Abstract
Background
To report the indications, visual outcomes, and intra-operative and post-operative complications of iris-sutured posterior chamber intraocular lens (IOL) in eyes with inadequate capsular support and complex ocular history.
Methods
A chart review and data analysis of eyes that underwent iris fixation of posterior chamber (PC) IOL for correction of aphakia, dislocated and subluxed IOLs, ectopia lentis, and IOL exchange. Data included clinical risk factors, associated eye conditions, previous surgeries, and concomitant procedures. The pre-operative and post-operative vision, manifest refraction, endothelial cell density, intraocular pressure (IOP), as well as intra-operative and post-operative complications were also recorded.
Results
One hundred and seventeen eyes from 114 patients were examined with a mean follow-up of 22.4 months. The most common identifiable predisposing risk factor was high myopia in 23 eyes. A significant improvement in uncorrected and best corrected visual acuity compared with baseline was observed. The most common post-operative complications included recurrent IOL subluxation in 16 (13.7%) eyes, IOP spike in 7 (5.9%) eyes, cystoid macular oedema in 5 (4.3%) eyes, and epiretinal membrane formation in 4 (3.4%) eyes. There was one (0.85%) case of sterile endophthalmitis.
Conclusions
Iris suture fixation of PC IOLs is a good treatment option for eyes with inadequate capsular support and complex ocular history.
Similar content being viewed by others
Introduction
Phacoemulsification is one of the most commonly performed procedures worldwide [1]. The latest improvements in surgical equipment and intraocular lens (IOL) designs made this procedure safe and efficacious. However, complicated cases are still encountered. Post-operative in-the-bag IOL dislocation is one such example, with an incidence ranging from 0.2 to 3% [2,3,4]. In addition, spontaneous crystalline lens dislocations, trauma, and zonulopathy, among others, may leave inadequate capsular support for IOL to be implanted in-the-bag.
In eyes lacking capsular support, several options for primary or secondary IOL implantation exist. An anterior chamber (AC) IOL can be placed using either the angular support or with iris fixation (iris claw). Alternatively, a posterior chamber (PC) IOL may be placed with either iris fixation (using suture or claw) or scleral fixation (suture, glue, or intrascleral haptic fixation). A recent metanalyses found no evidence of superiority among these options, although complications differed [5]. AC IOLs—although easy to implant—can result in endothelial decompensation or secondary glaucoma [6, 7]. Scleral-sutured IOLs can cause suture-related complications of suture breakage, erosion, and exposure, with endophthalmitis being the most feared outcome [8]. Retinal detachment (RD), intraocular haemorrhage, and elevated intraocular pressure (IOP) are also occasionally encountered [8, 9]. An intrascleral haptic fixation technique has been increasing in popularity with many modifications being used [10, 11].
Iris fixation offers some advantages including shorter surgical time and lower risk of intraocular haemorrhage and glaucoma progression [5]. Nonetheless, it can also be associated with potential complications, including pigment dispersion, chronic inflammation, progressive anterior synechia formation, and pupillary distortion leading to glare or halos [12,13,14]. The purpose of the current study was to assess the visual and refractive outcomes and complications of iris-sutured PC IOL implantation in eyes with inadequate capsular support and complex ocular history.
Materials and methods
This retrospective chart review was approved by the institutional review board at the Johns Hopkins University and was conducted in accordance with Health Insurance Portability and Accountability Act (HIPAA) regulations and Declaration of Helsinki. The charts of all patients who underwent iris fixation of a three-piece foldable acrylic IOL (MA50BM; Alcon Laboratories, Inc, Fort Worth, TX) from January 2010 to July 2018 for correction of aphakia, dislocated and subluxed IOLs, ectopia lentis, and IOL exchange were analysed. Patients with insufficient data or follow-up period less than 3 months were excluded. A total of 117 eyes from 114 patients met our inclusion criteria and were included in this study. These eyes have not been reported on before.
