Abstract
Purpose
This study aimed to assess the agreement in EBF between maternal recall and the dose-to-mother (DTM) technique.
Methods
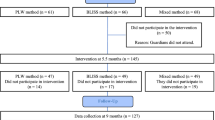
Indonesia, Malaysia, Mongolia, Pakistan, Sri Lanka, Thailand, and Vietnam participated in the study. A total of 207 and 118 mother-infant pairs were assessed at 3 and 6 months of child’s age. Using a standardized questionnaire, mothers were asked to recall child feeding during the previous 24 h, at 3 and 6 months. Those recalled to be EBF proceeded to be assessed using DTM technique. Non-milk oral intake (NMOI) cutoff of 86.6 g/d was used to classify EBF.
Results
According to DTM, 66% of infants were EBF at 3 months, while only 22% were EBF at 6 months. At 3 months, the overall % agreement between maternal recall and DTM method was 68%, kappa 0.06 (95% CI: 0.07–0.20), and at 6 months, the % agreement was only 21%, kappa -0.031 (95% CI -0.168 to 0.107). Human milk intakes were similar at 3 months and 6 months when expressed as g/d, but decreased when expressed as g/kg/d, with a large variation within and between countries; Pakistan being the lowest.
Conclusion
This study showed there were declining levels of EBF from 3 to 6 months in the participating countries from Asia and the agreement between maternal recall and DTM technique to classify EBF was low. To ensure that the DTM technique can be more widely used in evaluating breastfeeding promotion programs, consensus on the appropriate NMOI cutoff and simplification of the DTM protocol is necessary.
Similar content being viewed by others
Introduction
Many low- and middle-income countries (LMIC), including those in Asia, have undergone rapid developmental transition, and are now experiencing a double burden of malnutrition (DBM). In Asia, malnutrition is still widespread, although some countries have been successful in reducing child undernutrition (stunting and wasting). According to the regional estimates of the nutrition situation among children under five, the prevalence of stunting ranged from about 6% in East Asia to slightly over 30% in South Asia and almost 40% in Oceania (not including Australia and New Zealand) [1]. Wasting was only 1.7% in East Asia, 8.2% in Southeast Asia, and 14.1%, the highest, in South Asia [2]. However, overweight and obesity is increasingly on the rise as observed with the development transition. The prevalence of overweight/obesity has risen compared to the prevalence in 2000 and 2020, 4.5 to 5.2% in Asia and 5.2 to 8.0% in Oceania [2].
An important and effective ‘double-duty action’ to combat DBM, is the promotion of EBF as breastfeeding has nutrition and health benefits for both the child and mother [3]. In infants, breastfeeding lowers rates of infant gastrointestinal and respiratory tract infections, as well as decreasing the risk of long-term health issues such as diabetes and obesity [4,5,6,7]. In mothers, breastfeeding may benefit cardiovascular health, cancer risk, mental health, and diabetes risk [8, 9]. The World Health Organization (WHO) recommends that infants be exclusively breastfed for the first six months of life, and the Global Nutrition Target is that 50% of infants should be exclusively breastfed till 6 months of age by 2025 [10]. An objective, accurate method to assess breastfeeding practices is required to evaluate progress toward the breastfeeding target.
Monitoring of EBF is complex, and complicated by interpretation of the definition, recall bias, and data collection method. The commonly used method for collecting data on EBF, especially in large-scale surveys or studies, is maternal recall. Mothers are asked to recall if the baby is given breast milk and/or any fluids or semi-solid foods during the 24 h prior to the data collection, or simply a single question of whether mothers give breast milk alone or also other foods or liquid. Exclusive breastfeeding based on recalls ranges from 22% in East Asia, 44% in Southeast Asia, to 54% in South Asia [8]. However, the data based on recall should be interpreted cautiously due to the recognized maternal recall bias of this method.
A more objective method is desirable, especially to be used in evaluating the impact of breastfeeding intervention programs. An isotope technique, the stable isotope method of DTM, has been used to estimate of the amount of human milk consumed by breastfed infants [11]. The method also provides the estimation of non-milk oral intakes (NMOI), i.e., water consumed from other foods or liquids. The DTM technique has been used in studies in some LMICs which reported the discordance in EBF practice between maternal recall and the assessment by DTM technique, but the method has not been extensively used in the Asia region [12,13,14,15].
