Abstract
Background
Given the importance of infancy for establishing growth trajectories, with later-life health consequences, we investigated longitudinal body composition among infants from six economically and ethnically diverse countries.
Methods
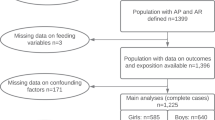
We recruited mother-infant dyads using the WHO Multicenter Growth Reference Study criteria. We measured fat-free mass (FFM) in 1393 (49% female) infants from birth to 6 months of age (Australia, India, and South Africa; n = 468), 3–24 months of age (Brazil, Pakistan, South Africa, and Sri Lanka; n = 925), and derived fat mass (FM), fat mass index (FMI), and fat-free mass index (FFMI). Height-for-age (HAZ), weight-for-age (WAZ), and weight-for-length (WHZ) Z-scores were computed. Sex differences were assessed using a t-test, and country differences using a one-way analysis of covariance. We further compared subsamples of children with average (−0.25 > HAZ < +0.25), below-average (≤−0.25) and above-average (≥+0.25) HAZ.
Results
HAZ performed well between 0 and 6 months, but less so between 3 and 24 months. The stunting prevalence peaked at 10.3% for boys and 7.8% for girls, at 24 months. By 24 months, girls had greater FMI (10%) than boys. There were significant differences in FFM (both sexes in all countries) and FM (Brazilian boys, Pakistani and South African girls) by 24 months of age between infants with average, above-average, and below-average HAZ.
Conclusion
In a multi-country sample representing more ideal maternal conditions, body composition was heterogeneous even among infants who exhibited ideal length. Having a mean HAZ close to the median of the WHO standard for length reduced FFM between-country heterogeneity but not FM, suggesting that other factors may influence adiposity.
Similar content being viewed by others
Introduction
A good start to life is critical to offset later risks including lower school achievement, reduced adult income, non-communicable disease susceptibility, and intergenerational risk [1]. Growth failure and/or rapid weight gain in early life is also associated with an array of adverse health effects in later life [2,3,4]. The WHO Growth Standards have provided better means of interpreting length and weight assessments independent of where the child is born. Along with normative data for foetal growth [5], the child growth standards form part of recent advances in monitoring child development. Normative data for body composition have been described as the next logical level of advancement [6]. The Multi-center Infant Body Composition Reference Study (MIBCRS) has come close to achieving this by developing reference charts for body composition using a multi-ethnic sample, to represent a suitable reference for body composition gain [7].
Data from the MIBCRS emphasise the important role of context [8], home environment and feeding practices [9] in shaping body composition. However, the performance of body composition relative to ideal growth, which is the gold standard for assessing child development in both clinical and epidemiological settings, remains unclear. While anthropometric measurements may provide better reproducibility and are easy to obtain, body composition assessments may provide a more precise picture of the biological response to the interplay of genetic, nutrition, and environmental effects than measures of body size. A better understanding of infant body composition patterns in addition to linear growth may present possible intervention opportunities to reduce the obesity risk in infancy and childhood, and possibly offset the risk of non-communicable disease in adulthood. Therefore, our aim was to investigate longitudinal sex and country differences in infant body composition relative to ideal growth in six countries under conditions that are more likely to facilitate improved linear growth. We hypothesised that children born to mothers selected accordingly to the WHO MGRS [10] will track the WHO growth standards median and have similar FMI and FFMI during infancy irrespective of which country they were born in.
Methods
Study settings
Data were from the Multi-center Infant Body Composition Reference Study (MIBCRS), a longitudinal, multinational study that followed infants from birth to 24 months of age in lower-middle (India, Pakistan, and Sri Lanka), upper-middle (Brazil and South Africa), and high-income (Australia) countries. The study complied with the International Ethical Guidelines for Biomedical Research Involving Human Subjects, and each participating country-site obtained ethical approval from its respective review committee. Written informed consent was obtained from mothers enrolled in the study. Data collection commenced in 2013 and was completed by December 2019.
