Abstract
Objectives
To systematically review the scientific evidence comparing the clinical effectiveness of bulk-fill versus incrementally layered conventional resin composites and to evaluate if one method offers clear merits with specific clinical outcomes.
Materials and methods
Using relevant mesh terms and pre-established eligibility criteria in PubMed, Embase, Scopus and Web of Science, a thorough scientific search was conducted with an end-date of 30.04.2023. Randomized controlled clinical trials that involved the direct comparison of Class I and Class II resin composite restorations applied using incremental layering techniques versus bulk-filled in permanent teeth with an observation period of at least six months were considered. To evaluate the bias risk of the finalized records, a revised version of the Cochrane risk-of-bias tool for randomized trials was implemented.
Results
Out of the 1445 records determined, 18 eligible reports were chosen for qualitative analysis. Data obtained was categorized as per, the cavity design, the intervention, the comparator(s), the methods of success/failure assessment, the outcomes, and follow-up. Two studies demonstrated an overall low-risk of bias, fourteen studies raised some concerns, and two studies exhibited high-risk.
Conclusion
Bulk filled resin composite restorations demonstrated clinical outcomes similar to those of incrementally layered resin composite restorations within a review interval of 6 months to 10 years.
Similar content being viewed by others
Introduction
Resin composite has been the preferred direct restorative material by dental practitioners for the treatment of anterior and posterior teeth, with acceptable success rates and longer-term clinical performance reported in the literature1. Resin composite materials offer the benefits of ease of handling, superior physical properties, ability to polymerize on demand, availability in wide range of colors and translucencies, biocompatibility, and satisfactory adhesion to the dental hard tissues2. Composites have reported excellent clinical performance with annual failure rates ranging from 1% to 5% and 1% to 3% for anterior and posterior teeth respectively3. Furthermore, composite resin materials may offer the scope to allow repair4, strengthen the residual tooth structure, and their prescription may facilitate conservative cavity preparation5.
The main challenges encountered when using direct composite resins are, polymerization shrinkage and shrinkage stress, the degree of polymerization conversion, and their limited depth of cure. These factors may influence clinical performance. Adequate polymerization and the use of proper placement techniques are critical for the optimal clinical performance of these restorations6.
Incremental layering of composite resin using increments of ≤2 mm has been suggested to decrease shrinkage stress, improve the degree of conversion, evade disintegration of the restoration margin, and provide adequate esthetics7. The three-site method followed by the use of an oblique layering technique has been considered to be a good approach for composite layering technique and aid with the reduction of polymerization shrinkage8. The split, simultaneous modeling of separated increments has also been suggested to reduce shrinkage issues9. Lower levels of microleakage have been reported with the use of a split horizontal incremental technique at the gingival margin of a cavity10. At the occlusal margin of a Class II restoration, the application of a split horizontal incremental technique followed by the application of a centripetal and oblique placement technique has demonstrated the lowest levels of microleakage11.
The incremental application of resin composite is, however, time consuming. It can be challenging whilst restoring more conservative cavities and is associated with the increased risk of contamination. The incremental application technique also has the scope for unwanted air entrapment between successive layers, which may culminate in adhesive failure between layers12. A rise in the elastic modulus and post-photopolymerization shrinkage has been observed with increasing number of increments7,13.
The challenges with incremental layering have paved the development of bulk-fill composite materials which may be applied in layers of thickness of 4–5 mm, thereby offering the merit of reduced treatment time and the potential of reduced volumetric shrinkage stress as well as improved curing depth whilst maintaining the desired micromechanical properties12.
Polymerization shrinkage of bulk fills is decreased by incorporation of stress modulators like addition-fragmentation monomer (AFM), aromatic urethane dimethacrylate (AUDMA); high molecular mass monomers such as BisEMA, UDMA, BisGMA, Procrylat; and highly reactive photoinitiators. Initiator system optimization and the inclusion of fillers like zirconium / silica, ytterbium trifluoride, proacrylate, mixed oxides, and barium aluminum silicate particles in bulk fill resins have also improved their radiopacity and curing depth14. Polymerization depth is enhanced by better light transmission to deeper areas because of lowered light dispersion at the filler-matrix meeting point by reducing filler load, and/or improving filler particle size15.
Nevertheless, there is inconsistency in determining the curing depth in the literature and a concern among clinicians regarding the degree of conversion16. Furthermore, some constituents and modifications have been reported by the manufacturers of bulk-fill composites, but still certain constituents are unrevealed which may affect the ultimate clinical performance14.
There is a need for a new systematic review that helps clinicians understand the clinical effectiveness of the two composite placement techniques (incremental and bulk-fill). This will also enable practitioners to decide if they can select bulk technique as a reliable alternative method to incremental technique.
The aim of this review was to assess the efficacy of incremental layering versus bulk-fill techniques for the fabrication of direct composite restorations by evaluating their respective clinical outcomes for the restoration of permanent teeth. The objective was to systematically determine if one placement method offers clear benefits over the other by comparing their outcomes (success/failure) of clinical parameters like retention, recurrent/secondary caries, marginal discoloration/staining, marginal adaptation/integrity, fracture, postoperative sensitivity, anatomic form, color match, and surface texture/ roughness.