The primary aim of this study was to understand breastfeeding practices in various countries in Asia using the accurate technique of DTM and to compare the DTM technique and maternal recall methods of assessing EBF. The study results will demonstrate the common challenges faced by countries in the region, and help raise awareness of policymakers on the need for an accurate indicator in evaluating intervention and promotion/execution of programmes to promote breastfeeding. Human milk intake by infants in the participating countries was also examined as a secondary aim.
Methods
Study site and participants
A longitudinal study in a convenient sample of mother-baby pairs assessed at 3 and 6 months was carried out in 7 countries in Asia, namely, Indonesia, Malaysia, Mongolia, Pakistan, Sri Lanka, Thailand, and Vietnam. Apparently, healthy mothers aged 18–40 y with parity ≤3 and intention to breastfeed until 6 months were included if their infants were aged <3 months, born 37–40 weeks of gestation, apparently healthy, weight-for-height ≥ -2 Z score. and reported to be exclusively breastfed at the time of recruitment and during the whole period prior to the visit. Mothers were asked if the infant was breastfed without providing any other foods or beverages/water. Nine follow-up questions were asked to verify that none of the foods/beverages were given to the infant [16]. Exclusion criteria included twins, low birth weight infants, infants with edema or fluid retention in the mother, and maternal smoking.
The expectation was that on average across the Asian countries, 50% of the babies would be exclusively breastfed when assessed using precise isotopic methods in the <3-month age group, despite a large variability. To estimate this proportion with 95% confidence interval and 20% relative precision, the total sample size required was 97. Thus, we planned to have 30 mother baby pairs to be recruited into the study from each of the seven participating countries. Ethical approval was obtained from the ethics committees or institutional review boards in all participating countries.
Study protocols and data collection
A standardized questionnaire was used by all participating countries to collect the background characteristics of the families and mothers. It was planned that each mother-child pair would have two visits, one at 3 months ± 7d and another at 6 months ± 7d. At each visit, mothers were asked to recall if the babies received breast milk only or any other foods during the previous 24 h using the same standardized questionnaire on infant feeding, as described above [16]. An infant was identified to be EBF by maternal recall if the mother did not report feeding any food other than breast milk. Medicines and syrups were not considered as food [16].
Anthropometry
Maternal and infant weight was taken on day 0 and day 14 of the DTM assessment at the 3-month and 6-month visits. Maternal weight was measured to the nearest 0.1 kg using a digital scale (Seca digital scale model 813; Seca Corporation) and infants were weighed to the nearest 0.1 kg using a digital infant scale (Seca digital scale model 383, Seca Corporation). Maternal height and infant length were measured using a ShorrBoard portable height and length measuring board, to the nearest 0.1 cm. All measurements of anthropometry were made in duplicates.
Dose-to-mother method
The IAEA protocol for assessing human milk intake using the DTM method was used by all participating countries [11]. In the present study, 10 or 30 g (99.8 atom % 2H) of deuterated water, accurately weighed to 0.01 g, was given to mothers, depending on which equipment to use in the measurement of deuterium enrichment. Mothers were requested not to breastfeed or consume any food or liquids for at least 30 min before dose administration. Baseline saliva samples were obtained from both the mother and her baby before the mother consumed the dose. Post-dose saliva samples were collected from both mothers and infants on days 1, 2, 3, 4, 13, and 14 after dosing. Enrichment of 2H in the saliva samples was determined by either the Isotope Ratio Mass Spectrometer (IRMS) or Fourier Transform Infrared Spectrometer (FTIR). The deuterium disappearance in the maternal body water and deuterium enrichment in infant’s body water was calculated by fitting the deuterium enrichment data to a model for water turnover in the mother and in the infant, using the “Solver” function in Microsoft Excel, using nonlinear regression to determine the line of best fit through the data. Quantity of breast milk intake, NMOI, and maternal body composition were determined using standard assumptions and formulae [11]. Children with NMOI ≥ 86.6 g/day were considered as non-EBF using stable isotopic DTM technique [17].
