Abstract
In addition to susceptibility to infections, conventional primary immunodeficiency disorders (PIDs) and inborn errors of immunity (IEI) can cause immune dysregulation, manifesting as lymphoproliferative and/or autoimmune disease. Autoimmunity can be the prominent phenotype of PIDs and commonly includes cytopenias and rheumatological diseases, such as arthritis, systemic lupus erythematosus (SLE), and Sjogren’s syndrome (SjS). Recent advances in understanding the genetic basis of systemic autoimmune diseases and PIDs suggest an at least partially shared genetic background and therefore common pathogenic mechanisms. Here, we explore the interconnected pathogenic pathways of autoimmunity and primary immunodeficiency, highlighting the mechanisms breaking the different layers of immune tolerance to self-antigens in selected IEI.
Similar content being viewed by others
Introduction
Autoreactivity may to some extent be physiological, participating in the positive selection of lymphocytes and homeostasis of the immune system, and autoreactivity can be traced in healthy individuals as circulating autoantibodies and minor lymphocytic tissue infiltrates.1 In contrast, aberrant responses to self-antigens underlie more than 80 inflammatory conditions, defined as autoimmune diseases. Common autoimmune diseases, such as rheumatoid arthritis (RA), Sjogren’s syndrome (SjS), and systemic lupus erythematosus (SLE), appear to have a polygenic nature and are often the consequence of a pathogenic interplay between environmental and genetic factors.2,3,4,5
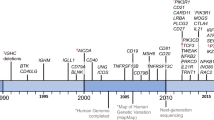
The term human inborn errors of immunity (IEI) is synonymous for primary immunodeficiency disorders (PIDs) and covers disorders with diverse clinical manifestations, ranging from susceptibility to infections to immune dysregulation and malignancy. As these disorders are caused by monogenic germline mutations, the term IEI highlights the increasingly identified genetic background of PIDs. To date, more than 430 monogenic traits falling under IEI have been reported.6 Not all mutations within genes linked to an IEI are pathogenic. The localization and severity of a mutation within a particular gene determines the resulting molecular dysfunction and the consequent aberration of immunity and/or immune tolerance.7 Further, the incomplete penetrance and variable expressivity of certain mutations reported as disease-causing call into question the monogenic etiology of IEI and the definite division between monogenic and poly- or oligogenic PIDs and suggest the strong influence of additional genetic and/or epigenetic modifiers.7
Although the terms autoimmunity and immunodeficiency appear contradictory, PIDs, even combined immunodeficiencies (CIDs), can manifest with autoimmunity, which can be their prominent phenotype.8,9 Interestingly, genetic variants reported in the context of IEI as disease causing, have been identified among patients with clear rheumatic phenotypes.10 Further, genes linked to IEI have been identified as risk genes in autoimmune rheumatic diseases.9,10,11,12 Such genes at the crossroads of autoimmunity and immunodeficiency are involved in immune checkpoint pathways, antigen receptor or cytokine signaling and, especially, type I interferon responses (Table 1). In addition to the evidence on a shared genetic basis of autoimmunity and immunodeficiency, the idea of the continuum of immunological diseases with sheer immunodeficiency or autoimmunity phenotypes representing two extremes of overlapping phenotypes caused by interconnected pathomechanisms is supplemented through the increasing identification of autoantibody-induced susceptibility to infection.13,14 Certain anti-cytokine autoantibodies have been reported to cause susceptibility to infections mimicking IEI. For example, autoantibodies to IFNγ can cause susceptibility to mycobacterial disease,15,16 autoantibodies to GM-CSF can induce susceptibility to infections with Aspergillus or Cryptococcus species17,18,19 and autoantibodies against type I interferons have been recently identified to underlie life-threatening COVID-19 pneumonia.20
In the present review, we discuss the genetic basis of autoimmunity in PIDs. Further, we explore how particular genetic defects linked to the currently known IEI break the different layers of immune tolerance to self-antigens. Our review is by no means an exhaustive investigation of the origins of autoimmunity in all known IEI. Instead, we highlight the diverse pathophysiological pathways underlying autoimmunity and their relevance for selected IEI.
Ineffective central tolerance
Random recombination events during thymic T-cell development yield a broad T-cell repertoire, including a large proportion of autoreactive thymocytes.21 Central T-cell tolerance is achieved through the mechanism of negative selection, whereby thymocytes recognizing self-antigens displayed on MHC molecules of medullary epithelial cells (mTECs) or thymic dendritic cells (DCs) with higher affinity undergo clonal deletion (Fig. 1). An alternative fate for autoreactive thymocytes is their differentiation into natural or constitutive CD4+CD25+Foxp3+ regulatory T cells (Tregs), which are able to suppress the induction and activation of effector T cells, preventing, or regulating immune responses.22,23 Despite their thymic origin, natural Tregs, together with adaptive or inducible Tregs, which have an extrathymic origin, are considered mechanisms of peripheral tolerance and will be discussed as such in this review.
Inborn errors of immunity (IEI) impairing the induction of central T-cell tolerance. AIRE medullary thymic epithelial cells (mTECs) express an array of tissue-specific antigens. Autoreactive T-cell precursors recognizing self-antigens with relatively high avidity undergo clonal deletion (negative selection) or differentiate into natural regulator cells (Tregs). However, some autoreactive T cells skip central tolerance and escape the thymus. Monogenic immunodeficiency disorders affect antigen presentation by mTECs, clonal deletion or T-cell differentiation into natural Tregs; monogenic disorders and the level at which they impair or likely impair central T-cell tolerance are highlighted in red [APECED autoimmune polyendocrinopathy, candidiasis and ectodermal dystrophy, IPEX immunodysregulation, polyendocrinopathy, enteropathy and X-linked]
Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy
Autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy (APECED, also known as autoimmune polyglandular syndrome type 1) is a rare multiorgan autoimmune disease caused by biallelic loss-of-function mutations in the gene encoding the autoimmune regulator (AIRE).24,25 AIRE is a transcription regulator orchestrating the expression of tissue-specific antigens (TSAs) by mTECs. As discussed previously, the latter is crucial for the induction of central tolerance through the process of negative selection. Autoimmunity in APECED commonly results in polyendocrinopathy but can affect nearly all organs. Chronic mucocutaneous candidiasis is the major infectious manifestation of APECED. A minority of patients display recurrent herpetic infections (HSV and VZV). Further, some patients are susceptible to infections with encapsulated bacteria, as they develop asplenia. Chronic mucocutaneous candidiasis in APECED is associated with the presence of neutralizing autoantibodies against Th17 cytokines (IL-17A, IL-17F, and IL-22), which suggests the autoimmune origin of immunodeficiency in this disorder.26,27
DiGeorge syndrome
DiGeorge syndrome (or 22q11.2 deletion syndrome) is the consequence of disturbed development of the pharyngeal pouches, especially of the third and fourth pouches, which causes thymic hypoplasia or aplasia.28 Residual thymic function defines the degree of T-cell deficiency, which can range from a severe combined immunodeficiency (SCID)-like phenotype with the absence of T cells to normal T-cell counts and function. DiGeorge syndrome results in a relatively high prevalence (~8% of patients) of autoimmunity, most commonly manifesting as autoimmune cytopenia. Considering that DiGeorge syndrome is the consequence of disturbed development of the thymus, autoimmunity is thought to stem from defects in central tolerance. However, unlike patients with APECED, most DiGeorge syndrome patients display a single or two autoimmune diseases, and autoimmune manifestations have a later onset, precluding major defects in negative selection.29 Low numbers of Tregs may be the consequence of reduced thymic generation of natural Tregs and may also account for autoimmunity in DiGeorge syndrome, though Treg counts did not correlate with autoimmune disease.30,31
NF-κB2 insufficiency
PID due to damaging monoallelic variants in NFKB2 leads to immunodeficiency characterized by recurrent respiratory tract infections and failed control of herpesviruses.32 In addition to immunodeficiency, the vast majority (~80%) of patients display at least one autoimmune manifestation, including autoimmune cytopenias, arthritis, and alopecia. Studies on NF-κB2-deficient mice revealed the significance of the alternative NF-κB pathway in the induction of central tolerance, as NF-κB2 controls AIRE expression and is required for the development of mTECs.33,34 Therefore, the breakdown of tolerance in NF-κB2 deficiency mimics the pathophysiology of APECED. Mice harboring the Lym1 mutation in Nfkb2, which prevents the processing of the precursor protein of NF-κB2, displayed lung and liver autoimmune infiltrates associated with decreased thymic expression of Aire.35 Even in the context of haploinsufficiency, mice displayed similar though milder autoimmunity. These mouse-derived findings together with the phenotypic overlap between APECED and NF-κB2 insufficiency,32 suggest impaired induction in central tolerance as the main mechanism of autoimmunity. In addition, patients with NFKB2 mutations display reduced Treg counts.36,37 This, together with the fact that mice with conditional deletion of nfkb2 in Tregs develop lethal autoimmunity due to the impaired suppressive function of Tregs,38 suggests an additional Treg defect, which may be relevant in the pathogenesis of autoimmunity in NF-κB2 insufficiency.
Omenn syndrome
Omenn syndrome is a genetically heterogeneous disorder commonly linked to biallelic mutations in recombinase activating gene 1 (RAG1) or recombinase activating gene 2 (RAG2).39 Mutations in other genes involved in somatic V(D)J recombination, the process defining the B-cell and T-cell receptor repertoire, can result in Omenn-syndrome-like disease with generalized dermatitis and lymphadenopathy-associated with oligoclonal T-cell expansion. Given its genetic background, Omenn syndrome highlights an impaired T-cell repertoire as a mechanism of autoimmunity in primary immunodeficiency. The expression of AIRE is reduced in the thymus of patients with Omenn syndrome, suggesting aberrations of central tolerance and negative selection.40 Decreased suppressive function of Tregs has been reported in patients with Omenn syndrome and may represent an alternative or additional pathomechanism compromising tolerance.41
Regulatory T cells
Despite the dominant tolerogenic function of the thymus, the induction of central tolerance is incomplete.42 Significant numbers of autoreactive T cells that could trigger autoimmunity are detected in the circulation of healthy individuals, highlighting the significance of the mechanisms inducing peripheral tolerance (Fig. 2).43,44 Tregs are a major group of immunosuppressive T cells that play an essential role in the maintenance of peripheral immune tolerance and the regulation of immune responses. Treg dysfunction has been reported for a variety of autoimmune diseases, including type 1 diabetes (T1D), RA, multiple sclerosis (MS), SLE, myasthenia gravis, and systemic sclerosis.45 Forkhead box P3 (FOXP3) is indispensable for their development and function, and the most definitive evidence on the role of both FOXP3 and Tregs in the maintenance of tolerance came from genetic studies on Scurfy (Sf) mice, which display fatal multiorgan autoimmunity as a consequence of mutations in Foxp3.46
Inborn errors of immunity (IEI) impairing the induction of peripheral tolerance. In the absence of adequate costimulation, the recognition of self-antigens displayed by immature dendritic cells has a tolerogenic outcome, resulting in anergy or clonal deletion. Tissue damage, however, can break the ‘immune privilege’ at the tissue or subcellular level, facilitating the presentation of self-antigens. If this happens in a milieu supporting dendritic cell activation, such as in the presence of uncontrolled proinflammatory cytokine signaling or in the context of persistent infection or Treg dysfunction, an autoimmune T-cell response can be primed and result in the activation of autoreactive B cells. The source of B-cell autoreactivity is either aberrant central B-cell tolerance or de novo generation in the context of a germinal center reaction (not shown). Monogenic immunodeficiency disorders affect peripheral tolerance by enhancing the capacity of antigen-presenting cells to prime T cells, by compromising Treg function or reducing their counts, by enhancing antigen receptor-mediated activation of lymphocytes and/or by impairing tolerogenic aspects of antigen receptor signaling; monogenic disorders and the level at which they impair peripheral tolerance are highlighted in red [GOF gain-of-function, APDS activated PI3Kδ syndrome, DADA2 deficiency of ADA2]
Monogenic diseases resulting in Treg deficiency (Table 2) highlight the dominant tolerogenic role of Tregs. The prototype of so-called Tregopathies is immunodysregulation, polyendocrinopathy, enteropathy, and X-linked (IPEX) syndrome, which is caused by biallelic loss-of-function mutations in FOXP3; therefore, patients with IPEX syndrome are the human equivalent of Scurfy mice.46,47 To date, 111 different FOXP3 mutations, located throughout the FOXP3 gene, have been reported in patients with IPEX syndrome.48 No clear phenotype-genotype correlation has been identified, and those patients typically display a triad of clinical manifestations consisting of early-onset severe enteropathy, T1D, and dermatitis.49 Other autoimmune manifestations include autoimmune cytopenias, arthritis, autoimmune thyroiditis, nephropathy, and hepatitis.
CTLA-4 insufficiency
Cytotoxic T-lymphocyte protein 4 (CTLA-4) is a transmembrane protein expressed mainly by T cells.50 It interacts with CD80 and CD86 on the surface of antigen-presenting cells (APCs) and functions as a coinhibitory molecule. This interaction has a higher affinity than that of the costimulatory molecule CD28 with CD80 and CD86, counteracting its activating effect.51 Regulatory T cells constitutively express CTLA-4, whereas its expression on the plasma membrane of conventional T cells follows their activation. The balance between CD28 and CTLA-4 signaling is critical for the outcome of T-cell interactions with APCs, which may lead to either an effective adaptive immune response or a primarily tolerogenic response. CTLA-4-deficient mice die of early-onset multiorgan autoimmunity, demonstrating the dominant tolerogenic function of CTLA-4.52 In contrast, heterozygosity for the Ctla-4 knockout mutation has been reported to result in a normal phenotype.53 Therefore, it was not until the description of human CTLA-4 insufficiency that it became clear that not just the presence of CTLA-4 but also the amount of its expression by T cells is critical for immune homeostasis and the maintenance of immune tolerance.54 CTLA-4 insufficiency in humans compromises the function of Tregs, resulting in lymphoproliferation and autoimmunity.55 To date, more than 50 heterozygous germline mutations have been reported to account for CTLA-4 insufficiency in more than 130 patients.54 Autoimmune manifestations of CTLA-4 insufficiency resemble those of IPEX syndrome, including enteropathy, autoimmune cytopenias, arthritis, and endocrinopathy.56 However, incomplete penetrance and variable expressivity of genetic variants causing CTLA-4 insufficiency question the strictly monogenic origin of immune dysregulation in this disorder and suggest the influence of additional genetic or epigenetic modifiers and environmental factors.
