Abstract
Patient care experiences are key to promoting better outcomes and are an essential consideration for successful implementation of genomics in paediatric care. To understand parents’ service experiences and needs regarding testing of their child for rare diseases, we conducted a scoping review. Five databases were searched (2000–2022), with 29 studies meeting the inclusion criteria. Experiences of care wholly delivered by genetic services were most commonly reported (n = 11). Results were synthesised by mapping extracted data to adapted Picker principles of person-centred care. Parents especially valued and emphasised the importance of feeling ‘cared for’, continuous relationships with clinicians, empathic communication, being kept informed while awaiting genetic test results, linkage with informational and psychosocial resources following results disclosure, and follow-up. Strategies were often proposed by authors to address long-standing unmet needs but evidence from the literature regarding their potential effectiveness was rarely provided. We conclude that ‘what matters’ to parents regarding genetic testing is not dissimilar to other aspects of care. Paediatric medical specialists have existing skill sets, trusted relationships and can apply familiar principles of ‘good’ care to enhance experiences of genetic testing. The lack of evidence for service improvement strategies highlights the pressing need to undertake rigorous design and testing of interventions alongside mainstreaming of genomics into paediatric care.
Similar content being viewed by others
Introduction
Exome and genome sequencing (E/GS) promise to provide more timely and accurate diagnoses for children with rare genetic conditions [1]. As the clinical and economic utility of E/GS as an early diagnostic investigation is increasingly recognised by healthcare funders, test availability in clinical settings is increasing [2, 3]. Genetic services are correspondingly struggling to meet demand [4]. To improve patient access, test ordering needs to expand beyond genetic services into mainstream clinical practice [5]. However, effecting practice change in healthcare is notoriously complex and challenging [6]. Interventions are needed to facilitate change and enhance care delivery [7], with understanding the perspectives and needs of diverse stakeholders, including patients and families, critical to identifying and developing effective interventions.
The importance of partnering with patients (and in paediatrics, parents) to help shape and improve service delivery to best meet their needs is increasingly recognised in healthcare [8, 9], evidenced by the inclusion of patient experience in contemporary quality of care standards [10, 11]. A core aspect of this work involves firstly understanding ‘what matters’ to patients (parents) in terms of service delivery [12]. What are their needs, and are they being met? As a first step to addressing these questions and to inform key considerations for service design and intervention development, we reviewed evidence about parents’ service experiences and needs in relation to genetic testing for rare diseases. To the best of our knowledge, the synthesis presented is the first to map experiences of care processes. Recent reviews have focused on singular aspects of care experiences such as understanding of information delivered by providers [13], or interrelated topics such as parent-reported outcomes [14], barriers to genetic test access [15], and the broader supportive care needs of parents caring for children with rare genetic conditions [16]. In mapping the current evidence landscape related to experiences of service provision as a whole, our review identifies opportunities for future intervention research to enhance parents’ care experiences throughout the patient journey and promote health and well-being outcomes [17, 18] in turn.
Methods
Methodology
A scoping review of peer-reviewed literature was undertaken. Scoping reviews serve a range of purposes, including identifying key factors related to a concept and gaps in understanding, and narrowing questions to address in subsequent systematic reviews [19]. Their iterative nature is a key methodological strength, in that it enables researchers to refine and clarify the concept of interest while engaging with the literature. A variety of guidance for conducting scoping reviews exist, with our approach guided by the Joanna Briggs Institute’s framework [20] and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses scoping review extension [21].
Literature search strategy
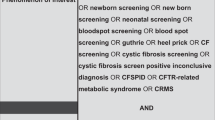
The literature search was developed under the guidance of an experienced medical librarian. Keyword and MeSH terms from relevant papers were incorporated into the search, with the refined search then run across five databases (Medline, Embase, PubMed, PsycInfo, Web of Science) on October 26, 2021. The search was also rerun on July 29, 2022 to identify any studies published since the initial search was conducted. Search terms included parents and caregivers, genetic and genomic tests, delivery of healthcare, experience, patient satisfaction, patient-centred care, and health service needs. The full search strategy is available in Supplementary Material 1. Records retrieved were imported into Endnote X9 (ref. [22]) for duplicate removal, then Rayyan [23] for title/abstract screening.
Study selection
Inclusion and exclusion criteria, mapped to the Joanna Briggs Institute’s Population, Concept, Context mnemonic [20], are summarised in Table 1. In brief, the study population is parents of children with rare conditions of suspected monogenic origin. Studies solely focused on experiences of being offered testing for the following were excluded due to being considered of limited utility in considering service needs for genome-wide, germline sequencing in mainstream settings. Paediatric cancers, as treatment-targeted testing and somatic mutations are the main focus; non-syndromic hearing loss, as targeted gene testing is used in the first instance and has a high diagnostic yield; [24] and autism spectrum disorder, a primarily multifactorial condition for which E/GS is not currently considered an appropriate investigation [25]. The experiences of adolescents were excluded due to their distinct nature [26] and our focus on exploring testing for children. The study concept defines experience as experience of care processes (i.e., delivery of care by health professionals), mirroring the way in which experience is defined in patient-reported experience measures [27]. The study context is primarily focussed on outpatient settings; studies examining parent experiences of rapid genomic sequencing delivered in acute care settings were excluded due to the unique challenges in this context (e.g., time pressures involved) that warrant review in their own right [28]. The year range (2000-present) aimed to enable comparisons in service experiences and needs across test modalities.