Statistical analysis
All analyses were performed using STATA version 16.0. Descriptive statistics of maternal and child characteristics, human milk intakes, and NMOI are presented as either n (%), Mean ± SD or as median (Quartile 1, Quartile 3). The overall agreement of EBF classification between the recall and DTM techniques is presented using Kappa statistic with 95% Confidence interval. The human milk intake was compared between the different sites at each time point, using analysis of variance for normally distributed data or Kruskal Wallis non-parametric for non-normally distributed data. The pairwise comparison was done with Bonferroni adjustment.
Results
Seven countries, Indonesia, Malaysia, Mongolia, Pakistan, Sri Lanka, Thailand, and Vietnam, were involved in the study. A total number of 206 mother-baby pairs at 3 months, and 118 mother-baby pairs at 6 months, participated in the study.
Table 1 shows the characteristics of mothers and infants at recruitment. The majority of the mother-baby pairs were of first and second parity, with mean maternal age of 28.7 ± 5 years old. About 75% of the mothers who participated had high school and university education levels, however, only about half were employed. A large proportion (over 70%) of mothers received maternal counseling during pregnancy, however, only 62% initiated breastfeeding immediately after childbirth. The average maternal height was 156 ± 6 cm and the mean percent body fat of mothers using the DTM method at 3 months postpartum was 33 ± 10%. Half of the infants recruited were boys. The overall birth weight and length of the infants were 3279 ± 454 g and 51 ± 3 cm, respectively.
Table 2 presents the comparison of the classification of EBF and non-EBF by maternal recall and that assessed by the DTM method at 3 and 6 months of infant age. At 3 months, 78% of mother-infant pairs were classified as EBF based on the 24 recall questionnaire, while at 6 months of age, only 58% of mother-infant pairs were EBF according to recall. At 3 months 68% of infants classified as EBF by recall were also classified as EBF by DTM and at 6 months this was only 21%. The overall agreements between the two methods measured as Kappa was very low at 3 months (kappa 0.06, 95% CI: 0.07–0.20) and 6 months (kappa −0.031, 95% CI: -0.168–0.107). The % agreement between EBF by recall and DTM at 3 months varied widely, from 50% in Pakistan to 87% in Mongolia (Fig. 1). At 6 months, this was much lower, only 5% in Vietnam, and highest in Indonesia (33%).
At 3 months the human milk intake of infants classified as EBF based on maternal recall was lower (median 761 g/d, IQR: 646, 906) than that of children classified by DTM technique (median 799 g/d, IQR: 686, 945). The NMOI of children classified as EBF based on maternal recall (median 60 g/d, IQR: 14, 120) was much higher than those identified by DTM (median 30 g/d, IQR: 0-61). At 6 months, the NMOI was larger in those defined as EBF by both the recall and DTM method (139 [95% CI: 95, 233] and 57 [95% CI: 47, 83], respectively) compared to NMOI at 3 months.
The median (quartile1, quartile3) amount of human milk intakes at 3 months (n = 207) was 760 g/d (646, 906) and at 6 months (n = 118) was 777 g/d (627, 894) as assessed by DTM method (Table 3). When expressed as g/d or g/kg body weight/d, the human milk intake was different between sites at both time points (p < 0.001). At 6 months, no estimation was made for Malaysia and Mongolia, as none of the mothers were EBF. The intake of Pakistani children was lower than that of Indonesian, Mongolian, and Sri Lankan children at 3 months. When the intake at 6 months was compared between sites that had the data, the intake of Pakistani children was lower than that of Indonesian and Sri Lankan children after Bonferroni adjustment for multiple comparisons.
