Abstract
Providing all infants with the best start to life is a universal but challenging goal for the global community. Historically, the size and shape of infants, quantified by anthropometry and commencing with birthweight, has been the common yardstick for physical growth and development. Anthropometry has long been considered a proxy for nutritional status during infancy when, under ideal circumstances, changes in size and shape are most rapid. Developed from data collected in the Multicentre Growth Reference Study (MGRS), WHO Child Growth Standards for healthy infants and children have been widely accepted and progressively adopted. In contrast, and somewhat surprisingly, much less is understood about the ‘quality’ of growth as reflected by body composition during infancy. Recent advances in body composition assessment, including the more widespread use of air displacement plethysmography (ADP) across the first months of life, have contributed to a progressive increase in our knowledge and understanding of growth and development. Along with stable isotope approaches, most commonly the deuterium dilution (DD) technique, the criterion measure of total body water (TBW), our ability to quantify lean and fat tissue using a two-compartment model, has been greatly enhanced. However, until now, global reference charts for the body composition of healthy infants have been lacking. This paper details some of the historical challenges associated with the assessment of body composition across the first two years of life, and references the logical next steps in growth assessments, including reference charts.
Similar content being viewed by others
Introduction
Historically, the growth, development and nutritional status of infants has been based on anthropometric measurements, most commonly, length (height), weight (mass) and head circumference [1,2,3]. Infancy has long been recognized as one of the most vulnerable life stages but more recently, the early years have been identified as critical in framing phenotypic metabolic profiles associated with health status in later life [4,5,6,7,8,9]. A focused lens on the early years also includes widespread acknowledgement of the importance of a healthy pregnancy and lactation for optimal fetal and infant growth, respectively [10]. Associations between birth size and susceptibility to ill-health as an adult suggest that the growth and development of the infant, including ‘quality’ of growth, is integral to the risk of later abnormal metabolic function. A better understanding of early life changes is particularly important given the dire forecasts regarding the increasing prevalence of cardiovascular diseases, numerous cancers, type 2 diabetes, and bone disease in coming decades. In each case, these disorders are associated with overweight and obesity [8, 11].
The first 1000 days – a critical window
The first 1000 days, from conception to 2 y of age, is widely referenced as a ‘critical window’ for growth and development. During this period, a significant part of the trajectory of an individual’s health status is shaped, and it may also represent the most opportune time for intervention [6, 12]. The ability to assess both growth and body composition during this period may greatly assist in the early identification of health risk, and with appropriate intervention, impact the potential of progression to ill-health [13, 14]. As a foundation, the aggregation of normative body composition and anthropometric data on infants, and ideally, during fetal growth, would enable the further characterization of a healthy pregnancy and quantify the quality of growth. Logic suggests that healthy growth and development is not limited to the first 1000 days but also includes pre-conception. This adds weight to the fact that the growth, body composition and health status of adolescents and young women, ahead of the childbearing years, also deserves closer attention [6, 15, 16].
The current state of play
Despite recognition of the fundamental importance of a good start to life, malnourishment and undernutrition are still commonplace in many mothers and young children [17,18,19,20]. Maternal and child undernutrition is estimated to account for approximately 3·5 million deaths (~11% of global DALYs) in children under 5 y, with stunting, severe wasting, and intrauterine growth restriction constituting the main risk factors [17, 21, 22]. Sadly, these trends are disproportionately higher in low- to middle-income countries, largely due to lifestyle and dietary factors [22,23,24]. In many settings, including in Africa and South Asia, the ‘double burden of malnutrition’, the combination of suboptimal nutrition and overweight, or the ‘triple burden’, when micronutrient deficiencies also exist, are widespread [20, 23, 25,26,27,28,29,30,31,32].