LRBA deficiency
Lipopolysaccharide-responsive and beige-like anchor protein (LRBA) deficiency, due to germline biallelic mutations in LRBA, phenocopies CTLA-4 insufficiency.57,58 The explanation for this is the fact that LRBA controls intracellular trafficking of CTLA-4, and a loss of LRBA expression results in reduced expression and mobilization of CTLA-4 on the surface of Tregs. In addition to the impaired suppressive function of Tregs, which is at least partially explained by the reduction in CTLA-4 expression,59 the majority of LRBA-deficient patients display reduced Treg counts.60 Autoimmunity is reported to be the most common manifestation of LRBA deficiency and includes enteropathy, autoimmune cytopenias, endocrinopathy, interstitial lung disease, and/or autoimmune hepatitis. The CTLA-4-Fc fusion molecule (abatacept) has been reported to ameliorate manifestations of LRBA deficiency, such as enteropathy and lung disease, which strongly suggests that a loss of proper expression of CTLA-4 is a major pathogenic mechanism underlying immune dysregulation in these patients.57,61
DEF6 deficiency
The differentially expressed in FDCP 6 homolog (DEF6), also known as IRF4 binding protein (IRF4BP), is a guanine nucleotide exchange factor (GEF) that transmits TCR signaling.62 DEF6 activates small GTPases, promoting calcium signaling and T-cell adhesion, and it is involved in the formation of immunological synapses as well as in T-cell differentiation and proliferation. Def6 deficiency in murine autoimmunity appears to depend on the genetic background and/or the employed model of autoimmune disease.63,64 The recent discovery of human DEF6 deficiency, which manifests as systemic autoimmunity and lymphoproliferation, revealed the homeostatic role of DEF6 in the human immune system.65 Similar to LRBA deficiency, DEF6 deficiency causes a CTLA-4 trafficking defect, resulting in reduced stimulation-induced CTLA-4 expression by Tregs. The latter, together with the phenotypic overlap between DEF6 deficiency and LRBA deficiency or CTLA-4 insufficiency and the reported therapeutic efficacy of CTLA-4-Ig therapy (abatacept) in treating autoimmunity, suggest that a loss of proper trafficking of CTLA-4 is a major mechanism of immune dysregulation in DEF6 deficiency.
CD25 deficiency
CD25 is the α chain of the interleukin 2 receptor (IL-2Rα), and it is constitutively expressed by natural Tregs.66 CD25 confers high-affinity binding of interleukin 2 (IL-2) to the trimeric IL-2 receptor, additionally consisting of a β chain (CD122, IL-2Rβ) and the common γ chain (CD 132, IL-2Rγc), which both mediate receptor signaling. CD25 deficiency results in an IPEX-syndrome-like phenotype, with early-onset autoimmunity and lymphoproliferation but also severe immunodeficiency, causing chronic viral infections as well as fungal and bacterial infections.67,68 In all identified patients, CD25 expression was abrogated, which makes the isolation of Tregs and the evaluation of the impact of CD25 deficiency on Treg function difficult.47 However, the study of Tregs from patients with CD25 deficiency as CD4+CD45RO+TIGIT+CD127low T cells demonstrated both their reduced frequency and their suppressive function.69 The latter has been suggested to be mainly because CD25 deficiency deprives Tregs from their capacity to consume IL-2.67 Consistent with this, adoptive transfer of CD25+ Tregs into CD25-deficient mice drastically decreased serum levels of IL-2 and restored abnormalities in peripheral lymphocyte subsets, highlighting the homeostatic role of IL-2 consumption by Tregs in the immune system.70
BACH2 insufficiency
The broad complex-tramtrack-bric a brac and Cap'n'collar homology 2 (BACH2) is a basic leucine zipper domain transcription factor involved in the maturation and differentiation of both T cells and B cells.71 BACH2-regulated gene expression promotes Treg development at the expense of effector T-cell differentiation, as demonstrated in mice lacking BACH2.71,72 Further, it promotes the survival of Tregs, regulates their activation, and is required for the development and maintenance of tissue-resident Tregs, especially in the gastrointestinal tract.73 BACH2 insufficiency has been reported in three patients from two unrelated families who displayed benign lymphoproliferation, enteropathy, and recurrent respiratory tract infections.71 The identification of low counts of peripheral blood Tregs in these patients is consistent with previous reports on BACH2-deficient mice and suggests a similar role of BACH2 in human Treg development.
STAT5b deficiency
Signal transducer and activator of transcription 5b (STAT5b) deficiency results in a combined immunodeficiency with severe growth delay and immune dysregulation commonly manifesting as interstitial lung disease.43,74 Growth delay reflects the involvement of STAT5b in growth hormone signal transduction. In lymphocytes, STAT5 associates with the IL-2Rβ chain of IL-2R, and immune dysregulation is the consequence of the loss of IL-2R-mediated STAT5 activation, which is required for sustained FOXP3 expression and the development of natural Tregs.75 Further, STAT5 upregulates IL-2Rα, activating a positive feedback loop, which enhances Treg responsiveness to IL-2. Similar to CD25 deficiency, STAT5b-deficient patients display an IPEX-syndrome-like phenotype and have reduced circulating Treg counts with compromised suppressor function.74,76,77
STAT3 gain of function
Signal transducer and activator of transcription 3 (STAT3) is a transcription factor that transmits the signaling of several cytokine receptors, such as those of IL-2, IL − 6, IL − 10, IL − 12, IL − 15, and IL − 23, controlling T-cell activation and differentiation.78 STAT3 loss-of-function mutations account for autosomal-dominant hyper-IgE syndrome (HIES), which is a primary immunodeficiency characterized by very high serum IgE levels, atopic eczema, bacterial and fungal infections, and various nonimmune developmental manifestations.79,80 More recently, germline heterozygous gain-of-function mutations in STAT3 were reported to account for early-onset organ-specific autoimmunity, eczema, and short stature.81 Enteropathy, autoimmune cytopenias, interstitial lung disease, and lymphoproliferative and infectious manifestations are also common in patients with STAT3 gain of function.82 The phenotypic variability of this syndrome can be at least partially explained through the variable functional impact of the different disease-causing variants, which differentially affect baseline and induced activation of STAT3. In particular, in their recent study, Jägle et al. evaluated the biological impact of 17 different STAT3 gain-of-function variants and proposed their clustering in three main groups: variants causing enhanced basal transcriptional activity of STAT3 as well as altered inducible STAT3 phosphorylation, variants predominantly affecting inducible activation of STAT3 and those resulting in enhanced DNA binding of STAT3. STAT3 variants, both those enhancing baseline transcriptional activity and those affecting inducible phosphorylation of STAT3, have been reported to more consistently cause immune dysregulation, displaying the highest penetrance for autoimmune and/or lymphoproliferative disease. The majority of STAT3 gain-of-function mutations resulted in reduced peripheral Treg counts. Further, reduced suppressive function of Tregs has been reported for some patients.83,84 Mechanistically, STAT3 activation results in the upregulation of secretion of cytokine signaling 3 (SOCS3).85,86 The latter inhibits STAT5 activation, which—as discussed above—induces FOXP3 and CD25 expression. Therefore, the potentiation of this signaling loop through STAT3 hyperactivation results in decreased differentiation and function of Tregs, likely accounting for autoimmunity in patients with STAT3 gain of function.
DOCK8 deficiency
Dedicator of cytokinesis 8 (DOCK8) is a GEF that is highly expressed in lymphocytes.87 DOCK proteins activate small guanine triphosphate binding proteins (GTPases), such as RAC and CDC42, affecting the actin cytoskeleton. Germline biallelic loss-of-function mutations in DOCK8 cause an autosomal-recessive form of HIES. In comparison to other monogenic PIDs, mutations in DOCK8 are common deletions. An explanation for this is the high frequency of repetitive sequence elements within and around DOCK8. In addition to infectious manifestations, including candidiasis, recurrent respiratory tract infections, and persistent cutaneous viral infections, DOCK8 deficiency has been associated with immune dysregulation manifesting as autoimmunity and atopy.87,88 Autoimmunity in DOCK8 deficiency has been reported to manifest as vasculitis, autoimmune hepatitis, or IPEX-syndrome-like disease. The identification of an increased proportion of autoreactive B cells within the compartment of mature naïve B cells in DOCK8-deficient patients suggests a defect in peripheral tolerance.89 Incomplete induction of peripheral tolerance and autoimmunity in DOCK8 deficiency reflects the involvement of DOCK8 in Treg homeostasis and function. Consistent with the aforementioned is the fact that patients with DOCK8 deficiency display low Treg counts with reduced suppressive function, though the exact mechanism accounting for this remains unknown.89
IRF4 deficiency
Interferon regulatory factor 4 (IRF4) is involved in T helper cell polarization and is required for the effector function of Tregs as it controls IL-10 and ICOS expression.90 Further, IRF4 expression by thymic epithelial cells is critical for efficient priming of natural Tregs.91 IRF4-deficient mice display progressive immune dysregulation and severe hypogammaglobulinemia.92 The first description of human IRF4 deficiency due to a germline homozygous splice acceptor site mutation in IRF4 has been recently reported and resembles the phenotype of IRF4-deficient mice.93 This patient displayed agammaglobulinemia and early-onset autoimmunity manifesting as polyendocrinopathy, including T1D, and displayed a low Treg count. She additionally suffered from eczema and died at the age of 2 years after allogeneic hematopoietic stem cell transplantation.
PI3Kδ deficiency
The relatively recently characterized IEI due to germline biallelic loss-of-function mutations in PIK3CD or PIK3R1 results in immunodeficiency, primarily due to severe hypogammaglobulinemia, as well as autoimmunity in the form of arthritis, psoriasis, and inflammatory bowel disease (IBD), most likely as a consequence of the compromised suppressive function of Tregs.94,95,96 In particular, mouse studies have suggested the involvement of PI3Kδ in the development and suppressive function of Tregs.97,98,99 However, as mentioned previously, all tested patients with biallelic mutations in PIC3CD or PIK3R1, resulting in a loss of PI3Kδ activity, had adequate Treg counts in their peripheral blood. The fact that the PI3Kδ-specific inhibitor idelalisib compromises the suppressive function of Tregs in vitro and ex vivo in patients with chronic lymphocytic leukemia,100 together with the fact that common side effects of idelalisib treatment resemble the inflammatory manifestations of a loss of PI3Kδ activity,101 strongly suggest immune dysregulation owing to the inadequate suppressive function of Tregs in this IEI.94
Aberrant T-cell receptor (TCR) signaling
TCR signaling controls the development and peripheral responses of T cells, ensuring both effective immunity and immune tolerance.102 TCR signaling defects could compromise central tolerance by affecting negative selection of autoreactive T cells. In addition, aberrant TCR signaling can affect the development and function of regulatory T cells, impairing the induction of peripheral tolerance. Finally, mutations in molecules involved in the TCR signaling cascade may result in autoimmunity by hyperactivating autoreactive T cells or depriving TCR signaling from tolerogenic aspects, such as the induction of anergy or activation-induced cell death.
ORAI1/STIM1 deficiency
The pathway of store-operated calcium entry (SOCE) is the main mode of calcium influx in immune cells and is involved in TCR, B-cell receptor (BCR), Fc gamma receptor (FcγR), and Fc epsilon receptor (FcεR) signaling as well as downstream effector responses.103,104 SOCE is activated in response to the depletion of intracellular stores of calcium, particularly of the endoplasmic reticulum. Stromal interaction molecule 1 (STIM1) has been identified as the major calcium sensor in the ER membrane that activates calcium channels in the plasma membrane upon calcium store release. Orai1 is the major calcium channel activated by STIM1 in most immune cells, especially in B cells and T cells.
Biallelic loss-of-function mutations in STIM1 and ORAI1, leading to STIM1 or ORAI1 deficiency, respectively, manifest with combined immunodeficiency and autoimmunity in the form of autoimmune hemolytic anemia and thrombocytopenia.104 Patients with STIM1 deficiency, as well as those with ORAI1 deficiency, display reduced Treg counts.105,106 The role of store-operated calcium entry (SOCE) in the development of regulatory T cells has been demonstrated in mice with T-cell-targeted deletion of both STIM isoforms, which have reduced peripheral and tissue-resident Tregs and develop autoimmunity and lymphoproliferation.107,108 While a reduction in Treg counts could explain autoimmunity in those patients, even in the case of STIM1 deficiency, which is more consistently associated with immune dysregulation, patients do not display an IPEX-syndrome-like phenotype. Impaired negative selection may also contribute to autoimmunity, though the normal Vβ repertoire of TCRαβ+ T cells in patients with STIM1 mutations suggests the absence of major defects in the induction of central tolerance.109,110 The recently reported regulatory function of STIM1 in controlling type I interferon responses111 could also be relevant in the pathogenesis of autoimmunity, at least in STIM1-deficient patients, and is consistent with the SLE-like autoantibody profile detected in these patients.105
Activated phosphoinositide 3-kinase δ syndrome
Phosphoinositide 3-kinase delta (PI3Kδ) mediates signal transduction downstream of diverse immune receptors, including the TCR, the BCR, costimulatory molecules, and cytokine receptors.94 The hyperactivation of PI3Kδ due to monoallelic gain-of-function mutations in PIK3CD or due to monoallelic loss-of-function mutations in PIK3R1 or PTEN results in immunodeficiency and immune dysregulation.112,113 In particular, the hyperactivation of PI3Kδ results in combined immunodeficiency, characterized by recurrent respiratory tract infections, bronchiectasis, mucocutaneous candidiasis, and susceptibility to viral infections, including failed control of herpesviruses.