Discussion
This study demonstrates the varying EBF practices in the seven Asian countries involved. According to DTM, 66% of infants were EBF at 3 months, while only 22% were EBF at 6 months. According to maternal recall, 78% of participants were EBF at 3 months and 58% at 6 months. There were large discrepancies in EBF between the recall and DTM methods when assessed at both 3 months (68% agreement) and 6 months (21%) of the infant’s age, and the differences varied across countries. As noted, the extent of discordance was high (agreement around 50–60%) in Malaysia, Pakistan, Sri Lanka, and Vietnam compared to that in Indonesia and Mongolia (over 80%) and Thailand (72%).
Several previous studies also reported discordance in EBF between maternal recall and the use of the DTM technique [12,13,14,15, 18, 19]. The magnitudes of discrepancy can not be compared due to the use of different questions on maternal recall and NMOI cutoffs in the DTM technique. Assessing EBF practice using the DTM technique showed that the actual EBF in many countries can actually be much lower than that reported in large-scale surveys. It is imperative that the DTM method be used when the accurate assessment of EBF is required, for example, in a subsample of a large-scale survey to verify the actual EBF practice and evaluate the effectiveness of the breastfeeding promotion program.
The reasons for the wide variation in the degree of discordance may be due to the maternal bias in the recall method, possibly influenced by prior knowledge about EBF being good for child’s health or not necessarily having a true understanding of the definition of EBF. A study in Thailand showed that some mothers considered giving a small amount of water to the babies to clean their mouths after feeding. Hence, it might not be considered giving water as part of the feeding [18]. The reported EBF mothers in this Thai study had a median NMOI of 30.8 (IQR: 6.5, 69.3) and reported no water or very little amount of water given for the reason mentioned. Interestingly, mothers who were defined as predominantly breastfeeding showed a median NMOI of 83.4 (IQR: 22.5, 141.5) suggesting that some mothers could have given only a minimum amount of water. Similar overlaps of NMOI between EBF and non-EBF were also reported by Moore et al. [19]. In the present study, we used the most recently proposed NMOI cutoff by Liu et al. (86.6 g/d) to categorise infants as EBF [17] as was also used in other recent studies [20, 21]. This cutoff has the advantage because it was validated against a close observation of breastfeeding at home.
Despite a wide variation in the quantity of human milk intake by study site, the milk intakes (g/d or g/kg body weight/d) were comparable to that reported in a recent systematic review of human milk intake data from all continents, and including both high, middle and low-income countries, at 3 and 6 months [22]. The milk intake among Pakistani infants was much lower than in other countries in the present study and that of the global estimates, which warrants concern, and the reasons for this finding deserve to be explored.
The DTM technique is a more objective measurement for understanding EBF than relying on mothers recall alone and has the added benefit of also providing the amount of human milk intake. Fear of inadequate breast milk production to meet the needs of infants has been a common reason for mothers to introduce foods other than breast milk, or worse to decline from breastfeeding. Hence, the benefits of having human milk intake estimation are twofolds. One, it demonstrates the adequacy of intake from breastfeeding within that population; another is to use the data to estimate the total nutrient intake of breastfed infants.
Nevertheless, a major limitation of the DTM method for use in large population studies is that its current protocol requires collecting 7 saliva samples over the duration of 13–14 days. The recent work on developing a parsimonious DTM design whereby only two post-dose saliva samples, instead of 6 samples in the full DM protocol, was shown to be adequate to classify EBF [23]. Therefore, this streamlined protocol needs to be operationalized in a large survey or study to document its feasibility and operational requirements, such as capacity building, standardization, and cost. A final methodological issue is that the classification of EBF based on a cut-off is a deterministic approach where every child has either 100% or 0% chance of being EBF based on the cut-off used. This is inefficient because the cut-off itself is based on a certain probability of being at a percentile of the NMOI distribution of a standard population (90th percentile for the 86.6 g/day cut-off) and the measurement of NMOI in the sampled data is prone to measurement error due to various factors including precision of instruments used and assumptions in calculation. If the DTM method is to be used for accurately defining EBF practice, there is an urgent need for a consensus on which NMOI cutoff or approach should be used.