In short, a poor start to life can have irreversible effects, including shorter adult stature, lower school achievement, reduced adult income, and lower birth weight of offspring [20, 22, 33]. Individuals who are small at birth and remain short but become obese during childhood, have an increased risk of co-morbidities of overweight and obesity [34,35,36]. The epidemiological evidence associating smaller size or relative thinness at birth and during infancy with higher rates of chronic disease in adulthood [37,38,39], is particularly strong [6, 40]. For example, increased risk of type 2 diabetes, hypertension, and obesity is greater in individuals with low birth weight and thinness at 2 y of age followed by rapid weight gain [4, 41,42,43,44], and under-nourishment early and overweight later in life, is commonly associated with earlier onset and more severe symptoms than individuals who were never undernourished. Sachdev and colleagues [45] recently cited the very concerning intraindividual double burden of undernutrition (as defined by anthropometry), and ‘metabolic obesity’ in a large study of Indian children. In normal and undernourished groups in this study, a high proportion of children had elevated cardiometabolic risk markers.
A major shortcoming of many studies has been a lack of objective body composition data and an overreliance on body weight and length [46] and indices such as BMI [40]. A number of studies [14, 47] have referenced the use of height, weight and skinfold thicknesses as surrogate methods to ‘assess’ body composition. Without quantification of body composition, we cannot be confident that changes in anthropometry, including BMI, are related to differential adiposity [8, 48]. Limitations of BMI have also been cited in relation to individuals of different ethnicity [6], and resulted in some inconsistences, for example, the ‘thin-fat’ phenotype reported in South Asian infants in some studies [49], but not others [13]. In summary, differences in relative adiposity across ethnic groups has been largely based on anthropometric measures and we are yet to fully understand the nutritional and wider environmental factors influencing such differences.
Greater clarity regarding the interrelationships between diet, nutrition, physical activity, body composition, functional capacity during infancy and childhood, and risk of later disease, is essential, particularly considering regional nuances [50, 51]. The size and shape, plus body composition of an individual, reflects the extent to which the amount and quality of the food consumed over an extended period has adequately (or not) met the needs of the body. As Lopez et al. [52] indicated, it is not surprising that poor nutrition is a major risk factor for disease. Indeed, it is regrettable that ‘nutrition is (still) a desperately neglected aspect of maternal, new-born and child health’ [53], along with quantification and monitoring of body composition [8].
Limitations in the traditional assessment of physical growth and development
A wide range of approaches have been used to assess the size, shape and/or composition of the body and its component parts. Anthropometric screening of height and weight, and the relationship between these measures at different ages, has also been used as a crude indicator of body composition, expressed as BMI, ponderal index or weight for height. Despite the extensive use of body weight as a marker of growth, commencing with birthweight, the relative proportions of lean and adipose tissue can be highly variable for the same body weight [6, 54, 55]. This implies that even at the simplest level, our understanding of the factors that determine the relative partitioning of nutrients in a 2-compartment model (fat mass [FM] and fat-free mass [FFM]), is limited.
At a population level, anthropometry is a convenient approach to monitor changes in physical growth and may also provide an approximation of corresponding changes in body composition. However, one of the factors that compromises the utility of anthropometric measures, including existing data on pregnant women and infants, relates to the lack of representativeness to all population groups [56, 57]. Similarly, the accuracy and precision of measurements should be optimal if anthropometry is utilized to assess relationships between early nutrition and longer-term health. There is also a lack of acknowledgement by some that anthropometric measures and indices are not measures of body composition per se, despite being convenient correlates of FM, FFM and bone mass, key indicators of adequacy of infant nutrition [58]. Noting the limitations, standardized anthropometric approaches to quantify changes in size and shape of mothers and infants should not be underestimated. However, it would be much more valuable to overlay traditional size and shape measures with body composition data to better define the ‘quality’ of physical growth.