Immune dysregulation as a consequence of the hyperactivation of PI3Kδ leads to benign lymphoproliferation, manifesting as lymphadenopathy, hepatomegaly, splenomegaly, and nodular lymphoid hyperplasia of mucosal surfaces as well as malignant lymphoproliferative disease and especially B-cell lymphomas. Further, patients with immune dysregulation due to the hyperactivation of PI3Kδ display a broad spectrum of autoimmune manifestations, including cytopenias, endocrinopathies, glomerulonephritis, and Sjögren’s syndrome. Immune dysregulation in patients with hyperactivated PI3Kδ is most likely the consequence of the hyperactivation of T cells.94,112,113,114 Studies on mice with hyperactivated PI3Kδ suggest defects in thymic negative selection but also ineffective peripheral tolerance due to resistance to activation-induced cell death and increased secretion of effector cytokines by T cells, which has also been demonstrated in patients with activated phosphoinositide 3-kinase δ syndrome (APDS).
ITCH E3 ubiquitin ligase deficiency
The ubiquitination of TCRs reduces their expression and therefore regulates T-cell activation.115 Itchy E3 ubiquitin-protein ligase, referred to hereafter as Itch, is a key tolerogenic molecule involved in this process. In addition to TCR subunits, Itch is involved in the ubiquitination of molecules involved in proximal TCR signaling, such as the TCRζ chain and mitogen-activated protein kinase kinase1 (MEKK1). In addition, Itch regulates Notch, a transcription factor promoting TCR signaling. The dysregulation of TCR-Notch signaling can drive both lymphoproliferation and autoimmunity.116 Itch-deficient T cells have a lower activation threshold, which, in the case of autoreactive T cells, could enhance their activation and prevent tolerogenic mechanisms, such as their conversion into anergic T cells.115 In addition to controlling T-cell activation, evidence from Itch-knockout mice suggests the direct involvement of Itch in regulating proinflammatory NF-κB activation in response to TNF or IL-1.117 Biallelic mutations in itchy E3 protein ubiquitination ligase (ITCH) result in syndromic polyautoimmunity and immunodeficiency, highlighting the regulatory role of ubiquitination in controlling TCR signaling and regulating inflammation.118,119 Patients with Itch defects display recurrent infections, including bacterial sepsis; however, clinically more prominent is their craniofacial dysmorphism and immune dysregulation, resulting in hepatosplenomegaly, interstitial lung disease, enteropathy, autoimmune hepatitis, and endocrinopathy, including hypothyroidism and T1D.
Biallelic loss-of-function mutations in LAT
Biallelic loss-of-function mutations in LAT, the gene encoding linker for activation of T cells (LAT), result in early-onset combined immunodeficiency and autoimmunity.120 In particular, those patients suffer from recurrent pneumonias, bronchiectasis, and herpesvirus infections, especially due to EBV or CMV. Immune dysregulation manifests as lymphadenopathy, splenomegaly, interstitial lung disease, and autoimmune cytopenia. Mechanistically, mutant LAT prevented TCR-downstream phosphorylation of phospholipase Cγ1 (PLCγ1). Mouse studies preceding the identification of the human PID due to biallelic LAT mutations have revealed the tolerogenic importance of TCR-induced docking PLCγ1 on LAT.121 In particular, mice harboring a homozygous mutation replacing the docking site of PLCγ1 on LAT, i.e., the tyrosine residue at position 136 of LAT, displayed lethal lupus-like autoimmunity. T cells from these mice displayed enhanced TCR-mediated activation. Further studies on these mice suggested that the uncoupling of LAT-PLCγ1 signaling may alter thymocyte selection, resulting in thymic release of autoreactive T cells, which would otherwise be eliminated through negative selection.122
Biallelic loss-of-function mutations in LCK
Autosomal-recessive deficiency of lymphocyte-specific protein tyrosine kinase (LCK) has been reported in a girl with early-onset recurrent respiratory tract infections, including pneumonia complicated by pneumatocele.123 This patient additionally displayed neutrophilic panniculitis, polyserositis, and recession after the introduction of a TNF inhibitor and ITP, suggesting immune dysregulation. In addition to defects in thymic selection of T cells as a consequence of aberrant TCR signaling, LCK deficiency appears to result in resistance to activation-induced cell death and reduced Treg counts.
Biallelic loss-of-function mutations in CD3G
Finally, autosomal-recessive CD3γ deficiency results in variable immunodeficiency, more commonly manifesting with hypogammaglobulinemia and recurrent respiratory tract infections.124,125 So far, all ten reported patients with CD3γ deficiency displayed autoimmune disease, most commonly manifesting as hypothyroidism and autoimmune cytopenias. Autoimmunity in CD3γ deficiency has been suggested to stem from thymic release of autoreactive T cells and in parallel Tregs with limited TCR diversity and reduced suppressive function.124,125
Complement deficiencies causing autoimmunity
Complement deficiencies, especially those of early components of the complement activation cascade, can lead to both recurrent infections and autoimmunity.12 Early classic complement deficiencies (C1, C2, or C4) cause susceptibility to infections with encapsulated bacteria and are frequently associated with autoimmunity, especially SLE.126,127 A deficiency of C4 or any of the components of the C1 complex results more commonly in SLE than C2 deficiency (88% of patients with C1q deficiency, 75% in the case of C4 deficiency, 57% of those with C1s/r vs. 10% in the case of C2 deficiency). Further, SLE associated with C4 or one of the C1 complex deficiencies displays an earlier onset and more severe disease course than C2 deficiency-associated SLE.126,128 Defects in the lectin pathway of complement activation can also cause or contribute to the pathogenesis of autoimmunity. Mannose-binding lectin (MBL) deficiency has a prevalence of 5% and is the most common complement deficiency.129 A deficiency of MBL increases the risk of pyogenic infections, especially in infants. In addition, it is associated with an increased risk for autoimmunity.130 Mannan-binding lectin-associated serine protease 2 (MASP-2) activates the lectin pathway of complement, assuming a role analogous to that of C1s/C1r in classic activation of complement. In addition to susceptibility to infections, MASP-2 deficiency results in SLE-like autoimmunity.131 Early complement components are implicated in the effective clearance of self-antigens, exposing apoptotic cells and immune complexes.12,130 Defects in both of these processes can lead to autoimmunity or contribute to its pathogenesis.
Immune dysregulation due to apoptosis defects
Lymphocyte expansion in the context of an adaptive immune response is controlled by apoptosis. Human defects in apoptosis leading to autoimmune lymphoproliferative disease (ALPS) highlight the homeostatic role of apoptosis-mediated clonal contraction.132
ALPS typically presents with chronic benign lymphoproliferation (lymphadenopathy, splenomegaly, and hepatomegaly), which may be accompanied by autoimmune cytopenias.133,134 Immune dysregulation in ALPS may also manifest with uveitis, thyroiditis, hepatitis, or SLE-like disease. Further, ALPS patients display an increased incidence of lymphoid malignancies. Susceptibility to infections is rare, mostly attributed to splenectomy or autoimmune neutropenia.135 Patients with Fas deficiency typically display marked elevations in CD4-CD8- double-negative T cells.136 Other typical laboratory findings include elevated vitamin B12, IL-10, and soluble Fas ligand (FasL/CD95L) levels. Although polyclonal hypergammaglobulinemia is also relatively common in ALPS, less than 10% of patients display hypogammaglobulinemia, which in some cases may be associated with previous immunosuppressive treatment.137 The diagnosis of ALPS is based on clinical and laboratory findings (Table 3A).
Immune dysregulation in ALPS is attributed to defects in lymphocyte apoptosis and especially aberrations in Fas-mediated extrinsic apoptosis.138,139 T-cell activation induces the expression of FasL, which binds Fas on nearby cells, including T cells. Fas is a death receptor containing intracellular death domains. The activation of Fas leads to the formation of the death-inducing signaling complex, which recruits and activates caspases 8 and 10, which are initiator caspases of the extrinsic apoptotic pathway. The majority of ALPS patients harbor heterozygous germline mutations in FAS (Table 3B).134 Incomplete penetrance and variable expressivity of the same FAS variants suggest the role of additional genetic modifiers.140 Consistent with the latter is the observation of an additional somatic FAS mutation accounting for a more severe phenotype in some patients.141,142 Germline mutations in the genes encoding FasL (FASLG) or caspase 10 (CASP10) have been identified in a small subgroup of patients with ALPS.133,134,143 The identification of NRAS and KRAS mutations in patients with ALPS and a propensity for hematopoietic malignancies suggests that in addition to extrinsic apoptosis, defects in the intrinsic apoptotic pathway can cause immune dysregulation.144,145
Type i interferon-mediated immune dysregulation
Type I interferons have numerous effects on the innate and adaptive immune systems.146 In particular, they modulate antigen-presenting function; promote inflammation, apoptosis, myeloid cell activation, and B-cell differentiation; and affect the function of several cells, such as microglial and endothelial cells. The activation of type I interferon-mediated responses can contribute to the pathomechanism of autoimmunity. Type I interferonopathies are a group of monogenic disorders caused by abnormal upregulation of type I interferons and typically manifest as vasculopathy, early-onset SLE or myositis.147,148 Known type I interferonopathies and their main clinical findings are listed in Table 4. Type I interferonopathies reflect the pathogenic role of constitutive activation of type I interferon-mediated immune responses.146,147 Defects in nucleic acid sensing, including the chemical modification or clearance of self-nucleic acids, deregulated activation of nucleic acid sensors and defects in molecules or pathways that regulate type I interferon signaling, can all result in diseases falling under type I interferonopathies. For example, mutations in genes encoding nucleases, such as TREX1 and RNase H2, which cause the prototype type I interferonopathy, Aicardi-Goutières syndrome (AGS), suggest the pathogenic role of the accumulation of self-nucleic acids, which results in systemic inflammation and autoimmunity by activating type I interferon responses.
STAT1 gain of function
Signal transducer and activator of transcription 1 (STAT1) is involved in both type I (IFNα and IFNβ) and type II (IFNγ) interferon receptor signaling.149 The activation of the IFNγ receptor results in phosphorylation and STAT1, which forms a homodimer that translocates in the nucleus, where it induces IFNγ-regulated genes. Stimulation with type I interferons in addition to STAT1 homodimers results in the formation of a STAT1-STAT2 and p48 (ISGF3G) heterotrimer that transactivates type I interferon-regulated genes, whose collective induction is referred to as the type I interferon signature. Heterozygous gain-of-function mutations in STAT1 result in immunodeficiency, typically manifesting as chronic mucocutaneous candidiasis (CMC).150 However, a significant proportion of patients (37%) display autoimmune manifestations, including endocrinopathy, autoimmune cytopenia, and SLE. STAT1 gain-of-function mutations do not affect the expression of FOXP3 or CTLA-4 or the development of Tregs.151 Despite the phenotypic overlap between APECED and immunodeficiency due to STAT1 gain of function, there is no evidence of a pathomechanistic connection between these two monogenic disorders. Considering the phenotypic similarities of interferonopathies such as SLE and the fact that treatment with interferon α results in endocrinopathy (such as thyroiditis), enhanced cytokine and interferon responses provide a plausible pathomechanism accounting for autoimmunity in the context of STAT1 gain of function.152,153 The recently identified enhanced expression of interferon signature genes in patients with STAT1 gain-of-function mutations154 is in accordance with the aforementioned hypothesis. Although, so far, there is no clear genotype-phenotype correlation, considering the varying gain-of-function effect of STAT1 variants, it would be interesting to evaluate whether autoimmunity associates with STAT1 variants resulting in stronger interferon signaling.
Deficiency of ADA2
Patients with a deficiency in adenosine deaminase 2 (ADA2) due to biallelic loss-of-function mutations in CECR1 display varying immunodeficiency mainly associated with hypogammaglobulinemia but also early-onset polyarteritis nodosa.155,156 The severity of polyarteritis nodosa in those patients ranges from cutaneous vasculitis to organ involvement, including early-onset and/or recurrent strokes. ADA2 is mainly expressed by myeloid cells and catalyzes the conversion of adenosine and 2′-deoxyadenosine to inosine and deoxyinosine, respectively. In contrast to adenosine deaminase 1 (ADA1), whose deficiency results in SCID, ADA2 has a considerably lower affinity for its substrates and is not acting intracellularly but is rather secreted. Phenotypic similarities between ADA2 deficiency (DADA2) and type I interferonopathies, such as AGS, suggest a shared pathogenic background.157 In accordance with this is the fact that DADA2 patients display a type I interferon signature correlating with disease activity, as shown in transcriptome analysis of their peripheral blood cells.157,158 The identification of DADA2 as a monogenic form of polyarteritis nodosa suggests that defects in adenosine catabolism result in inflammation by inducing the production of type I interferons.