Participant recruitment
Participant infants were enrolled at birth at the Launceston General Hospital, Tasmania (Australia), at the five hospitals with a maternity ward in Pelotas (Brazil), at St John’s Medical College Hospital, Bangalore (India), at Aga Khan University Hospital in Karachi (Pakistan), Chris Hani Baragwanath Academic Hospital in Johannesburg (South Africa), and at the University Unit of the De Soysa Hospital for Women, in Colombo (Sri Lanka). We recruited 1467 mother-infant dyads (48.7% girls); 476 infants in the sub-study using air-displacement plethysmography (ADP; 2089 data points) to determine body composition at birth, 1, 2, 3, 4 and 6 months of age, and 991 infants in the sub-study using the deuterium dilution technique (DD; 4503 data points) at 3, 6, 9, 12, 18 and 24 months of age. We excluded participants with flagged values (biologically implausible Z-scores and low- or high enrichment) and included 925 children (3708 observations) with data using the DD technique, and 468 children (1899 observations) using ADP. The sample size was calculated for the study sites to have a power of 90% to detect fat mass (FM) and fat-free mass (FFM) for boys and girls less than one standard deviation away from a reference study, that found a mean FM of 3.10 ± 0.5 kg and 3.05 ± 0.46 kg, and mean FFM 9.13 ± 1.06 kg and 8.99 ± 1.1 kg for boys and girls, respectively, which resulted in an estimation of 100 participants per site, 300 for birth to 6 months, and 400 for the 3 to 24 months cohorts [11].
Screening
We recruited women based on: a healthy singleton term infants born within 37 and 42 weeks of gestation, being 18 years or older, a non-smoker with at least secondary school education level, and willing to breastfeed for at least up to 6 months. Infants were to be without morbidity and congenital abnormalities. Infants with significant morbidity such as cardiorespiratory illnesses and congenital abnormalities which might affect infant growth, and mothers living with HIV/AIDS were excluded. Our criteria were consistent with those used in the WHO Multicenter Growth Reference Study (MGRS) and the INTERGROWTH-21st Project [10]. Maternal demography, obstetric history, and education were recorded using questionnaires. Breastfeeding and feeding practices were collected from birth in the birth to 6 months cohort and from the 3-month follow-up in the 3 to 24 months cohort. Infants were classified as being exclusively breastfed (EBF) if they did not consume semi-solid or solid foods and fluids. Questions on consumption on meat, poultry and egg were not asked in Sri Lanka. Excluding these questions in the computation of EBF did not change the prevalence in all countries. Consumption of pure water also did not significantly influence the prevalence of EBF in all countries except South Africa.
Anthropometry
Standardised protocols for anthropometry were developed based on the WHO-MGRS protocol. Newborns were weighed and length measured no later than 24 h after birth. Infant weight and length measurements took place at 1, 2, 3, 4, 6, 9, 12, 18, and 24 months. Weight was measured naked, using a pediatric electronic scale (Seca 376; Hamburg, Germany), accurate to the nearest 5 g. Length was measured using a Harpenden infantometer (300–1100 mm, accurate to 1 mm; Holtain Ltd, Crymych, Wales, UK) in all countries, except India and Sri Lanka, where they used the SECA 417 infantometer.
Air-displacement plethysmography (ADP)
In the birth to 6-month cohort, body composition was assessed by ADP (PEA POD, Software version 3.5.0, 201, COSMED USA) within 2–3 days of birth, and at 1, 2, 3, 4, 6 months employing standard procedures [12]. Total body density was calculated as the ratio of weight (kg) and the measured body volume (L) and was used to calculate the proportions of FM and FFM using assumed densities (0.9007 and 1.063 kg/L for FM and FFM, respectively).