The human body can be divided into different components and at all ages, water represents the largest proportion. Under healthy conditions, most body water exists within the lean tissue and accordingly, an assessment of TBW provides us with an index of FFM. Assuming a 2-compartment model, FM can be derived by subtracting FFM from body mass. The simple but versatile two-compartment model has been widely used in nutrition science to estimate both FFM and FM. The model continues to have currency because despite the availability of more sophisticated technology, the use of 3- and 4-compartment approaches require additional technical equipment and therefore tend to be restricted to smaller sample sizes [25, 26, 59].
It is also worth highlighting that to date, most body composition assessment techniques have been developed for, and validated in, adults, meaning their direct application to infants and young children is questionable. Once mature adult status has been attained, under healthy conditions, body size and composition remain relatively constant over time. In contrast, the dynamic and complex nature of the growth changes during infancy are such that the standardization of measurement is particularly challenging. The field of body composition assessment has rapidly evolved in the past few decades and has resulted in the contemporary availability of a range of sophisticated techniques [25, 47, 55, 60,61,62,63,64,65]. Amongst a myriad of options, hydrometry, based on isotope dilution [66], is a particularly useful tool for compositional assessment in infancy. Being non-radioactive, safe, and relative ease of administration, are all factors that have contributed to the increased utilization of stable techniques in recent times [67].
Despite advances in body composition assessment techniques, detailed knowledge of the specific compositional changes during pregnancy and across the first two years, remains limited [62, 68]. A more comprehensive understanding of the normal variability in the body composition of the mother, neonate and infant has the potential to significantly improve maternal and infant health and be a major step forward for the global health agenda. Valid and reliable body composition data would significantly advance our knowledge and understanding of normal growth plus the impact of reduced height velocity in undernourished infants, along with greater detail regarding stunting [69, 70].
Greater clarity regarding growth is not without its challenges
Assessment of growth in early life has many unique challenges [62], particularly given the assortment of intra-uterine and neonatal factors modulating fetal growth and tissue accretion at birth and into the early post-partum period [54, 55, 60]. Rapid fetal body composition changes late in a normal pregnancy include gains in both lean and adipose tissue, and weight [55, 60, 64].
Birth is characterized by fundamental changes in physiology and metabolism as the new-born adapts to an independent extra-uterine environment high in oxygen. Marked changes in weight and composition in the first 72 h of life [60, 71] include changes in the extracellular space, TBW and water levels in tissue fractions [72, 73]. For example, hydration of the FFM can decrease by about 5% across the first year of life and relative fat mass (%FM) changes from approximately 11–15% at birth to 30% at 6 months [72, 74,75,76]. This multiplies the potential complications in the accurate monitoring of growth and body composition during infancy.
As mentioned earlier, the prevention of chronic disease in later life, including co-morbidities of obesity, would greatly benefit from the ability to quantify body composition and track change over time. A better understanding of the specific contribution of intrauterine and post-natal periods to increased adiposity [34, 77,78,79] would be a significant advance. Another major advantage of detailed assessments of body composition during the early years would be to quantify the impact of interventions in this age group [19, 80, 81]. Likewise, it is important to focus more attention on premature infants whose growth is frequently stunted during the early postnatal period [63]. Although discharge weights and term-corrected statistics from around the world indicate that preterm babies typically make up for lost growth and catch up to their full-term counterparts, there is insufficient understanding of how FM and FFM contribute to this atypical growth pattern. Given the link between infant body composition in early life and cardiovascular, metabolic, and neurological outcomes, comprehending this process is crucial [82, 83].
A major evidence gap in the field is the lack of a comprehensive understanding of variability in growth between populations. Primarily, this shortcoming stems from the traditional bias for data collection in high-income countries [48]. Under normal, healthy or ‘ideal conditions’, infancy is a period of rapid linear growth with proportionate increases in FM and FFM [84].