Patient records were reviewed, and the following baseline data were collected: demographic information, associated eye conditions, time from initial cataract surgery and information on previous surgeries, predisposing risk factors, concomitant procedures, and indications for iris suture fixation. Baseline and post-operative data were recorded for uncorrected (UCVA) and best corrected visual acuity (BCVA), manifest refraction (MRx), IOP, and number of glaucoma medications. Data on central corneal endothelial cell density (ECD) was also collected whenever available. Measurement of ECD was performed using a noncontact specular microscope (Cellchek, Konan Medical, Irvine, CA). Endothelial cell loss (ECL) was expressed as the percentage of pre-operative to post-operative change in ECD over the pre-operative ECD.
All surgeries were performed by the same surgeon (YJD) at an academic tertiary referral centre.
The surgical procedure has been described in detail by our group [15, 16]. Briefly, hydrophobic acrylic three-piece IOL (MA50BM, Alcon Laboratories, Inc, Fort Worth, TX) was used in all cases. It was folded in a moustache technique and inserted into the AC. Then it was gently unfolded in a pupillary capture technique with the haptics being below the iris and the optic above. The haptics were sutured to the mid-peripheral iris with two modified McCannel sutures using 10–0 prolene on a CTC needle. The sutures were then cut at the knot and internalised. After that, the IOL optic was pushed behind the iris with the help of a Sinskey hook.
Ocular examination with Snellen visual acuity, tonometry, and slit-lamp biomicroscopy was performed on all patients at 1 day (POD1), 1 week (POW1), 1 month (POM1), and all subsequent post-operative visits. All post-operative complications were recorded. High myopia was defined as an axial length > 26 mm. IOP spike was defined as IOP ≥ 30 mmHg on POD1. Corneal oedema was defined as a new-onset post-operative oedema that persisted >1 month. Cystoid macular oedema (CME) was defined as a new-onset post-operative oedema that was confirmed with optical coherence tomography (OCT 3; Carl Zeiss Meditech Inc, Dublin, CA). Lens tilt was defined as decentration along the horizontal or vertical meridian, while lens dislocation was defined as physical displacement of IOL into the vitreous cavity/posterior pole.
The primary outcome indicator of the study was post-operative visual acuity, particularly BCVA. Secondary outcomes included changes in post-operative MRx, mean absolute refractive error, IOP, number of glaucoma medications, change in ECD, and post-operative complications.
Statistical analysis
The mixed model was used to compare the pre-operative with post-operative measurements at each time point by taking account of the partial paired data. Snellen visual acuity was transformed to logMAR equivalents to facilitate statistical analysis. Visual acuity of hand motion was set at 2.3 logMAR, whereas counting fingers was set at 1.85 logMAR [17, 18]. Eyes aimed for near were excluded from the analysis of post-operative UDVA, MRx, and spherical equivalent (SE). A p value < 0.05 was considered statistically significant. All analyses were performed by using software SAS 9.4 (SAS Institute Inc., Cary, NC).
Results
One hundred and seventeen eyes underwent iris fixation of PC IOL, with a mean follow-up of 22.4 ± 18.9 months (range: 3–84 months). The mean age at time of surgery was 67.5 ± 16.9 years (range: 13–91 years) (Table 1). One hundred and thirteen cases (96.6%) had prior cataract extraction (CE). Of those, the average time from CE to iris suture fixation was 7.9 ± 9.3 years (range: 2 weeks–37 years). Most patients (86.3%) presented with a concomitant ophthalmic condition, the most common of which were glaucoma (21.4%), ERM (16.2%), and uveitis-glaucoma-hyphema (UGH) (12.8%) (Table 1). Among those with glaucoma, 56% had previous glaucoma surgeries. About 69% of the total population had history of previous non-cataract surgical procedures, the most common of which were pars plana vitrectomy (PPV) (31.6%) and trabeculectomy (10.3%). Overall 5.2% had a history of previous IOL repositioning (Table 1).
The most common risk factors for post-operative IOL displacement (i.e., occurring after the initial cataract surgery) were: high myopia (25.5%), pseudoexfoliation (PEX) syndrome (17.7%), and ocular trauma (14.4%) (Table 2). Several indications for the current surgery (iris fixation) were encountered: IOL subluxation (34.2%), IOL dislocation (30.7%), aphakia (23.1%), and other less frequent indications (Table 2). Combined PPV procedure was performed in 41.0% of eyes.
