Abstract
Germline genome sequencing (GS) holds great promise for cancer prevention by identifying cancer risk and guiding prevention strategies, however research evidence is mixed regarding patient preferences for receiving GS results. The aim of this study was to discern preferences for return of results by cancer patients who have actually undergone GS. We conducted a mixed methods study with a cohort of cancer probands (n = 335) and their genetic relatives (n = 199) undergoing GS in a research setting. Both groups completed surveys when giving consent. A subset of participants (n = 40) completed semi-structured interviews. A significantly higher percentage of probands thought people would like to be informed about genetic conditions for which there is prevention or treatment that can change cancer risk compared to conditions for which there is no prevention or treatment (93% [311] versus 65% [216]; p < 0.001). Similar results were obtained for relatives (91% [180] versus 61% [121]; p < 0.001). Themes identified in the analysis of interviews were: (1) Recognised benefits of GS, (2) Balancing benefits with risks, (3) Uncertain results are perceived as unhelpful and (4) Competing obligations. While utility was an important discriminator in what was seen as valuable for this cohort, there was a variety of responses. In view of varied participant preferences regarding return of results, it is important to ensure patient understanding of test validity and identify individual choices at the time of consent to GS. The nature and value of the information, and a contextual understanding of researcher obligations should guide result return.
Similar content being viewed by others
Introduction
Germline genome sequencing (GS) is increasingly used to identify cancer risk and guide prevention [1]. While GS provides hope for reducing cancer morbidity and mortality, it also introduces ethical and implementation challenges [2].
GS can identify cancer variants that: (a) allow preventative intervention (clinically actionable), (b) have no preventative intervention available (non-actionable), although they can influence decisions relating to lifestyle, reproductive choices etc, (c) are of uncertain significance (VUS) or (d) are secondary to the diagnostic intention of testing (secondary findings). Pathogenic variants identified through patients’ GS will also have relevance to patients’ genetic relatives.
Research evidence is mixed regarding cancer patient preferences for receiving GS results. While some participants have reported wanting to know all results [3], others have declined testing, anticipating predictive knowledge as burdensome [4, 5]. Family concerns (particularly for parents), a previous cancer diagnosis and level of genomic knowledge are known to influence patient preferences [6].
Actionability of results has long been recognised as a criterion for returning GS results. Previous studies suggest that patients consider results with personal utility (such as for reproductive purposes) to be ‘actionable’, while researchers typically consider those with clinical utility to be ‘actionable’ [7, 8] and therefore worthy of return [9,10,11]. Research also suggests that a person’s preferences may be impacted by psychological factors, such as knowledge, worry about genetic risks [5], having genetically related children [12] and genetic causal beliefs [13], so that healthcare providers and patients may view the same results differently. These findings have implications for counselling prior to testing to manage patient expectations as well as for deciding which results to produce and return. It is therefore of great importance to understand how patients decide which results they wish to receive.
GS is still expensive in the community (~USD4000 on commencement of this study), and it is known that many patients who are interested in testing do not pursue it due to cost [14]. Adult GS is not publicly funded in Australia. To discern preferences for return of results by patients who are actually undergoing GS and to understand why they made this choice, we took the opportunity to assess preferences for return of results by patients with likely familial cancer and their genetic relatives who are actually undergoing GS as part of a research study, as these preferences are not studied outside of the hypothetical setting.
Subjects and methods
Participants
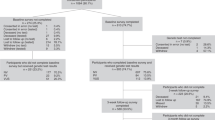
Participants were recruited to the Genetic Cancer Risk in the Young Study (RisC), which is being conducted at the Garvan Institute of Medical Research in Sydney, Australia. The primary aim of RisC is to identify clinically actionable, pathogenic gene variants that likely contribute to the development of cancer at an early age. RisC is recruiting probands with a likely genetic basis for their cancer diagnosis, and their genetic relatives, to undertake GS as part of the research protocol. The target population consists of [1]: adults with histologically confirmed malignancy under 40 years at diagnosis; OR having >1 primary cancer diagnosed <50 years; OR having >2 primary cancers at any age [2]; genetic relatives of RisC participants. All participants need to be able to read and speak English.
While testing is not initiated for clinical purposes, those participants found to carry a pathogenic cancer gene variant are referred to a genetic counsellor and offered a tailored risk-management plan through a subsequent study.
