Abstract
Purpose
To investigate the clinical features, prognostic outcomes of patients with orbital and ocular adnexal lymphoma (OALs) in Taiwanese cohort.
Methods
Total 112 patients with OALs were retrospectively reviewed. Demographic information such as age, gender, lymphoma subtype, tumor location and treatment modalities were recorded. The primary endpoints were disease-specific survival (DSS), and progression-free survival (PFS).
Results
The mean patient age was 59.0 ± 15.5 years (range, 23–92 years). The major histopathologic subtypes were mucosa-associated lymphoid tissue (MALT) lymphoma in 76 patients (67.9%), followed by diffuse large B-cell lymphoma (DLBCL) (9.8%), follicular cell lymphoma (FL) (8.0%), and small lymphocytic lymphoma (SLL) (5.4%). The anatomical locations for OALs were the orbit (44 patients, 39.3%), the conjunctiva (31 patients, 27.7%), the lacrimal gland (28 patients, 25.0%), and the eyelid (8 patients, 7.1%). With a mean follow-up time of 74.5 ± 59.8 months (range 6–342 months), the DSS for all patients were 93.1%, 87.7%, and 68.8% at 60, 120, and 180 months’ follow-up, respectively. The PFS at 60, 120, and 180 months’ follow-up were 86.2%, 61.2%, and 44.6%, respectively. Regarding the analysis of prognostic factors, patients with high grade lymphoma subtype and advanced stage exhibited a worse prognosis.
Conclusions
MALT type lymphoma constitutes most of OALs in Taiwan and occurs more frequently than in Western countries. Patients with MALT lymphoma, FL, SLL and earlier stage have favorable outcomes compared with patients of high grade lymphoma and Ann Arbor stage IV lymphoma.
Similar content being viewed by others
Introduction
Lymphoma is a diverse group of malignancy with different histopathological subtypes and clinical presentations that vary with geographic locations. The age-standardized incidence rate reveals lower incidence of non-Hodgkin lymphoma (NHL) in East Asia than in Western countries [1]. Among NHL subtypes, diffuse large B cell lymphoma (DLBCL) constitutes the majority in both Western and Eastern countries [2]. For mucosa-associated lymphoid tissue type (MALT), one of the indolent B-cell lymphoma, the incidence has been reported to be higher in Chinese population than North America and Europe that might be associated with genetic or environmental factors [2].
OALs can arise in the conjunctiva, eyelids, orbit as well as the lacrimal gland. OAL may be a primary process, arising within ocular adnexal structures, but it may also occur from primary lesions in the other organs with secondary involvement.
Compared with other sites in the body, ocular adnexal involvement is relatively rare, accounting for approximately 8% of all extranodal lymphomas [3]. The overall incidence of lymphoma has been increasing annually by 3% to 4% for decades [4], however, the rate of extranodal disease has been increasing at a greater rate, especially in the elderly, perhaps because of the longer life expectancy of the general population [3]. Within the extranodal subgroup, OALs has shown the greatest increase in incidence at a rate of up to 6.3% per year [5]. Similarly, some geographic variation in the distribution of periocular lymphoma may exist. Among all the OALs, the incidence of MALT lymphoma varies from 50% to 70% in Western populations and even higher from 80% to 90% in Asians [6, 7].
Currently, there are very few large cohort studies reported on OALs in Chinese population. Hence, the aim of the study was to evaluate the clinicopathological features of orbital and ocular adnexa lymphoma and their effect on survival, staging, its treatment options, and prognostic outcome in a cohort of Taiwanese patients.
Methods
Study design
This study was approved by the Ethical Review Committee of the National Taiwan University Hospital, Taiwan (Institutional Review Board reviewing number 201910130RINA). All procedures adhered to the tenets of the Declaration of Helsinki for research involving human subjects. This study was a retrospective observational case series based on data from single largest eye center treated by two ophthalmologists (S-LL and Y-HW) in Taiwan.
