Abstract
Cantu Syndrome (CS), [OMIM #239850] is characterized by hypertrichosis, osteochondrodysplasia, and cardiomegaly. CS is caused by gain-of-function (GOF) variants in the KCNJ8 or ABCC9 genes that encode pore-forming Kir6.1 and regulatory SUR2 subunits of ATP-sensitive potassium (KATP) channels. Many subjects with CS also present with the complication of lymphedema. A previously uncharacterized, heterozygous ABCC9 variant, p.(Leu1055_Glu1058delinsPro), termed indel1055, was identified in an individual diagnosed with idiopathic lymphedema. The variant was introduced into the equivalent position of rat SUR2A, and inside-out patches were used to characterize the KATP channels formed by Kir6.2 and WT or mutant SUR2A subunits coexpressed in Cosm6 cells. The indel1055 variant causes gain-of-function of the channel, with an increase of the IC50 for ATP inhibition compared to WT. Retrospective consideration of this individual reveals clear features of Cantu Syndrome. An additional heterozygous ABCC9 variant, p.(Ile419Thr), was identified in a second individual diagnosed with lymphedema. In this case, there were no additional features consistent with CS, and the properties of p.(Ile416Thr) (the corresponding mutation in rat SUR2A)--containing channels were not different from WT. This proof-of-principle study shows that idiopathic lymphedema may actually be a first presentation of otherwise unrecognized Cantu Syndrome, but molecular phenotyping of identified variants is necessary to confirm relevance.
Similar content being viewed by others
Introduction
Lymphedema is a progressive disease with swelling and fibrosis of the affected region, leading to functional problems and infections. Primary lymphedema can result from congenital dysfunction of the lymphatic system with defective transport of lymph (consisting of residual interstitial fluid, immune cells, and lipids) from the peripheral tissues to the central venous system. In classical views, passive forces are the main reason for lymph transport, but it is now clear that contractions of lymphatic smooth muscle cells and synchronized contraction waves driven by spontaneous action potentials are required for effective lymph propulsion. There is no cure or effective treatment for lymphedema subjects and only conservative measures, such as compression therapy (bandages/garments) in combination with exercise, manual lymphatic drainage and skin hygiene advice are currently available as treatment [1]. The lack of specific therapy options reflects a lack of understanding of the molecular mechanisms of lymphedema development.
KATP channels are hetero-octameric potassium-selective ion channels consisting of 4 pore-forming Kir6.x subunits (Kir6.1 or Kir6.2 encoded by KCNJ8 and KCNJ11, respectively) and 4 auxiluary sulfonylurea receptor SURx subunits (SUR1, SUR2 encoded by ABCC8 and ABCC9) [2]. ATP binds to Kir6.x subunits to inhibit channel function. Like other ABCC proteins, SUR subunits contain two cytoplasmic nucleotide binding domains (NBD) which undergo dimerization upon Mg2+-dependent binding of ATP or ADP between them and this dimerization allosterically activates the channel. Thus, KATP channels couple cell metabolism to excitability by sensing intracellular nucleotide levels [2]. Channel complexes with different combinations of Kir6.1 and SUR subunits are present in various tissues, with expression of Kir6.1 and SUR2B subunits being prominent in all smooth muscles, including lymphatic smooth muscle (LSM) [3,4,5]. Treatment with the SUR2-specific activator pinacidil, or introduction of a GOF variant in Kir6.1 (Kir6.1[GD-QR]) causes LSM hyperpolarization and severely decreases lymphatic contraction [5], suggesting that overactivity of KATP channels in LSM could be a primary cause of lymphedema. This is a likely explanation for the high frequency of lymphedema in Cantu Syndrome (CS), a rare genetic disease which results from GOF variants in Kir6.1 or SUR2 subunits [6,7,8,9,10]. In addition to lymphedema, CS is characterized by hypertrichosis, coarse facial features, osteochondrodysplasia, and multiple cardiovascular abnormalities including tortuous blood vessels, patent ductus arteriosus (PDA) and cardiac hypertrophy [11]. Because of its rarity, and diversity of features, CS can be underdiagnosed, or misdiagnosed. It also raises the possibility that cases of idiopathic lymphedema could also be caused by Kir6.1 or SUR2 GOF and may then also have other features that fit with the diagnosis of CS. In this study, we aimed to test this possibility by characterizing the effect of two ABCC9 variants that were identified in two individuals with lymphedema.