The value of high-quality, normative body composition data
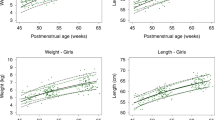
Despite some ambiguity regarding definition, normative data commonly references an observed, preferred, statistical statement of distribution of characteristics in a defined population at a specific point in time. Traditionally, growth assessments have been made on representative convenience samples and less commonly on populations in which preferred health has been characterized. More recent efforts, for example the INTERGROWTH-21st Consortium developed to ascertain if fetal growth, under optimal circumstances, has sufficient cross-population similarities to justify an international fetal and preterm postnatal growth standard, affirmed the appropriateness of such approaches [85]. The WHO Child Growth Standards developed from the MGRS are another excellent example in this context. These studies have made a significant contribution to our understanding of how children free of disease, should grow when reared following standard health practices including breastfeeding and infant and young child feeding (IYCF) practices in a non-smoking environment [86, 87]. Never before has the global community had the luxury of building on this foundation material with a complementary set of body composition data. The derivation of body composition reference charts for infants in the first 2 y of life represents the logical next step. The availability of the first normative body composition data, encompassing variability in the quality of growth of infants up to 2 y of age across different settings and ethnic groups, provides greater clarity regarding growth and development during this critical life stage [86].
Conclusion
Recently published reference charts for body composition or ‘quality’ of growth are a welcome addition to WHO Child Growth Standards generated from anthropometric data. A logical next step is to develop global consensus on definitions and protocols for both anthropometry and body composition assessment in infancy. Such a development would be a major advantage for the world’s youngest and most vulnerable population. Harmonization and standardization of measurement approaches could be achieved through a shared vision for global partnerships between UN agencies and stakeholder organizations, and a systematic increase in quality control mechanisms, including the strategic education and training of relevant health professionals.
References
Tanner JM, Whitehouse R, Takaishi M. Standards from birth to maturity for height, weight, height velocity, and weight velocity: British children, 1965. II. Arch Dis Child. 1966;41:613.
Tanner J. Growth as a monitor of nutritional status. Proc Nutr Soc. 1976;35:315–22.
Waterlow JC, Buzina R, Keller W, Lane J, Nichaman M, Tanner J. The presentation and use of height and weight data for comparing the nutritional status of groups of children under the age of 10 years. Bull world Health Organ. 1977;55:489.
Barker DJP. The developmental origins of adult disease. J Am Coll Nutr. 2004;23:588S–595S.
James W, Vadillo-Ortega F. Long-term fetal programming of body composition and longevity. Nutr Rev. 1997;55:S31.
Barker DJ. Human growth and chronic disease: a memorial to Jim Tanner. Ann Hum Biol. 2012;39:335–41.
Wells JC, Chomtho S, Fewtrell MS. Programming of body composition by early growth and nutrition. Proc Nutr Soc. 2007;66:423–34.
Barker D. Obesity and early life. Obes Rev. 2007;8:45–49.
Barker DJ. The origins of the developmental origins theory. J Intern Med. 2007;261:412–7.
Kunz LH, King JC. Impact of maternal nutrition and metabolism on health of the offspring. Semin Fetal Neonatal Med. 2007;12:71–7.
Macaulay S, Dunger DB, Norris SA. Gestational diabetes mellitus in Africa: a systematic review. PloS One. 2014;9:e97871.
Pietrobelli A, Agosti M. Nutrition in the first 1000 days: ten practices to minimize obesity emerging from published science. Int J Environ Res Public Health. 2017;14; https://doi.org/10.3390/ijerph14121491.
Kuriyan R, Naqvi S, Bhat KG, Ghosh S, Rao S, Preston T, et al. The thin but fat phenotype is uncommon at birth in Indian babies. J Nutr. 2020;150:826–32.
Whyte K, Johnson J, Kelly K, Horowitz M, Widen EM, Toro‐Ramos T et al. No sustained effects of an intervention to prevent excessive GWG on offspring fat and lean mass at 54 weeks: Yet a greater head circumference persists. Pediatric Obes. 2021;16:e12767.
