Abstract
Background
Dry eye disease (DED) is one of the most common conditions presenting to eye care providers and is increasingly recognized to have poor outcomes on quality of life, activities of daily living, and social and emotional well-being. Here, we aim to understand the association between dry eye symptoms and workplace productivity experienced by patients with non-Sjögren’s dry eye and Sjögren’s Syndrome.
Methods
MEDLINE, PubMed, Embase, Cochrane Library, CINAHL, Healthstar, and PsycINFO were searched from inception to May 2019.
Results
Thirty-one studies consisting of 50,446 study participants from 14 countries were included in this systematic review. Among non-Sjögren’s dry eye patients, there was significant absenteeism (ES = 0.19; 95% CI: [0.04, 0.35]), presenteeism (ES = 0.25; 95% CI: [0.15. 0.35]), productivity impairment (ES = 0.24; 95% CI: [0.20, 0.27]), activity impairment (ES = 0.30; 95% CI: [0.21, 0.38]), and subjective difficulties at work (ES = 0.58; 95% CI: [0.40, 0.75]). Patients with Sjögren’s Syndrome demonstrated significant absenteeism (ES = 0.13, 95% CI: [0.10, 0.17]), presenteeism (ES = 0.28, 95% CI: [0.24, 0.32]), productivity impairment (ES = 0.31, 95% CI: [0.27, 0.35]), and activity impairment (ES = 0.39, 95% CI: [0.32, 0.47]) in the workplace. In addition, patients with Sjögren’s Syndrome demonstrated significantly lower employment rate (ES = 0.42, 95% CI: [0.34, 0.50]), decreased number of hours worked (SMD = −0.21, 95% CI: [−0.39, −0.02]), and increased work disability (ES = 0.18; 95% CI: [0.09, 0.27]).
Conclusions
This is the first systematic review and meta-analysis to demonstrate the negative association between DED and several work productivity measures.
Similar content being viewed by others
Introduction
Dry eye disease (DED) is a multifactorial disease of the ocular surface characterized by aberrant tear film dynamics. DED is recognized as a worldwide health concern, with a prevalence ranging from 5 to 50% [1]. In the United States, more than 16 million adults have a clinical diagnosis of DED, and an additional 6 million people suffer from undiagnosed symptomatic dry eyes [2]. Although the disease is pervasive in women and older adults, DED is also increasingly diagnosed among young working adults [1, 3,4,5,6,7].
Among non-Sjögren’s Syndrome (non-SS) dry eye patients, the pathophysiology of DED is attributed to a combination of aqueous tear deficiency and increased tear evaporation [1, 8]. In contrast, dry eye symptoms in patients with Sjögren’s Syndrome (SS) is due to systemic immunologic dysfunction that results in autoimmune-driven inflammation of the ocular surface and lacrimal glands [1].
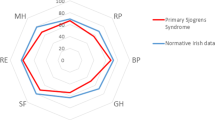
As a chronic and progressive condition, DED has a negative consequence on the physical and psychosocial domains of quality of life (QoL). Lacking a cure, patients seek medical care for persisting symptomatology, including foreign body sensation, blurred vision, pain, and photophobia, leading to significant utilization of medical resources and absence from work to attend medical appointments [1, 9, 10]. In severe DED, utility assessments have appraised the QoL impact to be equivalent to that of severe angina [11, 12] and worse than an immobilizing hip fracture [12]. Patients with DED commonly experience significant role restrictions secondary to physical limitations, decreased vitality, poorer general health, and increased bodily pain [13]. Blurred vision often interferes with visual tasks such as reading, driving, watching television, and the use of digital devices [1]. Moreover, dry eye has been linked to mental health outcomes such as depression [14,15,16,17,18], anxiety [15, 16], stress [16], and sleep disorders [19, 20].
In the last two decades, researchers have endeavored to develop a multidisciplinary understanding of the negative association of dry eye in the work environment and its socioeconomic implications. DED symptoms are often exaggerated in the workplace, fueled by electronic device usage, visually demanding tasks, suboptimal office illumination, and low indoor air quality [21, 22]. Consequently, work productivity and performance can be negatively affected, resulting in indirect costs such as absenteeism (missed work due to dry eye symptoms) and a significant economic burden to the patient and society [23,24,25]. In this systematic review and meta-analysis, we aim to characterize the relationship between dry eye and workplace functioning and the associated economic burden.
Methods
This systemic review protocol has been registered on PROSPERO (PROSPERO#CRD42019112182) and follows the preferred reporting items for systematic reviews and meta-analyses (PRISMA) recommendations and the meta-analysis of observational studies in epidemiology (MOOSE) guidelines for rigorous study methodology and reporting. The MOOSE statement checklist is detailed in Supplementary Appendix 1.
Search strategy and study selection
A formal literature search of the MEDLINE, PubMed, EMBASE, Cochrane Library, CINAHL, HealthSTAR, and PsycINFO databases was performed from inception to 4 December 2018. Variations of natural language terminology, as shown in our detailed search strategy (Supplementary Appendix 2), were used to retrieve eligible studies.
Two independent reviewers (GKS and JP) screened titles and abstracts and reviewed full-text articles using the inclusion and exclusion criteria. Covidence (Covidence Systematic Review software, Veritas Health Innovation, Melbourne, Australia), an online Cochrane study screening and data extraction tool, was utilized to screen, select, and assess the quality of included studies. Disagreements were resolved in a consensus meeting. References of all selected studies and relevant review articles were manually cross-referenced to identify relevant studies omitted by the search strategy. The search was rerun in May 2019 to identify newly published studies.
Study eligibility criteria
Study cohorts aged 18 years or older with symptomatic dry eyes or a clinical diagnosis of dry eye in non-SS DED and SS subjects were included. Studies examining the Sjögren’s population were differentiated between primary Sjögren’s Syndrome (pSS) and secondary Sjögren’s Syndrome (sSS) if specified. Primary SS is defined as an autoimmune disease occurring in isolation, while sSS occurs in association with other rheumatic diseases.