Materials and methods
Molecular genetic analysis
Next generation sequencing of a gene panel for lymphedema was performed as part of clinical diagnosis at the Amsterdam UMC. In short, target enrichment was done using a custom designed in-solution capture (SeqCap EZ Choice, Nimblegen). Enriched libraries were sequenced on a MiSeq sequencer, 2x150bp (Illumina). Sequencing reads were mapped to GRCh37/hg19 reference genome using BWA-MEM (0.7.12). Variants were identified using the HaplotypeCaller from GATK (3.8) (Genome Analysis Toolkit, Broad Institute) along with Picard tools (1.95). Variant prioritization and assessment was done using Alissa Interpret (Agilent) and Alamut (Sophia Genetics). The gene panel consisted of 37 genes: ABCC9, ALG8, BRAF, CBL, CCBE1, CDK19, DCHS1, FAT4, FLT4, FOXC2, GATA2, GJA1, GJC2, GLA, HGF, HRAS, ITGA9, KIF11, KRAS, MAP2K1, MAP2K2, MET, MPI, NAGA, NRAS, PEPD, PMM2, PTPN11, PTPN14, RAF1, RELN, SHOC2, SOS1, SOX18, SPRED1, TUBGCP6, VEGFC. These genes were selected based on variants in these genes being previously causally associated with lymphedema, or causing genetic syndromes in which lymphedema is one of the recognized phenotypes. Although KCNJ8 is now also known to be causal in CS [7, 8], this link was not recognized at the time of definition of the lymphedema gene panel.
Evaluation of variants in exons and flanking 20 intronic nucleotides with an allele frequency of less than 1% for recessive disorders, and less than 0.2% for dominant disorders, and variants labeled as (likely) pathogenic in ClinVar, HGMD or in house databases, indicated the ABCC9 variant as the only candidate in each subject.
Molecular biology and cell culture
Variants were introduced into rat SUR2A (pCMV_ rSUR2A; GenBankTM accession no. D83598.1) cDNA using site-directed mutagenesis and verified by direct Sanger sequencing. The residue numbering refers to the rSUR2A clone, which shares 97% sequence identity with the human sequence, and which was used to allow direct comparison with previous reports of the effects of other Cantu syndrome variants that also used rSUR2A. Cosm6 cells were cultured in Dulbecco’s modified Eagle’s medium (DMEM) and transfected using FuGENE 6 (Roche Applied Science) or PEI with wildtype pcDNA3.1_mKir6.2 (0.6 μg; GenBankTM accession no. D50581.1) and wildtype or variant pCMV_rSUR2A constructs (1 μg) in addition to 0.2 μg of pcDNA3.1_eGFP for visual detection of successful transfection. Excised patch-clamp recordings were made 48–72 h post-transfection.
Excised inside-out patch-clamp experiments
Pipettes were made from soda lime glass microhematocrit tubes (Kimble) and had resistance of 1–3 megohms when filled with pipette solution. The bath and pipette solutions (KINT) contained (in mM):140 KCl, 10 HEPES, 1 EGTA (pH = 7.4 with KOH). Currents were recorded at a constant holding potential of −50 mV in the absence and presence of nucleotides, as indicated. Where included, free Mg2+ concentrations were maintained at 0.5 mM by supplementation of MgCl2, calculated using CaBuf (Katholieke Universiteit Leuven). Rapid solution exchange was attained using a Dynaflow Resolve perfusion chip (Cellectricon). Experiments were performed at 20–22 °C. KATP channel currents in solutions of varying nucleotide concentrations were normalized to the basal current in the absence of nucleotides, and dose-response data were fit with a four-parameter Hill fit according to Eq. 1, using the Data Solver Function in Microsoft Excel,
where current in KINT = Imax = 1; Imin is the normalized minimum current observed in high [ATP]; [X] refers to the concentration of ATP; IC50 is the concentration of half-maximal inhibition; and H denotes the Hill coefficient.