To efficiently and rigorously screen the large number of records retrieved, two reviewers (EC, BM) independently reviewed the same subset (10%) of titles and abstracts. Results were compared, with disagreements resolved through discussion and refinements to the selection criteria accordingly made. One reviewer (EC) then applied the refined criteria to the remaining titles and abstracts. Three reviewers independently reviewed all of the full-text records retrieved (EC, BM, MM), with disagreements resolved through discussion and the criteria further refined through this process. Following full-text review, references of included studies were mined, and forward citation searching was conducted in Google scholar.
Data charting and synthesis
Data charted included study characteristics (country of origin, study aims, methodology, sample, genetic investigation(s) undertaken, service delivery model), parents’ experiences of care delivery, and strategies or interventions proposed (by parents or study authors) to address parents’ service needs. The charting form (an Excel spreadsheet) was piloted on five studies by EC, modified following team discussion (BM, MM), then applied across studies.
As no patient experience measures specific to genetics could be identified, findings were mapped to a generic framework (the Picker Principles of person-centred care) to help synthesise the results. This empirically-derived framework, developed by the Picker Institute, consists of eight core components of care known to be important to patients [29]. The Picker Principles and a variant based upon the same research, the Institute of Medicine framework, have been found to be broadly applicable to a wide range of disease contexts and care settings [10, 12].
The Picker principles were adapted to context and refined through ongoing discussion among members of the research team (EC, MM, BM). One reviewer (EC) then deductively coded parents’ service experiences to the adapted principles (see Table 2), with subcategories inductively generated in tandem to describe the nuances of parents’ experiences and needs. A second reviewer (MM) reviewed the mapping, and refinements were made until consensus was reached. Results are reported narratively.
Results
Study selection and characteristics
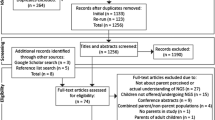
The initial search yielded 12,361 records (see Fig. 1). 7018 titles/abstracts were screened following duplicate removal, with 85 records retrieved for full-text review. Of these, 60 were excluded for reasons detailed in Supplementary Material 2. Three additional studies were included following citation searching. One further study, published since the initial search was run, was identified in the rerun search (Supplementary Fig. S1), generating a total sample of 29 studies for review inclusion.
The majority of studies (17/29) were conducted in North America; [30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46] others originated from Australia [47,48,49,50,51,52], Ireland [53,54,55], the Netherlands [56], UK [57], and Dutch Caribbean [58]. Study aims were diverse (see Supplementary Table S1), with most studies (19/29) deploying a qualitative study design [30, 32,33,34,35,36,37,38,39, 42,43,44, 46, 48, 50, 55,56,57,58]. Neurological phenotypes including intellectual disability and developmental delay were common clinical features among children referred for genetic investigation [31, 32, 35, 36, 38, 40,41,42,43, 46, 50, 52,53,54,55]. Close to half of the studies (14/29) specified the genetic investigation(s) considered or undertaken [35,36,37,38,39, 41,42,43,44,45, 50, 55, 56, 58]. In 10 of these, genome-wide sequencing tests (gene panels, exome or genome sequencing) were conducted, in both research [37, 43,44,45, 56] and clinical [35, 36, 39, 41, 58] settings.
A range of service delivery models were reported, albeit with varying precision. In 11 studies [33, 34, 36, 37, 41, 42, 48, 52,53,54, 57], parents were referred to specialised genetics services for genetic assessment and/or testing. In three additional studies [38, 50, 58], some parents initially received their child’s genetic test results from non-genetic paediatric medical specialists (referred to as paediatric medical specialists herein and meaning physicians who have not undertaken specialised training in medical genetics, in contrast to clinical geneticists) prior to genetics referral. Following assessment and pre-test counselling from genetic providers, parents in two studies received genetic test results from paediatric medical specialists and genetic counsellors [43, 45]. In another two studies [39, 49], pre- and post-test counselling was said to have been provided by various health providers including paediatric medical specialists. Paediatric neurologists were involved throughout the patient journey in one study [56], with clinical geneticists playing a supporting role. Paediatric medical specialists were also reported to be involved in another four studies;[31, 40, 51, 55] however the exact nature of their role was unclear. The service delivery model was unspecified or unclear in a further six studies [30, 32, 35, 44, 46, 47].
Parents’ service experiences
Satisfaction with service delivery and the experience of genetic testing as a whole was reported in eight studies [31, 40,41,42, 51, 52, 56, 58], two of which used the genetic counselling satisfaction scale [41, 52]. Specific aspects of service delivery parents valued or considered lacking were broadly similar across studies irrespective of differences in service delivery models and the type of genetic investigations conducted. Information-related challenges and needs were most commonly reported followed by (insufficient) support for families during and after results disclosure. A synthesis of the components of care influencing parent service experiences is presented in Table 3 and described below. While mapped separately, a number of these components were interrelated.