The association between dry eye diagnosis and workplace functioning was ascertained using outcome measures from validated questionnaires. The Work Productivity and Activity Impairment (WPAI) Questionnaire [26] defines absenteeism as work time missed due to dry eye; presenteeism as impairment at work or reduced on-the-job effectiveness; productivity impairment as overall work impairment, combining scores from absenteeism and presenteeism; and activity impairment as non-professional work impairment due to dry eye (e.g. housework). WPAI outcomes are expressed as impairment percentages, with higher numbers representing more significant impairment and reduced productivity. The Work Limitations Questionnaire [27] (WLQ) appraises four domains of work limitations, including time management (ability to manage time and schedule demands), physical demands (ability to perform tasks involving strength, movement, endurance, coordination, and flexibility), mental or interpersonal functioning (ability to navigate cognitive tasks and workplace social interactions), and output demands (ability to produce adequate work quantity and quality) to calculate overall work performance. A WLQ score of 0 implies no limitations, whereas a score of 100 identifies limitations 100% of the time. The Impact of Dry Eye on Everyday Life (IDEEL) instrument consists of a QoL module with three scales: work limitations, activity limitations, and emotional well-being. For each of these domains, a scale score is calculated between 0 (indicating total impairment) and 100 (indicating no impairment) [28].
Indirect costs of DED were explored using outcome measures such as hours worked, loss in paid or unpaid work hours, sick leave, and work disability. Other endpoints including subjective difficulty at work, recent work achievement, and job stress were also documented. All cost values were converted to represent monetary value in US dollars.
All original quantitative studies published in the English language were included. Data were retrieved from quantitative surveys designed to evaluate the impact of dry eye on daily activities and work functioning. While validated questionnaires were preferred, studies reporting data from non-validated rating scales were not excluded. Exclusion criteria included review articles, case reports, systematic reviews and meta-analyses, letters to editors, and commentaries. Conference abstracts were included if adequate study details and data were provided. Authors of published research works were contacted to obtain missing data or retrieve inaccessible articles. There were no restrictions placed on publication year or geographical settings.
Methodological assessment and data extraction
Critical appraisal of eligible studies was completed using the 27-item Modified Downs and Black Checklist, a validated instrument, to evaluate overall study quality for randomized and non-randomized studies (Supplementary Appendix 3). Study quality was independently scored by two reviewers (GKS and JP); disagreements were resolved through discussion and consensus. The quality assessment scores were as follows: excellent (26–27); good (20–25); fair (15–19); and poor (≤14). As per the quality appraisal criteria, only randomized controlled studies could achieve an “excellent” level of methodological quality.
A standardized data abstraction form, developed a priori, was used by two independent reviewers (GKS and JP) to collect the following data: author, publication year, study design, geographic location, study period, sample size, mean age of study participants, percentage of female participants, disease duration, employment characteristics, rating scale(s) or questionnaire(s), and the aforementioned study endpoints.
Statistical analysis
Meta-analysis was completed using STATA v. 15.0 (STATA Corporation, College Station, TX). The primary outcomes of interest were proportions, mean values, and standard deviation (SD). If unreported, SD was calculated using the range, confidence interval, standard error (SE), and p-value.
For continuous scale outcomes such as mean values, standardized mean difference (SMD) was calculated as the treatment effect or effect size as per the Cochrane Handbook for Systematic Reviews of Interventions [29]. SMD was chosen as the treatment effect since it is a mean difference standardized across all studies. To compute SMD for each study, the difference in mean values between DED and control cohorts for an outcome measure was divided by the SD for that same outcome measure. Weights were assigned to each SMD according to the inverse of its variance to compute the average. To estimate the summary effect, SMD for each study was then aggregated using the fixed or random-effect model based on the presence of heterogeneity.
To test heterogeneity, I2 statistics, Z-value, and χ2 statistics were computed. An I2 value < 50% implies low heterogeneity, and in these cases, a fixed-effect model was computed. An I2 statistics of 50% or more represents high heterogeneity, and as such, a random-effects model was calculated. In addition, a high Z-value, a low p-value (<0.01), and a large χ2 value imply significant heterogeneity, and therefore, a random-effects model using the DerSimonian and Laird methods was computed. Forest plots were generated for each outcome measure. Funnel plots were used to identify publication bias for each outcome measure.
Results
Selection process
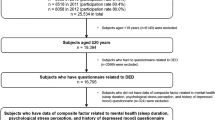
Of 4565 retrieved references, 209 studies were selected for full-text evaluation. After the full-text assessment, 27 studies and four conference abstracts met the eligibility criteria for study inclusion (Fig. 1).
Study characteristics
Table 1 describes the demographic characteristics of the 31 studies included in this systematic review. Selected studies consisted of 87,369 study participants including healthy controls (n = 70,430), non-Sjögren’s (non-SS) DED (n = 15,350), and Sjögren’s Syndrome (SS) (n = 1,589). As the correlation between DED and work productivity and the economic burden was reported in a subset of study cohorts, relevant data from 50,446 study participants are presented in this systematic review and consist of the following subgroups: non-SS DED (n = 8,292); Sjögren’s Syndrome (n = 1,516); and healthy controls (n = 2,687). The remaining 37,951 participants represent the study population from Farrand et al. [30], where the sample size among their dry eye and control groups were not delineated. The geographical distribution of the included studies is illustrated in Supplementary Fig. 1.
Outcome measures
The primary objective of the study was to analyze and quantify the relationship between dry eye and the following outcome measures: absenteeism (work time missed due to dry eye), presenteeism (impairment at work due to dry eye), productivity impairment (overall work impairment comprising of absenteeism and presenteeism scores), activity impairment (non-professional work impairment), work or activity limitations, employment rate, number of hours worked, and work disability. This relationship was directly explored in the non-Sjögren’s dry eye cohorts and indirectly in patients with Sjögren’s Syndrome known to experience sicca symptoms.