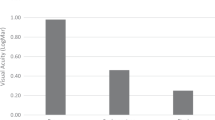
There was a noticeable improvement in post-operative UCVA compared with baseline. This improvement was statistically significant from POW1 and was observable throughout the subsequent follow-up period (Fig. 1). Number of eyes with UCVA of 20/40 or better was found to be higher at POM1 (17.2%) and POM3 (26.7%) than at baseline (14.0%) (p = 0.60 and p = 0.09, respectively). The mean post-operative BCVA was statistically better at each follow-up visit compared with baseline (Table 3). It was relatively stable through the follow-up (Fig. 2). A greater number of eyes demonstrated a BCVA of 20/40 or better at POM1 (49.5%) and POM3 (50.0%) than preoperatively (36.5%) (p = 0.06 and p = 0.05, respectively).
Changes in MRx are presented in Table 3. The mean absolute refractive prediction error was not significantly different during the follow-up period from that observed at POM1 (Table 3). For cases aimed for emmetropia or near emmetropia, myopic outcome in the average SE was observed postoperatively (Table 3).
Mean post-operative IOP was lower than pre-operative during the follow-up period (Table 3). Number of glaucoma drops was also lower postoperatively compared with baseline (Table 3). IOP spike was observed in seven cases (Table 2), one had a history of glaucoma. Two cases of new-onset glaucoma developed by the end of the follow-up period. These cases were medically managed.
Sixteen cases (13.7%) had recurrent IOL subluxation (Table 2), fourteen of which had either concomitant (seven eyes) or prior (seven eyes) PPV. The mean interval for post-operative re-subluxation was 5.3 ± 8.3 (range: 1 day–33 months) months. Without PPV cases, the re-subluxation rate was 2/45 (4.4%) cases.
Four eyes developed ERM postoperatively (Table 2). Of those, three eyes underwent a combined PPV with iris-sutured IOL procedure and one eye had a history of PPV with SB procedure. The mean interval for post-operative ERM formation was 3.8 ± 2.6 (range: 1–6) months. Five cases of CME were diagnosed postoperatively (Table 2); four received a combined PPV with iris-sutured IOL procedure. The mean interval for post-operative CME formation was 5.5 ± 2.7 (range: 1.5–9) months. It should be mentioned that due to pre-operative poor fundus visibility in some cases, the presence of CME and ERM may not have been assessed properly. If eyes with combined PPV surgery or a history of previous PPV were excluded, rate of ERM would be 0/45 (0%) and rate of CME would be 1/45 (2.2%).
Six eyes developed misshapen pupil. Five new cases of pseudophakic bullous keratopathy (PBK) were documented postoperatively (Table 2). For eyes with available data on central corneal ECD (n = 18 eyes), the mean ECD decreased from 1976 to 1788 cells/mm2 at post-operative month 3 (P = 0.065). Fuchs’ corneal dystrophy was diagnosed in three eyes before surgery, but none of these eyes decompensated during the follow-up period. Some haemorrhagic complications were noticed postoperatively: hyphema in three eyes (needed AC wash out in one eye) and vitreous haemorrhage in two eyes (necessitating PPV with AC wash out). A post-operative choroidal detachment occurred in one eye (Table 2). None of the studied eyes developed RD, pigment dispersion syndrome, or post-operative uveitis.
Sterile endophthalmitis was suspected in one eye 3 months after surgery. This eye had a combined PPV procedure due to retained lens fragment and a pre-operative BCVA of 20/60. This patient had a history of retinal surgeries and chronic CME. AC fluid was tapped and sent for cultures followed by intravitreal vancomycin and ceftazidime injection. Fortified antibiotics (hourly tobramycin and vancomycin) were prescribed. Gram stain showed no evidence of organisms, and cultures were negative for bacteria and fungi. On the last follow-up visit (9 months after surgery) BCVA was 20/70 in that eye. No eye was blinded in the study.