Data analyses
All statistical analyses were performed using Microsoft Excel or Prism (GraphPad). Significance values were calculated using One-way ANOVA test with Dunnett’s multiple comparisons. All values are expressed as mean ± SD.
Results
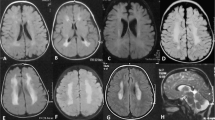
Subject 1 is a 28-year- old female [weight 52.4 kg (16th centile), height 172 cm (50th centile)], with lymphedema presents in both legs since childhood, and for which she was treated from the age of 14 years with bandages and compression stockings, intermittent pneumatic compression therapy and physiotherapy. At the age of 26 she was declared unfit for work because of her lymphedema. At that time, genetic testing with an next generation sequencing (NGS)-based lymphedema genepanel showed a variant in the ABCC9 gene (NM_005691.3): c.3164_3173delinsC, p.(Leu1055_Glu1058delinsPro; hereafter referred to as indel1055). This in frame deletion-insertion occurs in a highly conserved region of SUR2 TMD2, and was not present in the GnomAD population (https://gnomad.broadinstitute.org/). She was then referred to a clinical geneticist and retrospectively evaluated for other clinical features that might be consistent with a diagnosis of CS. She was born at term with a high birthweight of ~4.5 kg (>97th centile), with excess growth of dark hair (her parents had fair hair) on her scalp, forehead, back, and limbs (Fig. 1). Since childhood she has suffered from airway infections, asthma, diarrhea and stomach pain, and has undergone an operation for hallux valgus. Intellectual development was normal. She had laser therapy to remove the excess hair in her face and on her limbs. Eye examination (because of blurred vision) revealed dry eyes but also tortuosity of retinal vessels. On clinical examination at the age of 28, she had full lips and a broad nasal bridge, characteristic of CS, although cardiologic examination because of palpitations showed no abnormalities on ECG, echocardiography, or Holter monitoring. Subsequent genetic testing of her parents revealed that the ABCC9 variant was de novo. Based on these new data, the ABCC9 variant was re-classified as a likely pathogenic variant (ACMG score is PS2 [12]). As discussed below, functional analysis demonstrates GOF at the molecular level, confirming that the lymphedema in this case is part of the clinical and molecular diagnosis of CS.
Subject 2 is a 62 year-old female (weight 73.2 kg, height 166 cm). At the age of 46 she started treatment for lymphedema of the left leg with compression therapy and physiotherapy. Genetic testing with the same lymphedema gene panel identified a variant in ABCC9 (NM_005691.3): c.1256 T > C p.(lle419Thr) that affects a highly conserved amino acid in TMD1, and is present in only 1/250792 alleles in the GnomAD database. She was subsequently referred to a clinical geneticist to further evaluate for other features that might indicate a diagnosis of Cantu syndrome. However, apart from the lymphedema, and childhood asthma, she had a normal medical history, and clinical examination showed no excessive hairgrowth or relevant dysmorphic or other features, that could fit a diagnosis of CS. As discussed below, the variant also caused no GOF at the molecular level, suggesting that this variant is not pathogenic.
The indel1055 variant reduces ATP sensitivity of KATP channels
The human indel1055 variant (deletion of L1055 to E1058 and addition of Proline in hSUR2) is equivalent to deletion of L1051 to E1054 and addition of Proline in rat SUR2. I419 is located at the middle of the third transmembrane helix of SUR2 TMD1, and LTVE 1055-1058 is located in the middle of the second transmembrane helix of TMD2 (Fig. 2A, B). To examine the molecular consequences of these variants, each was introduced into rSUR2A, and inside-out patch-clamp recordings were performed on Cosm6 cells transiently transfected with mKir6.2 and WT or mutant rSUR2A, to measure channel activities (Fig. 3A–C).