We conducted a retrospective chart review of patients with orbital and ocular adnexal lymphoma (including lacrimal gland, extraocular muscle, connective tissue/orbital fat) who were diagnosed in the National Taiwan University Hospital between January 1, 1985, and December 31, 2019. Diagnoses of periocular lymphoma were based on the results of histopathologic examinations using immunohistochemical analysis via surgical biopsy. Patients with follow-up period of less than 6 months were excluded from this study unless they had died.
We classified histopathologic data that could not be defined by current systems as “other” in our study. For others that corresponded to REAL or WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues, the diagnosis of OALs subtype was definitive [8].
Clinical data
All the patients were categorized according to the classifications established by the World Health Organization. Data collected included patient age, sex, initial symptoms and signs, sites of involvement, operation method, pathological results, prognosis, follow-up duration, the state of concurrent bacterial or virus infection. In this study, all the patients were classified into either extranodal marginal zone B-cell lymphoma (EMZL) or non-EMZL group (including DLBCL, follicular lymphoma (FL), and others) for analysis of the demographic data, treatment modalities, treatment outcome and prognosis.
Staging workups were performed after the consultation with the hemato-oncology department. Staging was based on the Ann Arbor classification [9]. Since the study spanning 35 years, not all clinical parameters were available in all patients.
Involvement of lymph nodes, bone marrow, or other extranodal sites was determined with diagnostic tools available at the time of diagnosis and clinical data. Complete diagnostic evaluation includes full-body positron emission tomography (PET)–computed tomography (CT), CT, or magnetic resonance imaging (MRI) of the orbital and ocular adnexa and bone marrow biopsy.
Statistical analysis
Disease-specific survival (DSS) was defined as the interval between the date of diagnosis of lymphoma and the date of the date of last follow-up, or death by lymphoma. Progression-free survival (PFS) was defined as the time from diagnosis to disease recurrence after initial treatment, the date of death by any cause, or the date of last contact. Survival curves were estimated using the Kaplan–Meier method, and the level of significance among different outcomes was evaluated via log rank test. Univariate analysis and multivariate analysis were performed to identify prognostic factors for DSS.
Risk factors were compared using the χ2 test. P < 0.05 was considered statistically significant. Statistical analysis and calculation were made using SPSS software version 22.0 (SPSS Inc., Chicago, IL).
Results
Demographics and clinical features
Among the one hundred and twelve patients identified in our study, only three (2.7%) were T cell origin, and the majority OALs were B-cell lymphoma (n = 109, 97.3%). The average age at presentation was 59.0 ± 15.5 years (range, 23–92 years; median, 60.5 years), including 59 males (52.7%) and 53 females (47.3%). Seventy-six patients (67.9%) were identified in EMZL group, and the other thirty-six patients (32.1%) were classified into non-EMZL group.
There was no age or gender preference between EMZL or non-EMZL patients (p = 0.157 and p = 0.851, respectively). Bilateral involvements were observed in 21 patients (18.7%). Significantly more patients with EMZL had bilateral involvement (n = 19, 25.0%), compared to non-EMZL patients (n = 2, 5.6%) (p = 0.028). Orbit were the most common primary location for lymphoma involvement (n = 44, 39.6%), followed by conjunctiva (n = 31, 27.9%), lacrimal glands (n = 28, 25.2%) and eyelids (n = 8, 7.2%). Staging workup was able to be conducted on 92 patients, including 65 EMZL patients and 27 non-EMZL patients. More than half of patients (n = 49, 53.3%) had Ann-Arbor stage IE disease and 19 patients (20.7%) were stage IVE at the time of diagnosis. No significance was found among the bone marrow (BM) or non-bone marrow metastasis between EMZL and non-EMZL patients (p = 0.226). Most EMZL (n = 62, 95.4%) and non-EMZL patients (n = 23, 85.2%) were primary OALs, only 7 patients (7.6%) were systemic lymphoma with secondary orbital or ocular adnexa involvement or as a local invasion from adjacent periorbital structures. The data of hepatitis B virus (HBV) and hepatitis C virus (HCV) infection was able to be recorded in 112 and 97 patients, with 19 (17.0%) and 6 (6.2%) patients had chronic HBV and HCV infection, respectively. Chronic antigenic stimulation of hepatitis B affected significantly more EMZL patients than non-EMZL patients (n = 18, 23.7% vs n = 1, 2.8%; p = 0.013) (Table 1).
