantages, intraocular microsurgery remains technically challenging to perform. Physical manipulation of tissue must be accomplished with exceptionally high accuracy and precision in a tiny workspace. The scale of these manipulations is so small that intrinsic physiological hand tremor becomes a substantial concern. In result, the ability to accurately target a specific anatomical site or hold the surgical instrument stationary for prolonged durations is difficult. Also, humans have limited resolution when it comes to depth perception [3]. This limited resolution is insufficient to sense the exact depth of the posterior capsule during cataract surgery or accurately sense the distance between the tool and retinal anatomy during vitreoretinal surgery. For these reasons, robotic systems offer a promising solution to these human limitations due to their enabling of precise, tremor-free motion and offer increased depth resolution through a variety of integrated imaging modalities such as digital microscopy and optical coherence tomography (OCT). These advantages naturally increase both the safety and efficacy of surgical procedures. By improving resolution and accuracy of depth-sensing capabilities, such unified systems promise to supersede the current practice of relying on human vision through an optical stereo microscope. Additional benefits of robotic surgery in ophthalmology include collaborative capabilities for specific procedures (partially to fully automated) and the integration of augmented visual, auditory, and tactile feedback.
Types of robotic surgical systems
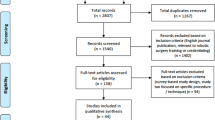
One method to categorise the range of intraocular robotic surgical systems is according to the degree of human vs. robotic control (Fig. 1).
-
(a)
In traditional surgery, a human surgeon controls the surgical tool(s) and uses an optical microscope as visual feedback.
-
(b)
In a robot-assisted tool, the surgical tool itself is modified to be a miniature robotic system (Fig. 2). The surgeon controls this tool to perform a hands-on surgical procedure while the robotic tool offers tremor cancellation, depth locking, and other features. An example of this type is “The MICRON”.
-
(c)
In teleoperated robotic surgery, the surgeon controls a robotic system through joysticks and uses an optical microscope or digital heads-up display as visual feedback. The joystick motion is directly mapped to robotic motion and therefore advantages such as haptic feedback, tremor filtering, and motion scaling can be implemented. Examples of this type include “RAM!S”, “The Preceyes Surgical System”, and “The intraocular robotic interventional surgical system (IRISS)”.
-
(d)
In a cooperative robotic system, the surgeon holds and controls the surgical tool simultaneously with the robotic system and uses a microscope and/or OCT as visual feedback. The surgeon maintains direct manual control over the motion of the surgical tool while the robotic system provides assistive compensation for hand tremor and allows for prolonged immobilisation of the surgical tool. An example of this type is the system from the “Catholic University of Leuven”.
-
(e)
Finally, in a partially or fully automated system, the robotic system is tightly integrated with the microscope and/or OCT to provide feedback and guidance to the motion commands of the robotic system, which directly holds and operates the surgical tool(s). Specific procedures or steps of a procedure are automatically performed by the robotic system while the surgeon supervises through the provided visual feedback. Override commands are commonly offered. An example of this type is “The intraocular robotic interventional surgical system (IRISS)”.
A hand-held robotic manipulator from the Robotics Institute at Carnegie Mellon University and Johns Hopkins University [5].
The following section presents the latest, most advanced intraocular robotic systems for each of the types outlined above.
Advanced surgical robotic systems
The MICRON
The MICRON, an active hand-held micro-manipulator was developed in 2010 through a collaboration between the Robotics Institute at Carnegie Mellon University and Johns Hopkins University [4]. Through an image-guidance approach, the handheld device reduced hand tremor to provide smooth motion during surgical procedures with a reported 52% reduction in tool-tip positional error. The tool was evaluated by performing retinal vein cannulation on ex vivo pig eyes and demonstrated an increase in success rate from 29 to 63% over the case of not using the augmented tool.