Discussion
The rate of PC IOL dislocation after a primary cataract surgery has been reported to be around 0.2–3% [2,3,4]. A large retrospective, population-based cohort study identified a cumulative risk of IOL dislocation following CE of 0.1% after 10 years, 0.2% after 15 years, 0.7% after 20 years, and 1.7% after 25 years [19]. Early cases of spontaneous IOL dislocation (<3 months) are generally a result of tearing of the posterior capsule and/or rupture of the equatorial zonules, whereas late in-the-bag dislocation is related to progressive zonular insufficiency and/or capsular bag contraction [20]. In PEX cases, for example, the mean interval between cataract surgery and IOL dislocation is usually 5.5–8.5 years [19, 21,22,23,24], but some cases could present as late as 18 years after surgery [25].
Once dislocation occurs, or the capsular support is lost or deemed inadequate, there are different approaches by which IOLs can be fixed in place. Iris fixation can be more technically demanding than scleral fixation and AC IOL placement. However, it can offer less suture-related complications in comparison with scleral-sutured IOLs [26]. Moreover, iris fixation facilitates placement of the IOL closer to the physiological anatomic position. Another advantage of the iris fixation technique is sparing of the conjunctiva, which can be advantageous in case of future glaucoma or retina surgeries.
Intrascleral haptic fixation technique has been increasing in popularity. There are many modifications of this technique [8,9,10,11]. Scleral IOL fixation using Gore-tex suture was shown to have a significant improvement in visual acuity without suture-related complications. However, a number of other non-suture-related complications, including hypotony, ocular hypertension, haemorrhagic complications, and CME formation, were observed [8]. Two other techniques should be mentioned: scleral-glued IOL technique described by Agarwal et al. [10] and IOL flange technique described by Yamane et al. [11]. One year follow-up of the scleral-glued IOL technique showed promising functional results with risk of 5.6% of IOL decentration, 3.7% of pigment dispersion, and 7.5% of CME [27]. Flange IOL study had a 36 months follow-up and reported good functional results with risk of 8% iris capture and 5% vitreous haemorrhage [11].
To our knowledge, there is only one randomised trial comparing three IOL fixation techniques (AC IOL, scleral-sutured IOL, and iris-sutured IOL) in eyes lacking capsular support [28]. All procedures were conducted with concomitant PKP in 176 patients. Visual outcomes were similar in all three groups, but iris-sutured PC IOLs were associated with significantly less frequent CME (20%) compared with AC IOLs (38%) and scleral-sutured IOLs (41%). The group with scleral fixation of PC IOLs had the highest number of complications. In a recent metanalyses comparing paired studies of transscleral-fixated, intrascleral-fixated, and iris-fixated IOLs, intrascleral fixation was found to have a lower risk of CME compared with transscleral fixation [5]. Also, lower risk of intraocular haemorrhage and glaucoma escalation was observed in iris fixation than in either of the other fixation techniques. However, iris fixation was associated with a higher risk of ECL compared with transscleral fixation.
Regarding visual outcomes, the aforementioned metanalyses did not find a significant difference in post-operative BCVA in any pair of comparisons [5]. Also, no significant difference was observed in the number of eyes achieved BCVA 20/40 or better at the final visit. We observed improvement in UCVA postoperatively compared with baseline. This improvement was statistically significant from POW1 and remained as such throughout the follow-up period. The mean post-operative BCVA was significantly better at each follow-up visit compared with baseline. Overall 49.5% of eyes achieved a BCVA of 20/40 or better postoperatively. Similar results were observed by other investigators [15, 16, 29]. It should be noted that our cohort consisted of a high number of complicated eyes with multiple previous posterior-segment surgeries, thus possibly limiting the patients’ visual potential.
A decrease of almost 200 cells/mm2 in corneal ECD was observed at POM3 after iris-sutured IOL procedure. At 6 months postoperatively, Yamane et al. reported decrease in ECD from 2341 cells/mm2 to 2313 cells/mm2 (p < 0.01) [11]. Similar results were reported by Agarwal et al. (5.2% ECL) at one year postoperatively [27]. Kim et al., did not observe a statistically significant difference in the ECL in iris fixation group (12.7% ± 8.7%) vs transscleral fixation group (10.9% ± 9.2%) [30].
Post-operative glaucoma can develop in eyes undergoing iris fixation procedure [15, 29]. In our cohort, two cases of new-onset glaucoma developed by the end of the follow-up period. Overall, post-operative IOP values were minimally lower than pre-operative values. Also, a decrease in number of glaucoma drops was noted.