Risk of bias
Using the Modified Downs and Black Checklist, most studies were assessed as “fair” (n = 18) or “good” (n = 11) study quality; only two studies had “poor” methodological evaluation (Supplementary Table 1). Due to limited available evidence, articles were not excluded from the analysis based on methodological rigor.
To identify publication bias, funnel plots comprised of scatter plots of the effect estimates from individual studies against the SE of a study’s sample size were generated (Supplementary Figs. 2 and 3). Among non-SS dry eye studies, analysis of funnel plots of meta-analyses for absenteeism, presenteeism, productivity impairment, and activity impairment, as well as difficulty at work and IDEEL domains, did not reveal any asymmetry (Supplementary Fig. 2a–f). In addition, studies consisting of the pSS patient population are symmetrically distributed on both sides of the combined effect size line in the funnel plots for absenteeism, presenteeism, productivity impairment, activity impairment, employment rate, hours worked, and work disability (Supplementary Fig. 3a–g).
Work productivity and impairment in DED
Eight studies [30,31,32,33,34,35,36,37], three of which focused on patients with Sjögren’s Syndrome, reported absenteeism, presenteeism, productivity impairment, and activity impairment using the WPAI rating scale (Supplementary Table 2).
In the non-Sjögren’s population, Fig. 2a–d summarizes the results for absenteeism (missed work-time due to dry eye), presenteeism (impairment at work due to dry eye), productivity impairment (overall work impairment due to absenteeism and presenteeism), and activity impairment (impairment in non-professional activities). Three studies [31, 32, 34] evaluated the relationship of DED with absenteeism and presenteeism, while four studies [30,31,32, 34] explored productivity and activity impairment in DED. High heterogeneity was observed for studies exploring absenteeism (I2 = 89.6%; p = 0.000), presenteeism (I2 = 64.3%; p = 0.061) and activity impairment (I2 = 85.4%; p = 0.000). Studies analyzing productivity impairment, on the contrary, had low heterogeneity (I2 = 36.1%; p = 0.196). Absenteeism (time lost at work due to DED symptoms) was reported to be significant (ES = 0.19; 95% CI: [0.04, 0.35]). Dry eye was also associated with impairment in workplace activities or presenteeism (ES = 0.25; 95% CI: [0.15, 0.35]). As expected, productivity (ES = 0.24; 95% CI: [0.20, 0.27]) and activity impairment (ES = 0.30; 95% CI: [0.21, 0.38]) were also observed among the DED subgroup.
Figure 2a–d describes outcomes in the non-Sjögren’s dry eye population, including a absenteeism, b presenteeism, c productivity impairment, and d activity impairment. Figure 2e–h reports outcome measures from patients with Sjögren’s Syndrome, including e absenteeism, f presenteeism, g productivity impairment, and h activity impairment.
Using a scale of 0 (no effect) to 10 (completely prevented one from working) in a WPAI questionnaire, McDonnell et al. [38] demonstrated a statistically significant mean productivity loss (1.63 ± 2.54 vs. 0.17 ± 0.66; p = 0.0003) and mean activity impairment (1.83 ± 2.3 vs. 0.59 ± 1.62; p < 0.0001) in DED subjects compared to age-matched controls. There were no statistically significant differences in hours missed due to health and hours worked between both cohorts. As outcomes were reported using a unique methodology, this study could not be included in our meta-analysis.
Figure 2e–h illustrates a forest plot of a proportion of subjects with Sjögren’s Syndrome experiencing absenteeism, presenteeism, productivity impairment, and activity impairment. Between three studies [35,36,37] with SS cases, non-significant heterogeneity was observed for absenteeism (I2 = 15.5%; p = 0.306), presenteeism (I2 = 0.0%; p = 0.397) and productivity impairment (I2 = 0.0%; p = 0.446), while high heterogeneity was found for activity impairment (I2 = 52.8%; p = 0.120). Absenteeism (ES = 0.13, 95% CI: [0.10, 0.17]), presenteeism (ES = 0.28, 95% CI: [0.24, 0.32]), productivity impairment (ES = 0.31, 95% CI: [0.27, 0.35]), and activity impairment (ES = 0.39, 95% CI: [0.32, 0.47]) were significant among pSS subjects.
Non-SS DED and limitations in the workplace
Using the WLQ instrument, Uchino et al. [39] and Yamada et al. [40] identified a statistically significant loss in work performance among subjects with ‘definite’ DED (4.8%) and ‘self-reported’ DED (6.1%) subgroups, respectively, compared to control groups (Supplementary Table 3). Intriguingly, the presence of dry eye was concomitantly associated with increased mental and interpersonal demands compared to healthy controls [39, 40]. A qualitative analysis of four studies reporting work limitations using the IDEEL scale demonstrated scores ranging from 62 to 85 out of 100 among non-SS dry eye subjects, where a score of 100 indicated a lack of work limitations (Supplementary Table 4) [29, 34, 41, 42]. In the same cluster of studies, daily activity limitations and emotional well-being scores ranged from 72 to 86 and 62 to 85, respectively, out of 100. Figure 3a summarizes a meta-analysis of two studies [29, 42] comparing IDEEL outcomes between subjects with non-Sjögren’s DED and healthy cohorts. Significant heterogeneity between the two studies examining work limitations (I2 = 99.5%; p = 0.000), daily activity limitations (I2 = 99.6%; p = 0.000), and emotional wellbeing (I2 = 99.4%; p = 0.000) was observed. Findings suggests non-significant differences in work limitations (SMD = −5.23; 95% CI: [−12.28, 1.81]), daily activity limitations (SMD = −5.66, CI: [−14.54, 3.22]), and emotional well-being (SMD = −4.25; CI: [−9.60, 1.10]) between DED and healthy cohorts. However, the strength of our interpretation is limited due to a small sample size of studies.