The histopathologic results according to the World Health Organization classification revealed 76 patients (67.9%) with EMZL, 11 (9.8%) with DLBCL, 9 (8.0%) with FL, 6 (5.4%) with small lymphocytic lymphoma (SLL), 4 (3.6%) with mantle cell lymphoma (MCL) and others. Eyelids were the least presented anatomical location among different subtypes of OALs, except for DLBCL (n = 2, 18.2%) (Table 2). Various clinical symptoms and sings were frequently encountered, and many patients had several different complaints. Palpable mass (n = 52, 46.4%) was the most reported symptoms, others varied among anatomical locations, including proptosis of orbits (n = 9, 20.5%), periorbital swelling of lacrimal gland (n = 4, 14.3%) and eyelid (n = 2, 25.0%), chemosis of conjunctiva (n = 3, 9.7%). Accidentally finding without noticeable symptoms/signs was also found in 3 patients (2.7%). Only one patient (0.9%) presented with B symptoms.
Treatment modalities and outcome
Observation without any interventions after tumor excision (surgery only) was chosen only in 9 patients (n = 37, 24.3%) of stage IE EMZL due to old age and comorbidities. Doxycycline as monotherapy was prescribed in 5 patients (n = 37, 13.5%) of stage IE EMZL. A total of 30 patients (n = 92, 32.6%) were treated with local radiotherapy. Radiotherapy constituted the primarily sole treatment for 18 patients (n = 92, 19.6%) and was combined with chemotherapy or chemotherapy with Rituximab in 10 (n = 92, 10.9%) and 2 patients (n = 92, 2.2%) respectively. The dosage of radiotherapy ranged from 20 to 40 Gy. Among the patients with advanced stage (Ann Arbor stage III and stage IV), chemotherapy regimen (cyclophosphamide, doxorubicine, vincristine, prednisone) was mostly conducted with immunomodulating agent rituximab (R-CHOP) as treatment strategy. A variety of combination regimens and single agent were used, including tetracycline ointment and proton pump inhibitor (Table 3).
Total 44 patients (n = 92, 47.8%) revealed complete remission (CR) at the last follow-up. Eleven patients (n = 92,12.0%) had partial response, and 18 patients (n = 92,19.6%) were shown to have stable disease. Only 8 patients (n = 92,8.7%) experienced refractory disease with recurrences. Lymphoma related death occurred in nine patients (n = 92,9.8%), and 2 EMZL patients (n = 92, 2.2%) were died due to advanced lung cancer. No significant differences (p = 0.285) of disease status at last follow-up between EMZL or non-EMZL subtypes were found (Table 4). Disease status was significantly associated (p < 0.01) with Ann Arbor stage. Complete remission was found in 36 patients (n = 60, 60.0%) of limited stage (Ann Arbor stage I or II) compared with 8 patients (n = 32, 25.0%) with advanced stage.