B-cell-intrinsic defects
Autoreactive B cells are subject to the mechanisms of central tolerance, which are deployed within the bone marrow and include clonal deletion and receptor editing.1,159 However, similar to T cells, the central tolerance of B cells is incomplete, and as a consequence, a considerable proportion of B cells escaping the bone marrow are autoreactive. The frequency of autoreactive B cells decreases along the course of B-cell maturation, falling from the staggering level of more than 55% within the population of early immature B cells to ~20% within mature B cells.1,160,161 The control of this sizable proportion of autoreactive mature B cells can be achieved through anergy, clonal ignorance, clonal deletion, and receptor revision. Somatic hypermutation in the context of the germinal center reaction can convert previously nonautoreactive cells into autoreactive cells. Germinal center checkpoints are employed in this case to prevent the breakdown of tolerance and are largely the mechanism inducing T-cell tolerance. T cells are gatekeepers of B-cell tolerance, and mechanisms of T-cell tolerance are relevant for the induction of B-cell tolerance.
Autosomal-recessive AID deficiency
Activation-induced cytidine deaminase (AID) catalyzes the deamination of cytosine into uracil, creating DNA mutations, and AID is involved in immunoglobulin class-switch recombination (CSR) and somatic hypermutation.162 Biallelic mutations in AICDA result in AID deficiency, which is the most common B-cell-intrinsic CSR defect.163,164 Autosomal-recessive AID deficiency causes hyper-IgM syndrome with low IgG and IgA levels. Apart from recurrent bacterial infections, reflecting antibody failure, the majority of patients display lymphadenopathy, and ~30% develop autoimmunity, presenting as autoimmune cytopenia, SLE, arthritis, autoimmune hepatitis, and Crohn’s disease. Autoimmunity in AID deficiency is a B-cell-intrinsic defect.165 Both defects in central and peripheral tolerance have been described, though the exact mechanism accounting for B-cell autoreactivity is not clearly understood. The resistance of B cells to apoptosis and the overexpression of BAFF could result in the skipping of the checkpoints of B-cell tolerance in these patients.166 An additional pathogenic correlate of autoimmunity in AID deficiency is the reduction in Treg counts, which may be explained through a T-cell-intrinsic mechanism, as T cells have been reported to transiently express AID.167 Further, the presentation of autoantigens by autoreactive B cells has been suggested as an alternative mechanism promoting the activation of autoreactive T cells.168
PKCδ deficiency
Protein kinase C δ (PKCδ) is a lymphocyte and primarily B-cell signaling mediator.169 PKCδ is phosphorylated in response to the activation of the BCR B-cell activating factor (BAFF) or in response to cytokines such as IL-4 and interferons. PKCδ-mediated signaling in B cells regulates their survival, proliferation, and apoptosis, including the proapoptotic pathway resulting in negative selection. Biallelic loss-of-function mutations in PRKCD, the gene encoding PKCδ, either result in PKCδ deficiency or affect its phosphorylation; in addition, these mutations cause immunodeficiency with variable immunoglobulin values and consistently reduced counts of class-switched memory B cells, characterized by immune dysregulation.170,171,172,173 Six patients from four unrelated families have been reported to develop disease as a consequence of biallelic PRKCD mutations. All of these patients developed autoimmunity before the age of 10 years, commonly manifesting as SLE or SLE-like disease, including photosensitivity and nephritis, arthritis, and antiphospholipid syndrome. The critical role of PKCδ in B cell homeostasis and tolerance, especially in negative selection in germinal centers, has been identified in PKCδ-deficient mice, which – similar to patients with PKCδ deficiency—display lymphoproliferation and systemic autoimmunity.174
Uncontrolled infections and autoimmunity: The example of failed control of ebv and mycobacteria
Pathogens of all kinds can cause tissue damage and elicit both innate and adaptive immune responses that not only eliminate them but also may result in the breakdown of tolerance.175,176,177 The mechanisms by which infections can trigger or accelerate autoimmunity have been extensively reviewed elsewhere.178,179,180 Briefly, mechanisms accounting for infection-triggered autoimmunity include the release of self-antigens, enhanced antigen presentation, bystander activation, superantigen-induced immune activation, and molecular mimicry. Mechanistic insight into the pathogenesis of autoimmunity has been gained through animal models of autoimmune disease, which also provides a platform for the evaluation of the role of particular viruses and bacteria in the initiation and maintenance of autoimmunity.181 Epidemiological studies have associated several autoimmune diseases, such as T1D, RA, SS, and SLE, with viral or bacterial infections.182,183,184,185,186 Further, pathogen-derived antigens have been identified in tissues or cells of patients with autoimmune diseases,182,185 and sequence similarities between pathogen-derived epitopes and self-antigen-derived epitopes that could elicit cross-reacting immune responses have been identified in numerous autoimmune diseases.187,188,189,190 Given the evidence suggesting the role of infections in precipitating autoimmunity, it is tempting to speculate that, at least in some IEI, susceptibility to infections, and especially chronic or persistent infections, may precipitate autoimmunity. As this is an extremely broad topic that should be addressed with a pathogen-specific approach, we will focus here on EBV, whose failed control is a hallmark of T-cell immunodeficiency and atypical mycobacterial infections, which are associated with Mendelian susceptibility to mycobacterial disease (MSMD).
Several lines of evidence connect EBV with autoimmunity. Epidemiological studies have associated EBV with autoimmune diseases such as RA, SLE and multiple sclerosis (MS).178,190 EBV-induced infectious mononucleosis has been suggested to induce the production of various autoantibodies, such as those against DNA, ribonucleoproteins, and erythrocytes.182,191,192 Further, EBV-derived proteins and nucleic acids have been more commonly identified in patients with SLE. In SLE patients, it has been shown that EBV-specific CD8+ T cells are diminished and less cytotoxic.193,194 Decreased CD8+ T-cell activity against EBV-infected B cells has been suggested to account for the accumulation of EBV-infected B cells in MS.195 RA patients displayed decreased percentages of IFNγ-producing EBV-specific CD8+ T cells.196 The abovementioned findings link defective control of EBV with autoimmunity. Several IEI primarily compromise the handling of EBV.197 For example, mutations in ITK, CD27, MAGT1, and CORO1A result in failed control of EBV infection and EBV-driven lymphoproliferation.198 Autoimmunity is neither a cardinal nor an early-onset feature of most of those disorders and has been reported in a minority of patients with ITK deficiency or X-linked immunodeficiency with magnesium defect, EBV infection and neoplasia (XMEN) syndrome who more commonly developed autoimmune cytopenia.199,200 Considering the plausible epidemiological and biological evidence of the role of EBV in autoimmunity, it can be speculated that EBV-driven mechanisms in the context of failed EBV control can at least partially induce the breakdown of tolerance in PIDs that selectively affect immune responses against EBV.
Mycobacterial infections, especially with nontuberculous mycobacteria, can induce autoantibody responses, such as those found in SLE, RA, and systemic vasculitis, and M. tuberculosis-derived antigens, such as heat shock protein 60 (HSP60) and HSP65, have been identified in the sera of patients with SLE.201,202,203 Nontuberculous mycobacterial infections have a relatively high prevalence among SLE patients.204 Epidemiological studies revealed a significant association of SjS with a history of previous nontuberculous mycobacterial infection.205 In addition to molecular mimicry, persistent antigenic stimulation in the context of mycobacterial infection could activate innate immune sensors and lower the activation threshold of autoreactive T cells.202 Common IEI resulting in MSMD,206 such as interleukin 12 receptor beta 1 (IL12Rβ1) or interferon γ receptor 1 (IFNγR1) deficiency, has only rarely been linked to autoimmunity, which manifests as SjS or SLE-like disease.207,208,209,210 The relatively low proportion of patients with monogenic defects in the IL-12/IFNγ axis and autoimmunity (3.4% among patients with IL12Rβ1 deficiency)207 suggests an additional genetic predisposition to autoimmunity other than the MSMD-causing genetic variation. Given the evidence suggesting that mycobacteria can precipitate autoimmunity, persistent mycobacterial infection may at least in part account for the breakdown of tolerance in these patients.
Multifactorial immune dysregulation: the example of IEI due to defects in the canonical NF-κB pathway
The activation of NF-κB transcription factors, especially those of the canonical pathway, plays a central role in the immune system and is a ubiquitous target of immune signaling211; therefore, it is discussed separately in this review. Diverse immune receptors, including antigen receptors, Toll-like receptors (TLRs), members of the tumor necrosis factor receptors (TNFRs) and the interleukin 1 receptor (IL-1R), activate the canonical NF-κB pathway, which converges in the nuclear translocation of an NF-κB dimer, which consists of c-Rel, RelA/p65 and/or p50.211 Heterozygous loss-of-function mutations in NFKB1, the gene encoding the precursor of p50, i.e., NF-κB1/p105, are the most common monogenic cause of CVID in Europeans, and, in addition to immunodeficiency, they are commonly associated with autoimmunity.212 More than half of patients with immunodeficiency due to damaging monoallelic NFKB1 mutations display autoimmune manifestations such as autoimmune cytopenias, arthritis, enteropathy, and vasculitis, and the frequency of autoimmunity increases with age.213,214 Heterozygous gain-of-function mutations in NFKBIA, the gene encoding the “nuclear factor of kappa light polypeptide gene enhancer in B cells inhibitor alpha” (IκBα), block IκBα degradation and therefore NF-κB1 release from its complex with IκBα and nuclear translocation, having a loss-of-function effect on the canonical NF-κB pathway.215 Approximately half of all 19 reported patients with PID due to NFKBIA mutations displayed autoimmune or autoinflammatory disease manifesting as SLE, RA, IBD, or hepatopathy.215,216,217,218,219
Despite mouse studies suggesting the involvement of the canonical NF-κB pathway in the development and function of Tregs,220,221 both Treg counts and in vitro suppressive function appear normal in tested patients with immunodeficiency due to monoallelic NFKB1 mutations.222 However, a recent study revealed reduced expression of ICOS in Tregs from all 5 tested patients with NFKB1 haploinsufficiency, which is consistent with the reduced effector function of Tregs.223 Those patients displayed reduced Treg counts, deviating from the rest of patients with monoallelic NFKB1 mutations,222 so it is unclear whether all pathogenic NFKB1 mutations consistently impair Treg counts or function and whether this is associated with autoimmune disease. Dysregulated stimulation-induced cytokine secretion and especially increased production of TNF can result in autoimmunity.224 Increased production of TNF has been described in patients with heterozygous NFKB1 mutations and may be an additional or alternative explanation for autoimmune or autoinflammatory disease in the context of immunodeficiency due to heterozygous NFKB1 mutations. Myeloid cell hyperactivation and the oversecretion of IL-1b have been reported to be the consequence of a recently identified gain-of-function NFKBIA mutation in a patient with autoinflammatory hepatopathy.219 Another mutation in NFKBIA, replacing Ser32, did not cause the oversecretion of IL-1β.225 However, the patient’s leukocytes displayed reduced LPS-induced production of all other tested proinflammatory cytokines (IL-6 and TNFα), except IL-1β, supporting the idea of a cytokine imbalance favoring IL-1β production as the cause of inflammatory disease in these patients.
The activation of the canonical NF-κB pathway, especially after triggering TCR or BCR, is controlled by the assembly of a protein complex consisting of CARD11, BCL-10, and MALT1, the so-called CBM signalosome.226 Germline mutations in the genes encoding the components of the CBM signalosome result in a broad spectrum of immunological phenotypes, including combined immunodeficiency, atopy, and autoimmunity, which is more clearly linked with Treg dysfunction. Germline gain-of-function mutations in CARD11 underlie B-cell expansion with NF-κB and T-cell anergy (BENTA) disease, which is a PID with recurrent respiratory tract and viral infections such as molluscum contagiosum and EBV viremia.227 BENTA patients also display autoimmune lymphoproliferative syndrome (ALPS)-like lymphoproliferation and SLE-like autoimmunity, including autoimmune cytopenias. Most BENTA-causing mutations are located in the coiled-coil or the LATCH domain of CARD11, interrupting the autoinhibitory interaction with the linker domain, resulting in CARD11 aggregation, the recruitment of BCL-10 and MALT1 and constitutive NF-κB activation in B cells and T cells.226,228 Interestingly, dominant-negative (DN) CARD11 mutations disrupting NF-κB activation have also been associated with autoimmunity.229 In addition to severe atopic disease, ~20% of patients with DN CARD11 mutations display autoimmunity manifesting as alopecia, idiopathic thrombocytopenic purpura, bullous-pemphigoid, or even IPEX-like disease. Although severe opportunistic infections (particularly Pneumocystis pneumonia) dominate the phenotype of combined immunodeficiency due to biallelic loss-of-function mutations in CARD11, Omenn syndrome and IBD have been reported as manifestations of PID due to full CARD11 deficiency, which results in compromised activation of the canonical NF-κB pathway and an absence of Tregs.226,230 MALT1 deficiency, as a consequence of germline biallelic loss-of-function mutations in MALT1, causes CID, including IPEX-syndrome-like immune dysregulation, which is associated with substantially reduced Treg counts.231 The IPEX-syndrome-like autoimmunity of MALT1-deficient patients is in accordance with the phenotype of mice harboring a point mutation that selectively inactivates the paracaspase activity of MALT1, which also display reduced Treg counts and die of multiorgan autoimmunity.232 BCL10 deficiency, similar to MALT1 deficiency, causes an IPEX-syndrome-like phenotype associated with profound Treg deficiency.233
Concluding remarks
Autoimmunity is an integral part of the clinical spectrum of PIDs or IEI. In this review, we have presented the cellular and molecular mechanisms accounting for the breakdown of tolerance to self-antigens in selected IEI (Figs. 1 and 2).