Corresponding to the above findings, studies investigating the non-SS (n = 4) and SS (n = 1) patient population reported subjective difficulties in the workplace due to dry eye, ranging from 22 to 75% [21, 43,44,45,46]. Figure 3b illustrates the results of four studies [21, 43, 44, 46] investigating subjective difficulties at work in the non-SS DED population. While there was significant heterogeneity between studies (I2 = 96.0%; p = 0.000), our meta-analysis revealed that subjects experience significant difficulty at work due to DED (ES = 0.58; 95% CI: [0.40, 0.75]) compared to healthy controls. In a Chinese study, a qualitative survey utilizing the National Eye Institute Visual Function Questionnaire (NEIVF-Q) revealed that dry eye symptoms impacted daily work, reading activities, emotional wellbeing, interpersonal relations, and sleep at ‘most’ of the times [47].
A cross-sectional survey across five European countries by Labetoulle and colleagues [44] demonstrated that patients perceive their DED as significantly associated with discomfort and daily pain and highly impactful on work life. Interestingly, a longer time to diagnosis and more frequent use of dry eye treatments was correlated with an increased burden of daily discomfort, pain, activity constraints, and impact on work life. Similarly, in a US-based study, patients with Sjögren’s disease described a significant impact of their illness in multiple facets of daily life, including physical activity, intimacy, career productivity, daily activities, social interactions and mental alertness compared to controls [48]. This study also validated that the negative association of DED on QoL domains was significantly higher among those with severe sicca symptoms compared to low sicca severity groups. Interestingly, a Korean study investigated the link between DED, recent work achievement and job stress and did not identify any statistically significant differences between dry eye and control groups [49].
Miljanović et al. [50] reported that those with dry eye symptoms were more likely to report difficulties carrying out professional work (OR = 3.49; 95% CI: [1.72–7.09]; p = 0.001) and activities of daily living (OR = 4.80; 95% CI: [2.47–9.35]; p < 0.001) compared to control subjects. Among the included studies, only two studies [50, 51] assessed for possible gender differences in workplace functioning in the dry eye population. Adjusting for confounding variables, Miljanović et al. [50] found that there were no significant gender differences in challenges with professional work as a result of DED (men: OR = 4.1; 95% CI: [1.84–9.13] vs. women: OR = 3.06; 95% CI: [1.72–5.44]). Likewise, Schaumberg and colleagues [51] did not identify gender-based disparities related to problems in carrying out professional duties (OR = 1.35, 95% CI: [0.97–1.83]; p < 0.05).
Economic burden of DED
Among a mixed cohort of subjects with DED, including those with Sjögren’s Syndrome, Nelson et al [23] reported a need to decrease work hours (11.4%) or change the line of work (7.1%) as a result of dry eye symptoms. In addition, in a typical DED patient, dry eye symptoms impaired the performance of work tasks on an average of 191 days per year and contributed to two days of absence from work. Bowman and colleagues [52] suggested a diminished capacity to work in pSS patients and demonstrated a statistically significant loss of regular paid hours from the current weekly schedule, unpaid work (housework time loss), and outside help (loss of hours spent by an individual working as a “helper” to aid the patient).
Studies reporting the employment characteristics of patients with Sjögren’s Syndrome are demonstrated in Supplementary Table 5 [37, 48, 52,53,54,55,56,57]. A subset of studies (n = 6) revealed high rates of work disability in pSS patients compared to control subjects, ranging from 5 to 66% [37, 48, 52,53,54,55,56,57]. Remarkably, Mandl et al. [55] reported an escalating trend in the rate of health-related work disability from the time of pSS diagnosis (26%) to 12 months (37%) and 24 months (41%) post-diagnosis. The relative risk of absence due to sick leave increased from the time of diagnosis (RR = 1.44) to 24 months after diagnosis (RR = 2.67) [55]. Meijer and colleagues [56] demonstrated an average sick leave of 14.7 days and 22.3 days per year among pSS and sSS patients, respectively.
Figure 4a shows a forest plot consisting of seven studies [37, 48, 52, 53, 56, 57], reporting the employment rate among patients with Sjögren’s Syndrome. Considerable heterogeneity (I2 = 81.2%; p = 0.000) was observed between these studies. Thus, a random-effects model was developed and identified that only 42% of SS patients were employed in a full-time or part-time job (ES = 0.42, 95% CI: [0.34, 0.50]). With non-significant heterogeneity (I2 = 37.7%, p = 0.201) observed, a meta-analysis of three studies indicated significantly fewer hours worked by SS patients (SMD = −0.21; 95% CI: [−0.39, −0.02]) compared to healthy controls (Fig. 4b) [37, 56, 57]. Figure 4c synthesizes results from five studies that examined work disability in the SS patient population and demonstrates significant work disability in SS patients (ES = 0.18; 95% CI: [0.09, 0.27]) [37, 48, 53,54,55]. Significant heterogeneity (I2 = 90.7%, p = 0.000) was observed among these five studies.
Among one of the most extensive economic studies conducted to date in dry eye management, Yu et al. [33] analyzed survey data from over 2,000 DED patients across the United States. The annual cost to society from diminished work productivity significantly outweighed the direct costs of DED medical treatment, and the total productivity loss per person ranged from $US 12,569 to $US 18,168 on an annual basis. Using a conservative, low estimate economic model, Bowman and colleagues [52] have reported the cost of illness in pSS patients to an approximate total indirect cost of $US 9,919 ($7,184–$12,654) compared to $US 1,152 ($397–$1,910) among control subjects. Indirect costs include time lost from work due to illness based on an existing work schedule among employed subjects, time lost performing household/voluntary work, and time spent by another individual (“helper”) assisting the person obtaining healthcare services. In a population-level study based on Canadian data, McCormick et al. [37] reported an adjusted excess productivity cost for paid and unpaid work as an average of $US 60 and $US 59 per week, respectively, among SS participants compared to healthy cohorts. Patients with Sjögren’s Syndrome were predicted to incur lost productivity costs of $US 3,126 each year compared to control subjects. Similarly, a Japanese study by Uchino et al. [39] reported a predicted productivity loss of $US 6,160 per person in those with definite DED and $US 2,444 in the probable DED group. In another Japanese study, the cost of work productivity loss per person exceeded by $US 799 in the ‘definite’ dry eye group compared to control groups [40].