Bryce J, Coitinho D, Darnton-Hill I, Pelletier D, Pinstrup-Andersen P, for the Maternal and Child Undernutrition Study Group. Maternal and child undernutrition: effective action at national level. Lancet. 2008;371:510–26.
Todd AS, Street SJ, Ziviani J, Byrne NM, Hills AP. Overweight and obese adolescent girls: the importance of promoting sensible eating and activity behaviors from the start of the adolescent period. Int J Environ Res Public health. 2015;12:2306–29.
Black RE, Victora CG, Walker SP, Bhutta ZA, Christian P, De Onis M, et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet. 2013;382:427–51.
Bhutta ZA, Black RE. Global maternal, newborn, and child health—so near and yet so far. N Engl J Med. 2013;369:2226–35.
Wells JC. Body composition of children with moderate and severe undernutrition and after treatment: a narrative review. BMC Med. 2019;17:1–9.
UNICEF. The State of the World’s Children 2019. Children, food and nutrition: growing well in a changing world. New York: United Nations Children’s Fund; 2019.
Black RE, Allen LH, Bhutta ZA, Caulfield LE, De Onis M, Ezzati M, et al. Maternal and child undernutrition: global and regional exposures and health consequences. Lancet. 2008;371:243–60.
Victora CG, Christian P, Vidaletti LP, Gatica-Domínguez G, Menon P, Black RE. Revisiting maternal and child undernutrition in low-income and middle-income countries: variable progress towards an unfinished agenda. The Lancet. 2021;397:1388–99.
Popkin BM, Corvalan C, Grummer-Strawn LM. Dynamics of the double burden of malnutrition and the changing nutrition reality. Lancet. 2020;395:65–74.
Rahman MA, Halder HR, Rahman MS, Parvez M. Poverty and childhood malnutrition: evidence-based on a nationally representative survey of Bangladesh. Plos One. 2021;16:e0256235.
Shepherd JA, Heymsfield SB, Norris SA, Redman LM, Ward LC, Slater C. Measuring body composition in low-resource settings across the life course. Obesity. 2016;24:985.
Wells JC. Body composition in infants: evidence for developmental programming and techniques for measurement. Rev Endocr Metab Disord. 2012;13:93–101.
Popkin BM, Adair LS, Ng SW. Global nutrition transition and the pandemic of obesity in developing countries. Nutr Rev. 2012;70:3–21.
Blankenship JL, Rudert C, Aguayo VM. Triple trouble: understanding the burden of child undernutrition, micronutrient deficiencies, and overweight in East Asia and the Pacific. Matern Child Nutr. 2020;16:e12950.
Keats EC, Das JK, Salam RA, Lassi ZS, Imdad A, Black RE, et al. Effective interventions to address maternal and child malnutrition: an update of the evidence. Lancet Child Adolesc Health. 2021;5:367–84.
Keats EC, Charbonneau KD, Das JK, Bhutta ZA. Large-scale food fortification has great potential to improve child health and nutrition. Curr Opin Clin Nutr Metab Care. 2021;24:271–5.
Vassilakou T. Childhood malnutrition: time for action. Children. 2021;8:103.
WHO. Strategic Action Plan to reduce the double burden of malnutrition in the South-East Asia Region 2016–2025. Colombo, Sri Lanka: WHO; 2016. https://apps.who.int/iris/bitstream/handle/10665.
Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child undernutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57.
Baird J, Fisher D, Lucas P, Kleijnen J, Roberts H, Law C. Being big or growing fast: systematic review of size and growth in infancy and later obesity. BMJ. 2005;331:929.
Maguolo A, Olivieri F, Zusi C, Del Giudice EM, Morandi A, Maffeis C. The risk of metabolic derangements is higher in children and adolescents with overweight or obesity born small for gestational age. Nutr Metab Cardiovasc Dis. 2021;31:1903–10.