Clear information, communication, and support for managing child’s ongoing care
Parents want straightforward, jargon-free information
While some parents felt well-informed throughout the patient journey and praised providers’ use of accessible language [31, 37, 44, 47, 49, 51, 52, 56, 57], others commented upon and expressed frustration with the incomprehensible nature of the genetic information providers imparted [31, 39, 42, 48, 54, 56]. Some parents [39, 48] described hiding their lack of understanding behind head nods and smiles, with several reluctant to speak up and ask questions because they found genetics intimidating and felt or feared sounding ‘stupid’ [48, 54]. A number found (or felt they would have found) visuals helpful in aiding their understanding [38, 44, 49], as well as lay summaries that could additionally be shared with family members, educators and health providers [44, 49, 52].
Parents find it difficult to absorb information during test appointments
Parents frequently described feeling overwhelmed at different stages of the genetic testing process, most notably at time of diagnosis [32, 34,35,36, 42, 46,47,48,49,50, 53, 57, 58]. As a result, many found it difficult to absorb and process information during appointments [32, 34,35,36, 46, 48,49,50, 57, 58]. Parents found (or indicated they would have found) take-away resources helpful along with the opportunity for follow-up to ask questions that only become apparent with the benefit of processing time [44, 45, 48, 50, 57]. A need to reduce the volume of information communicated to parents and focus on what parents are most interested in – implications for their child’s care – was also emphasised in several studies of parents whose children underwent genome-wide sequencing [39, 44, 45].
Parents struggle to use and make sense of genetic results
Across studies, challenges in making sense of what genetic test results mean for one’s child and family were commonly described [30, 32, 38, 39, 42, 45, 49, 50, 52, 53, 55, 56, 58]. Sense-making was an ongoing process for a number of parents, with inherently practical questions regarding implications for their child’s immediate care and future outlook continuing to be raised weeks to months after initial results disclosure [45, 53, 55]. Parents wanted to know how to use the genetic information they received and what the ‘next steps’ were [30, 31, 36, 42, 45, 49, 56], and many expressed frustration and disappointment with the inability of health professionals to provide the clarity and guidance they desired [32, 42, 50, 55, 56].
To fill this void of information, parents frequently turned to the Internet despite often being advised by health professionals not to do so [31, 32, 34, 38,39,40, 44, 46, 55, 58]. Internet-searching experiences were mixed in general [30, 31, 38, 39, 43, 46, 51, 55], whether it be for contextualising the meaning of genetic test results [34, 38, 39, 58], searching for possible diagnoses [30], or deciphering the information health professionals imparted [31, 58]. Some felt worse off after reading worst-case scenarios, with Internet searches not always based on accurate information [38, 46, 55]. Some parents expressed a need for health professionals to provide curated resources or links to reputable websites instead of parents being left to their own devices [40, 44]. Parents in two studies [49, 52] expressed a related need for tools to help them understand and keep up-to-date with research developments.
Impact of communication on parents’ affective responses
The potential for communication with providers to both exacerbate and ameliorate the affective responses parents experienced throughout the patient journey was commonly highlighted [40, 42, 47, 50, 52, 55, 57]. The way in which information was framed was particularly influential, with some parents reporting feeling hurt or shattered by providers’ blunt communication style and (poor) choice of words [40, 42, 55]. Parents emphasised the importance of providing hope, even in the face of considerable challenges and uncertainties [40, 42, 55]. Parents’ ability to cope and adapt to uncertainty was also enhanced when health professionals acknowledged the novelty and evolving nature of genomic information [50].
The emotional consequences of receiving incorrect information from paediatric medical specialists during initial results disclosure was highlighted in two studies [38, 51], with a mother in one [38] describing how she spent six weeks needlessly stressed about her child’s variant of uncertain significance while awaiting a consequent genetics appointment.
Involvement and support for families/carers
Parents want to be linked with formal and informal psychosocial supports post genetic testing
Parents wanted health providers to connect them with genetic support groups, other families, and/or counselling supports following results disclosure [31, 35, 38, 40, 47, 48, 52, 55, 57], and were often frustrated by health providers’ failure to facilitate these connections [35, 38, 55, 57]. Indeed, some parents felt let down, lost, and isolated as a result [35, 55, 57]. The value of offering or linking families with psychosocial support at the time of genetic diagnosis was highlighted in two studies [40, 51], with parents more likely to report positive or satisfactory experiences as a result. Some parents considered follow-up an important emotional support in and of itself following results disclosure [37, 45, 48, 52, 56]. They felt that having someone check in on parents during this emotionally challenging and often confusing period of time would be invaluable for helping parents cope and connect with supports as needed. In addition to these needs, parents in several studies [34, 40, 48, 53] expressed a need for a case manager or ‘link person’ to help parents connect with and navigate health services post-testing.
Partnering with parents is important but not all want to be involved to the same degree
Parents in a few studies expressed frustration with having a passive role when interacting with health providers throughout their child’s patient journey [34, 42, 53]. Specifically, some felt dismissed, removed from clinical decision-making, and that conversations were driven by health providers’ agendas rather than their own [34, 42, 53]. Not all parents perceived a passive role negatively, however. Some parents in a US study exploring Latinx parents’ experiences of genome-wide sequencing were comfortable with the genetic test decision-making process being clinician-driven given their self-assessed lack of understanding [36].
