Abstract
Purpose
To investigate outcomes for small versus large pupils in cataract surgery using different pupil expansion techniques.
Methods
Retrospective case-series reviewing 20,175 patients’ cataract surgery electronic medical records at Moorfields Eye Clinic in Bedford Hospital NHS Trust from January 2010 to April 2020. Outcomes such as visual acuity (VA), intraocular pressure, intraoperative, post-operative complications were recorded and small pupil expansion device outcome.
Results
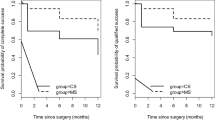
One thousand, four hundred twenty-six patients were identified as having small pupil (SP). Of these, 1110 patients (77.8%) had interventions to expand the pupil including 447 (31.3%) with intracameral phenylephrine (IC PE) alone, 194 (13.6%) with iris hooks and 469 (32.9%) with a Malyugin ring. The large pupil (LP) group had a statistically significant greater gain in VA than the SP group (p < 0.05). SPs had a significantly higher rate of intraocular complications including posterior capsular rupture (PCR) with vitreous loss (OR 2.75, p < 0.001). There was also a significantly higher rate of post-operative complications such as corneal oedema (OR 2.64, p < 0.001) and anterior uveitis (OR 2.11, p < 0.001) in the SP group. However, VA improvement and complications between the different pupil expansion groups showed no significant differences (p > 0.05) except for a greater rate of iris tears in the Malyugin group (p < 0.05).
Conclusion
To date, this is the largest reported case-series comparing Malyugin rings and iris hooks with other pupil expansion techniques. The various techniques to expand pupil size appear to be safe and equally effective in improving VA with a similar rate of complications except for a greater rate of iris tears with Malyugin ring.
Similar content being viewed by others
Introduction
In cataract surgery, the presence of small pupils (SPs) presents a major challenge [1]. It is estimated that 1–3% of cataract surgeries are associated with a SP. A SP restricts the area that the surgeon is able to work within and increases the chance of damaging the pupillary or capsular edge with surgical instruments. Visibility is also limited in smaller pupils as is the intensity of the red reflex, making it more difficult to perform capsulorrhexis and to crack and remove the nucleus. Thus, SPs are associated with increased complications including posterior capsule rupture (PCR) [1, 2]. Other possible complications arising from these limitations include damage to the iris and corneal endothelium. Common co-morbidities described in patients with SP include intraoperative floppy iris syndrome (IFIS), mitotic topical therapy and pseudoexfoliation syndrome (PXF).
IFIS is characterised by poor pupillary response and increased propensity for iris billowing and prolapse [3]. IFIS can occur with the current use of systemic alpha-1 antagonists which are used to treat benign prostatic hyperplasia. Tamsulosin has been identified as the most likely α-blocker causing IFIS, with risks increased up to forty times more compared to other alpha-1 antagonists and causing more severe IFIS [4]. IFIS can also occur with the use of other non-selective alpha-1 antagonists such as alfuzosin and terazosin [4].
Pupil dilation techniques have therefore been used to address smaller pupils and/or patients with IFIS or PXF. These techniques range from topical and intracameral mydriatics, iris hooks/retractors, Malyugin dilator rings and viscomydriasis. Topical mydriatics can act as sympathomimetics (phenylephrine), and anticholinergic agents (tropicamide or cyclopentolate). A combination of phenylephrine and tropicamide produces a stronger mydriatic effect than when used individually [5]. Mechanical dilation techniques such as hooks and rings work by direct mechanical manipulation to increase pupillary size intraoperatively. Viscoamydriasis is also used to increase pupil diameter, without the need of further pupil expansion devices [3].
There is a paucity of data available concerning visual outcome measures and complication rates in cataract surgery using pupil expansion devices in particular when comparing Malyugin rings and iris hooks with other techniques. We therefore investigated the outcomes and complication rates of pupil dilation techniques at our centre.
Methods
All patients who had cataract surgery without additional procedures between January 2010 and April 2020 were included. A retrospective study on cataract surgery electronic medical records at Moorfields Eye Clinic in Bedford Hospital NHS Trust was undertaken. Only consultants, senior fellows and senior staff grade surgeons were included. This research followed the principles in the Helsinki declaration and internal ethics approval was obtained.