Deuterium dilution (DD) technique
In the 3-to-24-month cohort, body composition was collected using DD at 3, 6, 9, 12, 18, and 24 months of age. Total body water (TBW) is predicted from the dilution of a known quantity of deuterium oxide (D2O) in body water, which is evenly distributed throughout the body within a few hours and can be sampled from saliva. From 3 to 9 months of age, all infants received an oral dose of 1 g sterile D2O (99.8 atom % 2H). From 12 to 24 months, the dose was increased to 1.5 g. The D2O was administered to the infant using a 3 mL syringe. The syringe was filled with the required amount of D2O and weighed before and after administration to determine the weight of D2O consumed. Saliva was sampled before D2O administration (baseline) and 2.5 and 3 h after administration. The baseline saliva sample was collected at least 15 min after the last feed, to ensure that no waste milk or other food was in the child’s mouth. Saliva samples were collected by moving swabs wrapped in cotton inside the child’s mouth until they were soaked. This procedure was repeated until 1 mL of saliva had been collected. If any D2O was regurgitated, the protocol was interrupted, and the mother was invited to return in seven days. Saliva samples were stored in a −20 °C freezer until analysis. The enrichment of deuterium in saliva was measured by isotope ratio mass spectrometry (IRMS) or by Fourier transform infrared (FTIR) spectrometer (Agilent 4500 Series). TBW was calculated using the weight of D2O consumed, the enrichment of the deuterium in the dose, and the enrichment of deuterium in the 3-h saliva sample, with a small correction (4.1%) for non-aqueous exchange of deuterium. FFM was estimated by dividing by an age-related constant for the hydration of FFM, and FM was the difference between body weight and FFM.
Data management and analyses
Data were captured on the REDCap system [13]. The WHO-2006 child growth standards for children from birth to 5 years were used to generate height-for-age (HAZ), weight-for-age (WAZ), and weight-for-length (WHZ) Z-scores in R, flagging biologically implausible values [14, 15]. Additional cleaning was performed with box plots and the plot clean function in the SITAR package (version 1.0.9) in R [16]. Stunting, underweight and wasting were defined as a Z-score of less than minus two (−2) of the median HAZ, WAZ and WHZ Z-scores, respectively. Overweight and obesity was defined as a WHZ Z-score of greater than +1.04, which corresponds to the 85th percentile.
Demographic characteristics were summarised using frequencies (%) for categorical variables and mean (±SD) for continuous variables. Sex differences in anthropometric and body composition measurements were assessed using the independent t-test while an analysis of covariance (ANCOVA) was used to assess country differences, adjusting for differences in the ages of the infants in the different cohorts. We used a one-tailed one-sample t-test to compare country means to the pooled mean at 6 months for the birth to 6-month cohort, and at 24 months for the 3-to-24-month cohort. Further, we performed cross-sectional analyses to compare body composition between subsamples of children who had an average HAZ (−0.25 > HAZ < +0.25), above-average (≥+0.25) and below-average (≤−0.25) HAZ using an ANCOVA. All continuous outcome variables were assessed for normality and log transformed. Data were back transformed and tabulated as geometric means (±SD). Graphs were generated using the ggplot2 package (version 3.3.5) and presented as means (±SE). All tests were performed at the 5% level of significance using R Studio version 1.1.383 (RStudio, Inc).
Results
Description of maternal characteristics
The demographic characteristics of the cohorts are presented in Table 1. Maternal age was youngest in South Africa and India, and oldest in Australia and Brazil. Mothers from India, Sri Lanka, and Pakistan had the lowest pre-pregnancy weight (up to 60 kg) compared to mothers from Brazil, South Africa, and Australia, who weighed about 10 kg more. Years of maternal education were lowest in Sri Lanka, with an average of 11 years of schooling and highest in Brazil, Pakistan, and Australia, with over 14 years of schooling. Exclusive breastfeeding up to 3 months of age was most common in India and Sri Lanka (95.7 & 96.9%), followed by Australia (67.2%), Pakistan (55.1%), Brazil (53.1%), and lowest in South Africa (41.5%). A prevalence of 62.1% of exclusive breastfeeding at 3 months and 28.8% at 6 months was observed in the pooled sample.
Maternal and growth characteristics of infants who had vs. no ADP data at 6-mo
Differences in maternal and infant characteristics between participants with ADP and those without are presented in Supplementary Table 1. We could not collect ADP at 6 months on 98 (~30%) participants who were above the weight allowable by the technique or those who could not be pacified. In both sexes, mothers of infants who had no ADP were significantly heavier than those of infants with ADP. Both male and female infants with no ADP were heavier at birth and at 6 months of age than those with ADP. A total 32 (60%) male and 19 (42%) female infants had a weight greater than 8 kg at age 6 months.