The Psychosocial Issues in Genomics in Oncology (PiGeOn) Project is a longitudinal, mixed methods sub-study of RisC, which aims to examine the psychosocial, behavioural and ethical impact of GS in this cohort. Patients consent to this study and the parent study at the same time. The consent process involved a verbal explanation of the study by a researcher, accompanied by written information. A subset of relatives gave consent with written information only (see Supplementary 1). The protocol for PiGeOn has been previously published [15]. A previous paper has also reported motivations for participation [16]. Both the RisC and PiGeOn studies were approved by the St Vincent’s Hospital Human Research Ethics Committee (HREC/16/SVH/24).
Procedure
All participants were asked to complete a survey at baseline, described elsewhere [15]. In brief, four measures assessed which genetic conditions participants considered ‘people’ would like to be informed about, for example known genetic conditions caused by single/multiple genes, and whether there was prevention or treatment available to alter risk. Demographic/disease details and consent data were collected by the parent study. Consent data consisted of participant decisions regarding which results they elected to receive in the actual RisC study. Options offered were: ‘gene variant that causes cancer’; and/or ‘incidental [secondary] finding that may be important to my health’. These options referred to cancer and non-cancer genes, respectively, both of which were assessed in the American College of Medical Genetics (ACMG) gene list.
For the qualitative sub-study, a subgroup of participants was asked to participate in semi-structured interviews after giving consent to GS, but before any genetic information was available. Purposive sampling was used to ensure heterogeneity in the demographics and cancer-related characteristics of the sample. Telephone interviews were scheduled within 1–2 weeks of consent. Interviews were conducted by one researcher (NB) and continued until data saturation. Interview questions are found in Supplementary 2.
Analysis
Descriptive statistical analysis of quantitative data was undertaken using IBM SPSS Statistics Version 25. Analysis of demographic/disease variables potentially associated with the desire to receive each type of result was performed using four multiple logistic regressions. The outcome variable was dichotomised as ‘yes, interested in receiving the result’, as indicated by participants’ ‘Yes’ response, vs. ‘not interested or unsure’, including ‘No’, ‘Maybe’, or ‘Don’t Know’. The predictor variables investigated included age; sex; education; urban versus rural place of residence; whether English was spoken in the home (proxy for culturally and linguistically diverse background); medical/science occupation; time since diagnosis; cancer incidence; and whether participants have first-degree genetic relatives with cancer diagnosis.
Interviews were recorded and transcribed verbatim. Thematic analysis [17] was used to code qualitative data. An initial coding tree was established and applied to further transcripts. New codes were developed iteratively as required and used to develop themes. Themes were developed and discussed by the research team, which comprised experts in medicine, psychology, genetic counselling, and bioethics. Differences were resolved through discussion, allowing rigour and reflexivity in the analysis. Triangulation of data was achieved through comparison of qualitative and quantitative results, and proband and relatives’ data, by framework analysis [18].
Results
The current analysis includes the first 534 survey respondents at baseline. Probands (n = 335) had a mean age of 41.7 years with 66% being female. Relatives (n = 199) had a mean age of 63.0 years with 59% being female. All probands and 24% of relatives had a previous cancer diagnosis. The survey response rate was 92% for both probands and relatives, and 100% for interviews (n = 40). See Table 1.
Quantitative results
With regard to their own GS results, almost all participants elected to be informed about gene variants that cause cancer (97% of probands and 96% of relatives), secondary findings deemed to be important to their health (96% of probands and relatives) and in the event of their death, for information important to health to be made known to relevant health professionals involved in their or other family members’ care (98% of probands and relatives).
With regard to the survey results, significantly more participants (311 (93%) probands and 180 (91%) relatives) thought people would like to be informed about genetic conditions for which there is prevention or treatment that can change risk versus no prevention or treatment (216 (65%) probands and 121 (61%) relatives), a difference of 28% [p < 0.001] for probands and 30% [p < 0.001] for relatives (Table 2). There was more uncertainty (‘Maybe’ or ‘Don’t know’ responses) amongst participants when thinking about whether people would like to be informed about genetic conditions for which there is no prevention or treatment (103 probands and 69 relatives) versus availability of prevention or treatment that can change risk (21 probands and 19 relatives).
More participants (303 (90%) probands and 183 (92%) relatives) thought people would like to be informed about genetic conditions for which there is treatment and lifestyle factors that can have a major impact on health versus a lower impact on health (285 (85%) probands and 174 (87%) relatives), a difference of 5% (p = 0.001) for probands and 5% (p = 0.012) for relatives (Table 2).
