Abstract
Spinal cord injury (SCI) can lead to severe loss of motor and sensory function with high disability and mortality. The effective treatment of SCI remains unknown. Here we find systemic injection of TGF-β neutralizing antibody induces the protection of axon growth, survival of neurons, and functional recovery, whereas erythropoietin-producing hepatoma interactor B2 (EphrinB2) expression and fibroblasts distribution are attenuated. Knockout of TGF-β type II receptor in fibroblasts can also decrease EphrinB2 expression and improve spinal cord injury recovery. Moreover, miR-488 was confirmed to be the most upregulated gene related to EphrinB2 releasing in fibroblasts after SCI and miR-488 initiates EphrinB2 expression and physical barrier building through MAPK signaling after SCI. Our study points toward elevated levels of active TGF-β as inducer and promoters of fibroblasts distribution, fibrotic scar formation, and EphrinB2 expression, and deletion of global TGF-β or the receptor of TGF-β in Col1α2 lineage fibroblasts significantly improve functional recovery after SCI, which suggest that TGF-β might be a therapeutic target in SCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) has many causes, including motor vehicle injuries (MVI), fall, sports-related injury, violence, and others. The most common and severe injuries to the spinal cord are traumatic in nature [1]. Traumatic injuries to the spine usually results in a fracture of the vertebral body, shifting the vertebral body forward to compress the spine parenchyma, leading to permanent neurological dysfunction [2]. The annual incidence of SCI in the United States is ~17,000 new cases each year and about 250,000–500,000 people suffer from SCI worldwide [3].
Following SCI, the fibrotic component of scar, which was consists of collagen, fibronectin, and fibroblasts, could present either a physical or molecular obstacle to the regeneration of severed axons [4, 5]. Typically, damaged neurons are also not replaced by tissue regeneration, and fibrotic scar-forming cells can persist chronically in the lesion site [6]. How to reduce the formation of fibrotic scar, which may promote functional recovery by providing space for axon regeneration and neurons survival after SCI, requiring further investigation.
Transforming growth factors-βs (TGF-βs), a family of multifunctional peptide growth factors, only has three closely related isoforms, TGF-β1, β2, and β3 [7, 8]. TGF-βs are only present in mammals and are important for tissue remodeling and/or repair to maintain tissue homeostasis [9, 10]. However, many diseases in different organs are associated with aberrant activation or elevated levels of TGF-β, such as fibrosis of skin, kidney, lung, liver, and metastasis of different tumors [11,12,13]. Recently, some studies have shown that fibrotic scar formation could be regulated by TGF-β [14, 15], whereas, the intrinsic mechanism of how TGF-β regulate fibrotic scar formation, still remains unclear.
Over the past decade, although advances have occurred in traditional research areas such as axon regeneration, inflammation, scar formation and engraftment of neural and supporting cells, but still surprisingly little is known about the mechanisms [16]. Some studies have shown that transected axons stop at the lesion site which was also the border of the fibrotic scar and fibroblasts have been shown to express various axonal growth-inhibitory molecules including NG2 proteoglycan, phosphacan, tenascin-C, semaphorin 3A, and EphB2 [4].
Here in this study, we report that TGF-β mediates fibroblasts distribution and fibrotic scar formation by activating miR-484 in fibroblasts. Deletion of global TGF-β or the receptor of TGF-β in Col1α2 lineage fibroblasts significantly inhibits EphrinB2 expression, fibroblasts distribution, and fibrotic scar formation in the lesion area. Moreover, improved axon growth, survival of neurons, and motor function recovery are also observed. Our findings of inhibition or deletion of TGF-β attenuates fibroblasts distribution and fibrotic scar formation could be a potential guidance for therapy of SCI.