The age of onset and the type of autoimmunity depend largely on the genetic defect underlying an IEI and its impact on both immunity and tolerance. Major defects in thymic negative selection commonly cause early-onset polyendocrinopathy and cutaneous autoimmunity, whereas major defects in Treg-induced peripheral tolerance typically manifest with early-onset enteropathy, endocrinopathy, and eczema. Several genetic defects, especially those affecting antigen receptor signaling or nodal signaling molecules, can simultaneously impair more than one layer of tolerance. On the other hand, unresolved infections may directly affect tolerogenic lymphocyte functions or exert a persisting adjuvant effect on immune cells, precipitating the breakdown of tolerance. The latter may be relevant for monogenic immune defects that predominantly compromise immunity and are associated with a lower prevalence and a later onset of autoimmunity.
Autoimmunity can be the prominent or the first manifestation of an IEI.10 In the case of the latter scenario, the diagnosis of primary immunodeficiency may be missed, as patients may receive glucocorticoids or other immunomodulatory agents inducing secondary immunodeficiency.234 The increasing number of genes linked to IEI facilitates an understanding of the immunopathogenesis of autoimmune disease, affecting therapeutic decision-making or even allowing the development of individualized therapies. The emerging identification of genes both involved in IEI and conferring susceptibility to systemic autoimmune diseases, as well as the increasing identification of autoantibodies and other intrinsic autoimmune disease mechanisms compromising immunity, strongly suggest the interconnectedness of the pathogenic pathways of autoimmunity and primary immunodeficiency (Fig. 3).235,236,237 Therefore, the identification of the mechanisms breaking immune tolerance in IEI may aid in the understanding of the pathophysiology of systemic autoimmune diseases and contribute to the development of pathophysiology-oriented therapeutics.
The interconnected pathogenic pathways of autoimmunity and primary immunodeficiency. Autoimmune disorders may result in immunodeficiency through the production of autoantibodies or through disease-intrinsic mechanisms, whereas the immune defects underlying immunodeficiency can affect the induction or the maintenance of immune tolerance and cause autoimmunity
References
Theofilopoulos, A. N., Kono, D. H. & Baccala, R. The multiple pathways to autoimmunity. Nat. Immunol. 18, 716–724 (2017).
Imgenberg-Kreuz, J., Rasmussen, A., Sivils, K. & Nordmark, G. Genetics and epigenetics in primary Sjögren’s syndrome. Rheumatology (Oxford). https://doi.org/10.1093/rheumatology/key330. (2019).
Okada, Y., Eyre, S., Suzuki, A., Kochi, Y. & Yamamoto, K. Genetics of rheumatoid arthritis: 2018 status. Ann. Rheum. Dis. 78, 446–453 (2019).
Demirkaya, E., Sahin, S., Romano, M., Zhou, Q. & Aksentijevich, I. New horizons in the genetic etiology of systemic lupus erythematosus and lupus-like disease: monogenic lupus and beyond. J. Clin. Med. 9, 712 (2020).
Ishigaki, K., Kochi, Y. & Yamamoto, K. Genetics of human autoimmunity: From genetic information to functional insights. Clin. Immunol. 186, 9–13 (2018).
Bousfiha, A. et al. Human inborn errors of immunity: 2019 update of the IUIS phenotypical classification. J. Clin. Immunol. 40, 66–81 (2020).
Gruber, C. & Bogunovic, D. Incomplete penetrance in primary immunodeficiency: a skeleton in the closet. Hum. Genet. 139, 745–757 (2020).
Delmonte, O. M., Castagnoli, R., Calzoni, E. & Notarangelo, L. D. Inborn errors of immunity with immune dysregulation: from bench to bedside. Front. Pediatr.7, 353 (2019).
Grimbacher, B., Warnatz, K., Yong, P. F. K., Korganow, A. S. & Peter, H. H. The crossroads of autoimmunity and immunodeficiency: Lessons from polygenic traits and monogenic defects. J. Allergy Clin. Immunol. 137, 3–17 (2016).
Sogkas, G. et al. High frequency of variants in genes associated with primary immunodeficiencies in patients with rheumatic diseases with secondary hypogammaglobulinaemia. Ann. Rheum. Dis. https://doi.org/10.1136/annrheumdis-2020-218280 (2020).
Warnatz, K. & Voll, R. E. Pathogenesis of autoimmunity in common variable immunodeficiency. Front. Immunol. 3, 210 (2012).
Grammatikos, A. P. & Tsokos, G. C. Immunodeficiency and autoimmunity: lessons from systemic lupus erythematosus. Trends Mol. Med. 18, 101–108 (2012).
Ku, C. L., Chi, C. Y., von Bernuth, H. & Doffinger, R. Autoantibodies against cytokines: phenocopies of primary immunodeficiencies? Hum. Genet. 139, 783–794 (2020).
Merkel, P. A., Lebo, T. & Knight, V. Functional analysis of anti-cytokine autoantibodies using flow cytometry. Front. Immunol. 10, 1517 (2019).
Baerlecken, N. et al. Recurrent, multifocal Mycobacterium avium-intercellulare infection in a patient with interferon-gamma autoantibody. Clin. Infect. Dis. 49, e76–8 (2009).
Asakura, T. et al. Disseminated mycobacterium genavense infection in patient with adult-onset immunodeficiency. Emerg. Infect. Dis. 23, 1208–1210 (2017).
Rosen, L. B. et al. Anti-GM-CSF autoantibodies in patients with cryptococcal meningitis. J. Immunol. 190, 3959–3966 (2013).
Crum-Cianflone, N. F., Lam, P. V., Ross-Walker, S., Rosen, L. B. & Holland, S. M. Autoantibodies to granulocyte-macrophage colony-stimulating factor associated with severe and unusual manifestations of Cryptococcus gattii infections. Open Forum Infect. Dis. 4, ofx211 (2017).
Trapnell, B. C. et al. Pulmonary alveolar proteinosis. Nat. Rev. Dis. Prim. 5, 16 (2019).
Bastard, P. et al. Auto-antibodies against type I IFNs in patients with life-threatening COVID-19. Science 24, eabd4585 (2020).
Bluestone, J. A. Mechanisms of tolerance. Immunol. Rev. 241, 5–19 (2011).
Lourenço, E. V. & La Cava, A. Natural regulatory T cells in autoimmunity. Autoimmunity 44, 33–42 (2011).
Kanamori, M., Nakatsukasa, H., Okada, M., Lu, Q. & Yoshimura, A. Induced regulatory T Cells: their development, stability, and applications. Trends Immunol. 37, 803–811 (2016).
Constantine, G. M. & Lionakis, M. S. Lessons from primary immunodeficiencies: autoimmune regulator and autoimmune polyendocrinopathy-candidiasis-ectodermal dystrophy. Immunol. Rev. 287, 103–120 (2019).
Perniola, R. Twenty years of AIRE. Front. Immunol. 9, 98 (2018).
Puel, A. et al. Autoantibodies against IL-17A, IL-17F, and IL-22 in patients with chronic mucocutaneous candidiasis and autoimmune polyendocrine syndrome type I. J. Exp. Med. 207, 291–297 (2010).
Kisand, K. et al. Chronic mucocutaneous candidiasis in APECED or thymoma patients correlates with autoimmunity to Th17-associated cytokines. J. Exp. Med. 207, 299–308 (2010).
Giardino, G. et al. Clinical and immunological features in a cohort of patients with partial DiGeorge syndrome followed at a single center. Blood 133, 2586–2596 (2019).
Davies, E. G. Immunodeficiency in DiGeorge syndrome and options for treating cases with complete athymia. Front. Immunol. 4, 322 (2013).
Sullivan, K. E., McDonald-McGinn, D. & Zackai, E. H. CD4(+) CD25(+) T-cell production in healthy humans and in patients with thymic hypoplasia. Clin. Diagn. Lab. Immunol. 9, 1129–1131 (2002).
Gennery, A. R. et al. Antibody deficiency and autoimmunity in 22q11.2 deletion syndrome. Arch. Dis. Child. 86, 422–425 (2002).
Klemann, C. et al. Clinical and immunological phenotype of patients with primary immunodeficiency due to damaging mutations in NFKB2. Front. Immunol. 10, 297 (2019).
Zhu, M. et al. NF-kappaB2 is required for the establishment of central tolerance through an Aire-dependent pathway. J. Clin. Invest. 116, 2964–2971 (2006).
Zhang, B. et al. NF-kappaB2 is required for the control of autoimmunity by regulating the development of medullary thymic epithelial cells. J. Biol. Chem. 281, 38617–38624 (2006).
Tucker, E. et al. A novel mutation in the Nfkb2 gene generates an NF-kappa B2 “super repressor”. J. Immunol. 179, 7514–7522 (2007).
Maccari, M. E. et al. Severe Toxoplasma gondii infection in a member of a NFKB2-deficient family with T and B cell dysfunction. Clin. Immunol. 183, 273–277 (2017).
Lee, C. E. et al. Autosomal-dominant B-cell deficiency with alopecia due to a mutation in NFKB2 that results in nonprocessable p100. Blood 124, 2964–2972 (2014).
Grinberg-Bleyer, Y. et al. The alternative NF-κB pathway in regulatory T cell homeostasis and suppressive function. J. Immunol. 200, 2362–2371 (2018).
Villa, A., Notarangelo, L. D. & Roifman, C. M. Omenn syndrome: inflammation in leaky severe combined immunodeficiency. J. Allergy Clin. Immunol. 122, 1082–1086 (2008).
Cavadini, P. et al. AIRE deficiency in thymus of 2 patients with Omenn syndrome. J. Clin. Invest. 115, 728–732 (2005).
Cassani, B. et al. Defect of regulatory T cells in patients with Omenn syndrome. J. Allergy Clin. Immunol. 125, 209–216 (2010).
Mouchess, M. L. & Anderson, M. Central tolerance induction. Curr. Top. Microbiol. Immunol. 373, 69–86 (2014).
Malhotra, D. et al. Tolerance is established in polyclonal CD4(+) T cells by distinct mechanisms, according to self-peptide expression patterns. Nat. Immunol. 17, 187–195 (2016).
Tivol, E. A. et al. Loss of CTLA-4 leads to massive lymphoproliferation and fatal multiorgan tissue destruction, revealing a critical negative regulatory role of CTLA-4. Immunity 3, 541–547 (1995).
Zhang, X., Olsen, N. & Zheng, S. G. The progress and prospect of regulatory T cells in autoimmune diseases. J. Autoimmun. 111, 102461 (2020).
Wildin, R. S. et al. X-linked neonatal diabetes mellitus, enteropathy and endocrinopathy syndrome is the human equivalent of mouse scurfy. Nat. Genet. 27, 18–20 (2001).
Cepika, A. M. et al. Tregopathies: monogenic diseases resulting in regulatory T-cell deficiency. J. Allergy Clin. Immunol. 142, 1679–1695 (2018).
Jamee, M. et al. Clinical, immunological, and genetic features in patients with Immune Dysregulation, Polyendocrinopathy, Enteropathy, X-linked (IPEX) and IPEX-like Syndrome. J. Allergy Clin. Immunol. Pr. 20, 30478–5 (2020).
Park, J. H. et al. Immune dysregulation, polyendocrinopathy, enteropathy, X-linked (IPEX) syndrome: A systematic review. Autoimmun. Rev. 19, 102526 (2020).
Verma, N., Burns, S. O., Walker, L. S. K. & Sansom, D. M. Immune deficiency and autoimmunity in patients with CTLA-4 (CD152) mutations. Clin. Exp. Immunol. 190, 1–7 (2017).
Yokosuka, T. et al. Spatiotemporal basis of CTLA-4 costimulatory molecule-mediated negative regulation of T cell activation. Immunity 33, 326–339 (2010).
Hogquist, K. A. & Jameson, S. C. The self-obsession of T cells: how TCR signaling thresholds affect fate ‘decisions’ and effector function. Nat. Immunol. 15, 815–823 (2014).
Waterhouse, P. et al. Lymphoproliferative disorders with early lethality in mice deficient in Ctla-4. Science 270, 985–988 (1995).
Mitsuiki, N., Schwab, C. & Grimbacher, B. What did we learn from CTLA-4 insufficiency on the human immune system? Immunol. Rev. 287, 33–49 (2019).
Kuehn, H. S. et al. Immune dysregulation in human subjects with heterozygous germline mutations in CTLA4. Science 345, 1623–1627 (2014).
Schwab, C. et al. Phenotype, penetrance, and treatment of 133 cytotoxic T-lymphocyte antigen 4-insufficient subjects. J. Allergy Clin. Immunol. 142, 1932–1946 (2018).
Lo, B. et al. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science 349, 436–440 (2015).
Tesch, V. K. et al. Long-term outcome of LRBA deficiency in 76 patients after various treatment modalities as evaluated by the immune deficiency and dysregulation activity (IDDA) score. J. Allergy Clin. Immunol. 145, 1452–1463 (2020).
Charbonnier, L. M. et al. Regulatory T-cell deficiency and immune dysregulation, polyendocrinopathy, enteropathy, X-linked-like disorder caused by loss-of-function mutations in LRBA. J. Allergy Clin. Immunol. 135, 217–227 (2015).
Gámez-Díaz, L. et al. The extended phenotype of LPS-responsive beige-like anchor protein (LRBA) deficiency. J. Allergy Clin. Immunol. 137, 223–230 (2016).
Kiykim, A. et al. Abatacept as a long-term targeted therapy for LRBA deficiency. J. Allergy Clin. Immunol. Pr. 7, 2790–2800.e15 (2019).
Fos, C. et al. Association of the EF-hand and PH domains of the guanine nucleotide exchange factor SLAT with IP3 receptor 1 promotes Ca²+ signaling in T cells. Sci. Signal. 7, ra93 (2014).
Fanzo, J. C. et al. Loss of IRF-4-binding protein leads to the spontaneous development of systemic autoimmunity. J. Clin. Invest. 116, 703–714 (2016).