Conclusions
The use of the deuterium dose to mother technique (DTM) showed the discordance between the maternal recall of EBF and that assessed by DTM in a multi-country study in Asia. The results showed that there is clearly discordance between the two methods, with some variation in the extent of discordance by countries. Consensus on the appropriate NMOI cutoff for classifying EBF from non-EBF is needed to be recommended for global use. To better evaluate the achievement of the global target on EBF, it is important to use an objective and accurate method for evaluation of the breastfeeding programs, such as the DTM technique.
Data availability
Data generated from this study are deposited at the IAEA repository on human milk intakes and can be available upon request.
References
FAO, UNICEF, WFP, WHO (2021) Asia and the Pacific regional overview of food security and nutrition 2020: Maternal and child diets at the heart of improving nutrition. Bangkok: FAO
UNICEF/WHO/World Bank Group – Joint Child Malnutrition Estimates (2021) Levels and trends in child malnutrition. Geneva: World Health Organization
Hawkes C, Ruel MT, Salm L, Sinclair B, Branca F. Double-duty actions: seizing programme and policy opportunities to address malnutrition in all its forms. Lancet. 2020;395:142–55. https://doi.org/10.1016/S0140-6736(19)32506-1
Lee MK, Binns C (2019) Breastfeeding and the risk of infant illness in Asia: A Review. Int J Environ Res Public Health 17. https://doi.org/10.3390/ijerph17010186
Saeed OB, Haile ZT, Chertok IA (2020) Association between exclusive breastfeeding and infant health outcomes in Pakistan. J Pediatr Nurs. 50:e62-e8. https://doi.org/10.1016/j.pedn.2019.12.004
Krawczyk A, Lewis MG, Venkatesh BT, Nair SN. Effect of exclusive breastfeeding on rotavirus infection among children. Indian J Pediatr. 2016;83:220–5. https://doi.org/10.1007/s12098-015-1854-8
Horta BL, Loret de Mola C, Victora CG. Long-term consequences of breastfeeding on cholesterol, obesity, systolic blood pressure and type 2 diabetes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:30–7. https://doi.org/10.1111/apa.13133
Nguyen B, Jin K, Ding D. Breastfeeding and maternal cardiovascular risk factors and outcomes: a systematic review. PLoS ONE. 2017;12:e0187923 https://doi.org/10.1371/journal.pone.0187923
Chowdhury R, Sinha B, Sankar MJ, Taneja S, Bhandari N, Rollins N, et al. Breastfeeding and maternal health outcomes: a systematic review and meta-analysis. Acta Paediatr. 2015;104:96–113. https://doi.org/10.1111/apa.13102
Zong X, Wu H, Zhao M, Magnussen CG, Xi B. Global prevalence of WHO infant feeding practices in 57 LMICs in 2010-2018 and time trends since 2000 for 44 LMICs. EClinicalMedicine. 2021;37:100971 https://doi.org/10.1016/j.eclinm.2021.100971
IAEA (2010) IAEA human health series no. 7: stable isotope technique to assess intake of human milk in breastfed infants. Vienna: International Atomic Energy Agency.
Samuel TM, Thomas T, Bhat S, Kurpad AV. Are infants born in baby-friendly hospitals being exclusively breastfed until 6 months of age? Eur J Clin Nutr. 2012;66:459–65. https://doi.org/10.1038/ejcn.2011.179
Medoua GN, Sajo Nana EC, Ndzana AC, Makamto CS, Etame LS, Rikong HA, et al. Breastfeeding practices of Cameroonian mothers determined by dietary recall since birth and the dose-to-the-mother deuterium-oxide turnover technique. Matern Child Nutr. 2012;8:330–9. https://doi.org/10.1111/j.1740-8709.2011.00293.x
Motswagole, Matenge STP, Mongwaketse T, Bogopa J, Kobue-Lekalake R, Mosetlha K, Kwape L. Application of the deuterium-oxide dose-to-mother technique to determine the exclusivity of breastfeeding in women in Kanye, Botswana. S Afr J Clin Nutr. 2015;23:128–33.
Mazariegos M, Slater C, Ramirez-Zea M. Validity of Guatemalan mother’s self-reported breast-feeding practices of 3-month-old infants. Food Nutr Bull. 2016;37:494–503. https://doi.org/10.1177/0379572116654644
World Health Organization and the United Nations Children’s Fund (UNICEF) (2021) Indicators for assessing infant and young child feeding practices: definitions and measurement methods. Geneva: World Health Organization and the United Nations Children’s Fund (UNICEF).