Results
Fibroblast secreting and EphrinB2 expression are inhibited in TGF-β knockout mice
We first examined the fibroblast distribution in the lesion site in the sham group, with or without TGF-β knockout group. A TGF-β neutralizing antibody (1D11; R&D System, Minneapolis, MN) or vehicle antibody of an identical IgG complex lacking any TGF-β-binding capabilities (13C4; R&D System, Minneapolis, MN) was injected into the mice three times a week from the day of SCI. Fibroblasts distribution could be inhibited by TGF-β in lung and tumor fibrosis [17] and the population of fibroblasts peaked at 7 days after SCI [18, 19]. And our results also revealed significantly increased fibroblasts gathered into the lesion site at 7 days after SCI in the 13C4 group after SCI, whereas markedly decreased after 1D11 injection (Fig. 1a, b). In addition, the EphrinB2 expression undergoes the same changing trend as fibroblast (Fig. 1a, c). Western-blot results confirmed the EphrinB2 expression was attenuated by TGF-β knockout (Fig. 1d, e). Significantly lower levels of active and total TGF-β1 in the spinal cord were seen in 1D11 group relative to 13C4 group (Fig. 1f, g). Altogether, our results reveal that TGF-β knockout in mice progresses with decreased fibroblast secreting and reduced EphrinB2 expression.
a Representative images of Immunohistochemistry and immunofluorescence analysis of FSP1 (red), EphrinB2 (green) and DAPI (blue) in each group at 2 weeks after SCI. Scale bars = 100 μm. Images on the middle row are high-resolution versions of the boxed regions in the top images, scale bars = 25 µm. b, c Quantitative analysis of FSP1 positive cells/field and relative fold change of EphrinB2 (*p < 0.05, **p < 0.01, n = 4). d Representative western blots showing the expression of EphrinB2 indifferent groups in vivo. e Quantitative analysis of the EphrinB2/β-tublin ratio in different groups mice after SCI (*p < 0.05, ***p < 0.001, ****p < 0.0001, n = 3). f, g Elisa analysis showing the concentration of TGF-β in spinal cord after SCI between 13C4 group control mice and 1D11 group mice (*p < 0.05, **p < 0.01, n = 4).
TGF-β knockout improves functional recovery of mice after SCI
We next determined the effects of TGF-β neutralizing antibody (1D11) and vehicle antibody (13C4) on the potential of neurological and motor function recovery after complete SCI. Immunofluorescence co-staining of serotonin (5-HT) and β-III-tublin was used to visualize the axon regeneration and neurons survival. Quantitation 4 weeks after SCI showed β-III-tublin+ nerves and 5-HT+ axons all failed to regrow through the lesion site in 13C4 group mice. Knockout TGF-β could reduce the dieback of 5-HT+ axons and β-III-tublin+ nerves (Fig. 2a–c). To evaluate the motor function recovery, we used the Basso Mouse Scale (BMS) of hindlimb function [20] and gait analysis. Results indicate that 1D11 group mice have better behavioral function recovery than 13C4 control group mice in BMS score and print area, stride length, and print length of the hind limb (Fig. 2d–h). Collectively, global TGF-β knockout in mice could improve functional recovery after SCI.
a Representative images of immunofluorescent analysis of 5-HT (red), β-III-tublin (green) and DAPI (blue) in each group at 4 weeks after SCI. Scale bars = 200 μm. Right images are high-resolution versions of the boxed regions in the left images, scale bars = 50 µm. b, c Quantitative analysis of intensity mean value of 5-HT and β-III-tublin (*p < 0.05, **p < 0.01, n = 4). d Quantitative analysis of BMS score between 13C4 control mice after SCI, 1D11 group mice after SCI and mice without SCI (*p < 0.05, **p < 0.01, n = 6). e–h Quantitative analysis of catwalk, including print length, stride length, and print area (*p < 0.05, n = 6). LF left front paw, RF right front paw, RH right hind paw. Statistical significance was determined by multifactorial ANOVA, and all data are shown as means ± standard deviations.
Genetic knockout TGF-β receptor 2 in fibroblasts attenuates EphrinB2 expression and induced nerve distribution
To examine whether EphrinB2 expression was mostly affected by the distribution of fibroblast through TGF- β activation. We generated a Col1α2-Cre::Tgfb2rflox/flox mouse model (Tgfbr2Col1α2−/−), where Tgfb2-receptors can be conditionally knocked out in Col1α2+ cells by injecting with tamoxifen three times weekly. Immunohistochemistry staining results showed significantly reduced FSP1+ fibroblasts in the Tgfbr2Col1α2−/− mice relative to Tgfbr2flox/flox mice (Tgfbr2f/f) (Fig. 3a, b). Moreover, EphrinB2 expression was markedly attenuated in Tgfbr2Col1α2−/− mice (Fig. 3c, d). In addition, immunostaining staining revealed significantly elevated β-III-tublin+ nerves distribution and markedly decreased Collagen III+ fibrotic scar area in Tgfbr2Col1α2−/− mice relative to Tgfbr2f/f mice (Fig. 4a–c). Taken together, the Tgfbr2Col1α2−/− mouse model could attenuate EphrinB2 expression and fibrotic scar formation, followed by increased nerve distribution. Indicating that the nerve function recovery may be improved by attenuated EphrinB2 expression which was mostly affected by fibroblasts via TGF- β activation.