Materials and methods
The review protocol
The protocol was formulated considering the suggestions of the Cochrane Collaboration for systematic reviews and conforming with the Preferred Reporting Items for Systematic Reviews and Meta‐Analysis Protocols (PRISMA‐P) Statement recommendations17,18. This review was registered with the International Prospective Register of Systematic Reviews (PROSPERO) under the registration number CRD42021258095.
Eligibility criteria
The Review question was, “In permanent teeth restored with direct composites, does incremental layering or bulk-fill technique perform better clinically?”
PICO model for clinical questions was used as follows:
Participants- Participants with permanent teeth restored using direct composite restorations.
Intervention- Bulk technique.
Comparison- Incremental layering technique.
Outcomes- Bulk-fill versus incrementally layered techniques were compared based on their performance (success/ failure) with regards to specific clinical parameters such as; retention, recurrent/secondary caries, marginal discoloration/staining, marginal adaptation/integrity, fracture, postoperative sensitivity, surface texture/ roughness, color match, and anatomical form.
Types of studies- Studies comparing Class I and Class II direct composite restorations restored by incremental layering technique versus bulk technique were involved. Randomized controlled trials (RCTs) were included in this review as bias is reduced by randomization and a meticulous instrument is provided to investigate the connection of an intervention and outcome by cause-effect association19. Non-randomized clinical studies, reviews, case reports, in vitro studies were excluded. Studies where a bulk fill composite was incrementally applied, or either bulk fill or incremental layering was individually assessed, were also excluded.
Timing- Studies with a review period of at least six months were included.
Language- Studies documented in English were selected.
Publication status- Only full papers published in peer-reviewed journals were considered.
Information sources and search strategy
PubMed (National Centre for Biotechnology Information, NCBI)/ MEDLINE (National Library of Medicine), EMBASE (OVID interface), Scopus (Elsevier B.V.), and Web of Science were the electronic databases that were applied. Scientific articles were selected from the electronic databases using different combinations of text words and medical subject headings (MeSH) related to ‘bulk-fill’, ‘incremental layering’, ‘conventional composite’, and ‘direct restorations.’ The electronic probing was accompanied by manually searching of the Journal of Esthetic and Restorative Dentistry, Operative Dentistry, and the Journal of Conservative Dentistry. Furthermore, reference lists of the studies involved were scanned to confirm information saturation of pertinent studies. There was no restriction with regards to the publication date of the literature search. Before the final analysis, the search was repeated and carried out until 30.04.2023.
Study selection
In RefWorks, “Close Duplicates” plus “Exact Duplicates” options were selected in the “View” tab and all associated citations were removed. The remaining studies were screened and evaluated as per their titles and abstracts. Trials that addressed the review question and met the eligibility benchmark, were shortlisted. Consequently, articles that met all the eligibility criteria were finalized. The whole process was provided by one researcher because the basis for this was a thesis project, and any concerns were discussed with the supervisors.
Data extraction
A checklist of information was attained from the selected articles to provide relevant information. Data collected from the shortlisted studies were organized in the form of tables to enable the presentation and evaluation of the proof acquired.
Evaluation of risk of bias in individual trials
The Oxford CEBM (Centre of Evidence-Based Medicine) tool was utilized to ascertain the level and grade of evidence of the articles involved in the review ranging from the highest Level 1a to the lowest Level 5.
The bias risk of the randomized clinical studies involved in the present systematic review were determined with the help of revised Cochrane risk-of-bias tool for randomized trials (RoB 2)20. If the Cochrane Handbook criteria was fulfilled by all the components, it was considered low bias risk; if the elements were questionable, it was viewed as high risk and, if inadequate attributes were found, it was marked as some concerns17.
Results
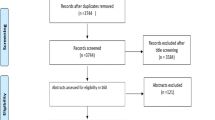
Selection of studies
As shown by Fig. 1, 1445 records were found following the primary investigation of the databases. The full text of 30 reports were thoroughly examined. Further eleven full-text reports were discarded21,22,23,24,25,26,27,28,29,30,31, and their exclusion criteria are listed in Table 1. Eighteen studies were evaluated for their study design and methods for final analysis of the results.
Quality assessment
All the included records displayed level 1b evidence [Individual randomized controlled trials (with narrow confidence interval)]. Since, consistent level 1 studies were observed, the Grade of Recommendation as per CEBM is A.
Characteristics of included studies
Descriptive information obtained in this systematic review is shown in Tables 2–4.
Assessment of risk of bias
Overall, bias risk for all domains was low for two studies32,33 (11.1%). Two studies34,35 demonstrated high risk (11.1%); and fourteen studies6,36,37,38,39,40,41,42,43,44,45,46,47,48 showed some concerns (77.8%) for overall bias risk as shown in Figs. 2 and 3.
Synthesis of results
Due to the variety of composite materials and bonding systems used, and the differences in the design of the involved studies, a meta-analysis that requires relatively homogenous studies could not be performed. Thus, the results were summarized in a qualitative way by listing data from the included studies as per the cavity design, the intervention, the comparator(s), the methods of success/failure assessment, the outcomes, and follow-up. The quality of the data obtained from the included studies was weighed via the risk of bias assessment, giving greater reliability to the higher quality study results.