The rate of recurrent subluxation after iris suture fixation procedure can range from 0 to 13% [15, 30]. In the current study, recurrent subluxations occurred in 13.7% of eyes postoperatively. The most common risk factor for re-subluxation in our cohort was concurrent or previous PPV (14/16 cases). If combined PPV cases and cases with a history of PPV were excluded, the re-subluxation rate would be 2/45 (4.4%). Our findings support the recent observation made by Vounotrypidis et al. that vitrectomy is a major underreported risk factor for IOL re-subluxation [31]. All eyes in our study were surgically managed.
Four eyes developed ERM postoperatively with a mean interval for ERM formation of 3.8 ± 2.6 (range: 1–6 months) months. Of those, three eyes had undergone a combined PPV with iris-sutured IOL procedure and one eye had a history of PPV with SB procedure. It is unclear whether the ERM formation was due to the iris suture procedure, the other risk factors, or a combination of all. The rate of ERM formation may be as high as 35.1% after PPV alone [32]. All cases were surgically managed during the follow-up period.
The rate of CME after uncomplicated phacoemulsification is 0.1–2.35% [33] and 15.8% after complicated surgery [34]. PPV alone may result in 15.2% of post-operative CME [32]. In our study, CME developed in five eyes postoperatively with a mean interval for CME development of 5.5 ± 2.7 (range: 1.5–9 months) months. Of note, all cases had other risk factors for the development of CME (four eyes had a combined PPV procedure and one eye had a complicated primary cataract surgery). In our study, all cases of post-operative CME were successfully managed with steroidal and nonsteroidal anti-inflammatory drops.
One concern after iris suture fixation of a PC IOL is iris chafing and development of pigment dispersion syndrome. A number of studies have reported that progressive pigment dispersion glaucoma has not been identified as a common late complication with this form of fixation [16, 28]. In our study, no new-onset cases of pigment dispersion or chronic uveitis were observed. The MA50BM hydrophobic acrylic IOL was used in all cases and has a posterior angulation of 10°. We surmise that this angulation could decrease the risk of iris chafing.
Limitations of this study include its retrospective design. This led to the absence of some data, as it was not recorded in every patient’s chart. Chart review also resulted in relatively small n values for some study characteristics, such as ECD. These limitations were unavoidable. However, this study is distinct from prior publications in its inclusion of high-complexity cases, long follow-up period and minimum follow-up inclusion of 3 months.
Our data demonstrate that the iris-sutured PC IOL procedure can be a beneficial treatment option for eyes with inadequate capsular support and complex ocular history. It may lead to improved vision, long-term stability, and safety. In eyes with previous or combined PPV, the outcome of iris-sutured IOL procedure was not as good as in eyes that did not undergo PPV. Complications from surgery may occur up to 9 months postoperatively. Longer minimum follow-up period is recommended for future studies of secondary IOL outcomes to capture complications of such procedures.
Summary
What was known before
-
There are different techniques for IOL fixation in eyes lacking adequate capsular support. Among them are scleral fixation (sutured IOL fixation, glued, or intrascleral haptic fixation), iris fixation (sutured or claw), or anterior chamber IOL placement.
What this study adds
-
Iris suture IOL fixation can lead to improved vision, long-term stability, and safety in eyes with inadequate capsular support and complex ocular history.
-
Complications from surgery may occur up to 9 months postoperatively. Longer minimum follow-up period is recommended for future studies to capture complications of such procedures.
-
Eyes with previous or combined PPV do not do as well as eyes that do not undergo PPV.
References
Price FW Jr, Whitson WE. Visual results of suture-fixated posterior chamber lenses during penetrating keratoplasty. Ophthalmology. 1989;96:123–40. S0161-6420(89)32760-6.
Stark WJ, Worthen DM, Holladay JT, Bath PE, Jacobs ME, Murray GC, et al. The FDA report on intraocular lenses. Aust J Ophthalmol. 1984;12:61–9.
Stark WJ Jr, Maumenee AE, Datiles M, Fagadau W, Baker CC, Worthen D, et al. Intraocular lenses: complications and visual results. Trans Am Ophthalmol Soc. 1983;81:280–309.