Multiple logistic regression demonstrated that, amongst probands, having a higher educational attainment and an English-speaking background were associated with thinking that people would desire to be informed about genetic conditions caused by one gene, for which there is prevention or treatment. For each category increase in education, odds increased by a factor of 1.39 (p = 0.038) for probands and 1.58 (p = 0.004) for relatives, and the odds of English-speaking probands considering these results desirable were 4.02 times that of probands from a non-English-speaking background (p = 0.005) (Supplementary Table 3).
Similarly, the odds of English-speaking probands thinking that people would wish to receive results about genetic conditions caused by multiple genes which could have a major impact on health for which prevention or treatment were available, were 2.41 times that of probands from a non English-speaking background (p = 0.041). Relatives with higher education were also more likely to consider these results desirable, with odds increasing by a factor of 1.59 (p = 0.007) per category increase in education (Supplementary Table 4), and also results about genetic conditions caused by many genes, which can have a lower impact on health: for every category increase in relatives’ education, the odds of considering that people would want to receive these results increased by a factor of 1.70 (p = 0.001) (Supplementary Table 5).
Conversely, probands with lower educational attainment were more likely to favour results about known genetic conditions caused by one gene, for which there is no prevention or treatment that can change risk. For every category increase in education level, the odds of thinking that people would like these results decreased by a factor of 0.77 (p = 0.006) (Supplementary Table 6). No other variables were significantly associated with the preference options listed in the survey.
Qualitative results
Responses of probands and their genetic relatives were combined, as themes were shared between groups. While most participants were clear on their preferences at the time of interview, some could not remember which results they had elected to receive, while others had ongoing decisional uncertainty, continuing to ponder whether and which results they should receive. Themes identified in the transcripts were: (1) Recognised benefits of GS, (2) Balancing benefits with risks, (3) Uncertain results are perceived as unhelpful and (4) Competing obligations. Quotes to illustrate each theme can be found in Table 3.
Recognised benefits of GS
This cohort, who had already given consent to germline GS, were enthusiastic about the benefits of testing with regards to all categories of results. Reflecting the quantitative results, interest in this information increased according to its perceived usefulness—whether it represented clinical, personal or individual utility (through answering questions about family cancers). Benefits were recognised from personal, family and community perspectives.
Personal benefits
Many participants wanted to receive all available results as a means to prevent future disease. As such, many participants felt that being tested through the research study was a privilege, since GS is not publicly funded in Australia. GS was also viewed as a way to reduce uncertainty about individual risk. Because the value of GS lay in its perceived utility, some participants did not want to receive results that were non-actionable.
Family benefits
Relatives, most of whom were parents, were particularly focussed on family reasons for participating in GS testing. Relatives had joined the study at the invitation of the proband (who was diagnosed with cancer). Probands were also aware of the familial implications and considered possible ways future generations could avoid disease. All positive results were therefore valued, even if the (potential) full benefit lay in the future.
Community benefit
GS results were also seen as contributing to the common good. Many participants were aware of the benefits they or their children had received from previous scientific research.
Balancing benefits with risks
Despite awareness of the benefits, the choice to undergo GS within the research study was seen as a balancing act between risks and benefits. Some participants had concerns about being overwhelmed by too much information. They desired information to be presented in an understandable framework, with accessible language.
The emotional cost of receiving difficult information was also recognised, with varying abilities of individuals to cope with knowledge of increased disease risk.
The most frequently articulated risk referred to increasing (individually risk rated) insurance premiums for products such as life insurance, although this interpretation was often erroneous, as all probands and some relatives would likely be declined such insurance anyway, due to their cancer diagnosis. Additionally, Australian insurers do not access health records directly but instead act on information disclosed by applicants and there is no obligation for individuals to disclose a relative’s genetic test result. (Health insurance is community risk rated in Australia).
In view of these risks, some participants envisaged themselves as gatekeepers, where they would calculate the risk/benefit score, and decide whether to notify relatives on these grounds.
Uncertain results are perceived as unhelpful
Participants were asked to imagine how they would feel if they received a VUS result (which was not an option for this study). Responses to the question varied, ranging from incomprehension (‘I don’t understand what you mean, either you are or aren’t at risk.’—Male relative, 59 years, no cancer), through to confidence of future certainty and clinical utility.
