Abstract
Research on the perspectives of patients and parents regarding genetic testing and its implications has been performed mostly in Europe, Canada, the United States, Australia and New Zealand, even though genetic testing is becoming increasingly available worldwide. We aimed to fill this knowledge gap by exploring the experiences and needs of parents in the Dutch Caribbean who received a genetic diagnosis for the rare disease of their child. We conducted 23 semi-structured interviews with 30 parents of children diagnosed with various rare genetic diseases in Aruba, Bonaire and Curaçao (ABC-islands). Two researchers independently analyzed the interviews using a thematic approach. Main themes identified were: (1) getting a genetic diagnosis, (2) coping, support and perceived social stigma, (3) living on a small island, and (4) needs regarding genetic services. Our results indicate that, despite reported limitations regarding the availability of healthcare and support services, receiving a genetic diagnosis for their child was valuable for most participants. While some of the participants’ experiences with and attitudes towards the genetic diagnosis of their child were similar to those reported in previous studies, we identified a number of aspects that are more specifically related to this Dutch Caribbean setting. These include coping through faith and religion, social stigma and being the only one on the island with a specific genetic disorder. The results of this study and the provided recommendations may be useful when developing genetic testing and counseling services in similar settings.
Similar content being viewed by others
Introduction
Recent advances in genomic technologies have greatly increased the probability of obtaining a genetic diagnosis for early onset rare diseases. A genetic diagnosis can have several benefits for children and their families: it may end a long lasting search for a diagnosis, enable tailored management and surveillance, provide information about prognosis and recurrence risk and facilitate access to patient support groups, education, health and social care [1]. As the costs of genetic testing are decreasing rapidly, genetic services are becoming increasingly available worldwide [2]. In Europe, Canada, the United States, Australia and New Zealand the perspectives and experiences of parents who received a genetic diagnosis for their child have been studied extensively [3,4,5,6,7,8,9,10,11,12]. However, little is known about the views of patients and parents in other parts of the world, even though there may be major differences due to different healthcare systems and unique economic, religious and cultural contexts. For example, access to therapy and support services might be limited [13] and options for future pregnancies, such as preimplantation genetic diagnosis, invasive prenatal diagnosis and termination of pregnancy, might be unavailable, illegal or unaccepted [14]. This could, in turn, negatively affect the value of receiving a genetic diagnosis. A recent systematic review on clinical genetic testing and counseling in low- and middle-income countries identified several ethical, social, and cultural issues that should be considered when (further) developing genetic services in these countries [2]. However, the majority of the studies included in this review was of a quantitative nature and the authors addressed the need for more qualitative studies, in order to gain more insight into the psychosocial and behavioral issues that could influence implementation and uptake of genetic services [2].
In 2011, a joint pediatric-genetics clinic with a visiting Dutch clinical geneticist was established to improve diagnostic opportunities for children with undiagnosed rare diseases in the Dutch Caribbean. Although the islands of the Dutch Caribbean are high-income economies, as defined by the World Bank [15], they face specific economic and healthcare challenges, due to their small size and relative remoteness. Because of the novelty of the local genetic service established on these islands and the aforementioned knowledge gap, we conducted a qualitative study to explore parents’ experiences with obtaining a genetic diagnosis for their child, their attitudes towards the genetic diagnosis and their needs regarding genetic services. The results of this study may provide useful insights that can contribute to improving genetic care for the Dutch Caribbean population. In addition, the findings can be used when establishing or improving genetic services in other countries.
Methods
Setting
The Dutch Caribbean consists of six islands that are part of the Kingdom of the Netherlands. Three of these islands (Aruba, Bonaire and Curaçao) are located in the southern Caribbean Sea just off the coast of Venezuela. Collectively, they are referred to as the ABC-islands. The population of the ABC-islands is of mixed ancestry and the majority of the population is religious (mainly Roman Catholic). Papiamento is the most widely spoken language, but most people speak Dutch, English and/or Spanish as well.