Environmental context
Various environmental factors influenced parents’ service experiences [31, 35, 38, 40, 42, 47, 48, 51, 53, 56]. Experiences of receiving genetic test results by telephone rather than in-person were often less positive [38, 40, 51], largely due to misunderstandings arising or the limited psychosocial support available in such instances. Personnel or resources present were also influential [38, 40, 47, 53, 56], with the involvement of genetic counsellors associated with more positive diagnostic experiences in one study [40], for example. In another study [48], the extent to which consultation rooms accommodated families with disabilities and other additional needs influenced parents’ experiences of care. Having sufficient time available to talk and ask questions was also important to parents [31, 37, 39, 40, 53, 54], with several disappointed when genetic consultations did not afford them this opportunity [31, 40, 53].
Timeliness
Timing in which testing is offered impacts parents’ experiences
Parental readiness to receive and process a genetic diagnosis influenced parents’ service experiences in several studies [31, 40, 42, 46]. Readiness was a function of time for some parents, with parents in one study [46] reflecting that they felt better prepared to face genetic testing after having time to adapt to their child’s intellectual disability and additional needs. Accordingly, more positive experiences were reported by parents whose children were older at time of genetic diagnosis in two studies [31, 40].
The importance of parents being able to decline the offer of genetic testing was also highlighted in one study [46], with parents describing the immense relief they experienced when, after being encouraged by physicians to consider genetic testing for their child, another health provider empowered them to decline the test offer.
Long wait times impact parents’ experiences
Long waits inherent to many genetic investigations negatively impacted parents service experiences in several studies [36, 49, 52, 56, 57]. Indeed, the wait for test results was described as one of the most challenging aspects of the genetic testing process in two studies [36, 57]. Parents emphasised the importance of being supported and kept informed by health providers during the stressful waiting period [52, 56, 57], the value of which was highlighted [52, 57].
Smooth transitions and continuity of care
Transitions between different providers involved in child’s testing journey are disjointed for many
Parents referred to genetic services were often confused, concerned and even fearful about what the appointment would entail [34, 48, 53, 54, 57]. Some felt unprepared due to receiving minimal information on what to expect from their referring provider [48, 53, 54]. Parents built-up the appointment in their minds as a result of their lack of understanding and a perception that genetics was ‘different’ from other health services [53, 54]. This perceived distinctiveness was affirmed following the appointment, with some parents citing the nature of the examination conducted and fact that both the child and the parents were ‘patients’ as examples [53, 54]. In addition to disjointed transitions to genetics, disjointed transitions post genetic testing were described in several studies [42, 50, 53], with parents often unclear as to who was responsible for follow-up. A related need for integrated, multidisciplinary care was emphasised [32, 49, 52, 57], with both positive [32, 49] and negative [52, 57] experiences of these noted.
Value of continuous relationships with health providers
The value of continuous relationships with health providers in enhancing parents’ service experiences, decision-making, understanding, and feelings of being supported was highlighted in several studies [35, 38, 42, 44, 49, 52]. Of note in two [38, 49], familiar providers such as paediatricians were considered helpful or best placed to help parents contextualise and make sense of their child’s genetic test results.
Effective care by trusted professionals
Confidence and trust in health providers influences parents’ experiences and behaviours
The importance of interactions with health providers inspiring confidence and trust was highlighted [30, 31, 44, 47, 49,50,51, 57], with parents more likely to report positive experiences when they felt like they were ‘in the hands of the experts’ [43, 47, 49]. Relatedly, more positive experiences were reported when non-genetic providers were open about their limited knowledge of certain genetic conditions and referred parents on [31]. The consequences of parents lacking confidence in providers’ genetics skill sets were described in a few studies [30, 54], with some parents expressing reluctance to ask questions or resorting to their own means to find out information.
Interrelated to confidence in providers, confidence in the information parents received was reported in two studies [50, 52], with confidence fostered when congruent explanations were provided by paediatric medical specialists and genetic providers and hampered when parents perceived providers to be withholding information.
Emotional support, empathy, and respect
Relational aspects of care were important to parents [31, 33, 34, 39, 42, 44, 47, 49, 51, 54, 56], with positive [31, 39, 42, 44, 49, 51, 52, 54, 56] and negative [42, 47, 51] experiences of receiving respectful and empathic care throughout their child’s patient journey described. In particular, parents placed great value on feeling ‘cared for’ by providers [33, 39, 44, 49, 56], and the ability of providers to respond to their emotional needs during genetics consultations [42, 51].
Additional needs of culturally and linguistically diverse (CALD) families
Specific needs and experiences of parents from CALD communities were reported in a subset of studies [33, 36, 39, 48, 58]. Two studies [33, 36] described additional challenges comprehending genetic information, often due to reliance upon medical translators and varying literacy levels. Of note, some parents in these studies stressed the importance of not assuming parents prefer to receive and best understand information communicated in their native language [33, 36]. Several studies [33, 48, 58] also highlighted the importance of receiving culturally safe and respectful care. Caregivers in one study reporting the genetic service experiences of Aboriginal and Torres Strait Islander peoples [48] described their discomfort interacting with providers of the opposite gender, and the consequent impact on their ability to comprehend information. Some felt the support of an indigenous health provider throughout the patient journey would have made them feel more at ease and aided their understanding.