Phacoemulsification was performed using the Infiniti machine (Alcon Laboratories, Switzerland). A 6.25 or 7.0 mm, 5–0 Malyugin ring or five flexible iris hooks were used. The choice of pupil expansion technique was determined by the operating surgeon. The pupil size was subjectively determined by the operating surgeon.
Data was collected from the electronic medical records system (Medisoft, Ltd, UK). This included baseline demographics, operated eye, co-morbidities (α-blocker use, corneal pathology, glaucoma, diabetes, age-related macular degeneration (AMD), PXF, dense cataract, retinal pathology, high myopia, amblyopia), biometry measurements, surgeon, intraoperative (IFIS, descemet membrane (DM) tear, iris prolapse, iris tear, PCR, vitreous loss, zonule dialysis) and post-operative complications (cystoid macular oedema (CMO), anterior uveitis, atonic pupil, retinal tear or detachment) visual acuity (VA), intraocular pressure (IOP) and pupil expansion technique if SP. VA was recorded as best corrected logMAR pre-operatively and then at 4 weeks post-operative. The data was accurate and complete because the system employs a forced manual entry mechanism which must be completed before a letter can be generated. Each free text entry box was also analysed to ensure that the correct data was extracted.
Statistical analysis
Multivariate analysis using repeated measures were conducted to compare the effects of group (large vs. SP) on IOP and VA. Where significant, post hoc testing was completed with covariates accounted for. Covariates of interest included: corneal pathology, AMD, diabetes, retinal pathology, glaucoma, amblyopia, IFIS, α-blocker, dense cataract, PXF and high myopia.
Explanatory models were tested using logistical regression analysis to determine predictors of complications for both large and SPs. Separate analysis was carried out for each complication. Pupil size was entered at the first step of analysis with the second step of analysis demographics (age, gender, ethnicity) and co-morbidities entered as explanatory models.
Multivariate analysis using repeated measures was also conducted to compare the effects of the intervention (intracameral phenylephrine (IC PE), Malyugin ring, iris hooks, no intervention) on IOP and VA. Post hoc tests used the Bonferroni correction. All statistical analyses was conducted using IBM Statistical Package for Social Sciences (SPSS) v26.
Results
A total of 20,175 patients were included, of which 1426 had SPs. In the SP group, 1110 patients (77.8%) had interventions to expand the pupil including 447 (31.3%) with IC PE alone, 194 (13.6%) with iris hooks and 469 (32.9%) with a Malyugin ring. The mean patient age was 78.6 in the SP group and 74.9 in the large pupil (LP) group. The SP group had more males (58%) whereas the LP group had more females (59%). Table 1 shows baseline clinical parameters and pre-operative versus post-operative logMAR VA outcomes between small and LPs. Mean duration of follow-up was 367.3 days in the SP group and 323.6 in the LP group.
Small pupil vs. large pupil outcomes
Intraoperative complications
The SP group, whilst controlling for other independent variables (corneal pathology, AMD, diabetes, retinal pathology, glaucoma, amblyopia, IFIS, α-blocker, dense cataract, PXF and high myopia), had a significantly higher rate of intraocular complications including PCR with vitreous loss (OR 2.75 (CI 1.69–4.46, p < 0.001)), DM tear (OR 8.42 (CI 3.32–21.35, p < 0.001)), Iris tear (OR 8.40 (CI 3.07–22.97, p < 0.001)), and zonular dialysis (OR 4.74 (CI 2.40–9.40, p < 0.001)). No significant increase risk was found for the SP group for retinal tears or detachments (p > 0.05).
Within these complications, specific risk factors were identified after controlling for other independent variables. There was a significantly higher rate of PCR in patients with dense cataracts (OR 4.71 (CI 2.68–8.29, p < 0.001)). Dense cataracts (OR 4.60 CI 1.84–11.51, p = 0.001)) and PXF (OR 17.82 (CI 0.49–5.48, p < 0.001)) also increased the rate of zonular dialysis. Whereas IFIS (OR 5.49 (CI 1.59–18.89, p = 0.007)) was the only significant risk factor for iris tears.