The health systems of the ABC-islands largely mirror that of the Netherlands, with a general practitioner as the first point of contact. Secondary care is provided at hospitals and private clinics. Residents are entitled to (basic) health insurance, which is paid through income tax. Highly specialized care that is not available on the island is provided through medical transfers to hospitals overseas. For example, there is no neonatal intensive care unit (NICU) in Bonaire and Aruba and patients from these islands are thus transferred by air ambulance to Curacao or Colombia. Visiting medical specialists provide additional specialized care, for example, a pediatric neurologist who visits Curaçao once a year to evaluate complex patients. Until 2011, there was no local clinical genetics service in the Dutch Caribbean, and because of this a joint pediatric-genetics clinic was established. Since then, a Dutch clinical geneticist (MvH) visits the pediatric departments of the local hospitals of the ABC-islands twice a year to evaluate patients suspected of having a genetic disorder. Patients are referred to the clinical geneticist by their pediatrician, who is usually present during the genetic consultation. Medical and family history are obtained and a dysmorphologic physical examination is performed. If indicated, blood samples are sent to the Netherlands for genetic testing to establish or confirm a diagnosis. If a genetic diagnosis is established, patients and their parents receive counseling during a follow-up visit with the clinical geneticist. During this visit the cause and implications of the genetic diagnosis are explained and, if applicable, recurrence risk and risks for family members are discussed. As the clinical geneticist visits only twice a year, the results of genetic testing are sometimes already communicated to parents by the pediatrician and parents receive additional counseling during the next visit of the clinical geneticist. A more extensive description of the Dutch Caribbean, its healthcare systems and the established clinical genetics service has been published elsewhere [16].
Study design
A qualitative study with semi-structured interviews was conducted with parents living in Aruba, Bonaire or Curaçao, whose child was diagnosed with a rare genetic disease. The interviews took place at local hospitals on all three islands (Dr. Horacio E. Oduber Hospital, Hospital San Francisco [Fundashon Mariadal] and Sint Elisabeth Hospital) in November 2018 and April/May 2019. Written informed consent for participating in the study was obtained from each participant.
Participants
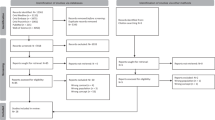
From the start of the genetic service program (November 2011) until November 2018, a total of 113 children (age at first visit <18 years) that were referred to the clinical genetics outpatient clinics in Aruba, Bonaire and Curaçao received a molecularly confirmed genetic diagnosis. A few of them had already received the genetic diagnosis elsewhere and were referred for (additional) genetic counseling. For this study, we included parents who [1] received a genetically confirmed diagnosis for the rare disease of their child at least six months ago, but no longer than five years ago, and [2] were able to speak Dutch and/or English. Initially, parents who spoke Spanish were also included. However, after the first interview in Spanish it became clear that a higher level of Spanish proficiency of the interviewer was needed to conduct an interview of good quality. Therefore, this interview was excluded and subsequently only parents who spoke Dutch and/or English were included.
Parents who met the inclusion criteria were invited at random for an interview. Participants were recruited until no new themes or perspectives arose during the interviews. The parents of 35 children had been invited by telephone to participate in the study, of which 11 families canceled the interview appointment later or did not show up. A total of 30 parents of 24 children (including one twin) participated.
Data collection
A semi-structured interview guide was developed by a clinical researcher (EV), together with a health scientist (LH) and clinical geneticist (MvH). Topics that were addressed included: [1] impact and consequences of receiving a genetic diagnosis [2], reproductive decisions/intentions [3], satisfaction with genetic counseling and services, and [4] (health)care needs and future expectations (see Supplementary 1 for the complete interview guide). At the end of the interview, additional questions were asked to capture the sociodemographic characteristics.
The interviews were conducted by a clinical researcher from the Netherlands (EV). She had met 11 of the 30 participants prior to the interviews, when attending the consultations of the clinical genetics outpatient clinic, in which she played an observational role. The interviews lasted between 16 and 69 min, with a median duration of 38 min. After the interview, participants received a financial compensation (the local equivalent of 10 euro) for their participation and travel costs.