Analysis of the systematic reviews with a relevant review question
A 16 item-criterion appraisal tool known as AMSTAR-2 was applied to methodologically inspect the quality of systematic reviews with a relevant review question49. The evaluation of the systematic reviews by AMSTAR 2 (Table 5) graded one study50 moderate quality as no critical flaws were found but study design selection was not explained, the effect of risk-of-bias (RoB) from included studies on the outcome of meta-analysis was not assessed, and funding sources for involved studies was not reported. Two studies51,52 were graded critically low, as both had critical flaws such as review protocol was not registered before commencement and the publication bias was not assessed. Additionally, exclusion of individual studies was not justified in one study52.
Discussion
Traditionally, the incremental application of resin composite is prescribed to allow efficient polymerization, to control polymerization shrinkage and stress, and to improve the C-factor. However, aggravated deformation of compromised cusps has been demonstrated with increasing number of increments13. Also, when incrementally layering composites, void formation between increments can take place, resulting in sensitivity, deterioration of the resin material, and cuspal deflection53,54. On the other hand, the bulk-fill application technique provides ease of placement, lower technical sensitivity, and is less time-consuming31. Bulk-filling also prevents disintegration of mechanical properties, with a reduced risk of void formation55. But, there is a significant variation between individual bulk-fill products regarding filler particle size and framework, plus method of clinical placement, which can impact their clinical performance14.
According to the studies included in this review, bulk-fill technique demonstrated no notable distinction in clinical performance compared to the incremental layering technique for the specific clinical parameters considered.
The success of a restoration in clinical studies is demonstrated by its endurance in the oral cavity, making retention the most significant evaluation criteria42. One report recorded retention failure with two Tetric EvoCeram bulk-fills and one incrementally placed Tetric EvoCeram restoration. The difference in retention was linked to the adhesive material or the method used35. Loss of retention was recorded with two Filtek Supreme XTE and none with Filtek Bulk Fill Posterior in a three-year study37. This was associated with the viscoelastic property of the bulk-fill material used due to which shrinkage stress was not a problem56. One Filtek bulk-fill was lost in a study due to technical error during restoration placement41.
Fracture and recurrent caries formation are the primary causes for the failure of directly placed composite restorations1,57. Even in this systematic review, the reasons for failures predominantly were tooth- and resin-fractures, followed by secondary caries in both bulk-fill restorations and incrementally layered conventional restorations respectively. Patients with temporomandibular disorders or parafunctional habits like bruxism can eventually impact the sound tooth, resulting in restoration- and tooth-fractures3,58. Two studies demonstrated a substantially notable number of failures caused by resin composite and/or tooth fractures, mostly amongst bruxist patients44,47. One report recorded teeth fractures with Quixfil bulk restorations (n = 2) and incremental Tetric Ceram resin (n = 1)48. Fracture risk is higher when premature fatigue of the bonding agent occurs at the restoration-tooth interface57,59, which was considered by the study as the probable cause of failure with Quixfil bulk-fills (n = 3)48. High fracture rate of resin composites, both conventional and bulk composites has been reported by many included studies37,39,44,47,48, which could be a material-specific constrain of composites3.
Biological factors may be the cause of secondary caries instead of the material being used to restore60. High caries-risk individuals or low socio-economic status patients with restricted access to health services are susceptible to recurrent caries formation1,57,61. In this review, patients with substandard dental hygiene and high caries risk were excluded in several records35,36,37,40,41,42,43,45,46,48. However, two records included high-risk caries participants which was linked to SDR flowable bulk +Ceram X mono (n = 2) and incremental Ceram X mono (n = 1) restoration failures due to secondary caries44,47. Despite selecting patients with good dental hygiene, in one of the included trials, secondary caries was detected with incrementally placed Tetric N-Ceram resins (n = 2) and QuiXfil bulk-fills (n = 2). It was assumed to be connected to restorative material’s physical framework or the adhesive system efficacy39.
During restoration placement, contamination with saliva and marginal adaptation faults were associated with secondary caries development (n = 5) in another study41,61,62. According to an earlier systematic review, a lower failure rate of direct restorations was observed to occur with the use of rubber dam isolation than those performed using saliva ejectors and cotton rolls as a means of attaining the required moisture control63. Amongst the four studies in this review where rubber dam isolation was used, the absence of any restorative failures were observed33,36,40,45.
Marginal adaptation is affected by the long-term deterioration of the bonding system and polymerization shrinkage of the composite used64. Marginal adaptation may deteriorate over time by hydrolysis of the adhesive interface which occurs when monomers absorb water and chemicals65. This was seen in an included study where marginal integrity had declined after 10 years in both groups39. Hydrolytic degradation of Optibond All-In-One adhesive was documented by included records which might have influenced the adhesive strength of restorations, thereby affecting the marginal integrity40,41. Using radiological assessment, marginal adaptation was found to be good over time with Filtek bulk fill posterior restorative group, whereas a formation of gap was observed from first day in 96.7% of the incrementally layered Filtek Z250XT group6. The ISO requirements for radiopacity were met by Filtek bulk fill posterior restorative in this study66. The marginally higher radiopacity of the incremental nanohybrid than enamel may have caused accurate discernment of defects60.