Canonigo-Balancio, A. J., Fos, C., Prod’homme, T., Bécart, S. & Altman, A. SLAT/Def6 plays a critical role in the development of Th17 cell-mediated experimental autoimmune encephalomyelitis. J. Immunol. 183, 7259–7267 (2009).
Serwas, N. K. et al. Human DEF6 deficiency underlies an immunodeficiency syndrome with systemic autoimmunity and aberrant CTLA-4 homeostasis. Nat. Commun. 10, 3106 (2019).
Vignoli, M. et al. CD25 deficiency: a new conformational mutation prevents the receptor expression on cell surface. Clin. Immunol. 201, 15–19 (2019).
Goudy, K. et al. Human IL2RA null mutation mediates immunodeficiency with lymphoproliferation and autoimmunity. Clin. Immunol. 146, 248–261 (2013).
Bezrodnik, L., Caldirola, M. S., Seminario, A. G., Moreira, I. & Gaillard, M. I. Follicular bronchiolitis as phenotype associated with CD25 deficiency. Clin. Exp. Immunol. 175, 227–234 (2014).
Roth, T. L. et al. Reprogramming human T cell function and specificity with non-viral genome targeting. Nature 559, 405–409 (2018).
Sharma, R. et al. A regulatory T cell-dependent novel function of CD25 (IL-2Ralpha) controlling memory CD8(+) T cell homeostasis. J. Immunol. 178, 1251–1255 (2007).
Afzali, B. et al. BACH2 immunodeficiency illustrates an association between super-enhancers and haploinsufficiency. Nat. Immunol. 18, 813–823 (2017).
Roychoudhuri, R. et al. BACH2 represses effector programs to stabilize T(reg)-mediated immune homeostasis. Nature 498, 506–510 (2013).
Sidwell, T. et al. Attenuation of TCR-induced transcription by Bach2 controls regulatory T cell differentiation and homeostasis. Nat. Commun. 11, 252 (2020).
Bernasconi, A. et al. Characterization of immunodeficiency in a patient with growth hormone insensitivity secondary to a novel STAT5b gene mutation. Pediatrics 118, e1584–e1592 (2006).
Cheng, G., Yu, A. & Malek, T. R. T-cell tolerance and the multi-functional role of IL-2R signaling in T-regulatory cells. Immunol. Rev. 241, 63–76 (2011).
Cohen, A. C. et al. Cutting edge: decreased accumulation and regulatory function of CD4+ CD25(high) T cells in human STAT5b deficiency. J. Immunol. 177, 2770–2774 (2006).
Acres, M. J. et al. Signal transducer and activator of transcription 5B deficiency due to a novel missense mutation in the coiled-coil domain. J. Allergy Clin. Immunol. 143, 413–416.e4 (2019).
Gharibi, T. et al. Targeting STAT3 in cancer and autoimmune diseases. Eur. J. Pharm. 878, 173107 (2020).
Zhang, Q., Boisson, B., Béziat, V., Puel, A. & Casanova, J. L. Human hyper-IgE syndrome: singular or plural? Mamm. Genome 29, 603–617 (2018).
Sogkas, G. et al. Dupilumab to treat severe atopic dermatitis in autosomal dominant hyper-IgE syndrome. Clin. Immunol. 215, 108452 (2020).
Flanagan, S. E. et al. Activating germline mutations in STAT3 cause early-onset multi-organ autoimmune disease. Nat. Genet. 46, 812–814 (2014).
Jägle, S. et al. Distinct molecular response patterns of activating STAT3 mutations associate with penetrance of lymphoproliferation and autoimmunity. Clin. Immunol. 210, 108316 (2020).
Nabhani, S. et al. STAT3 gain-of-function mutations associated with autoimmune lymphoproliferative syndrome like disease deregulate lymphocyte apoptosis and can be targeted by BH3 mimetic compounds. Clin. Immunol. 181, 32–42 (2017).
Khoury, T. et al. Tocilizumab promotes regulatory T-cell alleviation in STAT3 gain-of-function-associated multi-organ autoimmune syndrome. Clin. Ther. 39, 444–449 (2017).
Passerini, L. et al. STAT5-signaling cytokines regulate the expression of FOXP3 in CD4+CD25+ regulatory T cells and CD4+CD25- effector T cells. Int. Immunol. 20, 421–431 (2008).
Pillemer, B. B., Xu, H., Oriss, T. B., Qi, Z. & Ray, A. Deficient SOCS3 expression in CD4+CD25+FoxP3+ regulatory T cells and SOCS3-mediated suppression of Treg function. Eur. J. Immunol. 37, 2082–2089 (2007).
Biggs, C. M., Keles, S. & Chatila, T. A. DOCK8 deficiency: Insights into pathophysiology, clinical features and management. Clin. Immunol. 181, 75–82 (2017).
Alroqi, F. J. et al. DOCK8 deficiency presenting as an IPEX-like disorder. J. Clin. Immunol. 37, 811–819 (2017).
Janssen, E. et al. Dedicator of cytokinesis 8-deficient patients have a breakdown in peripheral B-cell tolerance and defective regulatory T cells. J. Allergy Clin. Immunol. 134, 1365–1374 (2014).
Huber, M. & Lohoff, M. IRF4 at the crossroads of effector T-cell fate decision. Eur. J. Immunol. 44, 1886–1895 (2014).
Haljasorg, U. et al. Irf4 expression in thymic epithelium is critical for thymic regulatory T cell homeostasis. J. Immunol. 198, 1952–1960 (2017).
Mittrücker, H. W. et al. Requirement for the transcription factor LSIRF/IRF4 for mature B and T lymphocyte function. Science 275, 540–543 (1997).
Bravo García-Morato, M. et al. New human combined immunodeficiency caused by interferon regulatory factor 4 (IRF4) deficiency inherited by uniparental isodisomy. J. Allergy Clin. Immunol. 141, 1924–1927.e18 (2018).
Sogkas, G., Adriawan, I. R., Dubrowinskaja, N., Atschekzei, F. & Schmidt, R. E. Homeostatic and pathogenic roles of PI3Kδ in the human immune system. Adv. Immunol. 146, 109–137 (2020).
Sogkas, G. et al. Primary immunodeficiency disorder caused by phosphoinositide 3-kinase δ deficiency. J. Allergy Clin. Immunol. 142, 1650–1653.e2 (2018).
Conley, M. E. et al. Agammaglobulinemia and absent B lineage cells in a patient lacking the p85α subunit of PI3K. J. Exp. Med. 209, 463–470 (2012).
Hanna, B. S. et al. PI3Kδ inhibition modulates regulatory and effector T-cell differentiation and function in chronic lymphocytic leukemia. Leukemia 33, 1427–1438 (2019).
Sauer, S. et al. T cell receptor signaling controls Foxp3 expression via PI3K, Akt, and mTOR. Proc. Natl Acad. Sci. USA 105, 7797–7802 (2008).
Patton, D. T. et al. Cutting edge: the phosphoinositide 3-kinase p110 delta is critical for the function of CD4+CD25+Foxp3+ regulatory T cells. J. Immunol. 177, 6598–6602 (2006).
Chellappa, S. et al. The PI3K p110δ Isoform Inhibitor Idelalisib Preferentially Inhibits Human Regulatory T Cell Function. J. Immunol. 202, 1397–1405 (2019).
Sharman, J. P. et al. Final results of a randomized, phase III study of rituximab with or without idelalisib followed by open-label idelalisib in patients with relapsed chronic lymphocytic leukemia. J. Clin. Oncol. 37, 1391–1402 (2019).
Bhattacharyya, N. D. & Feng, C. G. Regulation of T helper cell fate by TCR signal strength. Front. Immunol. 11, 624 (2020).
Feske, S. ORAI1 and STIM1 deficiency in human and mice: roles of store-operated Ca2+ entry in the immune system and beyond. Immunol. Rev. 231, 189–209 (2009).
Feske, S., Picard, C. & Fischer, A. Immunodeficiency due to mutations in ORAI1 and STIM1. Clin. Immunol. 135, 169–182 (2010).
Lian, J. et al. ORAI1 mutations abolishing store-operated Ca2+ entry cause anhidrotic ectodermal dysplasia with immunodeficiency. J. Allergy Clin. Immunol. 142, 1297–1310.e11 (2018).
Lacruz, R. S. & Feske, S. Diseases caused by mutations in ORAI1 and STIM1. Ann. N. Y. Acad. Sci. 1356, 45–79 (2015).
Cheng, K. T. et al. STIM1 and STIM2 protein deficiency in T lymphocytes underlies development of the exocrine gland autoimmune disease, Sjogren’s syndrome. Proc. Natl Acad. Sci. USA 109, 14544–14549 (2012).
Oh-Hora, M. et al. Dual functions for the endoplasmic reticulum calcium sensors STIM1 and STIM2 in T cell activation and tolerance. Nat. Immunol. 9, 432–443 (2008).
Picard, C. et al. STIM1 mutation associated with a syndrome of immunodeficiency and autoimmunity. N. Engl. J. Med. 360, 1971–1980 (2009).
Fuchs, S. et al. Antiviral and regulatory T cell immunity in a patient with stromal interaction molecule 1 deficiency. J. Immunol. 188, 1523–1533 (2012).
Srikanth, S. et al. The Ca2+ sensor STIM1 regulates the type I interferon response by retaining the signaling adaptor STING at the endoplasmic reticulum. Nat. Immunol. 20, 152–162 (2019).
Nunes-Santos, C. J., Uzel, G. & Rosenzweig, S. D. PI3K pathway defects leading to immunodeficiency and immune dysregulation. J. Allergy Clin. Immunol. 143, 1676–1687 (2019).
Lucas, C. L. et al. Dominant-activating germline mutations in the gene encoding the PI(3)K catalytic subunit p110δ result in T cell senescence and human immunodeficiency. Nat. Immunol. 15, 88–97 (2014).
Suzuki, A. et al. T cell-specific loss of Pten leads to defects in central and peripheral tolerance. Immunity 14, 523–534 (2001).
Moser, E. K. & Oliver, P. M. Regulation of autoimmune disease by the E3 ubiquitin ligase Itch. Cell. Immunol. 340, 103916 (2019).
Teachey, D. T. et al. Targeting Notch signaling in autoimmune and lymphoproliferative disease. Blood 111, 705–714 (2008).
Shembade, N. et al. The E3 ligase Itch negatively regulates inflammatory signaling pathways by controlling the function of the ubiquitin-editing enzyme A20. Nat. Immunol. 9, 254–262 (2008).
Kleine-Eggebrecht, N. et al. Mutation in ITCH Gene Can Cause Syndromic Multisystem Autoimmune Disease With Acute Liver Failure. Pediatrics 143, e20181554 (2019).
Lohr, N. J. et al. Human ITCH E3 ubiquitin ligase deficiency causes syndromic multisystem autoimmune disease. Am. J. Hum. Genet. 86, 447–453 (2010).
Keller, B. et al. Early onset combined immunodeficiency and autoimmunity in patients with loss-of-function mutation in LAT. J. Exp. Med. 213, 1185–1199 (2016).
Sommers, C. L. et al. A LAT mutation that inhibits T cell development yet induces lymphoproliferation. Science 296, 2040–2043 (2002).
Sommers, C. L. et al. Mutation of the phospholipase C-gamma1-binding site of LAT affects both positive and negative thymocyte selection. J. Exp. Med. 201, 1125–1134 (2005).
Hauck, F. et al. Primary T-cell immunodeficiency with immunodysregulation caused by autosomal recessive LCK deficiency. J. Allergy Clin. Immunol. 130, 1144–1152.e11 (2012).
Rowe, J. H. et al. Patients with CD3G mutations reveal a role for human CD3γ in Treg diversity and suppressive function. Blood 131, 2335–2344 (2018).
Lee, W. I. et al. A Novel CD3G mutation in a taiwanese patient with normal t regulatory function presenting with the CVID phenotype free of autoimmunity-analysis of all genotypes and phenotypes. Front. Immunol. 10, 2833 (2019).
Schejbel, L. et al. Molecular basis of hereditary C1q deficiency-revisited: identification of several novel disease-causing mutations. Genes Immun. 12, 626–634 (2011).
Lipsker, D. & Hauptmann, G. Cutaneous manifestations of complement deficiencies. Lupus 19, 1096–1106 (2010).
Eisen, D. P. & Minchinton, R. M. Impact of mannose-binding lectin on susceptibility to infectious diseases. Clin. Infect. Dis. 37, 1496–1505 (2003).
Tsutsumi, A., Takahashi, R. & Sumida, T. Mannose binding lectin: genetics and autoimmune disease. Autoimmun. Rev. 4, 364–372 (2005).
Pickering, M. C., Botto, M., Taylor, P. R., Lachmann, P. J. & Walport, M. J. Systemic lupus erythematosus, complement deficiency, and apoptosis. Adv. Immunol. 76, 227–324 (2000).
Stengaard-Pedersen, K. et al. Inherited deficiency of mannan-binding lectin-associated serine protease 2. N. Engl. J. Med. 349, 554–560 (2003).
Fleisher, T. A. & Oliveira, J. B. Monogenic defects in lymphocyte apoptosis. Curr. Opin. Allergy Clin. Immunol. 12, 609–615 (2012).
Rieux-Laucat, F., Le Deist, F. & Fischer, A. Autoimmune lymphoproliferative syndromes: genetic defects of apoptosis pathways. Cell Death Differ. 10, 124–133 (2003).
Bride, K. & Teachey, D. Autoimmune lymphoproliferative syndrome: more than a FAScinating disease. F1000Res. 6, 1928 (2017).
Neven, B. et al. A survey of 90 patients with autoimmune lymphoproliferative syndrome related to TNFRSF6 mutation. Blood 118, 4798–4807 (2011).