Data analysis
All interviews were audio recorded, after which they were transcribed verbatim and anonymized. Thematic analysis was performed as described by Braun and Clarke [17]. The software program MaxQDA 2020 was used to conduct thematic analysis. The transcripts were read repeatedly and coded independently by two researchers (EV and LvdH). Any discrepancies between the two researchers were discussed until consensus was reached. Based on coding analysis, main and subthemes were identified. Final themes were discussed with three researchers (EV, LvdH and LH). Exemplar quotes were translated into English and presented in the results section.
Results
A total of 23 interviews including 30 participants were conducted. Table 1 shows characteristics of the participants and their children. Seven interviews took place with both parents and 16 with one parent. The median age of the participants was 39 years (range 28–46 years) and 70% was female. Children had a median age of seven years (range 11 months – 20 years) at the moment the interviews were conducted, with a median age at genetic diagnosis of six years (range 2 months – 17 years). Eleven out of the 24 children (46%) had intellectual disability (ID). Monogenic ID syndromes were the most frequently established diagnoses. Most disorders were autosomal dominant and occurred de novo or inheritance was not determined because of financial restrictions or unavailable parental samples. To protect the privacy of the participants we do not include the specific diagnoses in this paper.
Four main themes were identified: [1] Getting a genetic diagnosis [2], Coping, support and perceived social stigma [3], Living on a small island, and [4] Needs regarding genetic services. Illustrative quotations from the interviews are presented in Table 2.
Theme 1: Getting a genetic diagnosis
Need for a diagnosis
Most participants reported that after realizing their child had ‘something’, they wanted to find out what it was and where it came from. Some of them already visited various healthcare professionals for this reason and were actively looking for (more) help (Table 2, quote 1.1). Participants especially wanted to know what they could expect for the future and whether they could do anything to improve the health and/or development of their child. A few participants, however, did not think their child had (many) health problems and agreed to genetic testing because it was advised by the pediatrician. One participant even mentioned he was not aware that genetic testing had been requested.
Impact of the genetic diagnosis
Despite initial feelings of shock, worry and disappointment after receiving the genetic diagnosis, many participants were relieved to get an explanation for the problems of their child. It brought them closure and acceptance (Table 2, quote 1.2). Other positive aspects that participants reported were feeling prepared for the future and being able to get in contact with other (parents of) patients with the same disorder. Additionally, some participants mentioned that the genetic diagnosis enabled them to make informed reproductive choices. For example, one participant could finally pursue her wish to have another child after hearing that the recurrence risk was negligible. Other participants decided not to have another child or were still contemplating it because of the recurrence risk (Table 2, quote 1.3). Some participants reported changes in clinical management through screening for additional medical problems related to the condition or through support services. Finally, a few participants reported that the diagnosis did not change anything, mainly because they were already doing as much as possible to guide and stimulate the development of their child.
While many participants believed the genetic diagnosis was beneficial, the diagnosis also caused participants to worry about possible future problems that might arise as part of the diagnosed genetic syndrome. Although for some participants it was a relief to know that the condition was genetic and not caused by something they did (Table 2, quote 1.4), others felt guilty because it was genetic. For example, one participant felt guilty about being a carrier of the autosomal recessive disorder that her child was diagnosed with (Table 2, quote 1.5).
Theme 2: Coping, support and perceived social stigma
Acceptance, positive reframing and a focus on being normal
Many participants expressed that the genetic diagnosis and the associated health problems were just something they had to accept and live with. Some participants said they already accepted that they had a ‘special’ child before the genetic diagnosis (Table 2, quote 2.1). However, other participants found it hard to accept that their child had a genetic syndrome, mainly because their other children were healthy and/or no one in the family had the same disorder. One participant also mentioned that it was difficult to accept the diagnosis, because she did not see anything abnormal in the appearance of her child (Table 2, quote 2.2). Several participants coped with the genetic diagnosis and the problems of their child by focusing on the positive sides and putting things in perspective (Table 2, quote 2.3). For some participants it was important to treat their child as normal as possible and let them live a normal life. One couple even trivialized the medical problems of their child, as well as the genetic diagnosis, and said their child was healthy (Table 2, quote 2.4).