a Representative images of Immunohistochemistry analysis of FSP1 in Tgfbr2Col1α2−/− mice and Tgfbr2flox/flox mice after SCI and Tgfbr2flox/flox mice without surgery (Sham) at 2 weeks. Scale bars = 100 μm. Images on the bottom are high-resolution versions of the boxed regions in the top images, scale bars = 25 µm. b, c Quantitative analysis of FSP1 positive cells/field (*p < 0.05, ****p < 0.0001, n = 4). c Representative images of immunofluorescence analysis of FSP1 (red), EphrinB2 (green) and DAPI (blue) in each group at 2 weeks after SCI. Scale bars = 50 μm. d Quantitative analysis of relative fold change of EphrinB2 (*p < 0.05, **p < 0.01, n = 4).
a Representative images of immunofluorescence analysis of collagen III (red), β-III-tublin (green) and DAPI (blue) in Tgfbr2Col1α2−/− mice and Tgfbr2flox/flox mice after SCI and Tgfbr2flox/flox mice without surgery (Sham) at 2 weeks. Scale bars = 200 μm. Right images are high-resolution versions of the boxed regions in the left images, scale bars = 50 µm. b, c Quantitative analysis of intensity mean value of collagen III and β-III-tublin (*p < 0.05, ****p < 0.0001, n = 4).
Genetic knockout TGF-β receptor 2 in fibroblasts improves functional recovery of mice after SCI
To confirm the functional recovery of mice after SCI in Tgfbr2Col1α2−/− mice. Co-staining of 5-HT+ and β-III-tublin+ was used to detect neurological function recovery, BMS and gait analysis were used to examine motor functional recovery of the hind limb. The results showed increased 5-HT+ axons and β-III-tublin+ nerves in the lesion area in Tgfbr2Col1α2−/− mice (Fig. 5a–c). Moreover, the BMS score was significantly elevated since 42d and the gait analysis revealed improved hind limb recovery in print area, stride length, and print length in Tgfbr2Col1α2−/− mice (Fig. 5d–h). Altogether, the releasing of axon inhibitory molecule EphrinB2 was mostly affected by fibroblasts via TGF-β activation. And genetic knockout TGF-β receptor 2 in fibroblasts could attenuate the secretion of EphrinB2 and then improve functional recovery of mice after SCI.
a Representative images of immunofluorescent analysis of 5-HT (red), β-III-tublin (green), and DAPI (blue) in each group at 4 weeks after SCI. Scale bars = 200 μm. Right images are high-resolution versions of the boxed regions in the left images, scale bars = 50 µm. b, c Quantitative analysis of intensity mean value of 5-HT and β-III-tublin (*p < 0.05, **p < 0.01, ****p < 0.0001, n = 4). d Quantitative analysis of BMS score between 13C4 control mice after SCI, 1D11 group mice after SCI, and mice without SCI (**p < 0.01, n = 6). e–h Quantitative analysis of catwalk, including print length, stride length and print area (*p < 0.05, **p < 0.01, n = 6). LF left front paw, RF right front paw, RH right hind paw. Statistical significance was determined by multifactorial ANOVA, and all data are shown as means ± standard deviations.
