Abstract
Purpose
To report the application of endoscopy in the management of ocular trauma, describe the clinical settings and the treatment outcomes.
Methods
Retrospective, consecutive, non-comparative case series at a tertiary eye care centre. Data recorded included aetiology of trauma, presenting vision, corneal condition at presentation, per-operative clinical findings during endoscopy, prognostication of the cases on table, final visual and anatomic outcome. Odds ratios for a favourable outcome were computed for various surgical indications.
Results
The study included 58 eyes of 58 patients. Males constituted 82% of all cases. Mean age at presentation was 35.55 ± 18.9 years, median 31.5 years. Commonest corneal condition causing opaque media was corneal oedema (44.8%) followed by corneal laceration in 25.8%, repaired corneal laceration in 13.7% and scarred cornea in 12%. Commonest indication for surgery was retinal detachment (36.2%) followed by vitreous haemorrhage (29.3%), retained foreign body (13.7%) and combined detachment with haemorrhage in 10.3%. Of the 58 eyes, 17 eyes were deemed inoperable on endoscopic examination and 11 eyes were deemed to have poor prognosis. Of the fair prognosis (n = 30), 60% had final vision of 20/400 (p = 0.0001) compared to 10% before surgery and 13.33% had final vision of 20/40 (p = 0.03) as compared to nil in the pre-operative period. Odds ratio for a favourable visual outcome was best for the indication of vitreous haemorrhage (OR = 9, p = 0.0006).
Conclusion
Endoscopy in ocular trauma with opaque media provides adequate visualisation and allows for prognostication. In cases deemed to have prognosis, suitable intervention leads to globe and vision salvage.
Similar content being viewed by others
Introduction
Ocular trauma is one of the major causes of visual loss worldwide, especially in the young population [1]. The rapidity with which the treatment is initiated often has a bearing on the final visual and anatomic outcome. Early post-trauma period unfortunately is often plagued with poor visibility in the posterior segment by causes such as repaired corneal tears and corneal oedema [2, 3]. Conventionally, such cases are operated either when the corneal visibility improves or are operated by alternate means of visualisation-like therapeutic keratoplasty or a temporary keratoprosthesis (TKP) [4,5,6]. TKPs can be associated with intraoperative complications and a prolonged surgery time, and would also require a corneal graft at the end of the surgery.
The first reported usage of the intraocular endoscope was to remove an intraocular foreign body in a case of trauma [7]. Over the years, though the usage of the ocular endoscope has increased, extensive literature on its application in cases with trauma is scarce. In the current communication, we report the application of endoscopy in the management of ocular trauma at our institute, describe the clinical settings and treatment outcomes and also discuss the on-table prognostication in such cases.
Methods
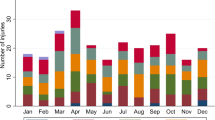
This was a retrospective, interventional, consecutive non-comparative case series. The study conformed to the tenets of the Declaration of Helsinki and was approved by the Institute Ethics committee. All case sheets of cases with trauma treated by intraocular endoscopic approach were retrieved from the institute’s medical record department register and the electronic medical record system. The study time period was from January 2014 till December 2019. These were cases that required a posterior segment intervention but where the cornea was too hazy to allow a conventional pars plana vitrectomy approach. Data points noted included demographics, aetiology of trauma, presenting vision, corneal condition at presentation, per-operative clinical findings during endoscopy, prognostication of the cases on table and final visual and anatomic outcome.
Surgery was performed using the 20/23G endoscope (E2 Laser and Endoscopy System; EndoOptiks, Inc, Little Silver, NJ, USA). The E2 Ophthalmic Laser Endoscopy System console combines endoscopic imaging and laser treatment capability. The console houses a high-resolution video camera, 175 or 300 W xenon light source and an 810-nm diode laser. The endoscope allows for a wide-field image providing a panoramic intraocular view of the entire retina or a close-up (down to 0.75 mm) and highly magnified view of pathology. The in-built video adaptor offers optimum zoom and manual focus of the endoscopic image.
Technique
The orientation of the optics of the endoscopic image on the monitor was ascertained initially by focusing on any object e.g., a conjunctival vessel and the orientation was checked on the screen to be upright. The endoscope probe (straight or curved) was then inserted in the eye through the pars plana by making a standard 20-gauge sclerotomy incision. Then, the intravitreal position of the tip of the irrigation cannula was verified before putting on the irrigation flow. A vitrectomy cutter was inserted through another sclerotomy site as in a conventional PPV approach. The vitreoretinal procedures were performed with the retina being viewed on the monitor in front of the surgeon instead of through the microscope.