Post-operative complications
There was a significantly higher rate of atonic pupil (OR 50.26 (CI 18.16–139.12, p < 0.001)), corneal oedema (OR 2.64 (CI 1.99–3.50, p < 0.001)), CMO (OR 1.77 (CI 1.15–2.71, p < 0.01)) and anterior uveitis (OR 2.11 (CI 1.35–3.31, p < 0.001)) in the SP group after controlling for other independent variables. The risk of CMO was also independently increased by co-morbidities including diabetes (p = 0.03), corneal pathology (p < 0.001), and having a dense cataract (p < 0.001). The risk of corneal oedema was also independently increased by co-morbidities including glaucoma, corneal pathology and dense cataracts (p < 0.001).
Small pupil expansion technique outcomes
Pre-operative versus post-operative logMAR VA improvement between the different pupil expansion strategies showed no significant difference when all other independent variables were controlled (p > 0.05). There were also no significant differences in post-operative IOP outcomes between the groups (p > 0.05). Table 2 shows intraoperative and post-operative complications between the different pupil expansion techniques. The proportion of patients with iris tears was significantly higher in the Malyugin ring group than in those cases requiring no intervention, IC PE alone or iris hooks. The proportion of endothelial damage with DM tears was also higher in the Malyugin ring group although post-operative corneal oedema was greater in the iris hooks group, however, neither of these were statistically significant. Although the proportion of patients who had a loss of ≥3 logMAR lines was highest in the SP group which had no intervention, this did not reach significance.
Discussion
This study comprehensively examines both the intraoperative and post-operative outcomes indicators for the most commonly employed pupil expanding techniques. Baseline characteristics were similarly matched in terms of age, gender, and ethnicity. The primary outcome of VA improvement was encouragingly improved in both small and LP groups but the difference was significantly greater for LPs. The SP group also had a significantly greater proportion of patients who lost three or more logMAR lines of vision reflecting the increased risk to these patients.
Complications were noted to be increased in both the intraoperative and post-operative phases with SPs. SPs had higher rates of PCR, DM tears, iris tears, atonic pupil, corneal oedema, CMO, anterior uveitis and zonular dialysis. This is unsurprising as SP cataract surgery often have other co-morbidities and anatomical challenges which require additional surgical manipulation [6]. In our study, PXF was associated with a higher incidence of SPs and dense cataract. Furthermore, as this study highlights, additional steps are necessary which in itself induces risks and complications.
Previous groups have shown a low rate of intraoperative complications for Malyugin ring and iris hooks [7,8,9]. Similarly in our study, we found a low overall rate of intraoperative complications for both techniques except for a higher rate of iris tears in the Malyugin ring group. It was also reassuring to see equivalent VA gains regardless of pupil expansion technique and no differences in significant loss of vision (loss of three or more logMAR lines) between them. Additionally, we report a low rate of post-operative complications with a long duration of follow-up for which there is limited data. Nderitu and colleagues [9] found higher rates of post-operative corneal oedema and anterior uveitis with Malyugin rings. However, at our centre, after controlling for co-variables in our multivariate analysis we did not confirm this. In their study they did not use a multivariate analysis and therefore it is possible other co-variables may have led to these increases in the Malyugin ring group.
It may not be surprising that the Malyugin ring has a higher rate of iris tears. When the Malyugin ring is deformed during retraction, the scrolls can unpredictably crush or release the pupil margin. This is because the scrolls behave like a torsional spring and compression spring with narrowing of the gap as the arms are moved towards each other and vice versa [10]. The new Malyugin ring 2.0 has tried to eliminate some of these issues by having a new smaller gauge material thereby reducing the amount of force required to compress the ring by 70%. Furthermore, larger spacing in between anterior and posterior scrolls allows for easier engagement and disengagement from the iris [6].
To date, this is the largest study of its kind comparing iris hooks and Malyugin rings to other pupil expansion techniques; demonstrating equivalent overall safety and VA outcomes. Another advantage of our study was that all cataract surgeries were performed by senior independent surgeons, reducing the risk posed by the learning curve of trainee surgeons which will induce further data bias. Furthermore, this study’s data was derived from a single centre where widespread electronic patient records exists. There is also forced entry whereby the record cannot be completed without specific options being selected, ensuring high completion rates, consecutive cases and accuracy. Each surgical record was also reviewed for their free text comments as surgeons often include information in other areas including devices used or complications. This reduced the risk of transcriptional or recall bias. We ensured that other independent co-variables were adequately controlled for in the multivariate analysis.