The MICRON was further improved in 2015 though incorporation of a Gough–Stewart platform that constrained the remote centre of motion near the tool tip [5]. The improved tool was evaluated under varying conditions to demonstrate trajectory-following errors of ≤20 µm and a 90% reduction in hand tremor. Most recently, the researchers demonstrated the ability to detect the puncture of a stretched vinyl membrane by integrating a force-sensing needle into the MICRON [6]. In addition, the group also demonstrated an automated position-holding feature that allowed the tool tip to be maintained inside an artificial vein for longer periods of time with significantly reduced tool-tip motion after venipuncture. However, to date, all evaluation studies have only been performed on artificial or animal eye models with no clinical evaluation.
RAM!S
In 2013, the Department of Robotics and Embedded Systems at the Technical University of Munich introduced RAM!S (Fig. 3), a hybrid parallel–serial mechanism that includes piezoelectric motors for actuation [7]. Kinematically, the mechanism consists of two joints coupled in parallel, one prismatic joint, and one optional revolute joint to collectively enable 6 DOF of tool motion [8]. The researchers claim the advantages of this mechanism include higher stiffness and increased precision over more common serial mechanism designs. RAM!S is also physically compact (94 ± 28 × 33.5 × 18.5 mm) and designed to secure to the head of a patient to mitigate the effects of patient motion. Additional cited metrics include a tool-tip positional precision of 5 µm, a total weight of 306 g, and a tool-tip workspace of 28 × 28 × 28 mm.
A novel mechanism from the Technical University of Munich [7].
The same team developed a virtual-fixture control method and experimentally evaluated its use on an ex vivo pig eye [9]. These virtual fixtures included the virtual constraint of the RCM and autonomous RCM adjustment. Additional work used the RAM!S device to develop teleoperated capabilities [10]. Using a controller that featured force feedback, a control scheme for the positional error was implemented. The resulting system allowed the surgeon to perform precise and comfortable micromanipulation. More recently, sub-retinal depth-tracking of a needle using OCT has been performed [11].
In the researcher’s latest work, the performance of the device’s software-constrained RCM was evaluated through a series of experiments using a tissue model and ex vivo pig eyes [12]. The RCM was demonstrated to operate with an accuracy of within 1 mm. Furthermore, the researchers used the system to track the depth of the needle during insertion into models, supplementing the microscopic imagery by also displaying OCT-generated volume scans of the needle. The researchers claimed that with the help of their system, surgeons could focus more on making decisions during sub-retinal injection and less on dexterous control of the tool.
The preceyes surgical system
The Eindhoven University of Technology in the Netherlands and later Preceyes B.V., a spin-off company of the university, has developed the Preceyes Surgical System (Fig. 4) as a high-precision device for vitreoretinal surgical procedures [13]. The robotic system is comprised of an input joystick held by the surgeon and a robotic system which controls the surgical instrument and performs the physical manipulation of intraocular tissue. The robotic system is rigidly secured to the operating room table or Stryker by a headrest and aligned to the surgical incision by the surgeon. By moving the input joystick, the surgeon can guide the motion of the tool through the incision and throughout the intraocular workspace. The surgeon uses a standard surgical microscope as visual feedback and the robotic system is compact enough to unobtrusively fit within the operating room environment.
An intraocular surgical system developed by Preceyes B.V [13].
The design of the robotic system is based on a parallelogram linkage common to many early surgical robotic systems. This design offers a mechanical remote centre of motion and improved tool-tip positional precision over serial linkages. The system’s safety and stability are enhanced by an adjustable counterweight which minimises the required joint torques and holds the system in a fixed configuration in the event of a power loss or system failure. The authors reported a tool-tip positional resolution of 10 µm and initially demonstrated the capabilities of Preceyes by creating venous occlusions in live, anesthetised pigs [13]. The use of the robot to assist in surgical procedures was considered amenable to the standard surgical workflow and allowed the surgeon to sit in his or her usual position.