Another study reported marginal degradation of incrementally packed Amelogen Plus restorations, beginning at six-months and deterioration at one-year follow-up. Conversely, the low shrinkage SureFil SDR bulk-fill and Filtek Bulk Fill Flow restorations showed marginal alteration only after a year33. Equivalent results were assessed in a similar study conducted with the same three resin composites34. This may be associated with the low elastic modulus of the bulk-fills, decreasing the polymerization stresses and hence, sustaining the marginal adaptation67. Likewise another record demonstrated poor marginal integrity of incrementally layered Filtek Ultimate restorations in comparison to Tetric EvoCeram Bulk Fill restorations45, caused by the increased water sorption of low molecular-weight monomers with the former68 and lower polymerization shrinkage of the latter69. Corroborating with a systematic review and meta-analysis of in vitro studies70, conventional resin composites with incremental techniques were found to have marginal integrity comparable to bulk fill composites in an included report34.
Marginal staining may be the first clinical sign of restoration failure71. It is usually caused by the faults present between the cavity margins and composite restoration because of substandard bonding, ineffective composite placement, or polishing methods, and/ or by successive stress fatigue72,73,74,75. Higher marginal discolouration may be linked to the presence of poor marginal adaptation76. The same was noted in an included study with incremental Filtek Ultimate group where marginal defects from contraction stress might have produced staining45. Marginal staining was reported in another report with multi-layered Tetric EvoCeram (n = 1) and Tertic N-Ceram Bulk Fill (n = 2). In comparison, no failures were seen with Sonic fill composite resin whose viscosity is reduced due to sonic vibration, resulting in better adaptation to the cavity walls and hence, improved marginal properties46.
Marginal discolouration has been documented to occur more frequently in cases using the self-etch technique77,78,79. According to a study, low bravo scores for marginal discoloration of both nano-hybrid (Tetric EvoCeram) and Tetric EvoCeram bulk-fill restorations may be because etching with phosphoric acid was not done42. Significantly lower marginal discolouration was observed with the restoration of cavities with bulk-fill composite in a single layer, compared to conventional composites in two included studies. But this was disregarded by both the studies as no additional treatment was required for minor surface discoloration6,45. Conversely, higher marginal discolouration was presented by bulk-fill composite systems than the conventional one in a study of this systematic review34.
Majority of the included studies recorded no post-operative sensitivity in the teeth restored33,34,35,36,37,38,40,42,43,44,45,47. Depth and dimensions of the cavity prepared, marginal seal and liner application in deep cavities, can also influence postoperative sensitivity41,42,80,81,82,83. Most studies assessing postoperative sensitivity did not describe the cavity depth or involved more shallow cavities. Only one study proved all the cavities being restored were 4–5 mm deep by radiographic assessment40 and most cavities were described to be deep in two studies44,47. Application of liners in deep cavities shields the pulpo-dentin complex, reducing heat/electric stimuli, dentin sensitivity, and helps in reparative dentin formation84. No post-operative sensitivity was noted in studies with liner applied in deep cavities38,41,42. Following 12-months, sensitivity was recorded in only one tooth with a deep cavity among the ones filled with bulk-fill via sonic activation. This was regarded to be caused by the absence of a calcium hydroxide based liner40. Use of flowable composite linings reported no restorative failures in another study43. Contradictory evidence was found concerning the application of liners and post-operative sensitivity in a Cochrane review85. According to one report, higher sensitivity was recorded with the use of incrementally applied Filtek Z250XT compared to Filtek bulk-fill posterior restorative, which may be linked to adhesive failure or cusp deflection6.
Surface texture modifications can be associated with the composite’s filler load, size, or hardness86. In one study, surface texture was rougher after finishing and polishing of some nanohybrid restorations, which was attributed to large fillers exfoliating from the matrix while polishing87. Slightly rougher surface was reported in a study with Filtek Ultimate group which was associated with void entrapment in the incremental layering method45. The differences in surface roughness / texture may be related to the fact that there is no specific finishing and polishing system for bulk-fill materials. For full-body bulk-fill resin composites, multistep finishing/polishing systems have been suggested to give greater polishability88.
Color stability in a study35 was contemplated to be influenced by intrinsic factors like resin’s organic matrix86,89. One trial reported better performance of incremental microhybrid Amelogen Plus compared to Filtek Bulk Fill Flow + Filtek Z350XT with regards to superficial staining33. This may be associated to better sorption ability of the nanoparticles in Filtek bulk fill90. Best results were observed with SDR + TPH3 as it was less prone to liquid absorption which was linked to the absence of triethylene-glycol dimethacrylate in TPH391. Good color stability was seen because of compact filler particles present in bulk- and conventional-resins used in a study46, and because of resistance to color modification provided by the presence of Urethane Dimethacrylate (UDMA) polymer matrix like that found in an earlier study92.
In one study, sonic fill was found to provide anatomically superior results compared to incremental Filtek bulk fill, Tetric EvoCeram bulk fill, and Clearfil photo posterior41.
Limitations of the study
The comparative assessment of both the techniques was difficult, as the included studies involved in the review had a number of variables such as, different etching and bonding techniques for different restorative materials (incrementally layered conventional resin composites and bulk-fill) along with varied patient, operator, cavity, and oral condition factors. Evaluation criteria methods were non-standardized and analysis for the clinical parameters were not always explicitly provided.