A Expected locations of Isoleucine 416 (red) and LTVE 1051-1054 (blue) mapped onto the vascular KATP (rKir6.1/rSUR2B; Protein Data Bank code 7MIT) structure [17]. B Schematic representation of the position of I419 (human)/I416 (rat) and LTVE in SUR2. C Alignment of amino acid sequence of human SUR2 and rat SUR2 conducted with Cobalt: https://www.ncbi.nlm.nih.gov/tools/cobalt/re_cobalt.cgi.
A–C The response of recombinant Kir6.2/SUR2A channels to MgATP was determined from voltage-clamped patches (−50 mV), as shown in representative traces. Dashed lines denote zero-current. D Dose dependent curves fitted by Hill equation show ATP inhibition of the three types of SUR containing channels. E Scatter plots show data from individual experiments with mean IC50 ± S.D. Statistical significance is denoted by triple asterisks and defined as p < 0.001, and no significance is denoted by “ns” and defined as p ≥ 0.05 according to One-way ANOVA test with Dunnett’s multiple comparisons.
Wild type Kir6.2/SUR2A channels were inhibited by ATP with an IC50 of ~30 μM in the presence of physiological levels of Mg2+. ATP-sensitivity was markedly reduced (~3.5-fold) by the indel1055 variant (IC50 for ATP in the presence of Mg2+ was 107 ± 23 μM, Hill coefficient 1.2 ± 0.2; n = 5). However, no significant change in MgATP sensitivity was observed for the p.(Ile416Thr) variant (IC50 21 ± 12 μM, Hill coefficient 1.3 ± 0.4; n = 9) (Fig. 3D and E).
In addition to channel inhibition, which results from binding of ATP to the Kir6 subunits, Mg-nucleotides also activate KATP channels via an interaction with the SUR subunits [2]. While the above experiments show decreased sensitivity of the indel1055 construct to ATP (in the presence of Mg2+), they do not differentiate between enhanced Mg-nucleotide activation and ATP inhibition. Kir6.2/SUR2A-WT channels were also inhibited by ATP in the absence of Mg2+ with an IC50 of 27 ± 11 μM (Hill coefficient 0.9 ± 0.3; n = 6). Inhibitory ATP sensitivity was decreased ~2-fold by the indel1055 SUR2 variant (IC50 for ATP was 53 ± 30 μM, Hill coefficient 1.0 ± 0.2; n = 5), but again there was no significant effect of the p.(Ile416Thr) variant (IC50 was 24 ± 7 μM, Hill coefficient 1.0 ± 0.5; n = 9) (Fig. 4D and E).
A–C The response to ATP was determined from voltage-clamped patches (−50 mV), as shown in representative traces. Dashed lines denote zero-current. D Dose dependent curves fitted by Hill equation show ATP inhibition of the three types of SUR containing channels. E Scatter plots show data from individual experiments with mean IC50 ± S.D. Statistical significance is denoted by asterisk and defined as p < 0.05, and no significance is denoted by “ns” and defined as p ≥ 0.05 according to One-way ANOVA test with Dunnett’s multiple comparisons.
The ratio of IC50[MgATP]/IC50[ATP] can be used to estimate the effect of MgATP activation. For the wild type Kir6.2 + SUR2A channel, this value is 1.1, while for the indel1055 variant this value is around 2.1, suggesting that the indel1055 variant leads to both an increased activation by MgATP and a decrease of ATP inhibition. Comparing the ATP sensitivities of the indel1055 in the presence of Mg2+ with other identified GOF variants, we find that indel1055 (IC50 = 107 μM), is more severe than p.(Asp207Glu) (IC50 = 56 μM), p.(Tyr981Ser) (IC50 = 40 μM), p.(Gly985Glu) (IC50 = 48 μM), p.(Arg1150Trp) (IC50 = 46 μM) in rSUR2, similarly severe to p.(Met1056Ile) (IC50 = 92 μM) in rSUR2, and less severe than p.(Arg1150Gln) (IC50 = 164 μM) in rSUR2 and p.(Val64Met) (IC50 = 198 μM) or p.(Cys166Ser) in mKir6.2 (which are equivalent to p.(Val65Met) and p.(Cys176Ser) in Kir6.1, respectively).