Nordman H, Jääskeläinen J, Voutilainen R. Birth size as a determinant of cardiometabolic risk factors in children. Horm Res Paediatrics. 2020;93:144–53.
Kensara OA, Wooton SA, Phillips DI, Patel M, Hoffman DJ, Jackson AA, et al. Substrate-energy metabolism and metabolic risk factors for cardiovascular disease in relation to fetal growth and adult body composition. Am J Physiol Endocrinol Metab. 2006;291:E365–E371.
Gluckman PD, Hanson MA, Cooper C, Thornburg KL. Effect of in utero and early-life conditions on adult health and disease. N Engl J Med. 2008;359:61–73.
Adair LS, Fall CH, Osmond C, Stein AD, Martorell R, Ramirez-Zea M, et al. Associations of linear growth and relative weight gain during early life with adult health and human capital in countries of low and middle income: findings from five birth cohort studies. Lancet. 2013;382:525–34.
Wells JC, Davies PS, Fewtrell MS, Cole TJ. Body composition reference charts for UK infants and children aged 6 weeks to 5 years based on measurement of total body water by isotope dilution. Eur J Clin Nutr. 2020;74:141–8.
Bhargava SK, Sachdev HS, Fall CH, Osmond C, Lakshmy R, Barker DJ, et al. Relation of serial changes in childhood body-mass index to impaired glucose tolerance in young adulthood. N Engl J Med. 2004;350:865–75.
Singhal A, Wells J, Cole TJ, Fewtrell M, Lucas A. Programming of lean body mass: a link between birth weight, obesity, and cardiovascular disease? Am J Clin Nutr. 2003;77:726–30.
Barker DJ, Osmond C, Forsén TJ, Kajantie E, Eriksson JG. Trajectories of growth among children who have coronary events as adults. N Engl J Med. 2005;353:1802–9.
Iliadou A, Cnattingius S, Lichtenstein P. Low birthweight and type 2 diabetes: a study on 11 162 Swedish twins. Int J Epidemiol. 2004;33:948–53.
Sachdev HS, Porwal A, Sarna A, Acharya R, Ramesh S, Kapil U et al. Intraindividual double-burden of anthropometric undernutrition and “metabolic obesity” in Indian children: a paradox that needs action. Europ J Clin Nutr. 2021;75:1205–17.
Joglekar C, Fall C, Deshpande V, Joshi N, Bhalerao A, Solat V, et al. Newborn size, infant and childhood growth, and body composition and cardiovascular disease risk factors at the age of 6 years: the Pune Maternal Nutrition Study. Int J Obes. 2007;31:1534–44.
Orsso CE, Silva MIB, Gonzalez MC, Rubin DA, Heymsfield SB, Prado CM, et al. Assessment of body composition in pediatric overweight and obesity: a systematic review of the reliability and validity of common techniques. Obes Rev. 2020;21:e13041.
Wells JC. Toward body composition reference data for infants, children, and adolescents. Adv Nutr. 2014;5:320S–329S.
Yajnik CS, Fall C, Coyaji KJ, Hirve S, Rao S, Barker D, et al. Neonatal anthropometry: the thin–fat Indian baby. The Pune maternal nutrition study. Int J Obes. 2003;27:173–80.
Kuzawa CW, Hallal PC, Adair L, Bhargava SK, Fall CH, Lee N, et al. Birth weight, postnatal weight gain, and adult body composition in five low and middle income countries. Am J Hum Biol. 2012;24:5–13.
Sachdev HS, Fall CH, Osmond C, Lakshmy R, Dey Biswas SK, Leary SD, et al. Anthropometric indicators of body composition in young adults: relation to size at birth and serial measurements of body mass index in childhood in the New Delhi birth cohort–. Am J Clin Nutr. 2005;82:456–66.
Lopez AD, Mathers CD, Ezzati M, Jamison DT, Murray CJ. Global and regional burden of disease and risk factors, 2001: systematic analysis of population health data. lancet. 2006;367:1747–57.