In 2018, the Preceyes Surgical System was used to conduct a clinical trial to compare robot-assisted surgery with traditionally performed surgery [14]. In this study, two sets of trials were performed in patients requiring the removal of retinal membranes and in patients that required sub-retinal injection. In the first stage, the Preceyes system was used to lift a flap of a retinal membrane from the macula surface using a bevelled needle. Twelve patients with macular holes were recruited for this study and the patients underwent general anaesthesia maintained with muscle relaxation and mechanical ventilation to ensure elimination of spontaneous respiration. The tool-tip directional motion perpendicular to the retina was constrained to increments of 10 µm. Once positioned, the surgeon imposed a virtual boundary in the control software such that any additional depth commands would be prohibited and iatrogenic retinal trauma could be prevented. Although the robot-assisted surgeon required more time than the unassisted surgeon to perform the surgical procedures (295 s compared with 80 s), the degree of iatrogenic retinal trauma during robot-assisted surgeries (defined as retinal touches and micro-haemorrhages) was decreased.
In the second stage, the Preceyes was used to perform sub-retinal injection of recombinant tissue plasminogen activator (rtPA) in three patients with central vision loss due to sub-retinal haemorrhage. In this study, three patients were placed under local anaesthesia and the robot assisted in the delivery of 0.025–0.10 ml of rtPA into the sub-retinal space. In one patient, transient intraoperative exacerbation of cataract precluded a clear view of the cannula tip and was manually completed, but otherwise the sub-retinal injections were successfully performed in all three patients.
Indicative of the safety of the robotic system, the robot-assisted procedures resulted in fewer overall inadvertent retinal touches and micro-haemorrhages across all trials. No system malfunctions or technical glitches were encountered and the robotic system was deemed by the surgeon to be unobtrusive within the operating theatre. While the robot-assisted surgeon performed slower than unassisted surgeon, the decrease in surgical complications and the increased precision of the robotic system suggests a bright future for the incorporation of surgical robotics into the field of intraocular eye surgery. The Preceyes recently acquired CE mark status and is expected to continue undergoing clinical evaluation by Preceyes B.V.
Catholic University of Leuven System
In 2014, the Micro- and Precision Engineering Group at the Catholic University of Leuven presented a teleoperated robotic system (Fig. 5) complete with motion scaling, tremor compensation, and scaled force feedback [15]. This system is a co-manipulated robotic system designed to offer a surgeon increased stability and precision by reducing the magnitude of hand-generated tremor and facilitating the ability to maintain a fixed position for prolonged durations. The device consists of a parallel arm mechanism with a mechanical remote centre of motion and is controlled through a spherical mechanism. This system was used to perform retinal vein cannulation on in vivo pig eyes [16]. Complete success was defined as a stable intravenous position of the needle tip for more than 3 min, and was confirmed in 15 out of 18 eyes. No technical failures of the robotic device were reported.
The intraocular robotic system of the Catholic University of Leuven, Belgium [17].
Following this initial success, the same group reported on the clinical evaluation of their system in the world’s first, in-human, robot-assisted retinal vein cannulation [17]. In this study, four patients with retinal vein occlusion (RVO) were treated at the University Hospital of Leuven through a phase I clinical trial. The trial involved the injection of Ocriplasmin into targeted retinal veins (estimated diameters 100–150 µm) with injection durations of up to 10 min. The successful results demonstrated the technical feasibility of performing retinal vein cannulation with the aid of robotic technology using a stereo microscope and suitable intraocular illumination. The robotic system is now being developed by MYNUTIA, a spin-off company of the university and the project leads are working to commercialise the developed technology.
The intraocular robotic interventional surgical system (IRISS)
The IRISS was developed at the University of California, Los Angeles through collaboration between the Mechatronics and Control Laboratory and the Stein Eye Institute (Fig. 6). The overall goal of this work is to develop a robotic surgical system capable of performing anterior and posterior intraocular surgical procedures through combinations of augmented reality teleoperation and full automation.