Prognostic factors
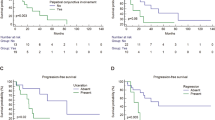
The mean follow-up time for all OALs was 74.5 ± 59.8 months (range 6–342 month). The disease specific survival (DSS) for all patients were 93.1%, 87.7%, and 68.8% at 60, 120, and 180 months, respectively (median survival, 288 months; 95% confidence interval [CI], 162–414 months). The Progression free survival (PFS) estimated by Kaplan–Meier analyses at 60, 120, and 180 months were 86.2%, 61.2%, and 44.6%, respectively (median survival, 142 months; 95% confidence interval [CI], 110–174 months) (Fig. 1a). The DSS was associated with the subtypes of OALs. (p = 0.002, log rank test). Low-grade subtypes including EMZL, FL and SLL had more favorable prognosis compared to high grade subtypes such as DLBCL and MCL (Fig. 1b).
a Disease-specific survival (DSS) and progression-free survival (PFS) analysis. The Kaplan–Meier survival curves for DSS and PFS for overall OALs patients. The median DSS was 288 months (95% confidence interval [CI], 162–414 months). The median PFS was 142 months (95% confidence interval [CI], 110–174 months). b Disease-specific survival (DSS) among patients with different subtypes of OALs. The Kaplan–Meier survival curves for DSS was significantly associated with different histopathological subtypes of OALs (p = 0.002). Low-grade subtypes like EMZL, FL and SLL had more favorable prognosis compared to DLBCL and MCL. DLBCL diffuse large B-cell lymphoma, EMZL extranodal marginal zone B-cell lymphoma, FL follicular lymphoma, MCL mantle cell lymphoma, Others: lymphoplasmacytic lymphoma, anaplastic large cell lymphoma; SLL small lymphocytic lymphoma.
Univariate analysis was performed by log rank test. Multivariate analysis was calculated by means of Cox proportional hazard model. Hazard ratio (HR) and 95% CI were both presented in each analysis. In univariate analysis and multivariate models for DSS, both high grade subtypes and higher Ann Arbor stage were identified to adversely affect the DSS. Eyelid involvement, bilateral OALs, and secondary disease with orbital and ocular adnexal involvement were poor prognostic factors but did not reach statistical significance in univariate analysis or multivariate model (Table 5).
Discussion
This retrospective study investigated the clinicopathological features of OALs in the ethnic Chinese population in Taiwan, as well as the prognostic factors for disease specific survival. Currently, our study is the largest published data of Chinese OALs patients. In our series, some results revealed different from previous reported observation in Western countries, South Korea or Japan. The various genetic factors or racial differences may affect the clinical presentations of OALs.
Our cohort exhibited slightly male predominance (male to female ratio 1.11) in overall OALs that was comparable with previous research [10, 11]. The incidence of non-Hodgkin lymphoma increases steadily with advancing age without peaking [12]. Studies in Western countries reported that the median age was at 64 years [12], while the median age at disease presentation in our patients was 60 years, which is higher compared to other reports in Asian countries (median age about 45years) [7, 13]. OALs cohort in our study demonstrated relatively low proportion of bilateral involvement (18.7%), while EMZL subtype had significantly more bilateral involvement (25.0%, p = 0.028). Previous literature found bilateral disease had a significant association with the poor prognosis of lymphoma [14, 15]. However, the present study showed no statistical connection between bilateral disease and the survival outcome in univariate and multivariate analysis.