Statistical analysis
The data were arranged on an excel spread sheet for statistical analysis. Relevant statistical analysis was done using MedCalc ver 12.2.1.0. (Ostend, Belgium). For statistical analysis, vision was converted from Snellen to logMAR equivalents. Mean and standard deviations were computed for all continuous variables. In case of non-parametric distribution, the median was calculated. Pre- and post-operative data were compared using the paired t test for parametric data and Wilcoxon rank sum test for non-parametric data. Odds ratios for favourable outcomes were computed for various surgical indications.
Results
The study included 58 eyes of 58 patients of the total 1405 cases of ocular trauma seen over this time period. Males accounted for 82% of the cases. Mean age at presentation was 35.55 ± 18.9 years, median 31.5 years. Commonest corneal condition causing opaque media was corneal oedema (44.8%) followed by corneal laceration (25.8%), repaired corneal laceration (13.7%) and scarred cornea (12%). The other causes for poor corneal visibility were corneal infiltrate and a keratoprosthesis in situ (1.85% each). Commonest indication for surgery was retinal detachment (36.2%) followed by vitreous haemorrhage (29.3%), retained foreign body (13.7%) and combined detachment with vitreous haemorrhage in 10.3%. As per the Birmingham Eye Trauma Terminology system, the types of injury noted were as shown in Table 1.
Based on the retinal evaluation per-operative, the cases were divided into those that were inoperable, those with poor visual prognosis and those with fair visual prognosis. Of the 58 eyes, 17 eyes were deemed inoperable on endoscopic examination due to the presence of a closed funnel retinal detachment and 11 eyes were deemed to have poor prognosis due to various observed retinal clinical findings (Fig. 1). The 11 eyes with poor prognosis included 5 eyes with optic atrophy, 3 with necrotic retina, 2 with advanced disc cupping and 1 with retinal ischaemia. Of those with a fair prognosis (n = 30), 60% achieved a final vision of 20/400 (p = 0.0001) compared to 10% before surgery and 13.33% had final vision of 20/40 (p = 0.03) as compared to 0 in the pre-operative period (Table 2). In the cases with a fair prognosis, 21 eyes underwent a spontaneous clearance of corneal oedema in the follow-up period. Nine eyes underwent a penetrating keratoplasty to achieve media clarity, and all grafts were clear till the last follow-up visit. Odds ratio for a favourable visual outcome and for globe salvage was calculated for the various indications for surgery. The odds were found to be the best for the indication of vitreous haemorrhage (OR = 9, p = 0.006 and OR = 10, p = 0.03 respectively) (Table 3). The total follow-up period was 11.33 ± 11.7 months (median 6 months).
The cases deemed to be of poor prognosis on table were revisited to understand the pre-operative condition of the posterior segment and the per-operative retinal condition. All those cases showed a closed funnel rhegmatogenous retinal detachment on table. Of the 17 cases, B-scan ultrasound picked up an equivocal retinal detachment in 2 cases pre-operatively. In all the other cases, the B scan was reported as having an attached retina. The commonest pre-operative B-scan finding was haemorrhagic choroidal detachment (n = 6) and attached retina with echogenic vitreous membranes (n = 6) (Table 4).
Discussion
In the current study we report the clinical settings and outcomes of management of cases with ocular trauma managed with ocular endoscopy. The study shows that of all such cases managed by endoscopy, an immediate prognostication was possible, which identified those with poor visual prognosis (Table 4). Among the rest, post surgery, there was a statistically significant improvement of vision. Analysing the indication for surgery, we concur that those who were operated for vitreous haemorrhage alone had significant odds of a better visual and anatomic outcome as compared to other indications. Cases where a poor visual prognosis was deemed on table, the pre-operative B scan had failed to pick up a closed funnel retinal detachment.
Al Sabti and Raizada reported their experience using endoscopy in ocular trauma in 50 eyes [1]. In their series, 37 eyes (74%) recorded an improvement of vision at the last follow-up, over a mean follow-up of 13.5 months. In comparison, in our study, 17 cases out of 58 were deemed inoperable on endoscopic evaluation. Of the remaining 41, 11 were deemed to have a poor prognosis on table itself at the conclusion of surgery. Of those where a fair prognosis was expected, 18/30 (60%) had vision improvement. This statistically was comparable to Sabti et al.’s results (p = 0.19).