Coping through faith and religion
A coping mechanism for several participants was their faith in God. It helped them to accept the genetic disorder of their child, because they believed it was something given to them by God, and it brought them strength and hope for the future (Table 2, quote 2.5). Also, some participants felt emotionally supported by their church community. At the same time, one participant felt conflicted between science and religion in her hope for her child to be cured (Table 2, quote 2.6). Another participant did not believe his child had a genetic syndrome, as he felt that this was something that was in the hands of God (Table 2, quote 2.7).
Family and peer support
Besides faith and religion, another source of support for some participants was their family. Participants received emotional support from their family members, mostly parents, as well as help with childcare. Furthermore, a few participants connected online with other parents of a child with the same disorder: this made them feel supported because these parents understood what they were going through (Table 2, quote 2.8).
Perceived social stigma
Several participants stated that in general, children with disabilities are not fully accepted by their society. They described that these children are not really part of the local community and not visible in everyday life (Table 2, quote 2.9). One participant mentioned that even her own husband never accepted the disorder of their child (Table 2, quote 2.10). A few participants discussed the possible reasons for this stigma. They explained that since the communities on these islands are relatively small, there is a lot of gossip which might lead to feelings of shame and fear of getting stigmatized. Two participants felt that in the Netherlands, where one of them had lived, people are more accepting towards people with disabilities. For one participant fear of stigma was a reason not to tell anyone besides her close family about her child’s genetic diagnosis (Table 2, quote 2.11). Another participant only recently told her mother about the genetic diagnosis, because she did not want her child to be treated differently. However, some participants tried to oppose the stigma: they described that they did not hide their child (with a visible disorder), but instead took him/her outside of the house as much as possible. Some participants expressed their worries about the limited opportunities for their child to find a future internship or job because of this stigma. (Table 2, quote 2.12).
A few participants felt upset or irritated by certain beliefs of other people regarding the cause or cure of the disease of their child. For example, one participant got advicefrom other people about how to cure her child, including praying to God, and giving cannabis oil and a certain type of milk to her child. Another couple mentioned that people believe that kidney diseases are caused by fright (Table 2, quote 2.13).
Theme 3: Living on a small island
Availability and quality of healthcare, support services and education
All participants indicated that they had health insurance and that almost all medical expenses were covered. Many participants said that they received sufficient care and were satisfied with the quality of their healthcare providers. However, some participants indicated that certain care is missing or not easily accessible on their island, such as subspecialized pediatric care. Several participants had to go abroad to receive specialized medical care and a few participants went abroad on their own initiative, for example to get a second opinion. Services such as physical and speech therapy are available, but some participants indicated that a lot of self-initiative was needed to obtain these services and would have liked them to be provided by, for example, school (Table 2, quote 3.1). Apart from this, some participants who had a child with intellectual disability found it difficult to get appropriate education for their child and were not satisfied with the availability and quality of special education. They experienced a lack of opportunities and facilities to support their child in general (Table 2, quote 3.2). A few children were living in a (day)care institution. Their parents had different feelings about that: One couple was very negative about the circumstances in the care institution, while a participant from another island was satisfied with the provided care.
Being the only one on the island
Some participants expressed that they would like to get in touch with other parents who have a child with the same genetic disorder: they wanted to share experiences and get information and advice. However, because of the small size of the islands and the rareness of the disorder it was difficult to find these parents (Table 2, quote 3.3). Consequently, the only option for most participants was to digitally connect with other parents. Although this worked for a few participants, for others it created a barrier: they did not know where to start, tried but did not succeed or preferred meeting other parents in person.
Theme 4: Needs regarding genetic services
Satisfaction with genetic services
Most participants were satisfied with the provided genetic services, although a few participants felt that it took too long before they received the genetic test results. One participant mentioned she was glad this service was available on the island, instead of having to go abroad for this (Table 2, quote 4.1). If they could go back in time, almost everyone would choose again to do genetic testing. Many participants would have wanted to get their child’s genetic diagnosis at a younger age. Participants expected that this would have had several consequences, such as getting appropriate help sooner, taking preventive measures and spending less time in uncertainty. In addition, one couple mentioned that if they would have known they were both carriers of a genetic condition, they could have searched for a way to have a healthy child (Table 2, quote 4.2). On the other hand, some participants felt they received the diagnosis at the right moment and others were unsure about the timing or felt that it did not really matter. Only one participant indicated that he would have liked to wait with genetic testing until his daughter was a bit older.