Participants with current cancer felt that their disease made a VUS irrelevant. The uncertainty integral to the experience of their disease trajectory meant that they did not feel that anything could significantly worsen their situation.
Due to the lack of perceived utility, many participants were not interested in receiving VUS results. Some participants thought it could actually be harmful as it could increase uncertainty, yet this was based on the flawed presumption that a VUS was necessarily pathogenic.
Competing obligations
Participants were asked whether they thought it was appropriate to participate in genetic research but choose not to receive results. Responses depended on whether participants prioritised individual or communal perspectives. Some participants accepted this scenario readily, generally attributing such a view to either altruism (participating solely to advance science), or the emotional inability to cope with challenging news. Others condemned this attitude in view of the potential of results to improve others’ health.
On being asked whether a choice not to receive results should be overridden if an actionable result was found, most participants hesitated. While a minority accepted the right of the individual to make such a choice, whatever its basis, most were reluctant to miss an opportunity to provide information of clinical utility that could have a significant health impact. Some respondents saw the return of such results as obligatory (and as such should be enforced by law) due to the perceived potential community benefit, warning of future legal action if disease developed as a result. However, the current limits of genomic science and subsequent complexity of the situation was also acknowledged.
Others suggested giving such a patient a further opportunity to deliberate and decide, or passing the results to a healthcare provider who could discuss it with the patient, such as by “dropping a few hints”. Some relatives felt that their age negated the need to be forewarned about potential disease.
Discussion
This study explored the views of cancer patients and their genetic relatives regarding which GS results they thought should be returned in the research context. We found that most participants expected that people would want to receive any results that they perceived to be useful (interpreted as actionable) and related to significant disease. The decision to receive results was calculated using a risk/benefit analysis, most thinking that benefits outweighed the risks, as has been found in previous research with cancer patients in the research setting [19].
The utility of genomic information was valued even if it was only potential future utility, as reported previously [20]. While utility is an accepted value by which to determine which results to return in the research setting, debate is ongoing over whether it is clinical utility, personal utility or individual utility that should be the standard [21]. The current cohort expressed willingness to receive results that had both personal (health related) and clinical utility. As such, if it is clinically indicated, practically feasible and if the patient agrees, it may be appropriate to return results of both personal and clinical utility. This could be said to respect patient best interests, as well as promote public support of genomic research [22].
It is noteworthy that a small number of respondents did not want any results returned. To put these responses in context, this was a research study and relatives, parents in particular, reported that their primary motivation was to help their children [16]. Most participants assumed such an attitude reflected an altruistic motivation for research participation. Previous studies have found that research participants who elected not to receive genomic findings may already have sufficient genomic information from previous testing or felt that information would not change their personal healthcare decision-making [23]. Some relatives in our cohort thought they were too old to worry about predictive GS results.
A number of interviewees were keen to be told all available information, assuming that receiving any kind of information will reduce uncertainty. This is common in both research and clinical contexts [23, 24]. There is no doubt that societal discourse has conditioned us to believe that information is good, as it implies control over our health. The rhetorical power of potential ‘life-saving’ GS encourages many patients to seek maximum information, and patients undergoing GS have reported a sense of empowerment [25], although high value placed by patients on GS has previously also been associated with overestimation of its validity [25]. However, in this context (research, where resources may be more limited) it is pertinent to ask whether it is appropriate to ask if patients want all results in view of the resources required to investigate all findings and report them, particularly if some results are of unknown significance, or if there is no plan to continue updating results once the study has concluded. At least, care needs to be taken during the consent process to manage patient expectations, especially due to the importance of the healthcare provider in influencing patient decisions to be tested [26]. Despite the support for the return of actionable secondary findings [9,10,11, 27], return of VUS and non-actionable secondary findings in translational research remains controversial, with debate in the literature about whether testing (and reporting) should be limited to the diagnostic question or whether there is an obligation to also screen for potentially clinically significant findings [28].
Actionable results were seen as more desirable by participants with greater educational attainment and who spoke English as their primary language. This could be related to better access to information, increased understanding of the significance of heightened cancer risk, and greater self-efficacy to act on results in these groups [29], and mirrors earlier findings that understanding predicts return of result preferences in cancer patients [5]. Numerous studies in the general population have found that genetic knowledge is lower amongst those with less education and low health literacy [30, 31], which could in turn impact choices regarding result return. One finding in variance to this trend was the greater perceived interest in non-actionable results seen in probands with lower educational attainment. We contend that this could be due to their misunderstanding of the limited utility of non-actionable results, therefore being more likely to believe these results would be valued by others. It will be important to recognise population needs and differences when implementing GS clinically, given that it is operating against a background where many from culturally and linguistically diverse groups are underserved in genomics provision (and indeed in the databases that support interpretation of results) [32]. Those who speak a language other than that being used in the study (or in clinic) are likely to need aids to facilitate understanding.