MiR-488 regulates FSP1+ fibroblasts distribution and EphrinB2 expression in the lesion site
A number of previous studies have shown that miRNAs are playing a crucial role in fibroblasts transition and regulation of nerve function [21,22,23]. In order to study the upstream of the EphrinB2, we predicted the miRNAs related to fibroblasts capable of regulating EphrinB2 after SCI through the bioinformatics website and GEO dataset (GSE131253), combining with the use of a Venn map. The result showed that 3 genes were co‐expressed, namely, miR‐488, miR-721, and miR-207 (Fig. 6a). However, only miR-488 was significantly upregulated in 1D11 injection group relative to 13C4 control group after validating their expression via qPCR in vivo (Fig. 6b). To detect the number of FSP1+ fibroblasts and expression EphrinB2, mice received intravenous injections of miR-488 inhibitors and miR-488 mimic. The immunostaining results showed markedly decreased FSP1+ fibroblasts and EphrinB2 expression in miR-488 injected group, while FSP1+ fibroblasts and EphrinB2 expression were highly increased after miR-488 mimics injection (Fig. 6c–e). In addition, co-staining of Collagen III and β-III-tublin revealed decreased fibrotic scar and increased nerve distribution in miR488 inhibitor group. However, markedly increased fibrotic scar and significantly decreased nerve were observed after miR-488 mimics injection (Fig. 7a–c). Taken together, TGF-β could stimulate FSP1+ fibroblasts accumulation in the surgery site then regulate the expression of EphrinB2 by targeting miR-488 in fibroblasts. Indicating knockout TGF-β could decrease the FSP1+ fibroblasts accumulation then lessen Collagen III+ fibrotic scar, moreover, reduced axon inhibitory EphrinB2 could induce axon regeneration, nerve survival, and motor function recovery.
a Prediction of targeted miRNAs in fibroblasts capable of regulating EphrinB2 after SCI via miRDB, miRNAMap, GEO(GSE131253) and mirnaid. b Relative expression level of the three miRNAs that were screened out are validated in 13C4 control group and 1D11 group mice at 2 weeks after SCI by qPCR. c Representative images of immunofluorescent analysis of FSP1 (red), EphrinB2 (green) and DAPI (blue) in each group at 2 weeks after SCI. Scale bars = 100 μm. d, e Quantitative analysis of relative fold change of EphrinB2 and FSP1 positive cells/ fileld (*p < 0.05, **p < 0.01, ns no significance, n = 4).
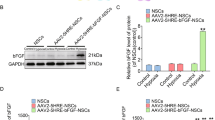
a Representative images of immunofluorescence analysis of collagen III (red), β-III-tublin (green) and DAPI (blue) in miR-488 inhibitor-treated mice and control group mice after SCI and mice without surgery (Sham) at 2 weeks. Scale bars = 200 μm. b, c Quantitative analysis of intensity mean value of collagen III and β-III-tublin in each group (*p < 0.05, **p < 0.01, n = 4). d The regulatory mechanism of miR-488 was through MAPK signaling pathway. Representative western blots showing the expression of pErk and Erk in the lesion area of spinal cord from Tgfbr2f/f mice without SCI, Tgfbr2f/f mice with SCI, Tgfbr2Col1α2−/− mice with SCI and Tgfbr2Col1α2−/− mice with miR484 inhibitor treatment after SCI in vivo. e Quantitative analysis of the relative pErk/ Erk expression in different groups (*p < 0.05, ***p < 0.001, ****p < 0.0001, n = 3).
The regulatory mechanism of miR-488 was through MAPK signaling pathway
Then, we explored if MAPK pathways take part in the miR-488 regulated process. We used western blot to assess the total protein and phosphorylated protein expression of ErK1/2. Results showed significant increased pErK expression in miR-488 mimics group and markedly decreased in miR-488 inhibitor group, which indicates the activation of MAPK signaling. Collectively, TGF-β regulated the expression of EphrinB2 by targeting miR-488 in fibroblasts and MAPK signaling pathway was involved in miR-488 regulation (Fig. 7d, e).
Discussion
Following SCI, little regeneration of axons and survival of neurons in the lesion area occurs. It has long thought that glia scar could attenuate axon regeneration by secreting CSPGs, which can inhibit axon regeneration [24, 25]. However, more and more studies suggest that glia scars are fundamental supporting factors for axon regeneration, neuroprotection, and tissue repair [26,27,28]. After SCI, fibroblasts, and macrophages invade and infiltrate into the lesion area, then fibroblasts could multiply and express fibronectin, collagens, and laminin to form the fibrotic scar which presents as a physical barrier to block the axon regeneration [15, 29]. In addition, fibroblasts can also secrete various inhibitory molecules including tenascin-C, ephrinB2, and NG2 [15, 19, 30].