Discussion
Occupational medicine is increasingly recognized as an effective platform for addressing health issues and initiating health promotion strategies to mitigate health risks and improve healthy living and economic productivity. However, the impact of ophthalmic diseases on workplace functioning is understudied. Here, we present the first systematic review and meta-analysis to underscore the relationship between DED and functional outcomes in the workplace. Patients with non-Sjögren’s dry eye experience significant absenteeism and subjective difficulties in the workplace. Sjögren’s Syndrome was associated with pronounced productivity and activity impairment, presenteeism, and absenteeism in the work environment. Moreover, patients with Sjögren’s Syndrome demonstrated decreased employment rate, reduced number of hours worked and increased work disability.
Quality of evidence and limitations
Aside from the limited number of available published studies reporting workplace dysfunction in the context of DED, the power of this systematic review was limited by the clinical, methodological, and statistical heterogeneities of included studies. From a clinical perspective, patients with DED included in this study consisted of varying disease durations, diagnostic criteria, and disease severity. Study subjects ranged from patients with asymptomatic and symptomatic non-SS dry eye to those with DED secondary to the autoimmune phenomenon, Sjögren’s Syndrome. Aside from xerophthalmia, Sjögren’s Syndrome is also tethered to a cluster of systemic manifestations, including xerostomia, dry skin, arthritis, and neuropathy. While our study findings related to the Sjögren’s subgroup may be valid, it remains unclear whether the dry eye phenomenon alone contributes to impaired work productivity and challenges in the workplace in this complex patient population. As such, the strength of our interpretation may be limited based on patient differences in DED etiology and related confounding factors. Albeit the significant differences in the non-SS and SS DED population, our meta-analyses ultimately underscore the significance of dry eye in the workplace, particularly across all WPAI domains, in both populations. In this study, it should be noted that we were unable to perform direct comparisons against the non-SS and SS subgroups due to the limited availability of comparative studies.
Studies included in this systematic review depended on data derived from self-administered questionnaires. Although many studies utilized commonly available and validated questionnaires, there was variability in the rating scales and parameters used to diagnose DED. The lack of consistency and reliability among included studies in the diagnostic parameters used for DED yields to methodological disparities. Moreover, data from non-validated questionnaires or generic health questionnaires such as SF-36 were not included in our meta-analyses and could not contribute to the value of our study findings. For future studies, we recommend using validated rating scales, particularly the Work Productivity and Activity Impairment (WPAI), Work Limitations Questionnaire (WLQ), Impact of Dry Eye on Everyday Life (IDEEL), and Stanford Health Assessment Questionnaire (SHAQ), which are proven to be sensitive in discriminating difficulties with workplace activities. In addition to the significant disparities across rating instruments, our study was limited in sample size by questionnaire-specific outcome measures. Moreover, non-English language citations were excluded in this study due to translation difficulties, contributing to the low sample size of included studies. As such, additional studies are required to make concrete conclusions in this area of interest.
Relationship between dry eye and workplace function
Our current understanding of the relationship between dry eye and work function is widely based on self-administered questionnaires. While our study has identified a negative correlation between dry eye and diminished workplace productivity and performance, the cause and effect relationship between these variables remains elusive and warrants further investigation.
A growing body of evidence describes strong associations between DED and mental health outcomes such as depression, anxiety, suicidal ideation, and sleep disorders [14,15,16, 19, 20]. DED is not only clinically associated with psychiatric comorbidities but also with chronic fatigue syndrome as well as chronic pain syndromes (CPS) [58, 59]. Patients with DED reported more frequent chronic pain syndromes, worse dry eye symptoms, and low ocular and non-ocular pain scores [59]. A large cohort study by Venof et al. [60] demonstrated a heritable component among CPS, including chronic widespread musculoskeletal pain (CWP), chronic pelvic pain (PP), irritable bowel syndrome (IBS), and DED. These conditions are co-inherited in families with shared genetic factors between CWP, PP, IBS, and DED.
Furthermore, as a systemic autoimmune disorder, primary Sjögren’s Syndrome causes profound fatigue symptoms in its patient population. In a large cohort study by Hackett et al. [61], physical and mental fatigue was associated with pain and depression, and particularly, ocular dryness was strongly associated with physical fatigue. Research experts hypothesize that an inherent level of somatization may contribute to the ocular symptoms of dry eye and give rise to chronic pain syndromes and physical fatigue [15]. Naturally, this can also lead to mental health concerns, diminished work productivity and performance, and overall reduced QoL. However, to establish the relationship between these complex variables, further investigation is necessary.
Therefore, with these multifaceted interactions in mind, our findings ultimately suggest the importance of clinician-led discussions surrounding workplace difficulties in DED patients and the development of personalized dry eye self-management plans to facilitate improved workplace performance. Eye care providers must assess for and acknowledge challenges endured by DED patients, such as performing sustained visual tasks or working in environments with harsh fluorescent lighting, low humidity, or poor air quality. Tailored interventions such as frequent ocular lubrication, specialized moisture-retaining eyewear, humidification of the environment, adjustments to office illumination, and ergonomic placement of computer monitors are examples of measures that can improve or alleviate symptoms of dry eye in the work environment.