Growth parameters and the prevalence of stunting, wasting, underweight, and overweight
Sex and country differences in weight and length are presented in Supplementary Table 2. In the birth-to-6-month cohort, Australian infants were heavier at birth than both Indian and South African infants. In the 3-to-24-month cohort, Brazilian infants were generally heavier and taller than Pakistani, South African, and Sri Lankan infants at different timepoints.
The mean weight-for-age (WAZ), length-for-age (HAZ), weight-for-length (WHZ) z scores by sex are presented in Fig. 1. In both the birth to 6-month and the 3-to-24-month cohorts, the mean WAZ and HAZ for the pooled sample was consistently between −0.5 SDS and the median of child growth standards, although the mean HAZ started below −0.5 SDS for length at and before 3 months. WHZ was consistently close to the median in both cohorts. In the birth to 6-month cohort significant differences were observed in WAZ and HAZ at birth, which reduced as the children grew, disappearing at 6 months. In contrast, the difference in WAZ and HAZ widened as children grew in the 3-to-24-month cohort.
In the pooled data, boys had a marginally higher prevalence of stunting, underweight, wasting, and overweight and obesity than girls, peaking at 10.3 vs. 7.8%, 8.0 vs. 5.9%, 6.8 vs. 4.3%, and 4.6 vs. 3.1% respectively at 24 months (Fig. 2).
Sex and country differences in body composition
Differences in FM, FFM, FMI, FFMI, and %FM are presented in Fig. 3 and Supplementary Table 3. The pooled data showed negligible sex differences in FM and FMI in both the birth-to-6-month and 3-to-24-month cohorts. Girls had greater a %FM at birth and 6 months in the birth-to-6-month cohort, and at all ages in the 3-to-24-month cohort. Boys had greater FFM and FFMI at all ages in both cohorts.
Mean (±SE) fat mass (A–D), fat-free mass (E–H), fat mass index (I–L), fat-free mass index (M–P), and fat mass % (Q–T) for boys and girls in the birth-to-6-month and 3-to-24-month cohorts. Differences between pooled and country means at 6 months and 24 months are denoted with asterisks (*p < 0.05, **p < 0.01, ***p < 0.001).
In the birth-to-6-month cohort, South African boys and girls had greater FM, FMI and %FM than Australian and Indian infants between birth and 3 months of age. In boys, Australia infants had greater FFM than South African and Indian infants up to 3 months. In girls, Australian and South African infants had greater FFM than Indian infants at all ages. Similar trends were observed in FFMI in both sexes.
In the 3-to-24-month cohort, FM, FMI, and %FM was highest in South African infants and lowest in Sri Lankan infants. Highest FFM and FFMI were found in girls and boys from Brazil, followed by Sri Lanka and Pakistan, with the lowest values observed in South Africa.
Differences between the pooled and country means at 6 and 24 months
In the birth-to-6-month cohort, there were no differences between country and the pooled means for WAZ, HAZ and WHZ in boys. In girls, Indian infants had lower WAZ (p < 0.05) and WHZ (p < 0.001) than the pooled mean at 6 months. In contrast, Australian and South African girls had higher WHZ (p < 0.05) compared to the pooled mean at 6 months. Australian boys had higher FFMI than the pooled mean at 6 months (p < 0.01), while their %FM was lower (p < 0.01). Similarly, mean FFM (p < 0.01) and FFMI (p < 0.001) were lower among Indian girls than the pooled mean at 6 months, but were greater among Australian girls. South African girls also had greater FFMI compared to the pooled mean at 6 months.
In the 3-to-24-month cohort, Brazilian boys and girls had higher WAZ, HAZ, WHZ (p < 0.001) than the pooled mean at 24 months. South African boys (p < 0.05) also had higher WHZ than the pooled mean at 24 months. WAZ and WHZ was lower among Pakistani and Sri Lankan boys and girls. Pakistani, South African and Sri Lankan boys had lower HAZ than the pooled mean at 24 months. Brazilian boys had greater FM (p < 0.05), while both sexes had greater FFM and FFMI (p < 0.001) than the pooled mean at 24 months. South African boys and girls had higher FM, FMI, and %FM (p < 0.001) but lower FFM and FFMI (p < 0.001) than the pooled mean at 24 months. Both Pakistani and Sri Lankan boys and girls had lower FM, FMI and %FM than the pooled mean at 24 months.