EphrinB2 is a cell surface transmembrane ligand of the hepatocellular carcinoma B receptor that produces erythropoietin, and is commonly expressed in mammals. Emerging studies show that EphrinB2 reverse signaling is essential for angiogenesis during development and disease progression [31, 32]. In the skeletal microenvironment, ephrin-B2 was mainly detected in human articular cartilage cells and osteoclasts [33]. The physiological interaction between these proteins promotes bone homeostasis, and its dysfunction can induce multiple myeloma [34, 35]. After SCI, the expression of EphrinB2 was upregulated in astrocytes and knockout EphrinB2 in astrocytes could induce axon regeneration after SCI in mice [36, 37]. EphrinB2 is expressed in the midbrain dopaminergic neurons, and the ligand specifically inhibits the growth of neurites and induces the cell loss of substantia nigra, but not ventral tegmental, dopaminergic neurons [38]. However, whether EphrinB2 secreted by fibroblasts could inhibit axon growth after SCI and intrinsic mechanism was unclear.
TGF-β plays a big role in cancer, scar deposition, and neurodegeneration. After SCI, following the increased inflammatory cytokines, TGF-β was highly expressed at the lesion site [39,40,41,42]. TGF-β mediates tissue fibrosis associated with inflammation and tissue damage. In addition, TGF-β induces fibroblasts to activate and differentiate into myofibroblasts then secrete extracellular matrix proteins [43]. Although some studies have shown TGF-β signaling pathway is significantly and selectively activated during the formation of the fibrotic scar [15, 36, 44] and spinal cord axon growth improvement [45,46,47]. However, the mechanism of how TGF-β activates fibrotic scar formation and then attenuates axon growth is still unknown.
In our study, systemic injection of TGF-β neutralizing antibody could induce the protection of axon growth, survival of neurons, and functional recovery, whereas EphrinB2 expression and fibroblasts distribution are attenuated. To validate the TGF-β activation in fibroblasts, we also knockout TGF-β type II receptor in fibroblasts by using Tgfbr2Col1α2−/− mice. Decreasing EphrinB2 expression and improved SCI recovery was also observed.
Furthermore, miR-488 was confirmed to be the most upregulated gene related to EphrinB2 releasing in fibroblasts after SCI by gene prediction. And our data suggested that miR-488 initiates EphrinB2 expression and physical barrier building through MAPK signaling after SCI (Fig. 8). In conclusion, our study points toward elevated levels of active TGF-β as inducer and promoters of fibroblasts distribution, fibrotic scar formation and EphrinB2 expression, and deletion of global TGF-β or the receptor of TGF-β in Col1α2 lineage fibroblasts significantly improve functional recovery after SCI, which suggest that TGF-β might be a therapeutic target in SCI.
Materials and methods
Mice
All animal experimental protocols were approved by the Animal Care and Use Committee of Tianjin Medical University. The Col1α2-CreER (Stock number: 029567) mice, Tgfbr2flox/flox (Stock number: 012603) mice, and 8-week-old C57BL/6J (wild type, WT, Stock number: 000664) mice were purchased from Jackson Laboratory. Heterozygous Col1α2-CreER mice were crossed with Tgfbr2flox/flox mice. The offspring were intercrossed to generate the following genotypes: Col1α2-CreER (tamoxifen-inducible Cre recombinase driven by the Col1a2, collagen, type I, alpha 2, promoter), Tgfbr2flox/flox (mice homozygous tgfbr2 flox allele, referred to as Tgfbr2f/f in the text), Col1α2-CreER:: Tgfbr2flox/flox (conditional deletion of Tgfb receptor 2 in Col1α2 lineage cells, referred to as Tgfbr2Col1α2−/− in the text). All animals were housed in identical environments (temperature 22–24 °C; humidity 60–80%) on a 12-h light-dark cycle.
Surgical procedures and treatment
Eight-week-old female mice were anesthetized by intraperitoneal injection with ketamine (75 mg/kg) and xylazine (10 mg/kg). Laminectomy of a single vertebra was performed to expose the spinal cord at the level of T10, then severe crush SCI was made by using No. 5 Domont forceps (Fine Science Tools, Foster City, CA) without spacers and with a tip width of 0.5 mm to completely compress the entire spinal cord laterally from both sides for 5s [26, 48,49,50]. Returned the mice to the home cages after recovery on a heating pad. Bladders were manually compressed twice a day and antibiotic (Gentamycin sulfate, Abcam, ab146573) was administered once a day for 3 days post-surgery. Animals were randomly assigned numbers and evaluated thereafter blind to genotype and experimental condition.