No other variables were associated with result preference, which is contrary to earlier studies [5, 12, 13] which identified a range of demographic and psychological predictors of preferences. For example, Guo et al. [12] and Kaphingst et al. [5] found that young women with breast cancer who had genetically related children were interested in carrier status regardless of actionability, whereas this variable was not associated with any result return preference in the current study. Our study included older participants (up to age 83) which may have impacted worry about children, although the majority of our sample were younger (median of 39 years). Forty-four percent of our sample were men however, and it is possible that men have a different perspective on their children’s future health risks than women.
Like earlier studies [5], we found no impact of clinical factors (such as time since diagnosis) on preferences. Kaphingst et al. [5] hypothesised that this may be because participants considered genomic results more informative regarding their general health than their cancer risk, and thus their cancer characteristics were not relevant to genomic decision-making. Indeed, these authors found that participants had diverse motivations for undertaking GS and learning their results, often unrelated to cancer [33]. While our participants frequently referred to cancer risk in interviews, this was generally with reference to the future, for either themselves or their children. Thus, their current cancer may have had less impact on their thinking and decision-making than their concerns about future risk.
There were mixed responses regarding the right of the individual to ‘not know’ their personal results from the study, even though they may benefit other patients in the future (through research). Clinically, genetics professionals have expressed support for the option for patients to decline to receive results [27], a position supported by the ACMG [34] as well as the National Pathology Accreditation Advisory Council in Australia [35]. While the choice to not engage with genetic conditions is well documented [36], there is some concern about potential implications, for both health professionals and other family members, of not passing on relevant information. The “right not to know” may, some argue, be better framed as a preference than a right; and may not hold in all circumstances [37]. Indeed, when the information could have critical health significance, the majority of respondents in this study supported overruling of individual choice. However, per our above comments, this view may be based on an at-present premature belief that genomic information can be life-saving. While the debate on the right not to know (especially in a research context) continues, it seems prudent to adopt a cautious approach.
Some interviewees were interested in receiving VUS results on the grounds that they may be of future interest. As our understanding of the medical significance of genetic data continues to evolve rapidly, so the implications of findings can change over time [38]. Developments in therapy may also alter treatment recommendations for genetically linked disease [39]. In the clinical context it has been shown that in 10–16% of VUS, explanatory variants were discovered through re-analysis 1–3 years later [28]. It is possible that there is a new role for a healthcare provider to take responsibility to regularly check for revised interpretations of variants. Certainly, annual reviews are now occurring in some laboratories [40]. Yet, apart from the difficulty in maintaining current contact information when the testing is done in a research context, this presents significant practical and ethical challenges. For example, concerns have been raised over ‘diverting the information deluge from physicians to patients’ [41]. It could also be argued there is no duty to recontact, as even clinicians do not have the responsibility for monitoring all aspects of patient health on an ongoing basis [42]. Limiting how long the obligation to return results should last for research projects has long been supported [43]. Guidance in this area is still emerging [44, 45]. In the clinical context, the genetic counselling appointment provides an opportunity to discuss the arrangements for review, for example patients might request referral to a cancer genetics service every 3–5 years.
Dynamic consent platforms have also been suggested as a way to coordinate and streamline long-term access to updated GS results [46]. The ongoing problem of primary physicians being under-skilled for interpreting genomic results [47] remains problematic if this role is given to them, as would be the resources required.
Some participants who did not want to receive their results personally were willing to have any relevant information passed on to their relatives or their health professionals. Thus reluctance to engage with results may reflect inability to cope with results. Those returning GS results need to check participant preferences to avoid communicating unwanted information, but also to ensure that relatives, who may benefit from learning the results, are not disadvantaged [48]. However, in view of differing interpretations of what makes results valuable to the individual, healthcare professionals should take care to clarify patient expectations prior to testing taking place, in both research and clinical contexts. This could include a staged return of results [49].