Horton R. Maternal and child undernutrition: an urgent opportunity. Lancet. 2008;371:179.
Nagel E, Hickey M, Teigen L, Kuchnia A, Curran K, Soumekh L, et al. Clinical application of body composition methods in premature infants. J Parenter Enter Nutr. 2020;44:785–95.
Lyons‐Reid J, Derraik JG, Ward LC, Tint MT, Kenealy T, Cutfield WS. Bioelectrical impedance analysis for assessment of body composition in infants and young children‐A systematic literature review. Clin Obes. 2021;11:e12441.
Victora CG, Sibbritt D, Horta BL, Lima RC, ScD TC, Wells J. Weight gain in childhood and body composition at 18 years of age in Brazilian males. Acta Paediatrica. 2007;96:296–300.
James WPT. The epidemiology of obesity: the size of the problem. J Intern Med. 2008;263:336–52.
Pietrobelli A, Faith MS, Allison DB, Gallagher D, Chiumello G, Heymsfield SB. Body mass index as a measure of adiposity among children and adolescents: a validation study. J Pediatrics. 1998;132:204–10.
Wells J, Fewtrell M. Measuring body composition. Arch Dis Child. 2006;91:612–7.
Demerath EW, Fields DA. Body composition assessment in the infant. Am J Hum Biol. 2014;26:291–304.
Toro-Ramos T, Paley C, Pi-Sunyer F, Gallagher D. Body composition during fetal development and infancy through the age of 5 years. Eur J Clin Nutr. 2015;69:1279–89.
Gallagher D, Andres A, Fields DA, Evans WJ, Kuczmarski R, Lowe WL Jr, et al. Body composition measurements from birth through 5 years: challenges, gaps, and existing & emerging technologies—A National Institutes of Health Workshop. Obes Rev. 2020;21:e13033.
Hamatschek C, Yousuf EI, Möllers LS, So HY, Morrison KM, Fusch C, et al. Fat and fat-free mass of preterm and term infants from birth to six months: a review of current evidence. Nutrients. 2020;12:288.
Yumani DF, de Jongh D, Lafeber HN, van Weissenbruch MM. A comparative study using dual-energy X-ray absorptiometry, air displacement plethysmography, and skinfolds to assess fat mass in preterms at term equivalent age. Eur J Pediatrics. 2021;180:919–27.
Davies PS. Stable isotopes: their use and safety in human nutrition studies. Eur J Clin Nutr. 2020;74:362–5.
Hills AP, Davidsson L. Stable isotope techniques to develop and monitor nutrition interventions. Curr Nutr Food Sci. 2010;6:100–4.
Owino VO, Slater C, Loechl CU. Using stable isotope techniques in nutrition assessments and tracking of global targets post-2015. Proc Nutr Soc. 2017;76:495–503.
Orsso CE, Colin-Ramirez E, Field CJ, Madsen KL, Prado CM, Haqq AM. Adipose tissue development and expansion from the womb to adolescence: an Overview. Nutrients. 2020;12:2735.
Leroy JL, Frongillo EA. Perspective: what does stunting really mean? A critical review of the evidence. Adv Nutr. 2019;10:196–204.
Soliman A, De Sanctis V, Alaaraj N, Ahmed S, Alyafei F, Hamed N et al. Early and long-term consequences of nutritional stunting: from childhood to adulthood. Acta Bio Med Atenei Parmensis 2021;92:e2021168.
Hull HR, Thornton JC, Ji Y, Paley C, Rosenn B, Mathews P, et al. Higher infant body fat with excessive gestational weight gain in overweight women. Am J Obstet Gynecol. 2011;205:211.e211–211.e217.
Fomon SJ, Haschke F, Ziegler EE, Nelson SE. Body composition of reference children from birth to age 10 years. Am J Clin Nutr. 1982;35:1169–75.