First presented in 2013 [18], the IRISS was aimed at remotely performing a wide range of anterior and posterior segment surgical procedures. The robotic system features a quick tool-exchange mechanism capable of mounting any commercially available surgical instrument and switching between them outside of the eye in a matter of milliseconds. In addition, a novel aspect of this robotic system is its dual-arm configuration which enables two tools to be simultaneously used within the eye through two surgical incisions in close proximity about the mechanically determined remote centre of motion [19]. The surgeon teleoperates the robotic system from a distance through a pair of custom joysticks that are mapped to the robot motion with a collection of motion-scaling and tremor-reduction techniques. These features help increase the safety and improve the performance of the surgeon. The system enables three-dimensional visual feedback through a stereo camera integrated into the digital microscope and displayed to the surgeon via a heads-up monitor.
The IRISS was validated on a set of common cataract and vitreoretinal surgical procedures using ex vivo pig eyes in a standard operating theatre [20]. Using the IRISS, the surgeon was able to successfully perform teleoperated anterior lens capsulorhexis, viscoelastic injection, hydro-dissection, lens aspiration, retinal vein cannulation, and vitrectomy [18, 20]. In particular, retinal vein cannulation was performed to demonstrate the ability of the IRISS to perform accurate targeting tasks. In many of the procedures, the second arm was used to control an additional tool and demonstrate the unique ability of the IRISS to simultaneously operate two surgical instruments. Finally, the IRISS was the first robotic system to successfully perform a complete a curvilinear capsulorhexis and an entire cataract surgery from start to finish.
However, with the introduction of femtosecond laser systems and other emerging technological advances, the completion of specific steps of cataract surgery such as corneal incisions, capsulorhexis, and lens fragmentation can be accomplished without any manual manipulation of intraocular tissue. While these laser-based methods naturally improve safety and decrease surgical complications, they are unable to perform the removal of emulsified cortical material or the insertion of an intraocular lens implant. These steps must still be manually performed by a surgeon and surgical complications remain due to the physiological limitations of a human surgeon and deficiencies in sensing capabilities.
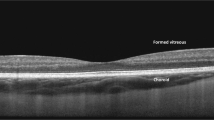
To this end, the IRISS was integrated with an OCT system and this feedback used to perform automated cataract extraction [21]. In this work (Fig. 7), ex vivo pig eyes were manually prepared by a surgeon and the robotic system modelled the eye anatomy, planned an extraction trajectory, and autonomously removed the lens material from the capsular bag. The system automatically aligns itself to the eye and guides an irrigation/aspiration handpiece through the corneal incision. The anatomical structures within the anterior segment are then identified and modelled from a set of preoperative OCT volume scans using an image-processing algorithm. This model is used by the system to plan a tool-tip trajectory through the capsular bag optimised for mobilising lens material and increasing surgical efficacy and efficiency while maintaining safety. This trajectory is then tracked by the system while controlling irrigation and aspiration forces as a function of tip-to-tissue distance. While the lens-extraction step is fully automated, intraoperative supervision and manual intervention abilities were provided to the surgeon. Intraoperative OCT scans localised around the tool tip are displayed to the surgeon in real time.
In the latest work from the IRISS group, the OCT-integrated robotic system was evaluated in a clinical setting on ex vivo pig eyes [22]. The automated procedure was performed on 30 eyes and preoperative, intraoperative, and postoperative OCT volume scans were acquired for analysis. In addition, microscope-based examination was performed by a trained surgeon to assess the integrity of the tissues and to determine if lens material remained. Results indicated that posterior capsule rupture was avoided in all 30 trials. Complete lens extraction was achieved on 25 of the samples—in five of the samples, minute particles of lens material were discovered in the postoperative evaluation hidden behind the iris where the OCT was unable to image.
Future work on the IRISS includes the integration of augmented reality and integration of specific, automated procedures into the surgical experience. We envision a surgical system with an augmented reality cockpit integrated with multi-sensory feedback including image overlays on microscope and OCT feedback displays, auditory, and haptic feedback. We have recently performed studies in the virtual environment (Fig. 8) to demonstrate that the addition of this feedback improves surgeon performance during pre-retinal membrane peeling procedures [23]. Participants over a range of skillsets were asked to perform virtual pre-retinal membrane peeling using two sets of feedback: (1) vision only and (2) vision with haptic feedback. The results demonstrated a reduction in task-completion time and retinal damage when the visual display was fully augmented.