For the antibody treatment experiment, 8-week-old WT female mice were intraperitoneally injected TGF-β neutralizing antibody (1D11; R&D Systems, Minneapolis, MN) or vehicle antibody of an identical IgG complex lacking any TGF-β-binding capabilities (13C4; R&D Systems, Minneapolis, MN) 5 mg/kg body weight for three times a week post SCI. Tail vein injections of a specific miR-488 inhibitor (synthesized by Millipore Sigma) were initiated at 48 h post SCI (100 µmol).
Behavioral analysis
At 1, 3, 5, 7, 14, 28, 42, and 56d post SCI, hindlimb movements were scored using the Basso Mouse Scale (BMS) in which 0 is no recovery and 9 is normal locomotor mobility [20]. Automated gait analysis was also performed pre–surgery and at 8 weeks post–surgery by using a “CatWalk” system (Noldus) [51]. All experiments were performed during the same period of the day (1:00 PM to 4:00 PM). For BMS, at least two examiners were blinded to the experimental group observed each mouse for 5 min. For Catwalk test, each mouse was trained to cross the Catwalk walkway daily for 7 days before SCI or control operation.
Immunohistochemistry, immunofluorescence
At the designated time point, the spinal cord harvested from the mice were fixed with 4% paraformaldehyde overnight and dehydrated in 20% sucrose solution for 24 h. After embed in optimal cutting temperature compound (OCT, Sakura Finetek), 20-μm-thick sagittal sections of the spinal cords were obtained using a cryostat microtome.
Immunostaining was performed using a standard protocol. Briefly, the 20th–25th slices were selected to incubate with primary antibodies at 4 °C overnight after blocking at room temperature by blocking solution (0.5% Triton X-100 in PBS and 5% donkey serum) for 1 h. The primary antibodies used were as follows: rabbit anti-5-HT (1:50, sc-65495, Santa Cruz Biotechnology), rabbit anti-FSP1 (1:300, 07-2274, Millipore), rabbit anti-EphrinB2 (1:100, MA5-32740, ThermoFisher Scientific), mouse anti-β-III-tublin (1:100, MA1-118, Invitrogen), rabbit anti-CollagenIII (1:100, ab7778, Abcam). The corresponding secondary antibodies were incubated 1 h at room temperature. Immunofluorescent images were captured using an LSM 780 confocal microscopy (Zeiss, Germany).
Prediction of target miRNAs
The target miRNAs were predicated using the GEO database (GSE131253, http://www.ncbi.nlm.nih.gov/geo/), miRDB database (http://mirdb.org/cgi-bin/search.cgi), miRNAMap (http://mirnamap.mbc.nctu.edu.tw/) and miRWalk (mirnaid, http://mirwalk.umm.uni-heidelberg.de/). Only miRNAs identified consistently by these three databases were selected.
Quantitative real-time polymerase reaction chain (qPCR)
The total RNA of the cells was extracted and purified using RNeasy Plus kit (Qiagen, USA) following the manufacturer’s instructions. For the reverse transcript, complementary DNA was synthesized using the SuperScript First-Strand Synthesis System (Invitrogen). The primers used in the RT-qPCR assay were synthesized by Life Technologies (ThemoFisher Scientific) based on sequences retrieved from miRDB database (http://mirdb.org/cgi-bin/search.cgi). The primer of miR-484 was: 5′-TCAGGCTCAGTCCCCTCCCGAC-3′, the primer of miR-721 was: 5′-CAGTG CAATTAAAAGGGGGAA-3′, and the primer of miR-207 was: 5′-GCTTC TCCTGGCTCTCCTCCCTC-3′. SYBR Green-Master Mix (Qiagen, Hilden, Germany) was used for the amplification and detection of cDNA on a C1000 Thermal Cycler (Bio-Rad Laboratories, CA). The mean cycle threshold (Ct) value of each target gene was normalized to the housekeeping gene GAPDH. The results were shown in a fold change using the ∆∆Ct method.