Suggestions for future study
The comparison between the two composite placement techniques will be more adequate with studies involving similar materials with fewer variable factors. Clinical trials with an extended observation period are required to attain stronger evidence and information regarding the performance of layering techniques clinically.
Conclusion
This systematic review disclosed that:
-
Direct resin composite restorations fabricated using incrementally layered techniques performed clinically just as well as those formed using bulk-fill technique in the permanent dentition.
-
The placement techniques demonstrated no significant differences with regards to, retention, recurrent/secondary caries, marginal discoloration/staining, marginal adaptation/integrity, fracture, postoperative sensitivity, surface texture/ roughness, color match, and anatomical form.
-
The bulk-fill technique is a good alternative treatment option to incremental filling, offering reduced restoration time and the scope for a reduction in feasible operator errors.
References
Montagner AF, Sande FH, Müller C, Cenci MS, Susin AH. Survival, reasons for failure and clinical characteristics of anterior/posterior composites: 8-year findings. Braz Dent J. 2018;29:547–54.
Alrahlah A. Diametral tensile strength, flexural strength, and surface microhardness of bioactive bulk fill restorative. J Contemp Dent Pract. 2018;19:13–19.
Demarco FF, Collares K, Correa MB, Cenci MS, Moraes RR, Opdam NJ. Should my composite restorations last forever? Why are they failing? Braz Oral Res. 2017;31:e56.
Blum IR, Jagger DC, Wilson NH. Defective dental restorations: to repair or not to repair? Part 1: direct composite restorations. Dent Update. 2011;38:78–84.
Bayraktar Y, Ercan E, Hamidi MM, Çolak H. One-year clinical evaluation of different types of bulk-fill composites. J Investig Clin Dent. 2016;8:e12210.
Hardan L, Sidawi L, Akhundov M, Bourgi R, Ghaleb M, Dabbagh S, et al. One-year clinical performance of the fast-modelling bulk technique and composite-up layering technique in class I cavities. Polymers. 2021;13:1873.
Almeida Junior LJ, Penha KJ, Souza AF, Lula EC, Magalhães FC, Lima DM, et al. Is there correlation between polymerization shrinkage, gap formation, and void in bulk fill composites? A μCT study. Braz Oral Res. 2017;31:e100.
Yadav KD, Prasad RS, Chaganti H, Saleem M, Pai A. Techniques in direct composite restoration. Modern Approaches Dent Oral Health Care. 2018;3:307–9.
Scolavino S, Paolone G, Orsini G, Devoto W, Putignano A. The Simultaneous Modeling Technique: closing gaps in posteriors. Int J Esthetic Dent. 2016;11:58–81.
Roopa R, Anupriya B. Effect of four different placement techniques on marginal microleakage in class II restorations: an in vitro study. World J Dent. 2011;2:111–116.
Chandrasekhar V, Rudrapati L, Badami V, Tummala M. Incremental techniques in direct composite restoration. J Conserv Dent. 2017;20:386–91.
Guney T, Yazici A. 24-month clinical evaluation of different bulk-fill restorative resins in class II restorations. Oper Dent. 2020;45:123–33.
Versluis A, Douglas W, Cross M, Sakaguchi R. Does an incremental filling technique reduce polymerization shrinkage stresses? J Dent Res. 1996;75:871–8.
Corral-Núnez C, Vildósola-Grez P, Bersezio-Miranda C, Alves-Dos Campos E, Fernández, Godoy E. State of the art of bulk-fill resin-based composites: a review. Revista De La Facultad De Odontología Universidad De Antioquia. 2015;27:177–96.
Haugen HJ, Marovic D, Par M, Khai Le Thieu M, Reseland JE, Johnsen GF. Bulk fill composites have similar performance to conventional dental composites. Int J Mol Sci. 2020;21:5136.
Van Ende A, De Munck J, Lise DP, Van Meerbeek B. Bulk-fill composites: a review of the current literature. J Adhes Dent. 2017;19:95–109.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. Wiley Cochrane series, 2nd ed. Newark: John Wiley & Sons, Ltd; 2019.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ Brit Med J. 2021;372:n71.
Hariton E, Locascio J. Randomised controlled trials - the gold standard for effectiveness research. BJOG. 2018;125:1716–1716.
Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ Brit Med J. 2019;366:4898.
Balkaya H, Arslan S, Pala K. A randomized, prospective clinical study evaluating effectiveness of a bulk-fill composite resin, a conventional composite resin and a reinforced glass ionomer in Class II cavities: one-year results. J Appl Oral Sci. 2019;27:e20180678.
Durão MDE, Andrade AK, Santos MDO, Montes MA, Monteiro GQ. Clinical performance of bulk-fill resin composite restorations using the United States Public Health Service and Federation Dentaire Internationale Criteria: a 12-month randomized clinical trial. Eur J Dent. 2020;15:179–92.
Manhart J, Chen H-Y, Neuerer P, Thiele L, Jaensch B, Hickel R. Clinical performance of the posterior composite QuiXfil after 3, 6, and 18 months in class 1 and 2 cavities. Quint Int. 2008;39:757–65.