Finding a better way: proposals to meet parent needs
Authors proposed strategies to improve service delivery in 19/29 studies [31,32,33,34, 38, 40, 43,44,45,46, 49,50,51,52,53, 55,56,57,58]. These strategies were targeted at the level of health services [31, 34, 49, 53, 56], providers [31, 33, 38, 40, 44, 50,51,52, 56,57,58], and parents [33, 34, 38, 40, 44,45,46, 49, 51,52,53, 58]. Most proposed strategies were intuitive suggestions from study authors [32, 33, 38, 43, 45, 46, 49,50,51,52, 55,56,57,58], with only one citing evidence for the effectiveness of certain strategies suggested (e.g., two-tiered disclosure appointments) [31]. Examples of intuitive strategies included education and training for health professionals [33, 38, 40, 50, 51, 55, 56], enhanced emotional and practical support during and following appointments [32, 34, 38, 40, 43,44,45, 49,50,51,52, 56, 57], and access to informational resources [34, 44, 46, 49, 52, 58].
Discussion
As a first step to considering how genomics care in paediatric settings can be designed to enhance patient (parent) experiences, we reviewed evidence about parents’ service experiences and needs in relation to genetic testing for rare genetic diseases. Key aspects of care considered important to parents were identified, with these aspects broadly mapping to an established framework, the Picker principles of person-centred care [12, 29]. The fact that principles well-known to be important to patients such as empathic communication and support, feeling listened to and heard, were highly valued by parents suggests that in the eyes of parents, ‘good’ care in genetics is not dissimilar from ‘good’ care in healthcare in general [59]. Others have also (albeit indirectly) drawn this parallel when commenting upon the utility of pre-eminent breaking bad news frameworks to communicating paediatric genetic test results [31, 40, 60]. These parallels should be reassuring to paediatric medical specialists. While the content of the service delivered may arguably be more complex, drawing upon their existing skill sets and applying familiar care principles will likely go a long way to enhancing parents’ care experiences throughout the patient journey.
Nonetheless, several challenges and needs specific to genetic testing were identified. The wait for genetic test results (genomic sequencing results especially) is often considerably longer than other diagnostic investigations. Studies report that parents desire to be supported and kept informed during this anxious time, although exactly what this would look like in practice was often unclear. Sense-making was also highly challenging for many parents due to the inherently complex and often-uncertain nature of their child’s test result. Much has been written about the need to appraise and acknowledge these uncertainties with families to facilitate adaptation [61, 62]. Paediatric medical specialists may be well-placed to do so, with prognostic uncertainty an inherent aspect of many developmental disability diagnoses, for example. Insights from the growing use of genomics in acute settings [28] may also help shed light on how clinicians working in outpatient clinics can be supported to help parents make sense of their child’s test result.
Given the consistency in which sense making challenges (and related frustrations) were reported across studies, the integration of E/GS into paediatrics also presents an opportunity to unpack this long-standing unmet need further. Parents’ desire for practical guidance and more information (a need which often cannot be met presently) may speak more to an underlying need for greater emotional support than information per se [62]. The UK Medical Research Council’s widely regarded guidance on developing complex interventions [63] highlights the importance of comprehensively understanding the problem an intervention seeks to address, from multiple perspectives. Adoption of this guidance in future intervention research will increase the likelihood of more effective and sustainable interventions being developed.
While the fact that aspects of care important to parents were broadly similar regardless of the type of genetic test delivered or model of care provided suggests our review findings are informative for mainstream service design, it is worth noting the relative scarcity of studies describing genetics care provided by paediatric medical specialists. Experiences of genomic sequencing delivered in clinical (i.e., non-research) settings were similarly scarce. The time and resources available in these settings differ, highlighting the need for further research and pragmatic research designs to better understand how service delivery can be best supported. It is encouraging that the service experiences and perspectives of parents from CALD backgrounds have begun to be examined. Future research should expand upon the small subset of studies included in this review to ensure genomic sequencing in paediatric settings is delivered in a way that meets the needs of diverse populations.
Given this review has affirmed the universal nature of core care components important to patients (parents) and exposed the lack of evidence to support proposed strategies, future research could develop a generic tool to help match identified needs to (evidenced-based) intervention categories. Possible benefits of such a tool include improving the ability to identify existing successful interventions that could be repurposed [64], and gaps where new interventions are needed.
To help design better solutions which fit local contexts, codesign with broad stakeholder input should be an integral feature of future intervention development. Encouragingly, some researchers have already begun to use codesign to build upon their exploratory work included in this review [65], with the acceptability of the parent supports developed enhanced as a result [66]. Future systematic reviews should examine how interventions are designed and the relationship between the (co)design process and intervention outcomes to enable successful approaches to be replicated elsewhere.
Limitations
The findings of this review need to be considered alongside its limitations. The search was limited to English-language publications. Some relevant literature may also have been missed despite our efforts to include a broad range of MeSH and keyword terms, with terms used to denote care experiences notoriously heterogeneous [17]. The Picker principles of person-centred care were an imperfect fit for a paediatric context having been developed from empirical research with adult patients in acute care settings [67]. Other frameworks such as the measure of processes of care [68] were reviewed, however challenges remain when applied to a genetics context where both the child and their parents are often ‘patients’. It is worth noting the many similarities of these frameworks and therefore using an alternate framework would likely have had limited impact on the synthesis of results. Nonetheless, the comprehensiveness of the Picker framework was a key strength, with aspects such as timeliness not captured in the measure of processes of care domains, for example.