Discussion
Gain-of-function effect of the lymphedema-associated SUR2 indel1055 variant
Lymphedema may result from reduced contractions of lymphatic smooth muscle cells [13], which are in turn highly sensitive to ABCC9- and KCNJ8-encoded KATP channels in the muscle [5]. Here, we report a case of idiopathic lymphedema that is causally associated with a GOF genetic variant in ABCC9. Functional characterization of this variant (Indel1055) reveals decreased sensitivity of recombinant KATP channels to ATP with or without the presence of Mg2+. Mechanistically, the variant causes a similar molecular effect to recognized Cantu Syndrome-associated SUR2 variants. The deleted amino acid sequence, LTVE1055-1058, is located in the second helix of TMD2 (Fig. 2A). This variant may therefore cause a shortening as well as a distortion of the helix due to the Proline insertion. A nearby variant p.(Met1060Ile) [10], which has been shown to be associated with CS, also increases MgATP activation. A second subject with idiopathic lymphedema without additional CS features also carried a rare coding variant, p.(Ile419Thr), in ABCC9. Although we cannot formally exclude the possibility that the variant might cause a GOF by increasing protein expression or trafficking in vivo, it did not alter recombinant channel activity and hence we conclude that the p.(Ile419Thr) variant is benign, and not causally related to the lymphedema.
Lessons for clinical lymphedema diagnosis and treatment
Retrospective evaluation showed that subject 1 (with the indel1055 variant) has a clinical history and features of CS, and we further show that this variant also causes gain-of-function at the molecular level, explaining the clinical features. It expands the molecular etiology of CS beyond previous reports, in which all reported variants have been simple missense mutations. The re-diagnosis from idiopathic lymphedema to CS indicates the need to consider other clinically relevant issues. Intriguingly, cardiac abnormalities were not reported in this subject, but, given the high penetrance of cardiac features in CS [14] together with the finding that the GOF in indel1055 is as severe as reported for other CS-associated variants with cardiac consequences, we would suggest that further cardiologic analysis may be warranted.
This case is a good example of how additional evidence in the form of molecular analyses and reverse phenotyping allowed clinical interpretation of a variant of unknown significance (VUS). Molecular phenotyping helped us to exclude causal association in subject 2, whilst allowing re-diagnosis of subject 1. Lymphedema is a clinical feature that usually presents during the teenage period, both in unexplained idiopathic cases and in CS [14]. Since our results support the hypothesis that lymphedema can be a first presentation of otherwise undiagnosed CS cases, clinicians should be aware of other features that could fit with a diagnosis of CS. Retrospective evaluation of neonatal history (including macrosomia, hypertrichosis, osteochondrodysplasia, and cardiomegaly) will suggest a clinical diagnosis of CS and should provoke futher genetic investigation. KCNJ8 and ABCC9 are two genes that deserve specific attention when requesting genetic testing for these cases. Given the recognized genetic basis of CS, these individuals could benefit from targeted therapy. Although data is still limited in humans with CS, treatment with KATP inhibitors such as glibenclamide can directly reverse molecular defects of CS and hence may improve lymphedema, in addition to other smooth muscle pathologies in CS [15, 16].
Data availability
The original data will be made available to any interested parties upon reasonable request.
References
Vignes S. [Lymphedema: From diagnosis to treatment]. Rev Med Interne. 2017;38:97–105.
Nichols CG. KATP channels as molecular sensors of cellular metabolism. Nature. 2006;440:471–6.
Mathias R, von der Weid PY. Involvement of the NO-cGMP-K(ATP) channel pathway in the mesenteric lymphatic pump dysfunction observed in the guinea pig model of TNBS-induced ileitis. Am J Physiol Gastrointest Liver Physiol. 2013;304:G623–34.
Telinius N, Kim S, Pilegaard H, Pahle E, Nielsen J, Hjortdal V, et al. The contribution of K(+) channels to human thoracic duct contractility. Am J Physiol Heart Circ Physiol. 2014;307:H33–43.
Davis MJ, Kim HJ, Zawieja SD, Castorena-Gonzalez JA, Gui P, Li M, et al. Kir6.1-dependent KATP channels in lymphatic smooth muscle and vessel dysfunction in mice with Kir6.1 gain-of-function. J Physiol. 2020;598:3107–27.