Manhart J, Chen H-Y, Hickel R. Three-year results of a randomized controlled clinical trial of the posterior composite QuiXfil in class I and II cavities. Clin Oral Invest. 2009;13:301–7.
Moda MD, Briso AF, Hoshino I, Frascino S, Santos PH, Gonçalves D, et al. Three-year randomized prospective clinical trial of class II restorations using flowable bulk-fill resin composites. Oper Dent. 2021;46:516–28.
van Dijken JWV, Pallesen U. A randomized controlled three-year evaluation of “bulk-filled” posterior resin restorations based on stress decreasing resin technology. Dent Mater. 2014;30:e245–e251.
van Dijken JWV, Pallesen U. Randomized 3-year clinical evaluation of class I and II posterior resin restorations placed with a bulk-fill resin composite and a one-step self-etching adhesive. J Adhes Dent. 2015;17:81–88.
Arhun N, Celik C, Yamanel K. Clinical evaluation of resin-based composites in posterior restorations: two-year results. Oper Dent. 2010;35:397–404.
Loguercio AD, Rezende M, Gutierrez MF, Costa TF, Armas-Vega A, Reis A. Randomized 36-month follow-up of posterior bulk-filled resin composite restorations. J Dent. 2019;85:93–102.
Hickey D, Sharif O, Janjua F, Brunton PA. Bulk dentine replacement versus incrementally placed resin composite: a randomised controlled clinical trial. J Dent. 2016;46:18–22.
Tardem C, Albuquerque EG, Lopes LD, Marins SS, Calazans FS, Poubel LA, et al. Clinical time and postoperative sensitivity after use of bulk-fill (syringe and capsule) vs. incremental filling composites: a randomized clinical trial. Braz Oral Res. 2019;33:e089.
Durão MDA, de Andrade AKM, do Prado AM, Montes MA, Monteiro GQ. Thirty-six-month clinical evaluation of posterior high-viscosity bulk-fill resin composite restorations in a high caries incidence population: interim results of a randomized clinical trial. Clin Oral Invest. 2021;25:6219–37.
Frascino SMB, Fagundes TC, Silva UAE, Rahal V, Barboza A, Santos PH, et al. Randomized prospective clinical trial of class II restorations using low shrinkage flowable resin composite. Oper Dent. 2020;45:19–29.
Endo Hoshino IA, Fraga Briso AL, Bueno Esteves LM, Dos Santos PH, Meira Borghi FS, Fagundes TC. Randomized prospective clinical trial of class II restorations using flowable bulk-fill resin composites:4-year follow-up. Clin Oral Invest. 2022;26:5697–710.
Al-Sheikh R. Effects of different application techniques on nanohybrid composite restorations clinical success. Open Dent J. 2019;13:228–35.
Salem MN, Hassanein OE, El Kassas DW, Shaalan OO. 12-months clinical evaluation of fiber reinforced bulk fill resin composite versus incremental packing of nanohybrid resin composite in restoration of deep proximal lesions of permanent molars: a randomized controlled trial. Acta Stomatol Croat. 2022;56:267–80.
Sekundo C, Fazeli S, Felten A, Schoilew K, Wolff D, Frese C. A randomized clinical split-mouth trial of a bulk-fill and a nanohybrid composite restorative in class II cavities: three-year results. Dent Mater. 2022;38:759–68.
Balkaya H, Arslan S. A two-year clinical comparison of three different restorative materials in class II cavities. Oper Dent. 2020;45:E32–E42.
Heck K, Manhart J, Hickel R, Diegritz C. Clinical evaluation of the bulk fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent Mater. 2018;34:e138–e147.
Atabek D, Aktaş N, Sakaryali D, Bani M. Two-year clinical performance of sonic-resin placement system in posterior restorations. Quint Int. 2017;48:743–51.
Bayraktar Y, Ercan E, Hamidi MM, Çolak H. One‐year clinical evaluation of different types of bulk‐fill composites. J Invest Clin Dent. 2017;8:e12210.
Colak H, Tokay U, Uzgur R, Hamidi MM, Ercan E. A prospective, randomized, double-blind clinical trial of one nano-hybrid and one high-viscosity bulk-fill composite restorative systems in class II cavities: 12 months results. Niger J Clin Pract. 2017;20:822–31.
Karaman E, Keskin B, Inan U. Three-year clinical evaluation of class II posterior composite restorations placed with different techniques and flowable composite linings in endodontically treated teeth. Clin Oral Investig. 2017;21:709–16.
van Dijken JWV, Pallesen U. Bulk-filled posterior resin restorations based on stress-decreasing resin technology: a randomized, controlled 6-year evaluation. Eur J Oral Sci. 2017;125:303–9.
Yazici AR, Antonson SA, Kutuk ZB, Ergin E. Thirty-six-month clinical comparison of bulk fill and nanofill composite restorations. Oper Dent. 2017;42:478–85.
Alkurdi R, Abboud S. Clinical evaluation of class II composite: resin restorations placed by two different bulk-fill techniques. J Orofac Sci. 2016;8:34–39.
van Dijken JWV, Pallesen U. Posterior bulk-filled resin composite restorations: a 5-year randomized controlled clinical study. J Dent. 2016;51:29–35.