Future applications for surgical robotics in ophthalmology
The incorporation of robotic systems into ophthalmological surgical practice promises improved precision and the possibility of entirely new surgical procedures that are currently infeasible or impossible to perform. Laser-based surgical procedures (such as femtosecond laser-assisted cataract surgery) have already provided super-human levels of accuracy and safety to lower intraoperative and postoperative complication rates. In addition, microscope-integrated OCT have enabled improved visualisation and introduced the ability to accurately sense depth during surgical procedures through incorporation of a real-time OCT image feed displayed alongside the microscope view. Despite these technological advances, surgical complications remain because manipulation of intraocular tissue remains dependent on human surgical skills, susceptible to hand tremor and subjected to limited resolution of depth perception.
For cataract surgery, robotic manipulators can be integrated with existing femtosecond laser systems to perform complete cataract extraction. Although cataract surgery is common and its complication rate is low compared with other intraocular surgeries, posterior capsule opacification (PCO) has been detected in 67% of surgical cases in a 4-year follow-up study [24]. PCO results from incomplete removal of lens from the capsular bag, caused by inadequate sensing and visualisation of the lens remnants—making complete removal difficult. Therefore, a future application of a robotic system is in the reduction of PCO through improved sensing of the lens equator and complete lens material cleaning in both pupillary and equatorial areas via capsular polishing techniques.
Sensing deficiencies also increase the risk of posterior capsule rupture, which is the most common complication that occurs during nucleus emulsification, cortex removal, and capsule polishing [25]. The capsular bag (including the posterior capsule) is an imperceptible and delicate tissue with thickness of ~10 µm [26]. Posterior capsule rupture may occur with inappropriate levels of aspiration or inaccurate manoeuvres of the phacoemulsification or irrigation/aspiration tool when in close proximity to the capsule. By combining high-resolution intraocular OCT imaging and high-accuracy robot manipulations, localisation of the posterior capsule in its entirety, from the posterior pole to the lens equator could be used to safely guide the surgical instrument for cataract extraction and subsequently reduce the risk of posterior capsule rupture. Furthermore, OCT feedback and accurate intraocular manipulation also enables precise OCT-guided intraocular lens implantation.
A potential future application of intraocular robotic systems includes gene and stem-cell therapy which are currently experiencing remarkable momentum for severe retinal disorders [27, 28]. To be effective, these procedures require accurate and prolonged injection in the vitreous or into the sub-retinal space where traditional intravitreal drug-delivery techniques are not ideal. Several studies on sub-retinal applications have been performed without robotic assistance and have demonstrated promising results in treating diseases such as age-related macular degeneration, Stargardt’s disease, and choroideremia [29,30,31,32]. However, compared with traditional intravitreal drug-delivery techniques, sub-retinal injection is associated with an increase in surgical complications such as vitreous haemorrhage, retinal detachment, and postoperative development of choroidal neovascularization [33, 34]. For these reasons, the method of drug delivery must be further studied to provide a safe and effective treatment option. A surgical robotic system is expected to possess the precision and accuracy critical for proper drug delivery and therefore may supersede human performance with hand-held tools.
Another potential future application of intraocular surgical robotic systems might involve the treatment of RVO. RVO is a hardening of a retinal vein and the formation of a blood clot that can cause vision loss through macular oedema, glaucoma, or vitreous haemorrhage and affects ~2% of the population [35]. One potential cure is retinal vein cannulation. In this technique, the clogged vein is cannulated by a micropipette and an anticoagulant is injected into the lumen to dissolve the clot. The anticoagulant must be continuously injected over a prolonged duration and therefore the surgical tool must be held steady inside the vein. However, retinal vein diameters are ~120–200 µm [36, 37] while human hand tremor has been measured as 200–350 µm [38]. Therefore, the motion stability and accurate positioning requirements results in a procedure that would be exceptionally difficult for a human surgeon to successfully perform, but not for a robotic system. To date, successful robot-assisted vein cannulation has been demonstrated in both animal models [13, 20, 39] and human patients [17] but has not yet received widespread validation as a safe and efficient therapeutical option.