Conclusion
Our review provides insight into how care can be designed to enhance patient (parent) experiences as the availability of E/GS in paediatric settings increases. Mainstreaming of genomics into medical care presents an opportunity to address long-standing unmet needs and improve how interventions are identified and developed. While further research in more diverse clinical settings is needed, paediatric medical specialists should find it reassuring that current evidence suggests ‘what matters’ to parents regarding genetic testing is not dissimilar to other services. Drawing upon their existing skill sets and applying familiar principles of ‘good’ care will likely go a long way to enhancing parents’ care experiences with genomics and their health and well-being outcomes in turn.
References
Wright CF, Fitzpatrick DR, Firth HV. Paediatric genomics: diagnosing rare disease in children. Nat Rev Genet. 2018;19:253–68.
Sachdev R, Field M, Baynam GS, Beilby J, Berarducci M, Berman Y, et al. Paediatric genomic testing: navigating Medicare rebatable genomic testing. J Paediatr Child Health. 2021;57:477–83.
Lewis C, Buchannan J, Clarke A, Clement E, Friedrich B, Hastings-Ward J, et al. Mixed-methods evaluation of the NHS Genomic Medicine Service for paediatric rare diseases: study protocol. NIHR Open Res. 2021; https://doi.org/10.3310/nihropenres.13236.1.
Fennell AP, Hunter MF, Corboy GP. The changing face of clinical genetics service delivery in the era of genomics: a framework for monitoring service delivery and data from a comprehensive metropolitan general genetics service. Genet Med. 2020;22:210–8.
Burton H, Hall A, Kroese M, Raza S. Genomics in mainstream clinical pathways. PHG Foundation; 2017. https://www.phgfoundation.org/report/genomics-mainstream-clinical-pathways. Accessed 29 Sept 2022.
Bauer MS, Damschroder L, Hagedorn H, Smith J, Kilbourne AM. An introduction to implementation science for the non-specialist. BMC Psychol. 2015; https://doi.org/10.1186/s40359-015-0089-9.
Skivington K, Matthews L, Simpson SA, Craig P, Baird J, Blazeby JM, et al. A new framework for developing and evaluating complex interventions: update of Medical Research Council guidance. BMJ 2021;374:n2061.
Bombard Y, Baker GR, Orlando E, Fancott C, Bhatia P, Casalino S, et al. Engaging patients to improve quality of care: a systematic review. Implement Sci. 2018; https://doi.org/10.1186/s13012-018-0784-z.
Bate P, Robert G. Experience-based design: from redesigning the system around the patient to co-designing services with the patient. Qual Saf Health Care. 2006;15:307–10.
Institute of Medicine. Crossing the quality chasm: a new health system for the 21st century. Natl Acad Press, Washington DC, 2001.
Australian Commission on Safety and Quality in Health Care. Patient-centred care: improving quality and safety through partnerships with patients and consumers, ACSQHC, Sydney, 2011.
Robert G, Cornwell J What matters to patients? Developing the evidence base for measuring and improving patient experience. The King’s Fund, London, 2011.
Gereis J, Hetherington K, Ha L, Robertson EG, Ziegler DS, Barlow-Stewart K, et al. Parents’ understanding of genome and exome sequencing for pediatric health conditions: a systematic review. Eur J Hum Genet. 2022;30:1216–25.
Hayeems RZ, Luca S, Assamad D, Bhatt A, Ungar WJ. Utility of genetic testing from the perspective of parents/caregivers: a scoping review. Children 2021;8:259.
Best S, Vidic N, An K, Collins F, White SM. A systematic review of geographical inequities for accessing clinical genomic and genetic services for non-cancer related rare disease. Eur J Hum Genet. 2022;30:645–52.
Pelentsov LJ, Laws TA, Esterman AJ. The supportive care needs of parents caring for a child with a rare disease: a scoping review. Disabil Health J 2015;8:475–91.
Doyle C, Lennox L, Bell D. A systematic review of evidence on the links between patient experience and clinical safety and effectiveness. BMJ Open. 2013;3:e001570.
McAllister M, Payne K, MacLeod R, Nicholls S, Donnai D, Davies L. What process attributes of clinical genetics services could maximise patient benefits? Eur J Hum Genet. 2008;16:1467–76.
Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018; https://doi.org/10.1186/s12874-018-0611-x.
The Joanna Briggs Institute. Methodology for JBI scoping reviews. The Joanna Briggs Institute, South Australia, Australia, 2015.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169:467–73.
Endnote. Version X9. Thomson Reuters, USA, 2018.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016; https://doi.org/10.1186/s13643-016-0384-4.
Sung V, Downie L, Paxton GA, Liddle K, Birman CS, Chan WW, et al. Childhood hearing Australasian medical professionals network: consensus guidelines on investigation and clinical management of childhood hearing loss. J Paediatr Child Health. 2019;55:1013–22.
Amor DJ. Investigating the child with intellectual disability. J Paediatr Child Health 2018;54:1154–8.
Wainstein T, Marshall SK, Ross CJ, Virani AK, Austin JC, Elliott AM, et al. Experiences with genetic counseling, testing, and diagnosis among adolescents with a genetic condition: a scoping review. JAMA Pediatr. 2022; https://doi.org/10.1001/jamapediatrics.2021.4290.