Information needs
In most cases, the genetic diagnosis had been disclosed by the clinical geneticist; in some cases this was done by the pediatrician. Several participants indicated they were satisfied with the genetic counseling they received. They felt that the explanation was clear and that they had enough possibilities to ask questions. However, a few indicated they were too shocked to understand all the information and to ask questions. Others felt that too much medical jargon was used, making it difficult to understand the information. One participant mentioned that her Dutch was not that good and that she would have liked to have someone to translate during the consultation. When asked about it, many participants said they searched the internet for more information, including two participants who specifically mentioned that they did this because the information they received during counseling was incomprehensible or insufficient.
Topics that participants would have liked to get more information on include recurrence risk and reproductive options (for themselves or their child) (Table 2, quote 4.3). A few participants still had questions regarding the genetic diagnosis: they did not fully comprehend why their child had this genetic disorder or did not completely understand the result of the genetic test. One participant even did not know her child had a genetic diagnosis. One participant, who received the diagnosis several years ago, mentioned that she would like to get an update on what is known about the genetic disorder and if there are any new advices for disease management.
Discussion
This is the first study in the Dutch Caribbean that explores the experiences of parents who received a genetic diagnosis for their child. The majority of the participants valued getting a genetic diagnosis and would, in retrospect, choose again to get genetic testing for their child. The consequences of a genetic diagnosis reported by our participants largely correspond with those reported by patients and parents in previous studies. These include benefits such as a sense of closure, reduced guilt, feeling prepared for the future, access to support groups and being able to make informed reproductive choices [4,5,6,7,8,9,10]. Negative consequences include worries about the future and feeling guilty because of passing on a disease/gene to their children [7, 11, 12]. Interestingly, making an informed reproductive choice was mentioned as a benefit by our participants despite limited reproductive options. This suggests that even in situations where reproductive technologies, such as preimplantation genetic testing or invasive prenatal diagnosis are unavailable or difficult to access, parents still value information about recurrence risk and can still make an informed reproductive choice. Only some of our participants reported changes in clinical management following the diagnosis. This might be related to reported difficulties with accessing support services and lack of specialized medical care in the Dutch Caribbean. However, a lack of medical utility has been reported in previous studies as well [4].
Even though many of the experiences and views that our participants shared are similar to those reported previously in literature, some findings seem to be more specifically related to the Dutch Caribbean setting. First of all, apart from acceptance, positive reframing and a focus on being normal, finding comfort in faith and religion was an important coping mechanism for several participants. This is in line with qualitative research on sickle cell disease in Jamaica, another Caribbean island [18]. A systematic review on genetic testing for cancer risk among ethnic minority groups described that spirituality and God were not a barrier to genetic testing, but a way of seeking guidance and support [19]. This is in accordance with our findings, although for one participant religion played a role in being less accepting towards the genetic diagnosis. It should be noted that finding comfort in faith and religion is a well-known coping mechanism in response to crises [20] and not unique to this specific setting. However, it is likely to be a more prominent coping style in areas where a high percentage of the population is religious, such as the Dutch Caribbean.
Secondly, several participants described that they felt that children with disabilities are not fully accepted by society, not really part of the community and not visible in everyday life, indicating a social stigma. Some participants tried to protect their child from this stigma by not sharing the genetic diagnosis or only sharing it with close family and friends. Concerns about stigma associated with having a (genetic) disease and the related wish not to be treated differently have also been identified in literature reviews of genetic testing in ethnic minority groups [19] and low- and middle-income countries [2]. Although social stigma associated with rare (genetic) diseases and health-related stigma in general are global phenomena [21,22,23], the burden of stigma may be higher for people in low-income and less developed settings [24, 25]. A few participants in our study suggested that social stigma was related to the small size of their communities. Indeed, there is evidence that people living in small (rural) communities experience greater health-related stigma compared to those living in urban areas [26, 27].