Differences in body composition between sub-samples of HAZ
Differences in HAZ, WHZ, FM, FFM, FMI, FFMI, and FM-to-FFM ratio between infants with average (−0.25 > & < +0.25), below-average (≤ −0.25), and above-average (≥ +0.25) HAZ are presented in Fig. 4. were no significant differences in WHZ except in Brazil and Sri Lanka where boys with below-average HAZ had lower WHZ than those with above-average and average HAZ, respectively. Boys from Brazil (p < 0.001) and girls from Pakistan (p < 0.05) and South Africa (p < 0.05) with below-average HAZ, had lower FM than above-average infants, and those with average HAZ in South Africa (p < 0.05). Above-average HAZ girls in Brazil and Pakistan had higher FFM than both average and below-average HAZ girls. Additionally, below-average HAZ boys and girls in Brazil and South Africa, boys in Pakistan and girls in Sri Lanka had lower FFM than both average and above-average HAZ infants. Below-average HAZ girls from Brazil also had lower FFMI than above-average HAZ girls. There were no significant differences in FMI and the FM-to-FFM ratio.
Comparison between infants with average (>−0.25 to <+0.25; solid), above-average (≥+0.25; dashed) and below-average (≤−0.25; dotted) HAZ for height-for-age Z-score, weight-for-length Z-score, fat mass, fat-free mass, fat mass index, fat-free mass index, and fat mass to fat-free mass ratio in the 3-to-24-month cohort. Mean (±SE) are presented.
Discussion
Our aim was to characterise infant body composition longitudinally and to assess how body composition behaves in relation to ideal growth. Women in these cohorts were of above-average socio-economic status, with low parity, and committed to exclusive breastfeeding to provide an optimum environment for child growth. We compared maternal and growth characteristics between infants who had ADP data at 6 months and those who didn’t and found differences in maternal and infant anthropometry. Infants of both sexes for whom ADP data was not collected at 6 months were born to mothers who were heavier before or during early pregnancy, and were consequently heavier at birth and at 6 months. Thus, body composition data in the birth to 6-month cohort represent a lighter population at 6 months, when using ADP. Data for the 3-to-24-month cohort (TBW-derived) may provide a better population estimate for body composition at 6 months irrespective of the method give the strong agreement between ADP-derived and TBW-derived body composition (intraclass correlation of 0.91 for FM and 0.92 for FFM), shown by Kuriyan et al. [8] on the same dataset.
Given the maternal commitment, the prevalence of breastfeeding at 3 months in the pooled sample (62.1%) was higher than the global average (42%) in LMICs [17] and notably higher than reported on average for each country [18, 19]. Consequently, the aggregate growth in height, weight and WHZ aligned with WHO child growth standards for these earlier infant months, except for Sri Lanka, which started about one standard deviation below. Consequently, the prevalence of stunting in this study was lower than regional/country averages. Although the aggregate HAZ maintained a steady level throughout infancy, a decline in South Africa and Pakistan and a lower start in Sri Lanka could have contributed to increase in the prevalence of stunting which peaked by 2 years. We speculate that as the infants age, greater exposure to living conditions, post-weaning practices and infections impact linear growth.
Children from South and Southeast Asia were lighter and had lower FM than infants from Australia, Brazil, and South Africa, and children from South Africa had the highest FM. As anticipated across all countries, infant FM and FFM accrued with age corresponding to increases in linear growth (size). After adjusting for length, for all countries FMI peaked early around 3–6 months and then steadily decreased. Similar patterns were observed across boys and girls, with little ratio differences (FM/FFM). The patterns observed were similar to those observed in other longitudinal studies [11, 20]. However, the pattern for FFMI was different where the peak occurred around 12 months and then slowly decreased. Boys consistently had greater FFM for size than females. While South African infants had greater FMI throughout infancy compared to Brazil, Pakistan and Sri Lanka, the opposite was true for FFMI where it was the lowest. The implication is that the ratio of FMI to FFMI was highest in South Africa, predisposing South African children to greater adiposity and non-communicable disease (NCD) risk trajectories [21].