Chun et al. [2] reported the anatomic and visual outcomes of eight eyes with open globe injury managed with vitrectomy utilising a TKP, and compared the results with nine others that were treated with endoscopic vitrectomy. They concluded that the endoscopy group had significantly shorter time to surgery (median 14 vs. 38 days; p = 0.034), and a shorter surgical time (median 2.9 vs. 8.4 h; p < 0.0005). Of the nine cases in their endoscopy group, four eyes (44%) achieved a vision of 20/200 or better at the last reported visit 6 months post surgery. This was also comparable to the outcome achieved in the current study (p = 0.4). As our study did not have a comparative arm of cases operated with a TKP, a similar comparison could not be made in our dataset.
Ayyildiz and Durukan reported the management of ocular trauma using a TKP vis-à-vis endoscopic visualisation [8]. In their series, eight eyes (57%) underwent TKP-assisted vitrectomy and six eyes (43%) underwent endoscopic vitrectomy. They concluded that though the post-operative functional and anatomical results were not significantly different between the two groups, median time from trauma to surgery and the median surgical time were significantly shorter in the endoscopy group. They also suggested a lesser complication rate in the endoscopy group.
In the absence of endoscopic visualisation, management of such cases greatly depends on pre-operative assessment with an ophthalmic B-scan ultrasound. Studies have shown B-scan ultrasound to have varying sensitivities and specificities in picking up retained foreign bodies or retinal detachments. Most studies attribute the sensitivity to vary from 70–85% [9, 10]. In our study, 17 cases had an inoperable retinal detachment, which was not picked up by B-scan ultrasound in the pre-operative evaluation. Endoscopy ensured immediate diagnosis on table and thus avoided unnecessary extensive procedure like a keratoprosthesis in these cases. In set ups where endoscopy or the know-how of a keratoprosthesis procedure is not available, such cases are treated conservatively. As such, there is no consensus regarding the timing of vitrectomy following ocular trauma, but several studies have reported better outcomes when surgery is performed within couple of weeks [11,12,13,14]. Endoscopic approach allows such an early intervention, which may ensure management before a retinal detachment develops or before a pre-existing retinal detachment develops end-stage proliferative vitreoretinopathy.
Prognostication of the final visual potential is a very important dimension of the management in ocular trauma. Currently different scales are available in ophthalmic literature for prognosticating the visual potential in cases of open globe injury [15,16,17,18]. The major limitation of all these prognostic scales was the fact that none of them accounted for the intraoperative evaluation for prognostication. Endoscopy, by allowing a direct visualisation of the intraocular structures, gives a better prognostication to the operating surgeon. This can assist appropriate patient counselling and keep the expectations regarding the post-operative outcomes realistic.
Like any other unconventional surgical methodology, endoscopic vitrectomy has a large learning curve. Head posture is quite different as compared to what the surgeon is used to usually as this requires a head posture towards display monitor. Often the head turn is exaggerated depending on the possible location of the camera monitor. Depth perception is nonexistent in endoscopic surgeries because of lack of stereopsis and a two-dimensional visualisation setup. As the light source and the camera are in the same axis, there is no shadowing. This eliminates the judgement of the instrument distance from the retina leading to high chances of possible tissue touch and retinal breaks especially for the uninitiated surgeon. The overall view is tunnel like, much different from the conventional panoramic view of the retina. Focusing the retina is not controlled on the table but has to be controlled by an assistant on the endoscope machine quite unlike the focusing of a binocular indirect ophthalmomicroscope lens. Rotation of the endoscope probe inadvertently causes rotation of the field of view, which can again lead to errors of judgement. Judgemental errors are more common in the peripheral retinal manoeuvring because easily identifiable landmarks like the foveal avascular zone and the optic disc are absent in the field of view. Thus, an imperative step is to ensure that the orientation is correct before surgical manoeuvring starts. In case of doubts, the probe can be retracted to allow for a greater field of vision and thus a better orientation. This may have to be repeated multiple times during surgery.
This study had its inherent limitations. Being retrospective in nature with a relatively small sample size, which finally was deemed to have any significant potential, was the biggest limitation. As this was a non-comparative series, no conclusion could be derived about the management outcomes vis-à-vis conservative approach or a surgical approach using a TKP. Trauma by itself is a major vision limiting factor. As the study was in a post-trauma subset, the bearing that trauma as a variable had on the final outcome could not be avoided. In conclusion, this study proposes a definite role of endoscopic approach in cases with post-segment trauma and an opaque anterior media. The advantages of endoscopy in such cases include a reliable prognostication, early intervention, preservation of resources by avoiding unnecessary extensive surgeries and a fair visual outcome in cases deemed to have prognosis. Going ahead, a prospective study comparing endoscopic approach versus a conservative approach or a surgical approach using a TKP would help ascertain the advantages or the absence of any, of endoscopy over the other two conventional approaches.