Lohman TG. Applicability of body composition techniques and constants for children and youths. Exerc Sport Sci Rev. 1986;14:325–57.
Butte NF, Hopkinson JM, Wong WW, Smith EOB, Ellis KJ. Body composition during the first 2 years of life: an updated reference. Pediatr Res. 2000;47:578–85.
Ellis K, Abrams S, Wong W. Body composition reference data for a young multiethnic female population. Appl Radiat Isotopes. 1998;49:587–8.
Andres A, Shankar K, Badger TM. Body fat mass of exclusively breastfed infants born to overweight mothers. J Acad Nutr Dietetics. 2012;112:991–5.
Monteiro POA, Victora CG. Rapid growth in infancy and childhood and obesity in later life–a systematic review. Obes Rev. 2005;6:143–54.
Ong KK, Loos RJ. Rapid infancy weight gain and subsequent obesity: systematic reviews and hopeful suggestions. Acta Paediatrica. 2006;95:904–8.
Oken E, Gillman MW. Fetal origins of obesity. Obes Res. 2003;11:496–506.
Gillman MW, Rifas‐Shiman SL, Kleinman K, Oken E, Rich‐Edwards JW, Taveras EM. Developmental origins of childhood overweight: potential public health impact. Obesity. 2008;16:1651–6.
Chomtho S, Wells JC, Williams JE, Davies PS, Lucas A, Fewtrell MS. Infant growth and later body composition: evidence from the 4-component model. Am J Clin Nutr. 2008;87:1776–84.
Landau‐Crangle E, Rochow N, Fenton TR, Liu K, Ali A, So HY, et al. Individualized postnatal growth trajectories for preterm infants. J Parenter Enter Nutr. 2018;42:1084–92.
Paviotti G, De Cunto A, Zennaro F, Boz G, Travan L, Cont G, et al. Higher growth, fat and fat‐free masses correlate with larger cerebellar volumes in preterm infants at term. Acta Paediatrica. 2017;106:918–25.
Kuzawa CW. Adipose tissue in human infancy and childhood: an evolutionary perspective. Am J Phys Anthropol. 1998;107:177–209.
Villar J, Ismail LC, Urias ES, Giuliani F, Ohuma EO, Victora CG, et al. The satisfactory growth and development at 2 years of age of the INTERGROWTH-21st Fetal Growth Standards cohort support its appropriateness for constructing international standards. Am J Obstet Gynecol. 2018;218:S841–S854.e842
Group WMGRS, de Onis M. WHO Child Growth Standards based on length/height, weight and age. Acta Paediatrica. 2006;95:76–85.
Bhan MK, Norum KR. The WHO multicentre growth reference study (MGRS): rationale, planning, and implementation. Food Nutr Bull. 2004;25:S15–26.
Funding
This work was supported, in part, by the International Atomic Energy Agency (CRP E43028). IAEA participated in the design, management, review, and approval of the manuscript. This work was supported, in whole or in part, by the Bill & Melinda Gates Foundation [OPP1143641]. Under the grant conditions of the Foundation, a Creative Commons Attribution 4.0 Generic License has already been assigned to the Author Accepted Manuscript version that might arise from this submission. Bill & Melinda Gates Foundation did not participate in the design, management, analysis, interpretation, or preparation of the manuscript. Open Access funding enabled and organized by CAUL and its Member Institutions.
Author information
Authors and Affiliations
Consortia
Contributions
APH drafted the paper and all authors have reviewed and contributed to the final version.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
A full list of members and their affiliations appears in the Supplementary Information.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Hills, A.P., Norris, S.A., Byrne, N.M. et al. Body composition from birth to 2 years. Eur J Clin Nutr (2023). https://doi.org/10.1038/s41430-023-01322-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41430-023-01322-7
This article is cited by
-
Infant growth and body composition from birth to 24 months: are infants developing the same?
European Journal of Clinical Nutrition (2024)