Liu Z, Diana A, Slater C, Gibson RS, Houghton L, Duffull SB. Development of a nonlinear hierarchical model to describe the disposition of deuterium in mother-infant pairs to assess exclusive breastfeeding practice. J Pharmacokinet Pharmacodyn. 2019;46:1–13. https://doi.org/10.1007/s10928-018-9613-x
Tongchom W, Pongcharoen T, Judprasong K, Udomkesmalee E, Kriengsinyos W, Winichagoon P. Human milk intake of Thai breastfed infants during the first 6 months using the dose-to-mother deuterium dilution method. Food Nutr Bull. 2020;41:343–54. https://doi.org/10.1177/0379572120943092
Moore SE, Prentice AM, Coward WA, Wright A, Frongillo EA, Fulford AJ, et al. Use of stable-isotope techniques to validate infant feeding practices reported by Bangladeshi women receiving breastfeeding counseling. Am J Clin Nutr. 2007;85:1075–82. https://doi.org/10.1093/ajcn/85.4.1075
Mulol H, Coutsoudis A. Limitations of maternal recall for measuring exclusive breastfeeding rates in South African mothers. Int Breastfeed J. 2018;13:19 https://doi.org/10.1186/s13006-018-0159-8
Whyte S, McLean-Smith J, Reid M. Concordance of the deuterium dose to mother method and 24-hour recall to measure exclusive breastfeeding at 6 weeks postnatally in rural/urban setting in Jamaica. Matern Child Health J. 2022;26:2126–36. https://doi.org/10.1007/s10995-022-03465-8
Rios-Leyvraz M & Yao Q. The volume of breast milk intake in infants and young children: a systematic review and meta-analysis. Breastfeeding Med. 2023:18. https://doi.org/10.1089/bfm.2022.0281
Liu Z, Diana A, Slater C, Preston T, Gibson RS, Houghton L, et al. Development of a parsimonious design for optimal classification of exclusive breastfeeding. CPT Pharmacomet Syst Pharm. 2019;8:596–605. https://doi.org/10.1002/psp4.12428
Acknowledgements
We would like to express gratitude to the International Atomic Energy Agency (IAEA) for providing technical support (Technical Cooperation RAS6073) and supplies for the study. This work was also supported, in part, by the national funding for participating countries. IAEA participated in the design, management, analysis, interpretation, preparation, review, and approval of the manuscript.
Author information
Authors and Affiliations
Contributions
PW, TP, CS, AJMA conceived the study and led the planning of the study protocol with inputs from country authors and MI; TP, TF, EW, NK, EP, TA, AY, MH, KJ, NTT, HVTT conducted field data, sample collection, and sample analysis; TT performed statistical analysis; PW drafted the first draft of the manuscript with inputs and approval of final manuscript from all authors.
Corresponding author
Ethics declarations
Competing interests
Pattanee Winichagoon, Tippawan Pongcharoen, Tetra Fadjarwati, Ermin Winarno, Norima A Karim, Enkhzul Purevsuren, Tanvir Ahmad, Ayesha Yameen, Manjula Hettiarachchi, Kunchit Judprasong, Nga Tran Thuy, Hien Vu Thi Thu, Munirul Islam, Christine Slater, Tinku Thomas, and Alexia J Murphy-Alford, confirmed no conflicts of interest.
Ethical approval
This study was conducted according to the guidelines laid down in the Declaration of Helsinki. The approval for the study in the country was obtained from the Ethical Review Committee in each country by the respective lead authors and other administrative approvals were also their responsibility.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Winichagoon, P., Pongcharoen, T., Fadjarwati, T. et al. Discordance in exclusive breastfeeding between maternal recall and deuterium dose-to-mother technique during the first 6 months of infants: A multi-country study in Asia. Eur J Clin Nutr 78, 135–140 (2024). https://doi.org/10.1038/s41430-023-01353-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01353-0