As electronic devices dominate workspaces and create visually demanding tasks, workplace accommodations, or modified work duties may be necessary to support employees and optimize work productivity and performance based on their DED severity. Furthermore, the literature demonstrates that it is not uncommon for DED patients to reduce work hours, change the line of work, and take a leave of absence to manage dry eye symptoms. Absenteeism and productivity loss due to DED unsurprisingly result in significant economic costs to employers and the government. Understanding the negative consequence of DED on QoL outcomes, including an individual’s work and economic potential, eye care providers, employers, and policy-makers need to acknowledge and address the challenges of DED in the workplace.
Conclusions
Our study findings suggest that DED appears to negatively alter the landscape of work productivity and economic capacity among the Sjögren’s Syndrome and non-Sjögren’s dry eye patient population. Although the dry eye population is quite heterogeneous, our meta-analyses have demonstrated that dry eye has a bearing on absenteeism, presenteeism, productivity impairment, and activity impairment in non- Sjögren’s DED and Sjögren’s Syndrome. An improved understanding of how DED impacts work productivity will allow clinicians to counsel patients on symptom management at work and encourage employers to develop a tailored approach for workplace accommodations for DED patients. Further studies using standardized and validated questionnaires to understand DED in the workplace are necessary to shed light on the humanistic and economic burden of DED.
Summary table
What was known before:
-
Dry eye disease (DED) is among the most common ocular surface diseases worldwide and is often the leading reason for patient visits to general practitioners, emergency departments, and eye care providers.
-
DED is a chronic and unremitting disease increasingly recognized to diminish the quality of life and impair activities of daily living, social health, and emotional well-being.
What this study adds:
-
Thirty-one studies consisting of 50,446 study participants were included in this systematic review, 19 of which were included in the meta-analysis, to study the association between DED and work productivity.
-
Non-Sjögren’s dry eye patients experience significant absenteeism, presenteeism, productivity and activity impairment, and subjective difficulties in the workplace.
-
Similarly, patients with Sjögren’s Syndrome demonstrated pronounced absenteeism, presenteeism, productivity impairment, and activity impairment in their work environments.
-
Additionally, patients with Sjögren’s Syndrome displayed a lower employment rate, decreased number of hours worked, and increased work disability.
-
Our study findings suggest that DED is negatively associated with work productivity and economic capacity among patients with Sjögren’s Syndrome and non-Sjögren’s dry eye.
-
Ophthalmologists and optometrists, as well as general practitioners, managing dry eye patients should be aware of the potential for impaired work performance and, as such, aim to optimize treatment of dry eye symptoms and tailor workplace accommodations appropriately.
References
Stapleton F, Alves M, Bunya VY, Jalbert I, Lekhanont K, Malet F, et al. TFOS DEWS II epidemiology report. Ocul Surf. 2017;15:334–65.
Farrand KF, Fridman M, Stillman IO, Schaumberg DA. Prevalence of diagnosed dry eye disease in the United States among adults aged 18 years and older. Am J Ophthalmol. 2017;182:90–8.
Yazdani C, McLaughlin T, Smeeding JE, Walt JG. Prevalence of treated dry eye disease in a managed care population. Clin Ther. 2001;23:1672–82.
Matossian C, McDonald M, Donaldson KE, Nichols KK, MacIver S, Gupta PK. Dry eye disease: consideration for women’s health. J Women’s Health. 2019;28:502–14.
Vehof J, Sillevis Smitt-Kamminga N, Nibourg SA, Hammond CJ. Sex differences in clinical characteristics of dry eye disease. Ocul Surf. 2018;16:242–8.
Blehm C, Vishnu S, Khattak A, Mitra S, Yee RW. Computer vision syndrome: a review. Surv Ophthalmol. 2005;50:253–62.
Tsubota K, Nakamori K. Dry eyes and video display terminals. N Engl J Med. 1993;328:584.
The definition and classification of dry eye disease: Report of the Definition and Classification Subcommittee of the International Dry Eye WorkShop (2007). Ocul Surf. 2007;5:75–92.
Tsubota K, Yokoi N, Shimazaki J, Watanabe H, Dogru M, Yamada M, et al. New Perspectives on Dry Eye Definition and Diagnosis: A Consensus Report by the Asia Dry Eye Society. Ocul Surf. 2017;15:65–76.
Koh S. Mechanisms of visual disturbance in dry eye. Cornea. 2016;35:S83–8.
Buchholz P, Steeds CS, Stern LS, Wiederkehr DP, Doyle JJ, Katz LM, et al. Utility assessment to measure the impact of dry eye disease. Ocul Surf. 2006;4:155–61.
Schiffman RM, Walt JG, Jacobsen G, Doyle JJ, Lebovics G, Sumner W. Utility assessment among patients with dry eye disease. Ophthalmology. 2003;110:1412–9.
Mertzanis P, Abetz L, Rajagopalan K, Espindle D, Chalmers R, Snyder C, et al. The relative burden of dry eye in patients’ lives: comparisons to a U.S. normative sample. Invest Ophthalmol Vis Sci. 2005;46:46–50.
Zheng Y, Wu X, Lin X, Lin H. The prevalence of depression and depressive symptoms among eye disease patients: a systematic review and meta-analysis. Nat Sci Rep. 2017;7:46453.
Wan KH, Chen LJ, Young AL. Depression and anxiety in dry eye disease: a systematic review and meta-analysis. Nat Eye. 2016;30:1558–67.
Asiedu K, Dzasimatu SK, Kyei S. Impact of dry eye on psychosomatic symptoms and quality of life in a healthy youthful clinical sample. Eye Contact Lens. 2018;44(Suppl 2):S404–9.
Jonas JB, Wei WB, Xu L, Rietschel M, Streit F, Wang YX. Self-rated depression and eye diseases: The Beijing Eye Study. PLoS ONE. 2018;3:e0202132.
Um SB, Yeom H, Kim NH, Kim HC, Lee HK, Suh I. Association between dry eye symptoms and suicidal ideation in a Korean adult population. PLoS ONE. 2018;13:e0199131.