Thirdly, participants’ experience with receiving a genetic diagnosis was influenced by the relative isolation of living on a small island. Although participants were generally satisfied with the available healthcare, some indicated that certain specialized care was lacking on their island. In addition, patients reported that support services were not easily accessible and that there were insufficient opportunities and facilities for children with intellectual disability. Moreover, their child was (almost always) the only one on the island with a specific genetic condition. This complicated the possibility to find peer support. Although some participants managed to connect with other parents online, others did not succeed in this or preferred meeting face-to-face. Regardless of country, for patients with (very) rare genetic diseases it may always be difficult to connect with peers [10, 28]. However, in many countries opportunities are created for (parents of) patients with rare diseases to connect with peers in person, in order to share experiences, learn from each other, and to give and receive emotional support [29, 30]. In the Dutch Caribbean, given the small population sizes of these islands, even for more common genetic diseases there may be only one or two patients with the same syndrome. This decreases the possibility of finding peers and may increase feelings of isolation, which could be a problem in other small, isolated or rural communities as well [31].
Another finding of this study is the need of participants for more information regarding the genetic diagnosis. Consistent with previous studies [3], participants’ understanding of the provided information was sometimes impaired by the use of too much medical jargon and feelings of shock after receiving the diagnosis. Culturally appropriate educational material explaining the diagnosis as well as general concepts of genetics and inheritance, using local language and illustrations may be a valuable instrument to improve patient knowledge [32,33,34]. Additional follow-up visits with the clinical geneticist may be useful to further address any questions that patients may have and to review the provided information. In particular, telemedicine may improve availability of such follow-up visits in remote areas [35, 36]. Furthermore, local clinicians should receive (additional) medical genetics education to address questions that patients may have during regular follow-up visits. Visiting medical specialists including clinical geneticists may contribute to medical genetics education through seminars and clinical teaching rounds [37].
One of the limitations of this study is that parents who did not speak English or Dutch were not included, possibly creating a selection bias. In addition, although all participants were proficient in Dutch or English, these languages were not the mother tongue of most participants and thus there was still a language barrier in some of the interviews. These participants may have misunderstood questions and may not have been able to express themselves fully. A recommendation for further research would be to have an interviewer that is also able to speak the local language (Papiamento). Furthermore, the interviewer had previously met some of the participants, when attending the consultations of the clinical genetics outpatient clinic. Although she played only an observing role, participants who recognized her may have felt uncomfortable with fully disclosing their thoughts. Lastly, participants had received the genetic diagnosis up to five years ago, which may have resulted in recall bias regarding certain topics, such as the response to diagnosis and experiences with genetic services.
In conclusion, this study provides valuable insights into the experiences and needs of parents in the Dutch Caribbean who received a genetic diagnosis for their child. Some of the experiences and views reported by our participants, such as the benefits and drawbacks of a genetic diagnosis, are similar to those identified in previous studies. Aspects such as coping style and living with a child with a genetic disorder are more strongly influenced by the specific Dutch Caribbean context. The findings of this study can be used to improve the genetic service on these islands, but also to inform genetic services that are being developed in similar settings. Finally, although Aruba, Bonaire and Curaçao face several economic and healthcare challenges, these islands have relatively good economies and are classified as high-income countries. As genetic testing is becoming more widespread available, further research in low- and middle-income countries is required to assess the needs regarding genetic counseling and testing, in order to provide appropriate and culturally tailored genetic services.
Data availability
The datasets generated and analyzed during the current study are available from the corresponding author on reasonable request.
References
Wright CF, FitzPatrick DR, Firth HV. Paediatric genomics: diagnosing rare disease in children. Nat Rev Genet. 2018;19:253–68.
Zhong A, Darren B, Loiseau B, He LQB, Chang T, Hill J, et al. Ethical, social, and cultural issues related to clinical genetic testing and counseling in low- and middle-income countries: a systematic review. Genet Med. 2021;23:2270–80.