Limitations to this study include the inability to study the survey differences observed in preferences of those with lower education or from a non-English-speaking background in the interviews due to inadequate sample size. This study included a qualitative component that is not meant to be generalisable, and GS was conducted in a research setting. Other cohorts may respond differently.
Conclusion
The current study found that most participants in a research setting wished to receive GS information. While utility was an important discriminator in what was seen as valuable for this cohort, there were a variety of interpretations and responses regarding what types of results should be returned. In view of diverse opinions, it is important to identify individual choices and manage expectations during the GS consent process. However, as the perceived utility of GS can diminish after receiving results, [50] and in view of the known challenges in ensuring fully informed consent [20], we suggest that the nature and value of the information for both patients and their genetic relatives and a contextual understanding of researcher obligations, should guide GS result return in the research context.
Data availability
Additional data are available from the corresponding author on reasonable request.
References
Kurian AW, Hare EE, Mills MA, Kingham KE, McPherson L, Whittemore AS, et al. Clinical evaluation of a multiple-gene sequencing panel for hereditary cancer risk assessment. J Clin Oncol. 2014;32:2001–9.
Blanchard A. Mapping ethical and social aspects of cancer biomarkers. N Biotechnol. 2016;33:763–72.
Fenton AT, Anderson EC, Scharnetzki E, Reed K, Edelman E, Antov A, et al. Differences in cancer patients’ and clinicians’ preferences for disclosure of uncertain genomic tumor testing results. Patient Educ Couns. 2021;104:3–11.
Roberts JS, Gornick MC, Le LQ, Bartnik NJ, Zikmund-Fisher BJ, Chinnaiyan AM, et al. Next-generation sequencing in precision oncology: Patient understanding and expectations. Cancer Med. 2019;8:227–37.
Kaphingst KA, Ivanovich J, Lyons S, Biesecker B, Dresser R, Elrick A, et al. Preferences for learning different types of genome sequencing results among young breast cancer patients: role of psychological and clinical factors. Transl Behav Med. 2018;8:71–9.
Mackley MP, Fletcher B, Parker M, Watkins H, Ormondroyd E. Stakeholder views on secondary findings in whole-genome and whole-exome sequencing: a systematic review of quantitative and qualitative studies. Genet Med. 2017;19:283.
Kohler JN, Turbitt E, Biesecker BB. Personal utility in genomic testing: a systematic literature review. Eur J Hum Genet. 2017;25:662–8.
Cléophat JE, Dorval M, El Haffaf Z, Chiquette J, Collins S, Malo B, et al. Whether, when, how, and how much? General public’s and cancer patients’ views about the disclosure of genomic secondary findings. BMC Medical Genomics. 2021;14:167.
Machini K, Douglas J, Braxton A, Tsipis J, Kramer K. Genetic counselors’ views and experiences with the clinical integration of genome sequencing. J Genet Couns. 2014;23:496–505.
Yu J-H, Harrell TM, Jamal SM, Tabor HK, Bamshad MJ. Attitudes of genetics professionals toward the return of incidental results from exome and whole-genome sequencing. Am J Hum Genet. 2014;95:77–84.
Gray SW, Park ER, Najita J, Martins Y, Traeger L, Bair E, et al. Oncologists’ and cancer patients’ views on whole-exome sequencing and incidental findings: results from the CanSeq study. Genet Med. 2016;18:1011–9.
Guo S, Goodman M, Kaphingst K. Comparing preferences for return of genome sequencing results assessed with rating and ranking items. J Genet Couns. 2020;29:131.
Hong SJ, Biesecker B, Ivanovich J, Goodman M, Kaphingst KA. Factors affecting breast cancer patients’ need for genetic risk information: from information insufficiency to information need. J Genet Couns. 2019;28:543–57.
Best MC, Butow P, Jacobs C, Savard J, Biesecker B, Ballinger ML, et al. Who should access Germline Genome Sequencing? A mixed methods study of patient views. Clin Genet. 2020;97:329–37.
Best M, Newson AJ, Meiser B, Juraskova I, Goldstein D, Tucker K, et al. The PiGeOn project: protocol of a longitudinal study examining psychosocial and ethical issues and outcomes in germline genomic sequencing for cancer. BMC Cancer. 2018;18:454.
Bartley N, Best M, Jacobs C, Juraskova I, Newson AJ, Savard J, et al. Cancer patients’ views and understanding of genome sequencing: a qualitative study. J Med Genet. 2020. https://doi.org/10.1136/jmedgenet-2019-106410.
Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol. 2006;3:77–101.
Gale NK, Heath G, Cameron E, Rashid S, Redwood S. Using the framework method for the analysis of qualitative data in multi-disciplinary health research. BMC Med Res Methodol. 2013;13:117.
Hitch K, Joseph G, Guiltinan J, Kianmahd J, Youngblom J, Blanco A. Lynch syndrome patients’ views of and preferences for return of results following whole exome sequencing. J Genet Couns. 2014;23:539–51.
Facio FM, Eidem H, Fisher T, Brooks S, Linn A, Kaphingst KA, et al. Intentions to receive individual results from whole-genome sequencing among participants in the ClinSeq study. Eur J Hum Genet. 2013;21:261–5.
Beskow LM, Burke W. Offering individual genetic research results: context matters. Sci Transl Med. 2010;2:1–5.
Wolf SM, Crock BN, Van Ness B, Lawrenz F, Kahn JP, Beskow LM, et al. Managing incidental findings and research results in genomic research involving biobanks and archived data sets. Genet Med. 2012;14:361–84.
Loud JT, Bremer RC, Mai PL, Peters JA, Giri N, Stewart DR, et al. Research participant interest in primary, secondary, and incidental genomic findings. Genet Med. 2016;18:1218–25.
Bishop CL, Strong KA, Dimmock DP. Choices of incidental findings of individuals undergoing genome wide sequencing, a single center’s experience. Clin Genet. 2017;91:137–40.
Bombard Y, Rozmovits L, Trudeau M, Leighl N, Deal K, Marshall D. Patients’ perceptions of gene expression profiling in breast cancer treatment decisions. Curr Oncol. 2014;21:203–11.
Katz SJ, Bondarenko I, Ward KC, Hamilton AS, Morrow M, Kurian AW, et al. Association of attending surgeon with variation in the receipt of genetic testing after diagnosis of breast cancer. JAMA Surg. 2018;153:909–16.
Eckstein L, Garrett JR, Berkman BE. A framework for analyzing the ethics of disclosing genetic research findings. J Law Med Ethics. 2014;42:190–207.
Vos J, Asperen CJ, Oosterwijk JC, Menko FH, Collee MJ, Garcia EG, et al. The counselees’ self‐reported request for psychological help in genetic counseling for hereditary breast/ovarian cancer: not only psychopathology matters. Psychooncology. 2013;22:902–10.
Walker AP, Tucker DC, Hall MA, Lohman K, Harrison H, Harrison BW, et al. Results communication and patient education after screening for possible hemochromatosis and iron overload: experience from the HEIRS Study of a large ethnically and linguistically diverse group. Genet Med. 2007;9:778–91.
Lea DH, Kaphingst KA, Bowen D, Lipkus I, Hadley DW. Communicating genetic and genomic information: health literacy and numeracy considerations. Public Health Genom. 2011;14:279–89.
Kaphingst KA, Blanchard M, Milam L, Pokharel M, Elrick A, Goodman MS. Relationships between health literacy and genomics-related knowledge, self-efficacy, perceived importance, and communication in a medically underserved population. J Health Commun. 2016;21:58–68.
Landry LG, Ali N, Williams DR, Rehm HL, Bonham VL. Lack of diversity in genomic databases is a barrier to translating precision medicine research into practice. Health Aff. 2018;37:780–5.
Kaphingst KA, Ivanovich J, Biesecker BB, Dresser R, Seo J, Dressler LG, et al. Preferences for return of incidental findings from genome sequencing among women diagnosed with breast cancer at a young age. Clin Genet. 2016;89:378–84.
Kalia SS, Adelman K, Bale SJ, Chung WK, Eng C, Evans JP. Recommendations for reporting of secondary findings in clinical exome and genome sequencing, 2016 update (ACMG SF v2.0): a policy statement of the American College of Medical Genetics and Genomics. Genet Med. 2017;19:249–55.
National Pathology Accreditation Advisory Council. Requirements for human medical genome testing utilising massively parallel sequencing technologies. Canberra: Australian Government Department of Health; 2017. Contract No.: 11713.
Mendes Á, Paneque M, Clarke A, Sequeiros J. Choosing not to know: accounts of non-engagement with pre-symptomatic testing for Machado-Joseph disease. Eur J Hum Genet. 2019;27:353.