Manhart J, Chen HY, Hickel R. Clinical evaluation of the posterior composite quixfil in class I and II cavities: 4-year follow-up of a randomized controlled trial. J Adhes Dent. 2010;12:237–43.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ Brit Med J. 2017;358:j4008.
Veloso SRM, Lemos CAA, de Moraes SL, do Egito Vasconcelos BC, Pellizzer EP, de Melo Monteiro GQ. Clinical performance of bulk-fill and conventional resin composite restorations in posterior teeth: a systematic review and meta-analysis. Clin Oral Invest. 2019;23:221–33.
Arbildo-Vega HI, Lapinska B, Panda S, Lamas-Lara C, Khan AS, Lukomska-Szymanska M. Clinical effectiveness of bulk-fill and conventional resin composite restorations: systematic review and meta-analysis. Polymers. 2020;12:1786.
Cidreira Boaro LC, Pereira Lopes D, de Souza ASC, Lie Nakano E, Ayala Perez MD, Pfeifer CS, et al. Clinical performance and chemical-physical properties of bulk fill composites resin —a systematic review and meta-analysis. Dent Mater. 2019;35:e249–e264.
Alrahlah A, Silikas N, Watts DC. Post-cure depth of cure of bulk fill dental resin-composites. Dent Mater . 2013;30:149–54.
Sajnani A, Hegde M. Leaching of monomers from bulk-fill composites: an in vitro study. J Conserv Dent. 2016;19:482–6.
Roggendorf MJ, Krämer N, Appelt A, Naumann M, Frankenberger R. Marginal quality of flowable 4-mm base vs. conventionally layered resin composite. J Dent. 2011;39:643–7.
Davidson CL, Feilzer AJ. Polymerization shrinkage and polymerization shrinkage stress in polymer-based restoratives. J Dent. 1997;25:435–40.
Askar H, Krois J, Göstemeyer G, Bottenberg P, Zero D, Banerjee A, et al. Secondary caries: what is it, and how it can be controlled, detected, and managed? Clin Oral Invest. 2020;24:1869–76.
Opdam NJ, Sande FHVD, Bronkhorst E, Cenci MS, Bottenberg P, Pallesen U, et al. Longevity of posterior composite restorations: a systematic review and meta-analysis. J Dental Res. 2014;93:943–9.
Roumanas ED. The frequency of replacement of dental restorations may vary based on a number of variables, including type of material, size of the restoration, and caries risk of the patient. J Evid Based Dental Pract. 2010;10:23–24.
Nedeljkovic I, Teughels W, De Munck J, Van Meerbeek B, Van Landuyt KL. Is secondary caries with composites a material-based problem? Dental Mater. 2015;31:e247–e277.
Burke FJT, Wilson NHF, Cheung SW, Mjör IA. Influence of patient factors on age of restorations at failure and reasons for their placement and replacement. J Dent. 2001;29:317–24.
Mjör IA, Shen C, Eliasson ST, Richter S. Placement and replacement of restorations in general dental practice in iceland. Oper Dent. 2002;27:117–23.
Wang Y, Li C, Yuan H, et al. Rubber dam isolation for restorative treatment in dental patients. Cochrane Library. 2016;2016:CD009858.
Poggio C, Chiesa M, Scribante A, Mekler J, Colombo M. Microleakage in class II composite restorations with margins below the CEJ: in vitro evaluation of different restorative techniques. Med Oral Patol Oral Cir Bucal. 2013;18:e793–8.
Hashimoto M, Ohno H, Kaga M, Endo K, Sano H, Oguchi H. In vivo degradation of resin-dentin bonds in humans over 1 to 3 years. J Dent Res. 2000;79:1385–91.
Yasa B, Kucukyilmaz E, Yasa E, Ertas E. Comparative study of radiopacity of resin-based and glass ionomer-based bulk-fill restoratives using digital radiography. J Oral Sci. 2015;57:79–85.
Campos EA, Ardu S, Lefever D, Jasse FF, Bortolotto T, Krejci I. Marginal adaptation of class II cavities restored with bulk-fill composites. J Dent. 2014;42:575–81.
Asmussen E, Peutzfeld A. Influence of pulse-delay curing on softening of polymer structures. J Dental Res. 2001;80:1570–3.
Boaro LC, Gonçalves F, Guimarães TC, Ferracane JL, Versluis A, Braga RR. Polymerization stress, shrinkage and elastic modulus of current low-shrinkage restorative composites. Dental Mater. 2010;26:1144–50.
Gerula-Szymańska A, Kaczor K, Lewusz-Butkiewicz K, Nowicka A. Marginal integrity of fowable and packable bulk fll materials used for class II restorations -a systematic review and meta-analysis of in vitro studies. Dental Mater J. 2020;39:335–44.
Loguercio AD, Mânica D, Ferneda F, Zander-Grande C, Amaral R, Stanislawczuk R, et al. A randomized clinical evaluation of a one- and two-step self-etch adhesive over 24 months. Oper Dent. 2010;35:265–72.
Kubo S, Yokota H, Yokota H, Hayashi Y. Three-year clinical evaluation of a flowable and a hybrid resin composite in non-carious cervical lesions. J Dent. 2009;38:191–200.