Ashtiani S, Makela N, Carrion P, Austin J. Parents’ experiences of receiving their child’s genetic diagnosis: a qualitative study to inform clinical genetics practice. Am J Med Genet Part A. 2014;164a:1496–502.
Lim Q, McGill BC, Quinn VF, Tucker KM, Mizrahi D, Patenaude AF, et al. Parents’ attitudes toward genetic testing of children for health conditions: a systematic review. Clin Genet. 2017;92:569–78.
Carmichael N, Tsipis J, Windmueller G, Mandel L, Estrella E. “Is it going to hurt?”: the impact of the diagnostic odyssey on children and their families. J Genet Couns. 2015;24:325–35.
Makela NL, Birch PH, Friedman JM, Marra CA. Parental perceived value of a diagnosis for intellectual disability (ID): a qualitative comparison of families with and without a diagnosis for their child’s ID. Am J Med Genet Part A. 2009;149a:2393–402.
Chassagne A, Pélissier A, Houdayer F, Cretin E, Gautier E, Salvi D, et al. Exome sequencing in clinical settings: preferences and experiences of parents of children with rare diseases (SEQUAPRE study). Eur J Hum Genet. 2019;27:701–10.
Halverson CM, Clift KE, McCormick JB. Was it worth it? Patients’ perspectives on the perceived value of genomic-based individualized medicine. J Community Genet. 2016;7:145–52.
Esquivel-Sada D, Nguyen MT. Diagnosis of rare diseases under focus: impacts for Canadian patients. J Community Genet. 2018;9:37–50.
Rosell AM, Pena LD, Schoch K, Spillmann R, Sullivan J, Hooper SR, et al. Not the end of the Odyssey: parental perceptions of whole exome sequencing (WES) in pediatric undiagnosed disorders. J Genet Couns. 2016;25:1019–31.
Krabbenborg L, Vissers LE, Schieving J, Kleefstra T, Kamsteeg EJ, Veltman JA, et al. Understanding the psychosocial effects of WES test results on parents of children with rare diseases. J Genet Couns. 2016;25:1207–14.
McAllister M, Davies L, Payne K, Nicholls S, Donnai D, MacLeod R. The emotional effects of genetic diseases: implications for clinical genetics. Am J Med Genet Part A. 2007;143a:2651–61.
Choudhury MC, Saberwal G. The role of patient organizations in the rare disease ecosystem in India: an interview based study. Orphanet J Rare Dis. 2019;14:117.
Penchaszadeh VB. Ethical issues in genetics and public health in Latin America with a focus on Argentina. J Community Genet. 2015;6:223–30.
The World Bank. High income. https://data.worldbank.org/income-level/high-income?view=chart.
Verberne EA, Ecury-Goossen GM, Manshande ME, Ponson-Wever M, de Vroomen M, Tilanus M, et al. Clinical and community genetics services in the Dutch Caribbean. J Community Genet. 2021;12:497–501.
Braun V, Clarke V. Using thematic analysis in psychology. Qualitative Res Psychol. 2006;3:77–101.
Anderson M, Asnani M. “You just have to live with it”: coping with sickle cell disease in Jamaica. Qual Health Res. 2013;23:655–64.
Hann KEJ, Freeman M, Fraser L, Waller J, Sanderson SC, Rahman B, et al. Awareness, knowledge, perceptions, and attitudes towards genetic testing for cancer risk among ethnic minority groups: a systematic review. BMC Public Health. 2017;17:503.
Pargament KI The psychology of religion and coping: theory, research, practice. New York: Guilford Press; 1997.
Birbeck GL, Bond V, Earnshaw V, El-Nasoor ML. Advancing health equity through cross-cutting approaches to health-related stigma. BMC Med. 2019;17:40.
Rai SS, Syurina EV, Peters RMH, Putri AI, Zweekhorst MBM. Non-communicable diseases-related stigma: a mixed-methods systematic review. Int J Environ Res Public Health. 2020;17:6657.
von der Lippe C, Diesen PS, Feragen KB. Living with a rare disorder: a systematic review of the qualitative literature. Mol Genet Genom Med. 2017;5:758–73.