Molnár, E. et al. Key diagnostic markers for autoimmune lymphoproliferative syndrome with molecular genetic diagnosis. Blood 136, 1933–1945 (2020).
Rensing-Ehl, A. et al. Clinical and immunological overlap between autoimmune lymphoproliferative syndrome and common variable immunodeficiency. Clin. Immunol. 137, 357–365 (2010).
Rieux-Laucat, F., Fischer, A. & Deist, F. L. Cell-death signaling and human disease. Curr. Opin. Immunol. 15, 325–331 (2003). 2003.
Rieux-Laucat, F. Inherited and acquired death receptor defects in human Autoimmune Lymphoproliferative Syndrome. Curr. Dir. Autoimmun. 9, 18–36 (2006).
Hsu, A. P. et al. Autoimmune lymphoproliferative syndrome due to FAS mutations outside the signal-transducing death domain: molecular mechanisms and clinical penetrance. Genet. Med. 14, 81–89 (2012).
Hauck, F. et al. Somatic loss of heterozygosity, but not haploinsufficiency alone, leads to full-blown autoimmune lymphoproliferative syndrome in 1 of 12 family members with FAS start codon mutation. Clin. Immunol. 147, 61–68 (2013).
Magerus-Chatinet, A. et al. Onset of autoimmune lymphoproliferative syndrome (ALPS) in humans as a consequence of genetic defect accumulation. J. Clin. Invest. 121, 106–112 (2011).
Miano, M. et al. FAS-mediated apoptosis impairment in patients with ALPS/ALPS-like phenotype carrying variants on CASP10 gene. Br. J. Haematol. 187, 502–508 (2019).
Niemela, J. E. et al. Somatic KRAS mutations associated with a human nonmalignant syndrome of autoimmunity and abnormal leukocyte homeostasis. Blood 117, 2883–2886 (2011).
Oliveira, J. B. et al. NRAS mutation causes a human autoimmune lymphoproliferative syndrome. Proc. Natl Acad. Sci. USA 104, 8953–8958 (2007).
Crow, M. K., Olferiev, M., Kirou, K. A. & Type, I. Interferons in Autoimmune Disease. Annu. Rev. Pathol. 14, 369–393 (2019).
Jiang, J. et al Interferons in the pathogenesis and treatment of autoimmune diseases. Clin. Rev. Allergy Immunol. https://doi.org/10.1007/s12016-020-08798-2 (2020).
Bienias, M. et al. Therapeutic approaches to Type I Interferonopathies. Curr. Rheumatol. Rep. 20, 32 (2018).
Mogensen, T. H. IRF and STAT transcription factors - from basic biology to roles in infection, protective immunity, and primary immunodeficiencies. Front. Immunol. 9, 3047 (2019).
Toubiana, J. et al. Heterozygous STAT1 gain-of-function mutations underlie an unexpectedly broad clinical phenotype. Blood 127, 3154–3164 (2016).
Chen, X. et al. Molecular and phenotypic characterization of nine patients with STAT1 GOF mutations in China. J. Clin. Immunol. 40, 82–95 (2020).
Ovadia, A., Sharfe, N., Hawkins, C., Laughlin, S. & Roifman, C. M. Two different STAT1 gain-of-function mutations lead to diverse IFN-γ-mediated gene expression. NPJ Genom. Med. 3, 23 (2018).
Rodero, M. P. & Crow, Y. J. Type I interferon-mediated monogenic autoinflammation: The type I interferonopathies, a conceptual overview. J. Exp. Med. 213, 2527–2538 (2016).
Kaleviste, E. et al. Interferon signature in patients with STAT1 gain-of-function mutation is epigenetically determined. Eur. J. Immunol. 49, 790–800 (2019).
Zhou, Q. et al. Early-onset stroke and vasculopathy associated with mutations in ADA2. N. Engl. J. Med. 370, 911–920 (2014).
Navon Elkan, P. et al. Mutant adenosine deaminase 2 in a polyarteritis nodosa vasculopathy. N. Engl. J. Med 370, 921–931 (2014).
Skrabl-Baumgartner, A. et al. Autoimmune phenotype with type I interferon signature in two brothers with ADA2 deficiency carrying a novel CECR1 mutation. Pediatr. Rheumatol. Online J. 15, 67 (2017).
Insalaco, A. et al. Variable clinical phenotypes and relation of interferon signature with disease activity in ADA2 deficiency. J. Rheumatol. 46, 523–526 (2019).
Cashman, K. S. et al. Understanding and measuring human B-cell tolerance and its breakdown in autoimmune disease. Immunol. Rev. 292, 76–89 (2019).
Gay, D., Saunders, T., Camper, S. & Weigert, M. Receptor editing: an approach by autoreactive B cells to escape tolerance. J. Exp. Med. 177, 999–1008 (1993).
Tiegs, S. L., Russell, D. M. & Nemazee, D. Receptor editing in self-reactive bone marrow B cells. J. Exp. Med. 177, 1009–1020 (1993).
Kumar, R., DiMenna, L. J., Chaudhuri, J. & Evans, T. Biological function of activation-induced cytidine deaminase (AID). Biomed. J. 37, 269–283 (2014).
Quartier, P. et al. Clinical, immunologic and genetic analysis of 29 patients with autosomal recessive hyper-IgM syndrome due to Activation-Induced Cytidine Deaminase deficiency. Clin. Immunol. 110, 22–29 (2004).
Revy, P. et al. Activation-induced cytidine deaminase (AID) deficiency causes the autosomal recessive form of the Hyper-IgM syndrome (HIGM2). Cell 102, 565–575 (2000).
Meyers, G. et al. Activation-induced cytidine deaminase (AID) is required for B-cell tolerance in humans. Proc. Natl Acad. Sci. USA 108, 11554–11559 (2011).
Mackay, F. et al. Mice transgenic for BAFF develop lymphocytic disorders along with autoimmune manifestations. J. Exp. Med. 190, 1697–1710 (1999).
Qin, H. et al. Activation-induced cytidine deaminase expression in CD4+ T cells is associated with a unique IL-10-producing subset that increases with age. PLoS One 6, e29141 (2011).
Durandy, A., Cantaert, T., Kracker, S. & Meffre, E. Potential roles of activation-induced cytidine deaminase in promotion or prevention of autoimmunity in humans. Autoimmunity 46, 148–156 (2013).
Salzer, E., Santos-Valente, E., Keller, B., Warnatz, K. & Boztug, K. Protein Kinase C δ: a Gatekeeper of Immune Homeostasis. J. Clin. Immunol. 36, 631–640 (2016).
Salzer, E. et al. B-cell deficiency and severe autoimmunity caused by deficiency of protein kinase C δ. Blood 121, 3112–3116 (2013).
Belot, A. et al. Protein kinase cδ deficiency causes mendelian systemic lupus erythematosus with B cell-defective apoptosis and hyperproliferation. Arthritis Rheum. 65, 2161–2171 (2013).
Kuehn, H. S. et al. Loss-of-function of the protein kinase C δ (PKCδ) causes a B-cell lymphoproliferative syndrome in humans. Blood 121, 3117–3125 (2013).
Kiykim, A. et al. Potentially beneficial effect of hydroxychloroquine in a patient with a novel mutation in protein kinase Cδ deficiency. J. Clin. Immunol. 35, 523–526 (2015).
Miyamoto, A. et al. Increased proliferation of B cells and auto-immunity in mice lacking protein kinase Cdelta. Nature 416, 865–869 (2002).
Ehl, S., Hombach, J., Aichele, P., Hengartner, H. & Zinkernagel, R. M. Bystander activation of cytotoxic T cells: studies on the mechanism and evaluation of in vivo significance in a transgenic mouse model. J. Exp. Med. 185, 1241–1251 (1997).
Llewelyn, M. & Cohen, J. Superantigens: microbial agents that corrupt immunity. Lancet Infect. Dis. 2, 156–162 (2002).
Fujinami, R. S., von Herrath, M. G., Christen, U. & Whitton, J. L. Molecular mimicry, bystander activation, or viral persistence: infections and autoimmune disease. Clin. Microbiol. Rev. 19, 80–94 (2016).
Hussein, H. M. & Rahal, E. A. The role of viral infections in the development of autoimmune diseases. Crit. Rev. Microbiol. 45, 394–412 (2019).
Rodríguez, Y. et al. Guillain-Barré syndrome, transverse myelitis and infectious diseases. Cell. Mol. Immunol. 15, 547–562 (2018).
Qiu, C. C., Caricchio, R. & Gallucci, S. Triggers of autoimmunity: the role of bacterial infections in the extracellular exposure of lupus nuclear autoantigens. Front. Immunol. 10, 2608 (2019).
Christen, U. & von Herrath, M. G. Infections and autoimmunity-good or bad? J. Immunol. 174, 7481–7486 (2005).
Draborg, A. H., Duus, K. & Houen, G. Epstein-Barr virus and systemic lupus erythematosus. Clin. Dev. Immunol. 2012, 370516 (2012).
Newkirk, M. M., Zbar, A., Baron, M. & Manges, A. R. Distinct bacterial colonization patterns of Escherichia coli subtypes associate with rheumatoid factor status in early inflammatory arthritis. Rheumatol. (Oxf.) 49, 1311–1316 (2010).
Kivity, S., Agmon-Levin, N., Blank, M. & Shoenfeld, Y. Infections and autoimmunity-friends or foes? Trends Immunol. 30, 409–414 (2009).
Rodriguez-Calvo, T. Enterovirus infection and type 1 diabetes: unraveling the crime scene. Clin. Exp. Immunol. 195, 15–24 (2019).
Nakamura, H., Shimizu, T. & Kawakami, A. Role of Viral Infections in the Pathogenesis of Sjögren’s Syndrome: Different Characteristics of Epstein-Barr Virus and HTLV-1. J. Clin. Med. 9, 1459 (2020).
Venigalla, S. S. K., Premakumar, S. & Janakiraman, V. A possible role for autoimmunity through molecular mimicry in alphavirus mediated arthritis. Sci. Rep. 10, 938 (2020).
Dow, C. T. & Proposing, B. C. G. Vaccination for Mycobacterium avium ss. paratuberculosis (MAP) Associated Autoimmune Diseases. Microorganisms 8, 212 (2020).
Sogkas, G. et al. CD74 is a T cell antigen in spondyloarthritis. Clin. Exp. Rheumatol. 38, 195–202 (2020).
Cusick, M. F., Libbey, J. E. & Fujinami, R. S. Molecular mimicry as a mechanism of autoimmune disease. Clin. Rev. Allergy Immunol. 42, 102–111 (2012).
Dematapitiya, C. et al. Cold type autoimmune hemolytic anemia- a rare manifestation of infectious mononucleosis; serum ferritin as an important biomarker. BMC Infect. Dis. 19, 68 (2019).
Fadeyi, E. A., Simmons, J. H., Jones, M. R., Palavecino, E. L. & Pomper, G. J. Fatal autoimmune hemolytic anemia due to immunoglobulin g autoantibody exacerbated by epstein-barr virus. Lab. Med. 46, 55–59 (2015).
Kang, I. et al. Defective control of latent Epstein-Barr virus infection in systemic lupus erythematosus. J. Immunol. 172, 1287–1294 (2004).
Larsen, M. et al. Exhausted cytotoxic control of Epstein-Barr virus in human lupus. PLoS Pathog. 7, e1002328 (2011).
Pender, M. P. Preventing and curing multiple sclerosis by controlling Epstein-Barr virus infection. Autoimmun. Rev. 8, 563–568 (2009).
Klatt, T. et al. Expansion of peripheral CD8+ CD28- T cells in response to Epstein-Barr virus in patients with rheumatoid arthritis. J. Rheumatol. 32, 239–251 (2005).
Cohen, J. I. Primary immunodeficiencies associated with EBV disease. Curr. Top. Microbiol. Immunol. 390, 241–265 (2015).
Latour, S. & Winter, S. Inherited immunodeficiencies with high predisposition to epstein-barr virus-driven lymphoproliferative diseases. Front. Immunol. 9, 1103 (2018).
Ghosh, S., Bienemann, K., Boztug, K. & Borkhardt, A. Interleukin-2-inducible T-cell kinase (ITK) deficiency - clinical and molecular aspects. J. Clin. Immunol. 34, 892–899 (2014).
Ravell, J., Chaigne-Delalande, B. & Lenardo, M. X-linked immunodeficiency with magnesium defect, Epstein-Barr virus infection, and neoplasia disease: a combined immune deficiency with magnesium defect. Curr. Opin. Pediatr. 26, 713–719 (2014).
Machado Ribeiro, F. & Goldenberg, T. Mycobacteria and autoimmunity. Lupus 24, 374–381 (2015).
Kakumanu, P. et al. Patients with pulmonary tuberculosis are frequently positive for anti-cyclic citrullinated peptide antibodies, but their sera also react with unmodified arginine-containing peptide. Arthritis Rheum. 58, 1576–1581 (2008).
Esaguy, N., Aguas, A. P., van Embden, J. D. & Silva, M. T. Mycobacteria and human autoimmune disease: direct evidence of cross-reactivity between human lactoferrin and the 65-kilodalton protein of tubercle and leprosy bacilli. Infect. Immun. 59, 1117–1125 (1991).
Mok, M. Y. et al. Non-tuberculous mycobacterial infection in patients with systemic lupus erythematosus. Rheumatol. (Oxf.) 46, 280–284 (2007).
Chao, W. C. et al. Association between a history of mycobacterial infection and the risk of newly diagnosed Sjögren’s syndrome: A nationwide, population-based case-control study. PLoS One 12, e0176549 (2017).