Santos et al. showed that an increase in economic inequality as measured by the Gini index was associated with a rise in FM and a decrease in FFM in the MIBCRS [9]. Surprisingly, birth weight and exclusive breastfeeding were associated with measures of lean mass as opposed to adiposity at 6 months. However, they showed that continued breastfeeding at 12 months was associated with reduction in FM but also FFM and FFMI, while meeting minimum dietary diversity was associated with positive increase in FFM and FFMI. These findings by Santos et al. [9] on the same cohort for the current study further highlight the strong ecological drivers of adiposity underpinning the differences observed in the current study.
When assessed in relation to ideal linear growth, FMI, FFMI and FM-to-FFM ratio patterns were similar and with less differences between length groups, possibly due to the relatively wide standard errors. There were more differences in FFM across the length groups within each country, but less so between countries and with relatively smaller standard errors. While the overall pattern for FM was similar, FM varied more across the length groups in Brazil and South Africa, with South African females exhibiting greatest FM at 24 months. For all the adiposity indices, South African girls had greater adiposity. This highlights important regional differences for obesity risk that starts in early life even with infants who maintained height close to the median of the WHO growth standard, further emphasising the need to integrate body composition monitoring into paediatric and public health practices to offset childhood obesity.
This study had several strengths and limitations. It is the largest harmonised multi-country infant body composition study completed to date. A limitation of this study was that challenges in administering the deuterium dilution solution to infants resulted in some participants having incomplete longitudinal measurements over time. However, we did factor this in and oversampled to partly compensate for missing data. Secondly, the differences in the assumptions and algorithms of the two methods used to measure body composition separately from birth to 6 months and from 3 to 24 months, do not allow for a smooth transition for longitudinal assessment from birth to 24 months. Lastly, we did not present data on living conditions, post-weaning practices and infections, which can affect linear growth and body composition.
In conclusion, patterns of body composition changes from birth to 2 years of age are similar across the countries and sexes, but the absolute FM and FFM adjusted for length is heterogeneous. This variance may indicate that independent of growth-restricting factors, infant FM and FFM gain are influenced by ethnic and dietary-pattern differences, such that in some settings may be contributing to early childhood obesity. Identifying factors that contribute to these body composition differences is critical. Notwithstanding, measuring body composition remains a research tool until more precise, accurate and quick measurements are achieved, and their clinical applicability established. Future research will need to support ease and accessibility of infant body composition assessments, better understanding the consequences of infant adiposity subgroups for later health and developing efficacious interventions to address early signs of childhood obesity.
Data availability
Data described in the manuscript, code book, and analytic code will be made publicly and freely available without restriction at: https://witscloud-my.sharepoint.com/personal/00000085_wits_ac_za/_layouts/15/onedrive.aspx?id=%2Fpersonal%2F00000085%5Fwits%5Fac%5Fza%2FDocuments%2FIAEA%20MIBCRS%20Data&ga=1.
References
Black RE, Victora CG, Walker SP, Qar Z, Bhutta A, Christian P, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
Cameron N, Pettifor J, de Wet T, Norris S. The relationship of rapid weight gain in infancy to obesity and skeletal maturity in childhood. Obes Res. 2003;11:457–60.
Norris SA, Osmond C, Gigante D, Kuzawa CW, Ramakrishnan L, Lee NR, et al. Size at birth, weight gain in infancy and childhood, and adult diabetes risk in five low- or middle-income country birth cohorts. Diabetes Care. 2012;35:75–9.
Adair LS, Fall CH, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 2013;382:525–34.
Villar J, Altman DG, Purwar M, Noble JA, Knight HE, Ruyan P, et al. The objectives, design and implementation of the INTERGROWTH-21st Project. BJOG Int J Obstet Gynaecol. 2013;120:9–26.
Hills AP, Norris SA, Byrne NM, Jayasinghe S, Murphy-Alford AJ, Loechl CU, et al. Body composition from birth to 2 years. Eur J Clin Nutr. 2023. https://doi.org/10.1038/s41430-023-01322-7.
Murphy-Alford AJ, Johnson W, Nyati LH, Santos IS, Hills AP, Ariff S, et al. Body composition reference charts for infants from birth to 24 months: multicenter infant body composition reference study. Am J Clin Nutr. 2023;117:1262–9.