World Health Organization. Epilepsy: a public health imperative. Geneva: World Health Organization; 2019.
Kemp CG, Jarrett BA, Kwon C-S, Song L, Jetté N, Sapag JC, et al. Implementation science and stigma reduction interventions in low- and middle-income countries: a systematic review. BMC Med. 2019;17:6.
Kalichman S, Katner H, Banas E, Kalichman M. Population density and AIDS-related stigma in large-urban, small-urban, and rural communities of the Southeastern USA. Prev Sci. 2017;18:517–25.
Elliot VL, Morgan D, Kosteniuk J, Froehlich Chow A, Bayly M. Health-related stigma of noncommunicable neurological disease in rural adult populations: a scoping review. Health Soc Care Community. 2019;27:e158–e88.
Germeni E, Vallini I, Bianchetti MG, Schulz PJ. Reconstructing normality following the diagnosis of a childhood chronic disease: does “rare” make a difference? Eur J Pediatr. 2018;177:489–95.
Delisle VC, Gumuchian ST, Rice DB, Levis AW, Kloda LA, Körner A, et al. Perceived benefits and factors that influence the ability to establish and maintain patient support groups in rare diseases: a scoping review. Patient. 2017;10:283–93.
Rizzo R, Van den Bree M, Challenger A, Cuthbert A, Ayllon MA, Clarke A, et al. Co-creating a knowledge base in the “22q11.2 deletion syndrome” community. J Community Genet. 2020;11:101–11.
Lauckner HM, Hutchinson SL. Peer support for people with chronic conditions in rural areas: a scoping review. Rural Remote Health. 2016;16:3601.
Lubitz RJ, Komaromy M, Crawford B, Beattie M, Lee R, Luce J, et al. Development and pilot evaluation of novel genetic educational materials designed for an underserved patient population. Genet Test. 2007;11:276–90.
Permuth-Wey J, Vadaparampil S, Rumphs A, Kinney AY, Pal T. Development of a culturally tailored genetic counseling booklet about hereditary breast and ovarian cancer for Black women. Am J Med Genet Part A 2010;152a:836–45.
Canedo JR, Miller ST, Myers HF, Sanderson M. Racial and ethnic differences in knowledge and attitudes about genetic testing in the US: systematic review. J Genet Couns. 2019;28:587–601.
Hilgart JS, Hayward JA, Coles B, Iredale R. Telegenetics: a systematic review of telemedicine in genetics services. Genet Med. 2012;14:765–76.
Mena R, Mendoza E, Gomez Peña M, Valencia CA, Ullah E, Hufnagel RB, et al. An international telemedicine program for diagnosis of genetic disorders: Partnership of pediatrician and geneticist. Am J Med Genet C Semin Med Genet. 2020;184:996–1008.
Sobering AK, Li D, Beighley JS, Carey JC, Donald T, Elsea SH, et al. Experiences with offering pro bono medical genetics services in the West Indies: Benefits to patients, physicians, and the community. Am J Med Genet C Semin Med Genet. 2020;184:1030–41.
Acknowledgements
The authors would like to thank all participants for sharing their thoughts and experiences during the interviews. This work was supported by Medical Laboratory Services Curaçao.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
The Medical Ethical Committee of the Amsterdam University Medical Center, location AMC, in Amsterdam assessed the study protocol and confirmed that the study was exempt from ethics review according to the Medical Research Involving Human Subjects Act.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Verberne, E.A., van den Heuvel, L.M., Ponson-Wever, M. et al. Genetic diagnosis for rare diseases in the Dutch Caribbean: a qualitative study on the experiences and associated needs of parents. Eur J Hum Genet 30, 587–594 (2022). https://doi.org/10.1038/s41431-022-01039-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-022-01039-4
This article is cited by
-
Physicians’ use and perceptions of genetic testing for rare diseases in China: a nationwide cross-sectional study
Orphanet Journal of Rare Diseases (2023)
-
What matters to parents? A scoping review of parents’ service experiences and needs regarding genetic testing for rare diseases
European Journal of Human Genetics (2023)
-
No gene to predict the future?
European Journal of Human Genetics (2022)