Goodrich J, Fitzsimons B. Capturing patient experience to improve healthcare services. Nurs Stand. 2019;34:24–8.
Lynch F, Nisselle A, Stark Z, Gaff CL, McClaren B. Parents’ experiences of decision making for rapid genomic sequencing in intensive care. Eur J Hum Genet. 2021;29:1804–10.
The Picker Institute Europe. The Picker principles of person-centred care. 2022. https://picker.org/who-we-are/the-picker-principles-of-person-centred-care/.
Barton KS, Wingerson A, Barzilay JR, Tabor HK. “Before Facebook and before social media…we did not know anybody else that had this”: parent perspectives on internet and social media use during the pediatric clinical genetic testing process. J Community Genet. 2019;10:375–83.
Demarest S, Marsh R, Treat L, Fisher MP, Dempsey A, Junaid M, et al. The lived experience of parents’ receiving the diagnosis of cdkl5 deficiency disorder for their child. J Child Neurol. 2022;37:451–60.
Glassford MR, Purcell RH, Pass S, Murphy MM, Bassell GJ, Mulle JG. Caregiver perspectives on a child’s diagnosis of 3q29 deletion: “we can’t just wish this thing away. J Dev Behav Pediatr. 2022;43:e94–e102.
Hallford H, Coffman MA, Obregon-Tito AJ, Morales AH, Williamson Dean L. barriers to genetic services for Spanish-speaking families in states with rapidly growing migrant populations. J Genet Couns. 2020;29:365–80.
Hernandez VR, Selber K, Tijerina MS. Visioning family-centered care in genetics: what parents and providers have to say. J Genet Couns. 2006;15:349–60.
Li X, Nusbaum R, Smith-Hicks C, Jamal L, Dixon S, Mahida S. Caregivers’ perception of and experience with variants of uncertain significance from whole exome sequencing for children with undiagnosed conditions. J Genet Couns. 2019;28:304–12.
Luksic D, Sukhu R, Koval C, Cho MT, Espinal A, Rufino K, et al. A qualitative study of Latinx parents’ experiences of clinical exome sequencing. J Genet Couns. 2020;29:574–86.
McConkie-Rosell A, Pena LDM, Schoch K, Spillmann R, Sullivan J, Hooper SR, et al. Not the end of the odyssey: parental perceptions of whole exome sequencing (WES) in pediatric undiagnosed disorders. J Genet Couns. 2016;25:1019–31.
Reiff M, Bernhardt BA, Mulchandani S, Soucier D, Cornell D, Pyeritz RE, et al. “What does it mean?”: uncertainties in understanding results of chromosomal microarray testing. Genet Med. 2012;14:250–8.
Watnick D, Odgis JA, Suckiel SA, Gallagher KM, Teitelman N, Donohue KE, et al. “Is that something that should concern me?”: a qualitative exploration of parent understanding of their child’s genomic test results. Hum Genet Genom Adv. 2021;2:100027.
Waxler JL, Cherniske EM, Dieter K, Herd P, Pober BR. Hearing from parents: The impact of receiving the diagnosis of Williams syndrome in their child. Am J Med Genet A. 2013;161:534–41.
Wynn J, Ottman R, Duong J, Wilson AL, Ahimaz P, Martinez J, et al. Diagnostic exome sequencing in children: A survey of parental understanding, experience and psychological impact. Clin Genet. 2018;93:1039–48.
Ashtiani S, Makela N, Carrion P, Austin J. Parents’ experiences of receiving their child’s genetic diagnosis: a qualitative study to inform clinical genetics practice. Am J Med Genet A. 2014;164:1496–502.
Inglese CN, Elliott AM. CAUSES Study, Lehman A. New developmental syndromes: Understanding the family experience. J Genet Couns. 2019;28:202–12.
Li KC, Birch PH, Garrett BM, MacPhee M, Adam S, Friedman JM. Parents’ perspectives on supporting their decision making in genome-wide sequencing. J Nurs Scholarsh. 2016;48:265–75.
Liang NSY, Adam S, Elliott AM, Siemens A, du Souich C, CAUSES Study. et al. After genomic testing results: parents’ long-term views. J Genet Couns. 2022;31:82–95.
Makela NL, Birch PH, Friedman JM, Marra CA. Parental perceived value of a diagnosis for intellectual disability (ID): a qualitative comparison of families with and without a diagnosis for their child’s ID. Am J Med Genet A. 2009;149A:2393–402.
Anderson M, Elliott EJ, Zurynski YA. Australian families living with rare disease: experiences of diagnosis, health services use and needs for psychosocial support. Orphanet J Rare Dis. 2013; https://doi.org/10.1186/1750-1172-8-22.
Dalach P, Savarirayan R, Baynam G, McGaughran J, Kowal E, Massey L, et al. “This is my boy’s health! Talk straight to me!” perspectives on accessible and culturally safe care among Aboriginal and Torres Strait Islander patients of clinical genetics services. Int J Equity Health. 2021; https://doi.org/10.1186/s12939-021-01443-0.
Nevin S, McLoone J, Wakefield CE, Kennedy S, McCarthy H. Genetic testing in the pediatric nephrology clinic: understanding families’ experiences. J Pediatr Genet. 2022;11:117–25.