The primary histopathologic subtype in our study was EMZL (67.9%), followed by DLBCL (9.8%), FL (8.0%), and SLL (5.4%). Similar to previous Asian studies, the incidence of EMZL in our cohort was higher than those in Western research (52%) [12, 16]. Previous literature review had described the predominance of EMZL OALs among Asians/Pacific regions [15, 17], although the exact mechanism for racial variation was still incomplete understood. Chronic antigen stimulation had been postulated as a causative agent in the development of B-cell transformation and lympho-proliferation leading to OALs, such as pathogenic association between Helicobacter pylori and gastric mucosa-associated lymphoid tissue (MALT) lymphoma [18, 19], Chlamydia psittaci in ocular adnexal lymphoma [20], and HCV in non-Hodgkin’s B-cell lymphomas [21, 22]. Direct infection of the orbit by H. pylori had been suggested but seemed highly implausible. Extranodal marginal zone lymphoma of orbital and ocular adnexa had thus been associated with persistent inflammation [23]. In Taiwan, the prevalence rate of H. pylori was about 53.9% (95%CI 36.6%−71.2%) with increasing as aging, much higher than Western populations [24]. Recent studies reported different results in H. pylori involvement in OALs [24, 25] that support the geographically diverging influence. The higher prevalence of EMZL in our patients may be correlated with the H. pylori infection in Taiwan. Although coinfection of H. pylori and C. psittaci was mentioned in OALs EMZL patients in previous studies [20, 25], the prevalence of C. psittaci was extremely low in Taiwan. Hepatitis C virus infection was often mentioned to be associated with non-gastric MALT lymphoma [26]. The most frequent non-gastric sites were the skin (35%), salivary glands (25%), and orbit (15%) [27]. Ferreri et al. found that of 55 patients with MALT-type ocular adnexal lymphoma, 13% were seropositive for HCV and seropositive patients were significantly more likely to have disseminated disease and more aggressive tumor behavior [21]. However, the incidence of hepatitis C infection is only 6.2% in our cohort. The association of hepatitis B virus infection in EMZL had been studied much less intensively than HCV infection. Previous studies had demonstrated the chronic hepatitis B infected patients having a 2–3-fold higher risk to develop NHL than non-infected patients. Previous observations had suggested that the lymphoid system is an important reservoir of HBV and had induced chronic antigen stimulation [28]. In Taiwan, an HBV-endemic area, it had been estimated that 15–20% population were carrier of occult HBV infection. Seventeen percent patients in our cohort had chronic HBV infection, a significant number compare to other Western studies [29], which may attribute to the higher prevalence of EMZL. The genetic abnormalities such as relatively higher incidence of chromosome translocations in Chinese than Caucasian patients and the abnormal activation of innate and adaptive immunological processes may also account for the variation between Asian and Western populations [30, 31].
Similar to previously published studies [16, 32], the ocular adnexal lymphoma in our cohort primarily involved orbit, especially for EMZL subtype. Eyelid lymphomas had a more aggressive course than other anatomical locations, and conjunctival lymphomas had a better prognosis than orbital or eyelid disease [14, 33]. Eyelid lymphoma accounted for only 7.1% in our cohort and revealed a worse prognosis than those at other sites, although the univariate and multivariate analysis did not show that the site was a statistically significant adverse predictor of survival. Similar to all previous reports [12, 34], the majority of our patients at the time of presentation were Ann Arbor stage IE disease. However, 28.3% patients presented with more advanced stage (IIIE or IVE), and BM involvement was noted in 16 patients (17.8%), both higher than other Asian and Western countries [11, 13, 34]. There may be such results because our study was performed in the largest tertiary referral center in Taiwan and could be influenced by sampling errors. Besides, racial difference and the social customs of Taiwan population may be associated with the higher rate of advanced stage patients in our study.
Surgery only without following treatments was performed in 9 stage IE EMZL patients due to old age and comorbidity (e.g., advanced lung adenocarcinoma in 2 patients). Oral doxycycline was used as a first-line treatment option in 5 patients with stage IE EMZL and 3 with complete remission. However, C. psittaci had not been identified in our cohort, suggesting its infection may be associated with geographic variability [35]. Majority of the EMZL patients with limited stages were treated with local radiotherapy, with a total radiation dosage of 20–40 Gy delivered in smaller fractions with good local control and avoidance of radiation-related side effects. Chemotherapy with or without Rituximab were prescribed for advanced stage group. Among EMZL subgroup, 52.3% of patients showed complete remission, and 37.0% non-EMZL patients had achieved complete remission. Compare with previous studies [10, 15, 34], complete remission was lower in our cohort in both EMZL and non-EMZL patients. The differences in complete remission rates might be associated with the slightly higher percentage of patients with advanced stage EMZL and non-EMZL in our cohort in comparison with Western population [36, 37]. Although considered as an indolent disease in previous studies [15, 32], 27.4% EMZL patient had systemic involvement noted during follow-up period, which demonstrated the heterogeneity among different races.