Poon ECM, Smales RJ, Yip KH. Clinical evaluation of packable and conventional hybrid posterior resin-based composites: results at 3.5 years. J Am Dental Assoc. 2005;136:1533–40.
Sadeghi M, Lynch CD, Shahamat N. Eighteen-month clinical evaluation of microhybrid, packable and nanofilled resin composites in class I restorations. J Oral Rehabilit. 2010;37:532–7.
Van Landuyt KL, Peumans M, Fieuws S, De Munck J, Cardoso MV, Ermis RB, et al. A randomized controlled clinical trial of a HEMA-free all-in-one adhesive in non-carious cervical lesions at 1 year. J Dent. 2008;36:847–55.
Heintze S. Systematic reviews: I. The correlation between laboratory tests on marginal quality and bond strength. II. The correlation between marginal quality and clinical outcome. J Adhes Dent. 2007;9:77–106.
Perdigão J, Kose C, Mena-Serrano AP, De Paula EA, Tay LY, Reis A, et al. A new universal simplified adhesive: 18-month clinical evaluation. Oper Dent. 2014;39:113–27.
Peumans M, De Munck J, Van Landuyt K, Van Meerbeek B. Thirteen-year randomized controlled clinical trial of a two-step self-etch adhesive in non-carious cervical lesions. Dental Mater. 2015;31:308–14.
Burrow M, Tyas M. Clinical investigation of G-bond resin-based adhesive to non-carious cervical lesions over five years. Aust Dental J. 2012;57:458–63.
Browning WD, Blalock JS, Callan RS, Brackett WW, Schull GF, Davenport MB, et al. Postoperative sensitivity: a comparison of two bonding agents. Oper Dent. 2007;32:112–7.
Costa T, Rezende M, Sakamoto A, Bittencourt B, Dalzochio P, Loguercio AD, et al. Influence of adhesive type and placement technique on postoperative sensitivity in posterior composite restorations. Oper Dent. 2017;42:143–54.
Berkowitz G, Spielman H, Matthews A, Vena D, Craig R, Curro F, et al. Postoperative hypersensitivity and its relationship to preparation variables in class I resin-based composite restorations: findings from the practitioners engaged in applied research and learning (PEARL) network. part 1. Compend Contin Educ Dent. 2013;34:e44–e52.
Briso ALF, Mestrener SR, Delício G, Sundfeld RH, Bedran-Russo AK, de Alexandre RS, et al. Clinical assessment of postoperative sensitivity in posterior composite restorations. Oper Dent. 2007;32:421–6.
de Souza Costa CA, Aparecida Giro EM, Lopes do Nascimento AB, Teixeira HM, Hebling J. Short-term evaluation of the pulpo-dentin complex response to a resin-modified glass-ionomer cement and a bonding agent applied in deep cavities. Dental Mater. 2003;19:739–46.
Schenkel AB, Peltz I, Veitz-Keenan A. Dental cavity liners for class I and class II resin-based composite restorations. Cochrane Database Syst. Rev. 2016;10:CD010526.
Novaes JBJ, Araújo PV, Damas F, Gala-Garcia A, Cortés ME. Clinical evaluation of packable resin class I restorations after 7 years. Braz J Oral Sci. 2009;7:1585–90.
El-Eraky M, Abdel-Fattah W, El-Said M. Clinical assessment of a nanohybrid and silorane low shrinkage composite in class I cavity preparation (preliminary report). Tanta Dental J. 2014;11:130–8.
Paolone G, Moratti E, Goracci C, Gherlone E, Vichi A. Effect of finishing systems on surface roughness and gloss of full-body bulk-fill resin composites. Materials. 2020;13:5657.
Lopes L, Cefaly D, Franco E, Mondelli R, Lauris J, Navarro M. Clinical evaluation of two “packable” posterior composite resins: two-year results. Clinical Oral Investig. 2003;7:123–8.
Rahim TNAT, Mohamad D, Md Akil H, Ab Rahman I. Water sorption characteristics of restorative dental composites immersed in acidic drinks. Dental Mater. 2012;28:e63–e70.
Lemos CAA, Mauro SJ, dos Santos PH, Briso ALF, Fagundes TC. Influence of mechanical and chemical degradation in the surface roughness, gloss, and color of microhybrid composites. J Contemp Dental Pract. 2017;18:283–8.
Bayne SC, Schmalz G. Reprinting the classic article on USPHS evaluation methods for measuring the clinical research performance of restorative materials. Clin Oral Investig. 2005;9:209–14.
Author information
Authors and Affiliations
Contributions
AS: conception, data acquisition, provision and management of study literature resources, synthesis, visualization, interpretation, and drafted the manuscript. ON: had oversight of the study planning and execution, and to the design, data acquisition, synthesis, interpretation, and drafted the manuscript. SBM, SB: conception, design, and critically revised the manuscript. All authors gave their final approval and agreed to be accountable for all aspects of the work. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sengupta, A., Naka, O., Mehta, S.B. et al. The clinical performance of bulk-fill versus the incremental layered application of direct resin composite restorations: a systematic review. Evid Based Dent 24, 143 (2023). https://doi.org/10.1038/s41432-023-00905-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41432-023-00905-4