In the immediate future, the direction of intraocular robotic systems is towards improved visualisation and robotic assistance of specific and routine tasks. Conceivably, these tasks could be fully or partially automated and independently performed from a human operator or surgeon. These achievements could only be accomplished through improved feedback from OCT or another image modality that is tightly integrated and accurately registered with the robotic system. Similarly, we envision surgical systems with immersive, augmented reality cockpits complete with multi-sensory feedback. Such integrated augmented reality visual displays could improve the safety and efficacy of performing complete intraocular procedures. This might be especially beneficial in complex retinal surgical cases such as dissecting severe pre-retinal tissue where accurate, bimanual manipulation is necessary but limited by current sensing capabilities and the difficulty of bimanual operation. In the distant future, it is conceivable that intraocular robotic systems guided by artificial intelligence could even possess the ability to make surgical decisions without any input from a human surgeon.
Conclusion
The full potential of robotics in intraocular surgical applications lies in the development of sight-improving or sight-saving procedures that are currently impossible for a human surgeon to perform. Prolonged cannulation of retinal vessels or accurate delivery of stem cells or gene-therapy drugs into sub-retinal spaces are applications that fall into this area, but there may be other applications, currently unimagined, waiting to be discovered. It has been widely demonstrated that improved tool precision can reduce anatomical damage and improve surgical outcomes in a clinical setting, and the ability to enable completely new surgical techniques uncommon in current practice is not unrealistic. Despite the potential, improvements to existing systems and their acceptance into general practice is required before intraocular surgical robotic systems can be commonly deployed into operating rooms or in the offices of practitioners.
References
Annual Report 2017, Intuitive Surgical, Inc. http://www.annualreports.com/HostedData/AnnualReportArchive/i/NASDAQ_ISRG_2017.pdf.
Warren H, Dasgupta P. The future of robotics. Investig Clin Urol. 2017;58:297–8.
Hibbard PB, Haines AE, Hornsey RL. Magnitude, precision, and realism of depth perception in stereoscopic vision. Cogn Res. 2017;2:25.
MacLachlan RA, Becker BC, Tabarés JC, Podnar GW, Lobes LA Jr, Riviere CN. Micron: an actively stabilized handheld tool for microsurgery. IEEE Trans Robot. 2011;28:195–212.
Yang S, MacLachlan RA, Riviere CN. Manipulator design and operation of a six-degree-of-freedom handheld tremor-canceling microsurgical instrument. IEEE/ASME Trans Mechatron. 2014;20:761–72.
Gonenc B, Chae J, Gehlbach P, Taylor RH, Iordachita I. Towards robot-assisted retinal vein cannulation: a motorized force-sensing microneedle integrated with a handheld micromanipulator. Sensors 2017;17:2195.
Nasseri MA, Eder M, Nair S, Dean EC, Maier M, Zapp D, et al. The introduction of a new robot for assistance in ophthalmic surgery. 2013 35th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). Osaka, Japan: IEEE; 2013. p. 5682–5.
Nasseri MA, Eder M, Eberts D, Nair S, Maier M, Zapp D, et al. Kinematics and dynamics analysis of a hybrid parallel-serial micromanipulator designed for biomedical applications. 2013 IEEE/ASME International Conference on Advanced Intelligent Mechatronics. Wollongong, Australia: IEEE; 2013. p. 293–9.
Nasseri MA, Gschirr P, Eder M, Nair S, Kobuch K, Maier M, et al. Virtual fixture control of a hybrid parallel-serial robot for assisting ophthalmic surgery: an experimental study. 5th IEEE RAS/EMBS International Conference on Biomedical Robotics and Biomechatronics. Sao Paulo, Brazil: IEEE; 2014. p. 732–8.