The long-term DSS and PFS outcomes for overall OALs in Taiwan demonstrated a relative indolent nature. However, the differences existed between lymphoma subtypes. The 60, 120, and 240 months DSS among EMZL subtype (95.6%, 87.3%, 58.2%) had favorable prognosis compared to DLBCL subtype (60, and 120 months DSS of 80.8% and 30.2% respectively). A recent study showed that the median overall survival was 57 months for OALs in Western population [38]. The overall survival for EMZL and FL at 5 and 10 years was 61.7% and 50.5%, respectively. Aggressive lymphoma subtypes also significantly correlated with poor prognosis in their study. However, the median age was higher than our cohort (70 years vs 60.5 years), and 41.1% patients were eventually died, which is higher than our cohort (9.82%, 11/112). The differences of survival between this recent study and our cohort might relate to age and the higher mortality.
Various prognostic factors had been advocated to affect the clinical outcome of OALs including Ann Harbor stage, anatomical location, age, gender, laterality and histological subtype. In present study, high grade histological subtypes and the advanced clinical stage were the variables that significantly correlated with poor prognosis in univariate and multivariate analysis. Gender, age, site of involvement, laterality, primary or secondary disease did not have statistically significant correlations with survival outcome.
The present retrospective cross-sectional study has several limitations. First, a relatively small number of patients and different histological subtypes, which may limit the analysis of prognostic factors affecting the outcome. Second, we did not analyze each histological subtype separately owing to small proportion of other OAL groups. Third, patients enrolled in this study had spanning 35 years; hence, not all samples were analyzed in comparable with current diagnostic criteria. Histological subtypes that were classified identical according to the older classification systems may now be regarded as different subtypes. It was only possible to classify a tumor as either B- or T cell lymphoma when updating the old classification systems.
In summary, the present study demonstrated the clinical characteristics and the prognostic factors that correlated with survival outcomes of OALs in Taiwan. The majority OALs in Taiwan was MALT type, with orbits being the primary involvement. Relative younger ages, more advanced stage, and higher ratio of chronic hepatitis B infection were found in Taiwan patients compared with Western countries, which may due to the combination of extrinsic (environmental, including infectious) and intrinsic (genetic, immunologic) components. Further multicentre studies that include different geographic areas and various ethnic group would be needed for elucidating the discrepancy of international epidemiology.
Summary
What was known before
-
Orbital and ocular adnexal lymphoma is the most common orbital neoplasm with prognostic factors varies among different populations.
What this study adds
-
The clinical features and prognostic factors for orbital and ocular adnexal lymphoma in Chinese population.
-
The survival outcomes of different orbital and ocular adnexal lymphoma subtypes in Taiwan.
References
Huh J. Epidemiologic overview of malignant lymphoma. Korean J Hematol. 2012;47:92–104.
Ko BS, Chen LJ, Huang HH, Wen YC, Liao CY, Chen HM, et al. Subtype‐specific epidemiology of lymphoid malignancies in Taiwan compared to Japan and the United States, 2002‐2012. Cancer Med. 2018;7:5820–31.
Freeman C, Berg JW, Cutler SJ. Occurrence and prognosis of extranodal lymphomas. Cancer. 1972;29:252–60.
Clarke CA, Glaser SL. Changing incidence of non-Hodgkin lymphomas in the United States. Cancer. 2002;94:2015–23.
Moslehi R, Devesa SS, Schairer C, Fraumeni JF Jr. Rapidly increasing incidence of ocu-lar non-hodgkin lymphoma. J Natl Cancer Inst. 2006;98:936–9.