Limitations include that over the period of the study, a new iteration of the ring had emerged but it was only used at our centre from mid-2019. The actual size of the pupil was not measured directly but rather categorised for the electronic medical record system and determined by the surgeon. Furthermore, we did not have a reason for why a particular technique was used, although it appears many of the surgeons had a particular preference. It is likely that the ring was used in more complicated cases which may influence the results. Additionally, we are not aware at what threshold the technique was employed, or the decision making process behind it. It is often based on their experience of management of a SP or their surgical experience to successfully complete a case with a SP, in addition to their handling of the first eye cataract case; this may have introduced systematic bias which could have their influenced the results in this study. Whilst there was excellent digital recording, the study design was retrospective in nature and all the data was derived from a single centre. In particular, post-operative VA outcomes were missing for a proportion of patients as well as the aetiology of the cataract not being available because of the retrospective collection.
In conclusion, to date, this is the largest observational study exploring the outcomes of iris hooks and Malyugin rings to other pupil expansion techniques in cataract surgery. The use of all the different SP management techniques led to successful and safe management of SPs with no significant difference in post-operative VA or IOP between techniques. However, extra care when using the Malyugin rings may be warranted to reduce the risk of iris trauma.
Summary
What was known before
-
Smaller pupils in cataract surgery can often be challenging to manage and may lead to higher rates of complication.
-
Several techniques available and commonly used to manage the SP in cataract surgery.
What this study adds
-
SPs were shown to have higher rates of specific complications.
-
The most commonly used devices to expand the SP appear to have equivalent visual and safety outcomes.
Change history
23 July 2021
A Correction to this paper has been published: https://doi.org/10.1038/s41433-021-01689-6
References
Sparrow JM, Taylor H, Qureshi K, Smith R, Birnie K & Johnston RL. The Cataract National Dataset electronic multi-centre audit of 55,567 operations: risk indicators for monocular visual acuity outcomes. Eye. 2012;26:821–6.
Narendran N, Jaycock P, Johnston RL, Taylor H, Adams M, Tole DM et al. The Cataract National Dataset electronic multicentre audit of 55,567 operations: risk stratification for posterior capsule rupture and vitreous loss. Eye. 2009;23:31–7.
Chang DF, Osher RH, Wang L, Koch DD. Prospective multicenter evaluation of cataract surgery in patients taking tamsulosin (Flomax). Ophthalmology. 2007;114:957–64.
Chatziralli IP, Sergentanis TN. Risk factors for intraoperative floppy iris syndrome: a meta-analysis. Ophthalmology. 2011;118:730–5.
Park J-H, Lee Y-C, Lee S-Y. The comparison of mydriatic effect between two drugs of different mechanism. Korean J Ophthalmol. 2009;23:40–2.
Grzybowski A, Kanclerz P. Methods for achieving adequate pupil size in cataract surgery. Curr Opin Ophthalmol. 2020;31:33–42.
Akman A, Yilmaz G, Oto S, Akova YA. Comparison of various pupil dilatation methods for phacoemulsification in eyes with a small pupil secondary to pseudoexfoliation. Ophthalmology. 2004;111:1693–8.
Chang DF. Use of Malyugin pupil expansion device for intraoperative floppy-iris syndrome: results in 30 consecutive cases. J Cataract Refract Surg. 2008;34:835–41.
Nderitu P, Ursell P. Iris hooks versus a pupil expansion ring: operating times, complications, and visual acuity outcomes in small pupil cases. J Cataract Refract Surg. 2019;45:167–73.
Bhattacharjee S. Pupil-expansion ring implantation through a 0.9 mm incision. J Cataract Refract Surg. 2014;40:1061–7.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised: Unfortunately, the spelling of the author’s name Rynda Nitiahpapand was incorrect.
Rights and permissions
About this article
Cite this article
Balal, S., Jbari, A.S., Nitiahpapand, R. et al. Management and outcomes of the small pupil in cataract surgery: iris hooks, Malyugin ring or phenylephrine?. Eye 35, 2714–2718 (2021). https://doi.org/10.1038/s41433-020-01277-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01277-0
This article is cited by
-
Evaluation of a uniplanar pupil expansion ring in small-pupil cataract surgery: a feasibility study
International Ophthalmology (2022)
-
Post-Radiation Cataract Management: Outcomes in Individuals with Uveal Melanoma
Current Ophthalmology Reports (2022)