Barthel A, Trematerra D, Nasseri MA, Zapp D, Lohmann CP, Knoll A, et al. Haptic interface for robot-assisted ophthalmic surgery. 2015 37th Annual International Conference of the IEEE Engineering in Medicine and Biology Society (EMBC). Milan, Italy: IEEE; 2015. p. 4906–9.
Zhou M, Roodaki H, Eslami A, Chen G, Huang K, Maier M, et al. Needle segmentation in volumetric optical coherence tomography images for ophthalmic microsurgery. Appl Sci. 2017;7:748.
Zhou M, Yu Q, Mahov S, Huang K, Eslami A, Maier M, et al. Towards robotic-assisted subretinal injection: a hybrid parallel-serial robot system design and preliminary evaluation. IEEE Trans Ind Electron. 2019. https://ieeexplore.ieee.org/document/8818660.
de Smet MD, Stassen JM, Meenink TC, Janssens T, Vanheukelom V, Naus GJ, et al. Release of experimental retinal vein occlusions by direct intraluminal injection of ocriplasmin. Br J Ophthalmol. 2016;100:1742–6.
Edwards TL, Xue K, Meenink HC, Beelen MJ, Naus GJ, Simunovic MP, et al. First-in-human study of the safety and viability of intraocular robotic surgery. Nat Biomed Eng. 2018;2:649.
Gijbels A, Vander Poorten EB, Stalmans P, Van Brussel H, Reynaerts D. Design of a teleoperated robotic system for retinal surgery. 2014 IEEE International Conference on Robotics and Automation (ICRA). Hong Kong, China: IEEE; 2014. p. 2357–63.
Willekens K, Gijbels A, Schoevaerdts L, Esteveny L, Janssens T, Jonckx B, et al. Robot‐assisted retinal vein cannulation in an in vivo porcine retinal vein occlusion model. Acta Ophthalmol. 2017;95:270–5.
Gijbels A, Smits J, Schoevaerdts L, Willekens K, Vander Poorten EB, Stalmans P, et al. In-human robot-assisted retinal vein cannulation, a world first. Ann Biomed Eng. 2018;46:1676–85.
Rahimy E, Wilson J, Tsao TC, Schwartz S, Hubschman JP. Robot-assisted intraocular surgery: development of the IRISS and feasibility studies in an animal model. Eye. 2013;27:972–8.
Wilson JT, Tsao TC, Hubschman JP, Schwartz S. Evaluating remote centers of motion for minimally invasive surgical robots by computer vision. 2010 IEEE/ASME International Conference on Advanced Intelligent Mechatronics. Montreal, Canada: IEEE; 2010. p. 1413–8.
Wilson JT, Gerber MJ, Prince SW, Chen CW, Schwartz SD, Hubschman JP, et al. Intraocular robotic interventional surgical system (iriss): mechanical design, evaluation, and master–slave manipulation. Int J Med Robot Computer Assist Surg. 2018;14:e1842.
Chen CW, Lee YH, Gerber MJ, Cheng H, Yang YC, Govetto A, et al. Intraocular robotic interventional surgical system (IRISS): semi‐automated OCT‐guided cataract removal. Int J Med Robot Computer Assist Surg. 2018;14:e1949.
Chen CW, Francone AA, Gerber MJ, Lee YH, Govetto A, Tsao TC, et al. Semiautomated optical coherence tomography-guided robotic surgery for porcine lens removal. J Cataract Refractive Surg. 2019;45:1665–9.
Francone A, Huang JM, Ma J, Tsao TC, Rosen J, Hubschman JP. The effect of haptic feedback on efficiency and safety during preretinal membrane peeling simulation. Transl Vis Sci Technol. 2019;8:2.
Jorge PD, Jorge D, Ventura CV, Ventura BV, Ventura MC, Santhiago MR, et al. Incidence of posterior capsule opacification following the implantation of a foldable hydrophilic acrylic intraocular lens: a 4 year follow-up study. Arquivos Brasileiros de oftalmologia. 2014;77:222–4.