Kuriyan R, Hills AP, Murphy-Alford A, Padmanabha R, Nyati LH, Byrne NM, et al. Body composition of infants at 6 months of age using a 3-compartment model. Eur J Clin Nutr. 2023. https://doi.org/10.1038/s41430-023-01351-2.
Santos IS, Costa CS, Hills AP, Ariff S, Wickramasinghe VP, Norris S, et al. Infant body composition at 6 and 24 months: what are the driving factors? Eur J Clin Nutr. 2023. https://doi.org/10.1038/s41430-023-01321-8.
de Onis M, Garza C, Victora CG, Onyango AW, Frongillo EA, Martines J. The WHO Multicentre Growth Reference Study: Planning, study design, and methodology. Food Nutr Bull. 2004;25:15–26.
Butte NF, Hopkinson JM, Wong WW, Smith EO, Ellis KJ. Body composition during the first 2 years of life: an updated reference. Pediatr Res. 2000;47:578–85.
Urlando A, Dempster P, Aitkens S. A new air displacement plethysmograph for the measurement of body composition in infants. Pediatr Res. 2003;53:486–92.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inf. 2019;95:103208.
de Onis M, Garza C, Onyango AW, Rolland-Cachera MF. WHO growth standards for infants and young children. Arch Pediatr. 2009;16:47–53.
WHO. Child growth standards. 2017. http://www.who.int/childgrowth/software/en/.
Cole TJ, Donaldson MDC, Ben-Shlomo Y. SITAR–a useful instrument for growth curve analysis. Int J Epidemiol. 2010;39:1558–66.
Neves PAR, Vaz JS, Maia FS, Baker P, Gatica-Domínguez G, Piwoz E, et al. Rates and time trends in the consumption of breastmilk, formula, and animal milk by children younger than 2 years from 2000 to 2019: analysis of 113 countries. Lancet Child Adolesc Health. 2021;5:619–49.
Statistics South Africa. South Africa demographic and health survey 2016 key indicators report. 2016. Available from: https://www.statssa.gov.za/publications/.
Melo DS, de Oliveira MH, dos Santos Pereira D. Brazil’s progress in protection, promoting and supporting breastfeeding from the perspective of the global breastfeeding collective. Rev Paul de Pediatr. 2021;39:e2019296.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982;35:1169–75.
Koontz MB, Gunzler DD, Presley L, Catalano PM. Longitudinal changes in infant body composition: association with childhood obesity. Pediatr Obes. 2014;9:e141–4.
Acknowledgements
SAN is supported by the DSI-NRF Centre of Excellence in Human Development at the University of the Witwatersrand, Johannesburg, South Africa. ISS is supported by the Brazilian National Council for Scientific and Technological Development (CNPq). The authors wish to thank the staff who collected, captured, and cleaned the data.
Funding
This work was supported, in part, by the International Atomic Energy Agency (CRP E43028). IAEA participated in the design, management, analysis, interpretation, preparation, review, and approval of the manuscript. This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation [OPP1143641]. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. Bill & Melinda Gates Foundation did not participate in the design, management, analysis, interpretation, or preparation of the manuscript. Open access funding provided by University of the Witwatersrand.
Author information
Authors and Affiliations
Consortia
Contributions
ISS, APH, SA, PVW, SAN, AMA, RK, and MIBCRS designed the research (project conception, development of overall research plan, and study oversight). LHN and SAN performed the statistical analyses and wrote the first draft of the paper. All authors reviewed and approved the final content of the paper.
Corresponding author
Ethics declarations
Competing interests
RK is an Associate Editor for The European Journal of Clinical Nutrition and played no role in the Journal’s evaluation of the manuscript. All other authors declare no competing interest.
Ethics approval
The study protocol was cleared by the Ethics Research Committee of the institution in each country where the study was conducted. All women signed an informed consent form agreeing to participate in the study.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Norris, S.A., Nyati, L.H., Murphy-Alford, A. et al. Infant growth and body composition from birth to 24 months: are infants developing the same?. Eur J Clin Nutr (2024). https://doi.org/10.1038/s41430-023-01386-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-023-01386-5