Kratz RP, Mazzocco TR, Davidson B, Colvard DM. The shearing intraocular lens: a report of 1000 cases. J Am Intraocul Implant Soc. 1981;7:55–7.
Li X, Ni S, Li S, Zheng Q, Wu J, Liang G, et al. Comparison of three intraocular lens implantation procedures for aphakic eyes with insufficient capsular support: a network meta-analysis. Am J Ophthalmol. 2018;192:10–19. S0002-9394(18)30204-6.
Lyle WA, Jin JC. Secondary intraocular lens implantation: anterior chamber vs posterior chamber lenses. Ophthalmic Surg 1993;24:375–81.
Hennig A, Evans JR, Pradhan D, Johnson GJ, Pokhrel RP, Gregson RM, et al. Randomised controlled trial of anterior-chamber intraocular lenses. Lancet 1997;349:1129–33. S0140673696110436.
Khan MA, Gupta OP, Smith RG, Ayres BD, Raber IM, Bailey RS, et al. Scleral fixation of intraocular lenses using gore-tex suture: clinical outcomes and safety profile. Br J Ophthalmol. 2016;100:638–43. https://doi.org/10.1136/bjophthalmol-2015-306839.
Hannush SB. Sutured posterior chamber intraocular lenses: indications and procedure. Curr Opin Ophthalmol. 2000;11:233–40.
Agarwal A, Kumar DA, Jacob S, Baid C, Agarwal A, Srinivasan S. Fibrin glue-assisted sutureless posterior chamber intraocular lens implantation in eyes with deficient posterior capsules. J Cataract Refract Surg. 2008;34:1433–8. https://doi.org/10.1016/j.jcrs.2008.04.040.
Yamane S, Sato S, Maruyama-Inoue M, Kadonosono K. Flanged intrascleral intraocular lens fixation with double-needle technique. Ophthalmology 2017;124:1136–42. S0161-6420(16)32178-9.
Michaeli A, Soiberman U, Loewenstein A. Outcome of iris fixation of subluxated intraocular lenses. Graefes Arch Clin Exp Ophthalmol. 2012;250:1327–32. https://doi.org/10.1007/s00417-012-2057-x.
Chu MW, Font RL, Koch DD. Visual results and complications following posterior iris-fixated posterior chamber lenses at penetrating keratoplasty. Ophthalmic Surg 1992;23:608–13.
Por YM, Lavin MJ. Techniques of intraocular lens suspension in the absence of capsular/zonular support. Surv Ophthalmol 2005;50:429–62. S0039-6257(05)00084-6.
Soiberman U, Pan Q, Daoud Y, Murakami P, Stark WJ. Iris suture fixation of subluxated intraocular lenses. Am J Ophthalmol. 2015;159:353–9. https://doi.org/10.1016/j.ajo.2014.11.009.
Stutzman RD, Stark WJ. Surgical technique for suture fixation of an acrylic intraocular lens in the absence of capsule support. J Cataract Refract Surg. 2003;29:1658–62. S0886335003000543
Holladay JT. Proper method for calculating average visual acuity. J Refract Surg. 1997;13:388–91.
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M. Visual acuities “hand motion” and “counting fingers” can be quantified with the freiburg visual acuity test. Investig Ophthalmol Vis Sci. 2006;47:1236–40. doi: 47/3/1236
Pueringer SL, Hodge DO, Erie JC. Risk of late intraocular lens dislocation after cataract surgery, 1980-2009: a population-based study. Am J Ophthalmol. 2011;152:618–23. https://doi.org/10.1016/j.ajo.2011.03.009.
Ascaso FJ, Huerva V, Grzybowski A. Epidemiology, etiology, and prevention of late IOL-capsular bag complex dislocation: review of the literature. J Ophthalmol. 2015;2015:805706. https://doi.org/10.1155/2015/805706.
Krepste L, Kuzmiene L, Miliauskas A, Januleviciene I. Possible predisposing factors for late intraocular lens dislocation after routine cataract surgery. Medicina. 2013;49:229–34. doi: 1305-05e.