Desai P, Minassian DC, Reidy A. National cataract surgery survey 1997–8: a report of the results of the clinical outcomes. Br J Ophthalmol. 1999;83:1336–40.
Nordlund ML, Marques DM, Marques FF, Cionni RJ, Osher RH. Techniques for managing common complications of cataract surgery. Curr Opin Ophthalmol. 2003;14:7–19.
MacLaren RE, Bennett J, Schwartz SD. Gene therapy and stem cell transplantation in retinal disease: the new frontier. Ophthalmology. 2016;123:S98–106.
Schwartz SD, Regillo CD, Lam BL, Eliott D, Rosenfeld PJ, Gregori NZ, et al. Human embryonic stem cell-derived retinal pigment epithelium in patients with age-related macular degeneration and Stargardt’s macular dystrophy: follow-up of two open-label phase 1/2 studies. Lancet. 2015;385:509–16.
Rakoczy EP, Lai CM, Magno AL, Wikstrom ME, French MA, Pierce CM, et al. Gene therapy with recombinant adeno-associated vectors for neovascular age-related macular degeneration: 1 year follow-up of a phase 1 randomised clinical trial. Lancet 2015;386:2395–403.
Constable IJ, Pierce CM, Lai CM, Magno AL, Degli-Esposti MA, French MA, et al. Phase 2a randomized clinical trial: safety and post hoc analysis of subretinal rAAV. sFLT-1 for wet age-related macular degeneration. EBioMedicine. 2016;14:168–75.
Schwartz SD, Hubschman JP, Heilwell G, Franco-Cardenas V, Pan CK, Ostrick RM, et al. Embryonic stem cell trials for macular degeneration: a preliminary report. Lancet. 2012;379:713–20.
Schwartz SD, Tan G, Hosseini H, Nagiel A. Subretinal transplantation of embryonic stem cell–derived retinal pigment epithelium for the treatment of macular degeneration: an assessment at 4 years. Investigative Ophthalmol Vis Sci. 2016;57:ORSFc1–9.
Singh MS, Park SS, Albini TA, Canto-Soler MV, Klassen H, MacLaren RE, et al. Retinal stem cell transplantation: balancing safety and potential. Prog. Retinal Eye Res. 2019:100779. https://doi.org/10.1016/j.preteyeres.2019.100779.
Sørensen NB. Subretinal surgery: functional and histological consequences of entry into the subretinal space. Acta Ophthalmol. 2019;97:1–23.
Laouri M, Chen E, Looman M, Gallagher M. The burden of disease of retinal vein occlusion: review of the literature. Eye. 2011;25:981–8.
Goldenberg D, Shahar J, Loewenstein A, Goldstein M. Diameters of retinal blood vessels in a healthy cohort as measured by spectral domain optical coherence tomography. Retina. 2013;33:1888–94.
Wong TY, Islam FA, Klein R, Klein BE, Cotch MF, Castro C, et al. Retinal vascular caliber, cardiovascular risk factors, and inflammation: the multi-ethnic study of atherosclerosis (MESA). Investig Ophthalmol Vis Sci. 2006;47:2341–50.
Riviere CN, Rader RS, Khosla PK. Characteristics of hand motion of eye surgeons. Proceedings of the 19th Annual International Conference of the IEEE Engineering in Medicine and Biology Society. ‘Magnificent Milestones and Emerging Opportunities in Medical Engineering’ (Cat. No. 97CH36136). 4. Chicago, USA: IEEE; 1997. p. 1690–3.
de Smet MD, Meenink TC, Janssens T, Vanheukelom V, Naus GJ, Beelen MJ, et al. Robotic assisted cannulation of occluded retinal veins. PLoS ONE 2016;11:e0162037.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Gerber, M.J., Pettenkofer, M. & Hubschman, JP. Advanced robotic surgical systems in ophthalmology. Eye 34, 1554–1562 (2020). https://doi.org/10.1038/s41433-020-0837-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-0837-9