Au NH, Mather R, To A, Malvankar-Mehta MS. Sleep outcomes associated with dry eye disease: a systematic review and meta-analysis. Can J Ophthamol. 2019;54:180–9.
Na K, Han K, Park Y, Na C, Joo C. Depression, Stress, Quality of Life, and Dry Eye Disease in Korean Women: A Population-Based Study. Cornea. 2015;34:733–8.
van Tilborg M, Murphy PJ, Evans KS. Impact of dry eye symptoms and daily activities in a modern office. Optom Vis Sci. 2017;94:688–93.
Wolkoff P, Karcher T, Mayer H. Problems of the ‘outer eyes’ in the office environment: an ergophthalmologic approach. J Occup Environ Med. 2012;54:621–31.
Nelson JD, Helms H, Fiscella R, Southwell Y, Hirsch JD. A new look at dry eye disease and its treatment. Adv Ther. 2000;17:84–93.
Reddy P, Grad O, Rajagopalan K. The economic burden of dry eye: a conceptual framework and preliminary assessment. Cornea. 2004;23:751–61.
McDonald M, Patel DA, Keith MS, Snedecor SJ. Economic and Humanistic Burden of Dry Eye Disease in Europe, North America, and Asia: A Systematic Literature Review. Ocul Surf. 2016;14:144–67.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4:353–65.
Lerner D, Amick BC III, Rogers WH, Malspeis S, Bungay K, Cynn D. The Work Limitations Questionnaire. Med Care. 2001;39:72–85.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. (eds). Cochrane Handbook for Systematic Reviews of Interventions, 6th edn. Cochrane 2019. Available from www.training.cochrane.org/handbook.
Rajagopalan K, Abetz L, Mertzanis P, Espindle D, Begley C, Chalmers R, et al. Comparing the discriminative validity of two generic and one disease-specific health-related quality of life measures in a sample of patients with dry eye. Value Health. 2005;8:168–74.
Farrand KF, Stillman IÖ, Fridman M, Schaumberg DA. Impact of dry eye disease on quality of life, work productivity, daily activities, and health care resource in a survey of 74,095 American adults [abstract]. Value Health. 2016;19:A127.
Nichols KK, Bacharach J, Holland E, Kislan T, Shettle L, Lunacsek O, et al. Impact of dry eye disease on work productivity, and patients’ satisfaction with over-the-counter dry eye treatments. Invest Ophthalmol Vis Sci. 2016;57:2975–82.
Patel VD, Watanabe JH, Strauss JA, Dubey AT. Work productivity loss in patients with dry eye disease: an online survey. Curr Med Res Opin. 2011;27:1041–8.
Yu J, Asche CV, Fairchild CJ. The economic burden of dry eye disease in the united states: a decision tree analysis. Cornea. 2011;30:379–87.
Sindt CW, Foulks GN. Efficacy of an artificial tear emulsion in patients with dry eye associated with meibomian gland dysfunction. Clin Ophthalmol. 2013;7:1713–22.
Baldini C, Bartoloni E, Priori R, Carubbi F, Alunno A, Quartuccio L. Work productivity in primary sjögren’s syndrome: a cross-sectional multicenter study [abstract]. Ann Rheum Dis. 2016;75:552.
Bejarano M, Secco A, Catalan Pellet A, Mamani M, Papasidero S, Demarchi J et al. Work productivity and activity impairment in primary Sjögren’s Syndrome. Arthritis Rheumatol. 2017; 69 (Suppl 10). (abstract)
McCormick N, Marra CA, Sadatsafavi M, Kopec JA, Aviña-Zubieta JA. Excess Productivity Costs of Systemic Lupus Erythematosus, Systemic Sclerosis, and Sjögren’s Syndrome: A General Population-Based Study. Arthritis Care Res. 2019;71:142–54.
McDonnell PJ, Pflugfelder SC, Stern ME, Hardten DR, Conway T, Villaneuva L, et al. Study design and baseline findings from the progression of ocular findings (PROOF) natural history study of dry eye. BMC Ophthalmol. 2017;17:265.
Uchino M, Uchino Y, Dogru M, Kawashima M, Yokoi N, Komuro A, et al. Dry eye disease and work productivity loss in visual display users: the Osaka study. Am J Ophthalmol. 2014;157:294–300.
Yamada M, Mizuno Y, Shigeyasu C. Impact of dry eye on work productivity. Clinicoecon Outcomes Res. 2012;4:307–12.
Camp A, Wellik SR, Tzu JH, Feuer W, Arheart KL, Sastry A, et al. Dry eye specific quality of life in veterans using glaucoma drops. Cont Lens Anterior Eye. 2015;38:220–5.
Pouyeh B, Viteri E, Feuer W, Lee DJ, Florez H, Fabian JA, et al. Impact of ocular surface symptoms on quality of life in a united states veteran affairs population. Am J Ophthalmol. 2012;153:1061–6.
Kawashima M, Yamatsuji M, Yokoi N, Fukui M, Ichihashi Y, Kato H, et al. Screening of dry eye disease in visual display terminal workers during occupational health examinations: the Moriguchi study. J Occup Health. 2015;57:253–8.
Labetoulle M, Rolando M, Baudouin C, van Setten G. Patient’s perception of DED and its relation with time to diagnosis and quality of life: an international and multilingual survey. Br J Ophthalmol. 2017;101:1100–5.
Sullivan RM, Cermak JM, Papas AS, Dana MR, Sullivan DA. Economic and quality of life impact on dry eye symptoms in women with Sjögren’s Syndrome. Adv Exp Med Biol. 2002;506(Pt B):1183–8.
van Tilborg M, Kort H, Murphy P, Evans K. The influence of dry eye and office environment on visual functioning. Stud Health Technol Inf. 2015;217:427–31.
Wang Y, Lv H, Liu Y, Jiang X, Zhang M, Li X, et al. Characteristics of symptoms experienced by persons with dry eye disease while driving in China 2017; 31:1550-5.