Hayashi K, Hirata A, Hayashi H. Possible predisposing factors for in-the-bag and out-of-the-bag intraocular lens dislocation and outcomes of intraocular lens exchange surgery. Ophthalmology. 2007;114:969–75. S0161-6420(06)01317-0.
Ostern AE, Sandvik GF, Drolsum L. Late in-the-bag intraocular lens dislocation in eyes with pseudoexfoliation syndrome. Acta Ophthalmol. 2014;92:184–91. https://doi.org/10.1111/aos.12024.
Jones JJ, Jones YJ, Jin GJ. Indications and outcomes of intraocular lens exchange during a recent 5-year period. Am J Ophthalmol. 2014;157:15–162.e1. https://doi.org/10.1016/j.ajo.2013.08.019.
Jakobsson G, Zetterberg M, Lundstrom M, Stenevi U, Grenmark R, Sundelin K. Late dislocation of in-the-bag and out-of-the bag intraocular lenses: ocular and surgical characteristics and time to lens repositioning. J Cataract Refract Surg. 2010;36:1637–44. https://doi.org/10.1016/j.jcrs.2010.04.042.
Vote BJ, Tranos P, Bunce C, Charteris DG, Da Cruz L. Long-term outcome of combined pars plana vitrectomy and scleral fixated sutured posterior chamber intraocular lens implantation. Am J Ophthalmol. 2006;141:308–12. S0002-9394(05)01020-2.
Kumar DA, Agarwal A, Prakash G, Jacob S, Saravanan Y, Agarwal A. Glued posterior chamber IOL in eyes with deficient capsular support: a retrospective analysis of 1-year post-operative outcomes. Eye. 2010;24:1143–8. https://doi.org/10.1038/eye.2010.10.
Schein OD, Kenyon KR, Steinert RF, Verdier DD, Waring GO 3rd, Stamler JF, et al. A randomized trial of intraocular lens fixation techniques with penetrating keratoplasty. Ophthalmology. 1993;100:1437–43. S0161-6420(93)31458-2.
Condon GP, Masket S, Kranemann C, Crandall AS, Ahmed II. Small-incision iris fixation of foldable intraocular lenses in the absence of capsule support. Ophthalmology.2007;114:1311–8.S0161-6420(07)00438-1.
Kim KH, Kim WS. Comparison of clinical outcomes of iris fixation and scleral fixation as treatment for intraocular lens dislocation. Am J Ophthalmol. 2015;160:46–469.e1. https://doi.org/10.1016/j.ajo.2015.06.010.
Vounotrypidis E, Schuster I, Mackert MJ, Kook D, Priglinger S, Wolf A. Secondary intraocular lens implantation: a large retrospective analysis. Graefes Arch Clin Exp Ophthalmol. 2019;257:125–34. https://doi.org/10.1007/s00417-018-4178-3.
Banker TP, Reilly GS, Jalaj S, Weichel ED. Epiretinal membrane and cystoid macular edema after retinal detachment repair with small-gauge pars plana vitrectomy. Eur J Ophthalmol. 2015;25:565–70. https://doi.org/10.5301/ejo.5000609.
Wetzig PC, Thatcher DB, Christiansen JM. The intracapsular versus the extracapsular cataract technique in relationship to retinal problems. Trans Am Ophthalmol Soc. 1979;77:339–47.
Moisseiev E, Kinori M, Glovinsky Y, Loewenstein A, Moisseiev J, Barak A. Retained lens fragments: nucleus fragments are associated with worse prognosis than cortex or epinucleus fragments. Eur J Ophthalmol. 2011;21:741–7. https://doi.org/10.5301/EJO.2011.6483.
Funding
Unrestricted research grants from the Michael O’Bannon foundation and the Turner family.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dzhaber, D., Mustafa, O.M., Tian, J. et al. Outcomes and complications of iris-fixated intraocular lenses in cases with inadequate capsular support and complex ophthalmic history. Eye 34, 1875–1882 (2020). https://doi.org/10.1038/s41433-019-0759-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-019-0759-6
This article is cited by
-
Preferred surgical techniques for secondary intraocular lens implantation in adults with aphakia
International Ophthalmology (2023)