Rosain, J. et al. Mendelian susceptibility to mycobacterial disease: 2014-2018 update. Immunol. Cell. Biol. 97, 360–367 (2019).
Jindal, A. K. et al. Recurrent salmonella typhi infection and autoimmunity in a young boy with complete IL-12 receptor β1 deficiency. J. Clin. Immunol. 39, 358–362 (2019).
Sogkas, G. et al. First association of interleukin 12 receptor beta 1 deficiency with Sjögren’s syndrome. Front. Immunol. 8, 885 (2017).
Göktürk, B. et al. Infectious diseases, autoimmunity and midline defect in a patient with a novel bi-allelic mutation in IL12RB1 gene. Turk. J. Pediatr. 58, 331–336 (2016).
Ling, G. et al. IL-12 receptor 1β deficiency with features of autoimmunity and photosensitivity. Autoimmunity 49, 143–146 (2016).
Miraghazadeh, B. & Cook, M. C. Nuclear factor-kappaB in autoimmunity: man and mouse. Front. Immunol. 9, 613 (2018).
Tuijnenburg, P. et al. Loss-of-function nuclear factor κB subunit 1 (NFKB1) variants are the most common monogenic cause of common variable immunodeficiency in Europeans. J. Allergy Clin. Immunol. 142, 1285–1296 (2018).
Schröder, C. et al. Late-onset antibody deficiency due to monoallelic alterations in NFKB1. Front. Immunol. 10, 2618 (2019).
Lorenzini, T. et al. Characterization of the clinical and immunologic phenotype and management of 157 individuals with 56 distinct heterozygous NFKB1 mutations. J. Allergy Clin. Immunol. S0091–6749(20)30422-X (2020).
Boisson, B., Puel, A., Picard, C. & Casanova, J. L. Human IκBα Gain of Function: a Severe and Syndromic Immunodeficiency. J. Clin. Immunol. 37, 397–412 (2017).
Sogkas, G. et al. A novel NFKBIA variant substituting serine 36 of IκBα causes immunodeficiency with warts, bronchiectasis and juvenile rheumatoid arthritis in the absence of ectodermal dysplasia. Clin. Immunol. 210, 108269 (2020).
Batlle-Masó, L. et al. Genetic diagnosis of autoinflammatory disease patients using clinical exome sequencing. Eur. J. Med. Genet. 63, 103920 (2020).
Seghezzo, S. P., Dvorak, C. C., Cowan, M. J., Puck, J. M. & Dorsey, M. J. Extended Follow-up After Hematopoietic Cell Transplantation for IκBα Deficiency with Disseminated Mycobacterium avium Infection. J. Clin. Immunol. 40, 248–250 (2020).
Tan, E. E. et al. Dominant-negative NFKBIA mutation promotes IL-1β production causing hepatic disease with severe immunodeficiency. J. Clin. Invest. 130, 5817–5832 (2020).
Chang, J. H. et al. Ubc13 maintains the suppressive function of regulatory T cells and prevents their conversion into effector-like T cells. Nat. Immunol. 13, 481–490 (2012).
Sun, S. C., Chang, J. H. & Jin, J. Regulation of nuclear factor-κB in autoimmunity. Trends Immunol. 34, 282–289 (2013).
Kaustio, M. et al. Damaging heterozygous mutations in NFKB1 lead to diverse immunologic phenotypes. J. Allergy Clin. Immunol. 140, 782–796 (2017).
Vasanthakumar, A. et al. The TNF receptor superfamily-NF-κB axis is critical to maintain effector regulatory T cells in lymphoid and non-lymphoid tissues. Cell. Rep. 20, 2906–2920 (2017).
Kollias, G. TNF pathophysiology in murine models of chronic inflammation and autoimmunity. Semin. Arthritis Rheum. 34, 3–6 (2005).
Janssen, R. et al. The same IkappaBalpha mutation in two related individuals leads to completely different clinical syndromes. J. Exp. Med. 200, 559–68 (2004).
Lu, H. Y. et al. Germline CBM-opathies: from immunodeficiency to atopy. J. Allergy Clin. Immunol. 143, 1661–1673 (2019).
Gupta, M. et al. Clinical, immunological, and molecular findings in four cases of B cell expansion with NF-κB and T cell anergy disease for the first time from India. Front. Immunol. 9, 1049 (2018).
Bedsaul, J. R. et al. Mechanisms of regulated and dysregulated CARD11 signaling in adaptive immunity and disease. Front. Immunol. 9, 2105 (2018).
Dorjbal, B. et al. Hypomorphic caspase activation and recruitment domain 11 (CARD11) mutations associated with diverse immunologic phenotypes with or without atopic disease. J. Allergy Clin. Immunol. 143, 1482–1495 (2019).
Fuchs, S. et al. Omenn syndrome associated with a functional reversion due to a somatic second-site mutation in CARD11 deficiency. Blood 126, 1658–1669 (2015).
Charbit-Henrion, F. et al. Deficiency in Mucosa-associated Lymphoid Tissue Lymphoma Translocation 1: A Novel Cause of IPEX-Like Syndrome. J. Pediatr. Gastroenterol. Nutr. 64, 378–384 (2017).
Bornancin, F. et al. Deficiency of MALT1 paracaspase activity results in unbalanced regulatory and effector T and B cell responses leading to multiorgan inflammation. J. Immunol. 194, 3723–3734 (2015).
Torres, J. M. et al. Inherited BCL10 deficiency impairs hematopoietic and nonhematopoietic immunity. J. Clin. Invest. 124, 5239–5248 (2014).
Jablonka, A. et al. Peripheral blood lymphocyte phenotype differentiates secondary antibody deficiency in rheumatic disease from primary antibody deficiency. J. Clin. Med. 9, 1049 (2020).
Fessler, J. et al. Lymphopenia in primary Sjögren’s syndrome is associated with premature aging of naïve CD4+ T cells. Rheumatology (Oxford) keaa105 (2020).
Martin, M., Guffroy, A., Argemi, X. & Martin, T. [Systemic lupus erythematosus and lymphopenia: Clinical and pathophysiological features]. Rev. Med. Interne 38, 603–613 (2017).
Du, J. et al. The association between the lymphocyte-monocyte ratio and disease activity in rheumatoid arthritis. Clin. Rheumatol. 36, 2689–2695 (2017).
Okada, Y. et al. Genetics of rheumatoid arthritis contributes to biology and drug discovery. Nature 506, 376–381 (2014).
Chopra, C. et al. Immune deficiency in Ataxia-Telangiectasia: a longitudinal study of 44 patients. Clin. Exp. Immunol. 176, 275–282 (2014).
McAllister, K. et al. Identification of BACH2 and RAD51B as rheumatoid arthritis susceptibility loci in a meta-analysis of genome-wide data. Arthritis Rheum. 65, 3058–3062 (2013).
Morris, D. L. et al. Genome-wide association meta-analysis in Chinese and European individuals identifies ten new loci associated with systemic lupus erythematosus. Nat. Genet. 48, 940–946 (2016).
Plenge, R. M. et al. Replication of putative candidate-gene associations with rheumatoid arthritis in >4,000 samples from North America and Sweden: association of susceptibility with PTPN22, CTLA4, and PADI4. Am. J. Hum. Genet. 77, 1044–1060 (2005).
Sun, C. et al. High-density genotyping of immune-related loci identifies new SLE risk variants in individuals with Asian ancestry. Nat. Genet. 48, 323–330 (2016).
Barton, A. et al. Rheumatoid arthritis susceptibility loci at chromosomes 10p15, 12q13 and 22q13. Nat. Genet 40, 1156–1159 (2008).
Tanaka, Y. et al. Association of the interferon-gamma receptor variant (Val14Met) with systemic lupus erythematosus. Immunogenetics 49, 266–271 (1999).
Kong, X. F. et al. Haploinsufficiency at the human IFNGR2 locus contributes to mycobacterial disease. Hum. Mol. Genet. 22, 769–781 (2013).
Moncada-Vélez, M. et al. Partial IFN-γR2 deficiency is due to protein misfolding and can be rescued by inhibitors of glycosylation. Blood 122, 2390–2401 (2013).
Wei, W. H., Viatte, S., Merriman, T. R., Barton, A. & Worthington, J. Genotypic variability based association identifies novel non-additive loci DHCR7 and IRF4 in sero-negative rheumatoid arthritis. Sci. Rep. 7, 5261 (2017).
Fu, Q. et al. Association of a functional IRF7 variant with systemic lupus erythematosus. Arthritis Rheum. 63, 749–754 (2011).
Ciancanelli, M. J. et al. Infectious disease. Life-threatening influenza and impaired interferon amplification in human IRF7 deficiency. Science 348, 448–453 (2015).
Yokoyama, N. et al. Association of NCF1 polymorphism with systemic lupus erythematosus and systemic sclerosis but not with ANCA-associated vasculitis in a Japanese population. Sci. Rep. 9, 16366 (2019).
Zhao, J. et al. A missense variant in NCF1 is associated with susceptibility to multiple autoimmune diseases. Nat. Genet. 49, 433–437 (2017).
Yu, H.H., Yang, Y.H. & Chiang, B.L. Chronic granulomatous disease: a comprehensive review. Clin. Rev. Allergy Immunol. https://doi.org/10.1007/s12016-020-08800-x (2020).
Tsoi, L. C. et al. Identification of 15 new psoriasis susceptibility loci highlights the role of innate immunity. Nat. Genet. 44, 1341–1348 (2012).
Papageorgiou, A. et al. A BAFF receptor His159Tyr mutation in Sjögren’s syndrome-related lymphoproliferation. Arthritis Rheumatol. 67, 2732–2741 (2015).
Warnatz, K. et al. B-cell activating factor receptor deficiency is associated with an adult-onset antibody deficiency syndrome in humans. Proc. Natl Acad. Sci. USA 106, 13945–13950 (2019).
Cortes, A. et al. Identification of multiple risk variants for ankylosing spondylitis through high-density genotyping of immune-related loci. Nat. Genet. 45, 730–738 (2013).
Kreins, A. Y. et al. Human TYK2 deficiency: Mycobacterial and viral infections without hyper-IgE syndrome. J. Exp. Med. 212, 1641–1662 (2015).
Oliveira, J. B. et al. Revised diagnostic criteria and classification for the autoimmune lymphoproliferative syndrome (ALPS): report from the 2009 NIH International Workshop. Blood 116, e35–e40 (2010).
Crow, Y. J., Shetty, J. & Livingston, J. H. Treatments in Aicardi-Goutières syndrome. Dev. Med. Child Neurol. 62, 42–47 (2020).
Lin, B. et al. A novel STING1 variant causes a recessive form of STING-associated vasculopathy with onset in infancy (SAVI). J. Allergy Clin. Immunol. S0091-6749, 30963–30965 (2020).
Fiehn, C. Familial Chilblain Lupus - what can we learn from Type I interferonopathies? Curr. Rheumatol. Rep. 19, 61 (2017).
Briggs, T. A. et al. Spondyloenchondrodysplasia due to mutations in ACP5: a comprehensive survey. J. Clin. Immunol. 36, 220–234
Torrelo, A. CANDLE syndrome as a paradigm of proteasome-related autoinflammation. Front. Immunol. 8, 927 (2017).
Saito, R. et al. Retinal vasculopathy with cerebral leukodystrophy: clinicopathologic features of an autopsied patient with a heterozygous TREX 1 mutation. J. Neuropathol. Exp. Neurol. 78, 181–186 (2019).
Rice, G. I. et al. Genetic and phenotypic spectrum associated with IFIH1 gain-of-function. Hum. Mutat. 41, 837–849 (2020).
Lässig, C. et al. Unified mechanisms for self-RNA recognition by RIG-I Singleton-Merten syndrome variants. Elife 7, e38958 (2018).
Martin-Fernandez, M. et al. Systemic Type I IFN inflammation in human ISG15 deficiency leads to necrotizing skin lesions. Cell. Rep. 31, 107633 (2020).
Meuwissen, M. E. et al. Human USP18 deficiency underlies type 1 interferonopathy leading to severe pseudo-TORCH syndrome. J. Exp. Med. 213, 1163–1174 (2016).
Van Esch, H. et al. Defective DNA polymerase α-primase leads to X-linked intellectual disability associated with severe growth retardation, microcephaly, and hypogonadism. Am. J. Hum. Genet. 104, 957–967 (2019).
Rodero, M. P. et al. Type I interferon-mediated autoinflammation due to DNase II deficiency. Nat. Commun. 8, 2176 (2017).
Funding
Open Access funding enabled and organized by Projekt DEAL. Authors receive funding by the DZIF TTU 07.806_00 (German Centre for Infection Research), the Deutsche Forschungsgemeinschaft (DFG, German Research Foundation) under Germany’s Excellence Strategy – EXC 2155 “RESIST” – Project ID 39087428, the German Federal Ministry of Education and Research (BMBF, 01GM1910E) and the Rosemarie-Germscheid Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sogkas, G., Atschekzei, F., Adriawan, I.R. et al. Cellular and molecular mechanisms breaking immune tolerance in inborn errors of immunity. Cell Mol Immunol 18, 1122–1140 (2021). https://doi.org/10.1038/s41423-020-00626-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41423-020-00626-z
Keywords
This article is cited by
-
The role of non-canonical Hippo pathway in regulating immune homeostasis
European Journal of Medical Research (2023)
-
Immune-mediated cytopenias (IMCs) after HSCT for pediatric non-malignant disorders: epidemiology, risk factors, pathogenesis, and treatment
European Journal of Pediatrics (2023)
-
RNA modifications: importance in immune cell biology and related diseases
Signal Transduction and Targeted Therapy (2022)
-
T Cell Abnormalities in X-Linked Agammaglobulinaemia: an Updated Review
Clinical Reviews in Allergy & Immunology (2022)