Summary
What was known before
-
Endoscopy is a useful adjunct in cases with posterior segment pathology following trauma.
-
There is a significant learning curve for the operating surgeon.
What this study adds
-
Endoscopy allows for prognostication of cases with posterior segment pathology following trauma.
-
Appropriate prognostication avoids penetrating keratoplasty in cases with nil prognosis.
-
In appropriate cases, endoscopic approach allows for a resolution of corneal oedema and avoids the need for unnecessary keratoplasty.
References
Sabti KA, Raizada S. Endoscope-assisted pars plana vitrectomy in severe ocular trauma. Br J Ophthalmol. 2012;96:1399–403.
Chun DW, Colyer MH, Wroblewski KJ. Visual and anatomic outcomes of vitrectomy with temporary keratoprosthesis or endoscopy in ocular trauma with opaque cornea. Ophthalmic Surg Lasers Imaging. 2012;43:302–10.
Colyer MH, Weber ED, Weichel ED, Dick JS, Bower KS, Ward TP, et al. Delayed intraocular foreign body removal without endophthalmitis during Iraqi Freedom and Enduring Freedom. Ophthalmology. 2007;114:1439–47.
Garcia-Valenzuela E, Blair NP, Shapiro MJ, Gieser JP, Resnick KI, Solomon MJ, et al. Outcome of vitreoretinal surgery and penetrating keratoplasty using temporary keratoprosthesis. Retina. 1999;19:424–9.
Gallemore RP, Bokosky JE. Penetrating keratoplasty with vitreoretinal surgery using the Eckardt temporary keratoprosthesis: modified technique allowing use of large corneal graft. Cornea. 1995;14:33–8.
Pesko K, Stmen P. Perforation keratoplasty after pars plana vitrectomy and use of temporary keratoprosthesis. Cesk Slov Oftalmol. 1998;54:148–53.
Thorpe H. Ocular endoscope: instrument for removal of intravitreous non magnetic foreign bodies. Trans Am Acad Ophthalmol Otolaryngol. 1934;39:422.
Ayyildiz O, Durukan AH. Comparison of endoscopic-assisted and temporary keratoprosthesis-assisted vitrectomy in combat ocular trauma: experience at a tertiary eye center in Turkey. J Int Med Res. 2018;46:2708–16.
Kim S, Lee S. Comparison of ultrasound and intraoperative finding in patients with vitreous hemorrhage. Investigative Ophthalmol Vis Sci. 2005;46:5436.
Deramo VA, Shah GK, Baumal CR, Fineman MS, Corrêa ZM, Benson WE, et al. Ultrasound biomicroscopy as a tool for detecting and localizing occult foreign bodies after ocular trauma. Ophthalmology. 1999;106:301–5.
Cupples HP, Whitmore PV, Wertz FD 3rd, Mazur DO. Ocular trauma treated by vitreous surgery. Retina. 1983;3:103–7.
Meredith TA, Gordon PA. Pars plana vitrectomy for severe penetrating injury with posterior segment involvement. Am J Ophthalmol. 1987;103:549–54.
Ryan SJ, Allen AW. Pars plana vitrectomy in ocular trauma. Am J Ophthalmol. 1979;88:483–91.
Benson WE, Machemer R. Severe perforating injuries treated with pars plana vitrectomy. Am J Ophthalmol. 1976;81:728–32.
Kuhn F, Maisiak R, Mann L, mester V, Morris R, Witherspoon CD. The ocular trauma score (OTS). Ophthalmol Clin North Am. 2002;15:163–5.
Issac DL, Ghanem VC, Nascimento MA. Prognostic factors in open globe injuries. Ophthalmologica. 2003;217:431–5.
Sternberg P Jr, de Juan E Jr, Michels RG, Auer C. Multivariate analysis of prognostic factors in penetrating ocular injuries. Am J Ophthalmol. 1984;98:467–72.
Schmidt GW, Broman AT, Hindman HB, Grant MP. Vision survival after open globe injury predicted by classification and regression tree analysis. Ophthalmology. 2008;115:202–9.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Dave, V.P., Chakurkar, R., Tyagi, M. et al. Intraocular endoscopy in the management of ocular trauma: clinical settings and treatment outcomes at a tertiary eye care centre. Eye 35, 1904–1908 (2021). https://doi.org/10.1038/s41433-020-01179-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41433-020-01179-1