Jenkins C, Rose GE, Bunce C, Wright JE, Cree IA, Plowman N, et al. Histological features of ocular adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Br J Ophthalmol. 2000;84:907–13.
Lee JL, Kim MK, Lee KH, Hyun MS, Chung HS, Kim DS, et al. Extranodal marginal zone B-cell lymphomas of mucosa-associated lymphoid tissue-type of the orbit and ocular adnexa. Ann Hematol. 2005;84:13–8.
Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, et al. WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues. Lyon, France, International Agency for Research in Cancer (IARC); 4th, 2017.
Graue GF, Finger PT, Maher E, Rocca DD, Rocca RD, Lelli GJ Jr, et al. Ocular adnexal lymphoma staging and treatment: American Joint Committee on Cancer versus Ann Arbor. Eur J Ophthalmol. 2013;23:344–55.
Oh Dong-Eun, Kim Yoon-Duck. Lymphoproliferative diseases of the ocular adnexa in Korea. Arch Ophthalmol. 2007;125:1668–73.
Sjö LeneDissing. Ophthalmic lymphoma: epidemiology and pathogenesis. Acta Ophthalmol. 2009;87:1–20.
Olsen TG, Holm F, Mikkelsen LH, Rasmussen PK, Coupland SE, Esmaeli B, et al. Orbital lymphoma—an international multicenter retrospective study. Am J Ophthalmol. 2019;199:44–57.
Yu H, Du YX, Sun ZC, Fu XR, Tan N, Gong WF, et al. Clinical features and treatment outcomes of primary ocular adnexal mucosa-associated lymphoid tissue lymphoma: a single center retrospective analysis of 64 patients in China. Int J Ophthalmol. 2019;12:1731.
Jenkins C, Rose GE, Bunce C, Cree I, Norton A, Plowman PN, et al. Clinical features associated with survival of patients with lymphoma of the ocular adnexa. Eye. 2003;17:809–20.
Desai A, Joag MG, Lekakis L, Chapman JR, Vega F, Tibshirani R, et al. Long-term course of patients with primary ocular adnexal MALT lymphoma: a large single-institution cohort study. Blood. 2017;129:324–32.
Ohtsuka K, Hashimoto M, Suzuki Y. High incidence of orbital malignant lymphoma in Japanese patients. Am J Ophthalmol. 2004;138:881–2.
Moslehi Roxana F, Bruce C. and Maria J. Schymura. Descriptive epidemiology of ophthalmic and ocular adnexal non-Hodgkin’s lymphoma. Expert Rev Ophthalmol. 2011;6:175–80.
Chan CC, Smith JA, Shen D, Ursea R, LeHoang P, Grossniklaus HE. Helicobacter pylori (H. pylori) molecular signature in conjunctival mucosaassociated lymphoid tissue (MALT) lymphoma. Histopathol. 2004;19:1219–26.
Ferreri AJ, Ponzoni M, Viale E, Guidoboni M, Conciliis CD, Resti AG, et al. Association between Helicobacter pylori infection and MALT-type lymphoma of the ocular adnexa: clinical and therapeutic implications. Hematol Oncol. 2006;24:33–7.
Ferreri AJ, Guidoboni M, Ponzoni M, De Conciliis C, Dell’Oro S, Fleischhauer K, et al. Evidence for an association between Chlamydia psittaci and ocular adnexal lymphomas. J Natl Cancer Inst. 2004;96:586–94.
Ferreri AJ, Viale E, Guidoboni M, Resti AG, De Conciliis C, Politi L, et al. Clinical implications of hepatitis C virus infection in MALT-type lymphoma of the ocular adnexa. Ann Oncol. 2006;17:769–72.
Arnaud P, Escande MC, Lecuit M, Validire P, Levy C, Plancher C, et al. Hepatitis C virus infection and MALT-type ocular adnexal lymphoma. Ann Oncol. 2007;18:400–1.