Cooper PE, McClenaghan C, Chen X, Stary-Weinzinger A, Nichols CG. Conserved functional consequences of disease-associated mutations in the slide helix of Kir6.1 and Kir6.2 subunits of the ATP-sensitive potassium channel. J Biol Chem. 2017;292:17387–98.
Cooper PE, Reutter H, Woelfle J, Engels H, Grange DK, van Haaften G, et al. Cantu syndrome resulting from activating mutation in the KCNJ8 gene. Hum Mutat. 2014;35:809–13.
Brownstein CA, Towne MC, Luquette LJ, Harris DJ, Marinakis NS, Meinecke P, et al. Mutation of KCNJ8 in a patient with Cantu syndrome with unique vascular abnormalities - support for the role of K(ATP) channels in this condition. Eur J Med Genet. 2013;56:678–82.
Harakalova M, van Harssel JJ, Terhal PA, van Lieshout S, Duran K, Renkens I, et al. Dominant missense mutations in ABCC9 cause Cantu syndrome. Nat Genet. 2012;44:793–6.
McClenaghan C, Hanson A, Sala-Rabanal M, Roessler HI, Josifova D, Grange DK, et al. Cantu syndrome-associated SUR2 (ABCC9) mutations in distinct structural domains result in KATP channel gain-of-function by differential mechanisms. J Biol Chem. 2018;293:2041–52.
Grange DK, Nichols CG, Singh GK: Cantu Syndrome; In Adam MP, Ardinger HH, Pagon RA et al. (eds). GeneReviews((R)). Seattle (WA), 1993.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Foster J, et al. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Scallan JP, Zawieja SD, Castorena-Gonzalez JA, Davis MJ. Lymphatic pumping: mechanics, mechanisms and malfunction. J Physiol. 2016;594:5749–68.
Grange DK, Roessler HI, McClenaghan C, Duran K, Shields K, Remedi MS, et al. Cantú syndrome: Findings from 74 patients in the International Cantú Syndrome Registry. Am J Med Genet C Semin Med Genet. 2019;181:658–81.
McClenaghan C, Huang Y, Yan Z, Harter TM, Halabi CM, Chalk R, et al. Glibenclamide reverses cardiovascular abnormalities of Cantu syndrome driven by KATP channel overactivity. J Clin Invest. 2020;130:1116–21.
York NW, Parker H, Xie Z, Tyus D, Waheed MA, Yan Z et al. Kir6.1- and SUR2-dependent KATP over-activity disrupts intestinal motility in murine models of Cantu Syndrome. JCI Insight. 2020;5:e141443.
Sung MW, Yang Z, Driggers CM, Patton BL, Mostofian B, Russo JD et al. Vascular KATP channel structural dynamics reveal regulatory mechanism by Mg-nucleotides. Proc Natl Acad Sci USA. 2021;118:e2109441118.
Funding
These studies were supported by R35 grant HL140024 from the NIH (to CGN), R21 grant HD103347 (to Dorothy K. Grange and CGN), K99 grant HL150277 (to CMC) and the E-Rare Joint Transnational Cantú Treat program I-2101-B26 (to GvH).
Author information
Authors and Affiliations
Contributions
Clinical characterization was carried out by IC, MA, MH. Molecular genetic analysis was carried out by IC, KD, GH. Mutagenesis and recombinant ion channel analysis was carried out by JG, CMC. The paper was initially drafted by JG and CGN. All authors gave final approval for publication.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
Genetic testing was performed as part of clinical diagnosis. Ethical approval was not required. Informed consent was obtained for the images presented in Fig. 1.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Gao, J., McClenaghan, C., Christiaans, I. et al. Lymphedema as first clinical presentation of Cantu Syndrome: reversed phenotyping after identification of gain-of-function variant in ABCC9. Eur J Hum Genet 31, 188–194 (2023). https://doi.org/10.1038/s41431-022-01210-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-022-01210-x
This article is cited by
-
The value of exomes across the ages
European Journal of Human Genetics (2023)