Elisa analysis
Whole blood sample was collected by cardiac puncture immediately after euthanasia of the mouse. The injured spinal cord tissue, around 1 cm in length at the level of T10, was ground into mud using a ceramic mortar and pestle under cooling. The mud of bone tissue was then homogenized in pre-cooled RIPA lysis and extraction buffer (ThermoFisher Scientific) for 1 h. The buffer solution was centrifuged at 15,000 rpm for 20 min at 4 °C. The supernatant was collected for protein concentration quantification with BCA Protein Assay Kit (ThermoFisher Scientific). An equal amount of protein from each sample was subjected to determine the concentration of active and total TGF-β1 in the serum and spinal cord by using TGF-β1 ELISA Development kit (R&D system, MB100B) following the manufacturer’s instruction.
Western blotting
The total protein from the spinal cord was lysed using radioimmunoprecipitation assay (RIPA) lysis and extraction buffer (ThermoFisher Scientific) supplemented with protease inhibitor cocktail (ThermoFisher Scientific). After centrifugation at 15,000 × g for 10 min at 4 °C, the supernatants were collected for measuring the protein concentration with BCA Protein Assay Kit (ThermoFisher Scientific). Load 30 µg of total protein per well and the proteins were separated by SDS-PAGE and blotted on a polyvinylidene difluoride (PVDF) membrane (Bio-Rad Laboratories, Hercules, CA, USA). The membrane was blocked in 5% w/v bovine serum albumin (BSA, Sigma-Aldrich) and incubated with blocking buffer diluted primary antibodies overnight at 4 °C. The primary antibodies used include EphrinB2 (1:1000, ThermoFisher Scientific), ERK (1:1000; CST), p-ERK (1:1000; CST) and β-actin (1:1000, CST). The protein bands were visualized by ECL substrate (ThermoFisher Scientific) and exposed under ChemiDoc XRS System (BioRad, USA).
Statistics
All data analyses were performed and illustrated using Prism software (Version 7, GraphPad, USA). Data are presented as means ± standard deviations (SD). For comparisons between two groups, we used two-tailed Student t-tests. For comparisons among multiple groups, we used one-way or two-way analysis of variance (ANOVA) followed by Tukey’s multiple-comparison post hoc test. The level of significant difference among groups was defined and noted as *p < 0.05, **p < 0.01, ***p < 0.001, ****p < 0.0001. Sample size was based on preliminary data as well as on observed effect sizes.
Change history
18 August 2022
This article has been retracted. Please see the Retraction Notice for more detail: https://doi.org/10.1038/s41420-022-01159-2
References
Ahuja CS, Wilson JR, Nori S, Kotter MRN, Druschel C, Curt A, et al. Traumatic spinal cord injury. Nat Rev Dis Primers. 2017;3:17018.
McDonald JW, Sadowsky C. Spinal-cord injury. Lancet. 2002;359:417–25.
Courtine G, Sofroniew MV. Spinal cord repair: advances in biology and technology. Nat. Med. 2019;25:898–908.
Tang X, Davies JE, Davies SJ. Changes in distribution, cell associations, and protein expression levels of NG2, neurocan, phosphacan, brevican, versican V2, and tenascin-C during acute to chronic maturation of spinal cord scar tissue. J Neurosci Res. 2003;71:427–44.
Cooper JG, Jeong SJ, McGuire TL, Sharma S, Wang W, Bhattacharyya S, et al. Fibronectin EDA forms the chronic fibrotic scar after contusive spinal cord injury. Neurobiol Dis. 2018;116:60–68.
D’Ambrosi N, Apolloni S. Fibrotic scar in neurodegenerative diseases. Front Immunol. 2020;11:1394.
Poniatowski LA, Wojdasiewicz P, Gasik R, Szukiewicz D. Transforming growth factor Beta family: insight into the role of growth factors in regulation of fracture healing biology and potential clinical applications. Mediators Inflamm. 2015;2015:137823.
Xu X, Zheng L, Yuan Q, Zhen G, Crane JL, Zhou X, et al. Transforming growth factor-beta in stem cells and tissue homeostasis. Bone Res. 2018;6:2.
Wan M, Li C, Zhen G, Jiao K, He W, Jia X, et al. Injury-activated transforming growth factor beta controls mobilization of mesenchymal stem cells for tissue remodeling. Stem Cells. 2012;30:2498–511.
Blobe GC, Schiemann WP, Lodish HF. Role of transforming growth factor beta in human disease. N Engl J Med. 2000;342:1350–8.
Tang Y, Wu X, Lei W, Pang L, Wan C, Shi Z, et al. TGF-beta1-induced migration of bone mesenchymal stem cells couples bone resorption with formation. Nat. Med. 2009;15:757–65.