Verdijk RM. Lymphoproliferative tumors of the ocular adnexa. Asia Pac J Ophthalmol. 2017;6:132e42.
Hooi JK, Lai WY, Ng WK, Suen MM, Underwood FE, Tanyingoh D, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153:420–9.
Lee SB, Yang JW, Kim CS. The association between conjunctival MALT lymphoma and Helicobacter pylori. Br J Ophthalmol. 2008;92:534–6.
Strianese D, Tranfa F, Finelli M, De Renzo A, Staibano S, Schiemer R, et al. Hepatitis C virus infection in ocular adnexal lymphomas. Arch Ophthal. 2010;128:1295–9.
Arcaini L, Burcheri S, Rossi A, Paulli M, Bruno R, Passamonti F, et al. Prevalence of HCV infection in nongastric marginal zone B-cell lymphoma of MALT. Ann Oncol. 2007;18:346–50.
Marcucci F, Spada E, Mele A, Caserta CA, Pulsoni A. The association of hepatitis B virus infection with B-cell non-Hodgkin lymphoma–a review. Am J Blood Res. 2012;2:18.
Chen MH, Hsiao LT, Chiou TJ, Liu JH, Gau JP, Teng HW, et al. High prevalence of occult hepatitis B virus infection in patients with B cell non-Hodgkin’s lymphoma. Ann Hematol. 2008;87:475–80.
Coupland SE. Molecular pathology of lymphoma. Eye. 2013;27:180–9.
Chuang SS, Lee C, Hamoudi RA, Liu H, Lee PS, Ye H, et al. High frequency of t (11; 18) in gastric mucosa-associated lymphoid tissue lymphomas in Taiwan, including one patient with high-grade transformation. Br J Haematol. 2003;120:97–100.
Tanimoto K, Kaneko A, Suzuki S, Sekiguchi N, Watanabe T, Kobayashi Y, et al. Primary ocular adnexal MALT lymphoma: a long-term follow-up study of 114 patients. Jpn J Clin Oncol. 2007;37:337–44.
Svendsen FH, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, et al. Lymphoma of the Eyelid–An International Multicenter Retrospective Study. Am J Ophthalmol. 2017;177:58–68.
Olsen TG, Heegaard S. Orbital lymphoma. Surv Ophthalmol. 2019;64:45–66.
Rosado MF, Byrne GE Jr, Ding F, Fields KA, Ruiz P, Dubovy SR, et al. Ocular adnexal lymphoma: a clinicopathologic study of a large cohort of patients with no evidence for an association with Chlamydia psittaci. Blood. 2006;107:467–72.
Kirkegaard MM, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF, et al. Conjunctival lymphoma—an international multicenter retrospective study. Jama Ophthalmol. 2016;134:406–14.
Svendsen FH, Rasmussen PK, Coupland SE, Esmaeli B, Finger PT, Graue GF. Lymphoma of the eyelid–an international multicenter retrospective study. Am J Ophthalmol. 2017;177:58–68.
Zschoche M, Zimpfer A, Scheef BO, Jünemann AM, Guthoff RF, Junghanss C. Histopathological features and Ann Arbor stage in periocular lymphoma. Vivo. 2020;34:1965–74.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Hsu, CR., Chen, YY., Yao, M. et al. Orbital and ocular adnexal lymphoma: a review of epidemiology and prognostic factors in Taiwan. Eye 35, 1946–1953 (2021). https://doi.org/10.1038/s41433-020-01198-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01198-y
This article is cited by
-
Comprehensive analysis of orbital lymphoma in a Turkish cohort: clinical characteristics, histological subtypes, treatment modalities, prognostic factors, and implications for management
Annals of Hematology (2024)
-
Proteotranscriptomics of ocular adnexal B-cell lymphoma reveals an oncogenic role of alternative splicing and identifies a diagnostic marker
Journal of Experimental & Clinical Cancer Research (2022)