Wilkins EJ, Archibald AD, Sahhar MA, White SM. “It wasn’t a disaster or anything”: parents’ experiences of their child’s uncertain chromosomal microarray result. Am J Med Genet A. 2016;170:2895–904.
Zurynski Y, Deverell M, Dalkeith T, Johnson S, Christodoulou J, Leonard H, et al. Australian children living with rare diseases: experiences of diagnosis and perceived consequences of diagnostic delays. Orphanet J Rare Dis. 2017; https://doi.org/10.1186/s13023-017-0622-4.
Nevin SM, Wakefield CE, Barlow-Stewart K, McGill BC, Bye A, Palmer EE, et al. Psychosocial impact of genetic testing on parents of children with developmental and epileptic encephalopathy. Dev Med Child Neurol. 2022;64:95–104.
Barr O, Millar R. Parents of children with intellectual disabilities: their expectations and experience of genetic counselling. J Appl Res Intellect Disabil. 2003;16:189–204.
Barr O, McConkey R. A different type of appointment: the experiences of parents who have children with intellectual disabilities referred for genetic investigation. J Res Nurs. 2007;12:637–52.
Fitzgerald J, Wilson C, Kelly C, Gallagher L. ‘More than a box of puzzles’: understanding the parental experience of having a child with a rare genetic condition”. Eur J Med Genet. 2021;64:104164.
Krabbenborg L, Schieving J, Kleefstra T, Vissers LELM, Willemsen MA, Veltman JA. et al. Evaluating a counselling strategy for diagnostic WES in paediatric neurology: an exploration of parents’ information and communication needs. Clin Genet. 2016;89:244–50.
Skirton H. Parental experience of a pediatric genetic referral. MCN Am J Matern Nurs. 2006;31:175–84.
Verberne EA, van den Heuvel LM, Ponson-Wever M, de Vroomen M, Manshande ME, Faries S, et al. Genetic diagnosis for rare diseases in the Dutch Caribbean: a qualitative study on the experiences and associated needs of parents. Eur J Hum Genet. 2022;30:587–94.
Levetown M and the Committee on Bioethics. Communicating with children and families: from everyday interactions to skill in conveying distressing information. Pediatrics . 2008;121:e1441–60..
Witt MM, Jankowska KA. Breaking bad news in genetic counseling—problems and communication tools. J Appl Genet. 2018;59:449–52.
Parascandola M, Hawkins JS, Danis M. Project MUSE - patient autonomy and the challenge of clinical uncertainty. Patient Auton Chall Clin Uncertain. 2002;12:245–64.
Lipinski SE, Lipinski MJ, Biesecker LG, Biesecker BB. Uncertainty and perceived personal control among parents of children with rare chromosome conditions: the role of genetic counseling. Am J Med Genet C Semin Med Genet. 2006;142C:232–40.
O’Cathain A, Croot L, Duncan E, Rousseau N, Sworn K, Turner KM, et al. Guidance on how to develop complex interventions to improve health and healthcare. BMJ Open. 2019;9:e029954.
Waltz TJ, Powell BJ, Fernández ME, Abadie B, Damschroder LJ. Choosing implementation strategies to address contextual barriers: diversity in recommendations and future directions. Implement Sci. 2019; https://doi.org/10.1186/s13012-019-0892-4.
Nevin SM, Wakefield CE, Dadich A, LeMarne F, Macintosh R, Beavis E, et al. Hearing parents’ voices: a priority-setting workshop to inform a suite of psychological resources for parents of children with rare genetic epilepsies. PEC Innov. 2022;1:100014.
Nevin SM, Wakefield CE, Le Marne F, Beavis E, Macintosh R, Sachdev R, et al. Piloting positive psychology resources for caregivers of a child with a genetic developmental and epileptic encephalopathy. Eur J Paediatr Neurol. 2022;39:129–38.
Gerteis M, Edgman-Levitan S, Daley J, Delbanco TL. Through the patient’s eyes: understanding and promoting patient-centered care. Jossey-Bass, San Francisco, 1993.
Cunningham BJ, Rosenbaum PL. Measure of processes of care: a review of 20 years of research. Dev Med Child Neurol. 2014;56:445–52.
Acknowledgements
The authors would like to thank Poh Chua, medical librarian, for her assistance with the literature search strategy.
Funding
This work was supported by the Victorian Government’s Operational Infrastructure Support Program. EC was supported by a National Health and Medical Research Council (NHMRC) postgraduate research scholarship. The contents are solely the responsibility of the individual authors and do not reflect the views of the NHMRC. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Contributions
EC conceptualised the review, and led the literature retrieval, screening, extraction and analysis, as well as preparation of the initial draft and revisions. BM and MM contributed to the conceptualisation of the review, project supervision, literature screening and analysis, and draft revisions. CG contributed to the conceptualisation of the review, project supervision, and draft revisions.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Crellin, E., Martyn, M., McClaren, B. et al. What matters to parents? A scoping review of parents’ service experiences and needs regarding genetic testing for rare diseases. Eur J Hum Genet 31, 869–878 (2023). https://doi.org/10.1038/s41431-023-01376-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41431-023-01376-y
This article is cited by
-
A new impact factor for EJHG in 2022
European Journal of Human Genetics (2023)