Dive L. From a right to a preference: rethinking the right to genomic ignorance. J Med Philos. 2021;46:605–29.
Stevens YA, Senner GD, Marchant GE. Physicians’ duty to recontact and update genetic advice. Per Med. 2017;14:367–74.
Giesbertz NA, van Harten WH, Bredenoord AL. A duty to recontact in genetics: context matters. Nat Rev Genet. 2019;20:371–2.
Couzin-Frankel J. Genomics breeds new legal questions. Science. 2019;364:521.
Knoppers B, Thorogood A, Zawati MN. Re-Learning the 3 R’s? Reinterpretation, recontact and return of genetic variants Genet Med. 2019;21:2401–2.
Hollands GJ, French DP, Griffin SJ, Prevost AT, Sutton S, King S, et al. The impact of communicating genetic risks of disease on risk-reducing health behaviour: systematic review with meta-analysis. BMJ. 2016;352:i1102.
Fabsitz RR, McGuire A, Sharp RR, Puggal M, Beskow LM, Biesecker LG, et al. Ethical and practical guidelines for reporting genetic research results to study participants: updated guidelines from a National Heart, Lung, and Blood Institute working group. Circ Cardiovasc Genet. 2010;3:574–80.
Bombard Y, Brothers KB, Fitzgerald-Butt S, Garrison NA, Jamal L, James CA, et al. The responsibility to recontact research participants after reinterpretation of genetic and genomic research results. Am J Hum Genet. 2019;104:578–95.
Carrieri D, Howard HC, Benjamin C, Clarke AJ, Dheensa S, Doheny S, et al. Recontacting patients in clinical genetics services: recommendations of the European Society of Human Genetics. Eur J Hum Genet. 2019;27:169–82.
Haga SB, Barry WT, Mills R, Ginsburg GS, Svetkey L, Sullivan J, et al. Public knowledge of and attitudes toward genetics and genetic testing. Genet Test Mol Biomark. 2013;17:327–35.
Chow-White P, Ha D, Laskin J. Knowledge, attitudes, and values among physicians working with clinical genomics: a survey of medical oncologists. Hum Resour Health. 2017;15:42.
Clift K, Macklin S, Halverson C, McCormick JB, Abu Dabrh AM, Hines S. Patients’ views on variants of uncertain significance across indications. J Commun Genet. 2020;11:139–45.
Martyn M, Kanga-Parabia A, Lynch E, James PA, Macciocca I, Trainer AH, et al. A novel approach to offering additional genomic findings—a protocol to test a two-step approach in the healthcare system. J Genet Couns. 2019;28:388–97.
Bradbury AR, Patrick-Miller L, Long J, Powers J, Stopfer J, Forman A, et al. Development of a tiered and binned genetic counseling model for informed consent in the era of multiplex testing for cancer susceptibility. Genet Med. 2015;17:485–92.
Acknowledgements
We thank the patients who participated in the PiGeOn Project. We thank David Goldstein, Mary-Anne Young, Judy Kirk, Kate Vines, and Richard Vines for their contributions to this study.
Funding
The PiGeOn Project is funded by a National Health and Medical Research Council (NHMRC) of Australia Project Grant (ID1124749). Investigators received the following support: PB: NHMRC Senior Principal Research Fellowship (APP1121630); MCB: Post-Doctoral Research Fellowship from the Cancer Institute of NSW (MB00352); MLB: Cancer Institute NSW Career Development Fellowship (CDF171109); BM: NHMRC Senior Research Fellowship Level B (ID1078523); DMT: NHMRC Principal Research Fellowship (APP1104364). Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
MCB, PB, JS, CJ, MLB, DTM, BB, KT, IJ, BM, TS and AJN were responsible for the conception and initial study design, and refining the study design. MCB, PB, NB and CEN were responsible for co-ordinating the acquisition of study data. GD and TS were responsible for statistical analysis. MCB, PB, JS, CJ, NB, MLB < BB, IJ, BM and AJN were involved in qualitative analysis. All authors were involved in drafting the paper and have read and approved the final paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval
This study was approved by the St Vincent’s Hospital Human Research Ethics Committee (HREC/16/SVH/24).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Best, M.C., Butow, P., Savard, J. et al. Preferences for return of germline genome sequencing results for cancer patients and their genetic relatives in a research setting. Eur J Hum Genet 30, 930–937 (2022). https://doi.org/10.1038/s41431-022-01069-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-022-01069-y