Segal B, Bowman SJ, Fox PC, Vivino FB, Murukutla N, Brodscholl J, et al. Primary Sjögren’s Syndrome: health experiences and predictors of health quality among patients in the United States. Health Qual Life Outcomes. 2009;7:46.
Cho KJ, Kim HK, Lim MH, Baek HS, Yang YA, Kang BH, et al. Depression, ADHD, job stress, and sleep problems with dry eye disease in Korea. J Psychiatry. 2015;18:331–5.
Miljanović B, Dana R, Sullivan DA, Schaumberg DA. Impact of dry eye syndrome on vision-related quality of life. Am J Ophthalmol. 2007;143:409–15.
Schaumberg DA, Uchino M, Christen WG, Semba RD, Buring JE, Li JZ. Patient reported differences in dry eye disease between men and women: impact, management, and patient satisfaction. PLoS ONE. 2013;8:e76121.
Bowman SJ, St. Pierre Y, Sutcliffe N, Isenberg DA, Goldblatt F, Price E, et al. Estimating indirect costs in primary Sjögren’s Syndrome. J Rheumatol. 2010;37:1010–5.
Callaghan R, Prabu A, Allan B, Clarke AE, Sutcliffe N, Pierre YS, et al. Direct healthcare costs and predictors of costs in patients with primary Sjögren’s Syndrome. Rheumatology. 2007;46:105–11.
Dias LH, Miyamoto ST, Valim V, Altoé R. Impact of Symptoms and Disease Activity on Quality of Life in Primary Sjögren’s Syndrome. Ann Rheum Dis. 2015;74(Suppl 2):812. (abstract 0422).
Mandl T, Jørgensen TS, Skougaard M, Olsson P, Kristensen L. Work disability in newly diagnosed patients with primary Sjögren’s Syndrome. J Rheumatol. 2017;44:209–15.
Meijer JM, Meiners PM, Huddleston Slater JJR, Spijkervet FK, Kallenberg CG, Vissink A, et al. Health-related quality of life, employment and disability in patients with Sjögren’s Syndrome. Rheumatology. 2009;48:1077–82.
Westhoff G, Dörner T, Zink A. Fatigue and depression predict physician visits and work disability in women with primary Sjögren’s syndrome: results from a cohort study. Rheumatology. 2012;51:262–9.
Chen C, Cheng H, Chen H, Tsai S, Kao C, Lin H, et al. Dry eye syndrome and the subsequent risk of chronic fatigue syndrome – a prospective population-based study in Taiwan. Oncotarget. 2018;9:30694–703.
Galor A, Covington D, Levitt AE, McManus KT, Seiden B, Felix ER, et al. Neuropathic ocular pain due to dry eye is associated with multiple comorbid chronic pain syndromes. J Pain. 2016;17:310–8.
Venof J, Zavos HMS, Lachance G, Hammond CJ, Williams FMK. Shared genetic factors underlie chronic pain syndromes. Pain. 2014;155:1562–8.
Hackett KL, Davies K, Tarn J, Bragg R, Hargreaves B, Miyamoto S, et al. Pain and depression are associated with both physical and mental fatigue independently of comorbidities and medications in primary Sjögren’s syndrome. RMD Open. 2019;5:e000885.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
There was no external funding source acquired for this research. The authors do not have any financial relationships or conflicts of interest to disclose in relevance to this article.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41433_2020_1282_MOESM6_ESM.docx
Supplementary Figure 2. Funnel plots for outcome measures derived from the Work Productivity and Activity Impairment (WPAI) questionnaire for non-Sjögren’s dry eye studies including (a) absenteeism, (b) presenteeism, (c) productivity impairment, and (d) activity impairment. Other outcomes include (e) difficulty at work and (f) Impact of Dry Eye on Everyday Living (IDEEL) questionnaire domains. The effect estimates and the standard error (SE) are plotted on the horizontal and vertical axes. A symmetrical funnel plot indicates no publication bias.
41433_2020_1282_MOESM7_ESM.docx
Supplementary Figure 3. Funnel plots for outcome measures in patients with Sjögren’s Syndrome, including (a) absenteeism, (b) presenteeism, (c) productivity impairment, (d) activity impairment, (e) employment rate, (f) hours worked, and (g) work disability. The effect estimates and the standard error (SE) are plotted on the horizontal and vertical axes. A symmetrical funnel plot indicates no publication bias.
41433_2020_1282_MOESM8_ESM.docx
Supplementary Table 1. Methodological assessment of included studies using the Modified Downs and Black Quality Assessment Checklist.
41433_2020_1282_MOESM9_ESM.docx
Supplementary Table 2. Work productivity and activity impairment among Sjögren’s Syndrome and non-Sjögren’s dry eye populations.
41433_2020_1282_MOESM10_ESM.docx
Supplementary Table 3. Work performance loss and limitations in the workplace, including time management, physical demands, mental or interpersonal demands, and output demands in the general dry eye population using the Work Limitations Questionnaire (WLQ).
41433_2020_1282_MOESM11_ESM.docx
Supplementary Table 4. Impact of dry eye on work limitations, daily activity, and emotional well-being among non-Sjögren’s dry eye patients using the Impact of Dry Eye on Everyday Living (IDEEL) questionnaire.
41433_2020_1282_MOESM12_ESM.docx
Supplementary Table 5. Employment characteristics of patients with Sjögren’s Syndrome, including employment rate, hours worked, sick leave, and work disability rate.
Rights and permissions
About this article
Cite this article
Sivakumar, G.K., Patel, J., Malvankar-Mehta, M.S. et al. Work productivity among Sjögren’s Syndrome and non-Sjögren’s dry eye patients: a systematic review and meta-analysis. Eye 35, 3243–3257 (2021). https://doi.org/10.1038/s41433-020-01282-3
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01282-3