Wang X, Li F, Xie L, Crane J, Zhen G, Mishina Y, et al. Inhibition of overactive TGF-beta attenuates progression of heterotopic ossification in mice. Nat Commun. 2018;9:551.
Zhen G, Wen C, Jia X, Li Y, Crane JL, Mears SC, et al. Inhibition of TGF-beta signaling in mesenchymal stem cells of subchondral bone attenuates osteoarthritis. Nat Med. 2013;19:704–12.
Li S, Gu X, Yi S. The regulatory effects of transforming growth factor-beta on nerve regeneration. Cell Transpl. 2017;26:381–94.
Wang W, Liu R, Su Y, Li H, Xie W, Ning B. MicroRNA-21-5p mediates TGF-beta-regulated fibrogenic activation of spinal fibroblasts and the formation of fibrotic scars after spinal cord injury. Int J Biol Sci. 2018;14:178–88.
Assinck P, Duncan GJ, Hilton BJ, Plemel JR, Tetzlaff W. Cell transplantation therapy for spinal cord injury. Nat Neurosci. 2017;20:637–47.
Wei Y, Kim TJ, Peng DH, Duan D, Gibbons DL, Yamauchi M, et al. Fibroblast-specific inhibition of TGF-beta1 signaling attenuates lung and tumor fibrosis. J Clin Invest. 2017;127:3675–88.
Zhu Y, Soderblom C, Trojanowsky M, Lee DH, Lee JK. Fibronectin matrix assembly after spinal cord injury. J Neurotrauma. 2015;32:1158–67.
Soderblom C, Luo X, Blumenthal E, Bray E, Lyapichev K, Ramos J, et al. Perivascular fibroblasts form the fibrotic scar after contusive spinal cord injury. J Neurosci. 2013;33:13882–7.
Basso DM, Fisher LC, Anderson AJ, Jakeman LB, McTigue DM, Popovich PG. Basso Mouse Scale for locomotion detects differences in recovery after spinal cord injury in five common mouse strains. J Neurotrauma. 2006;23:635–59.
Zhang Q, Guo B, Hui Q, Chang P, Tao K. miR-137 Inhibits proliferation and metastasis of hypertrophic scar fibroblasts via targeting pleiotrophin. Cell Physiol Biochem. 2018;49:985–95.
Wu SG, Li HT, Wang LL, Yan L. Lidocaine promotes fibroblast proliferation after thermal injury via up-regulating the expression of miR-663 and miR-486. Kaohsiung J Med Sci. 2020;36:274–80.
Nagpal V, Rai R, Place AT, Murphy SB, Verma SK, Ghosh AK, et al. MiR-125b is critical for fibroblast-to-myofibroblast transition and cardiac fibrosis. Circulation. 2016;133:291–301.
Yiu G, He Z. Glial inhibition of CNS axon regeneration. Nat Rev Neurosci. 2006;7:617–27.
Silver J, Miller JH. Regeneration beyond the glial scar. Nat Rev Neurosci. 2004;5:146–56.
Anderson MA, Burda JE, Ren Y, Ao Y, O’Shea TM, Kawaguchi R, et al. Astrocyte scar formation aids central nervous system axon regeneration. Nature. 2016;532:195–200.
Liddelow SA, Barres BA. Regeneration: not everything is scary about a glial scar. Nature. 2016;532:182–3.
Shechter R, Raposo C, London A, Sagi I, Schwartz M. The glial scar-monocyte interplay: a pivotal resolution phase in spinal cord repair. PLoS ONE. 2011;6:e27969.
Klapka N, Muller HW. Collagen matrix in spinal cord injury. J Neurotrauma. 2006;23:422–35.
Kawano H, Kimura-Kuroda J, Komuta Y, Yoshioka N, Li HP, Kawamura K, et al. Role of the lesion scar in the response to damage and repair of the central nervous system. Cell Tissue Res. 2012;349:169–80.
Adams RH, Diella F, Hennig S, Helmbacher F, Deutsch U, Klein R. The cytoplasmic domain of the ligand ephrinB2 is required for vascular morphogenesis but not cranial neural crest migration. Cell. 2001;104:57–69.
Gerety SS, Wang HU, Chen ZF, Anderson DJ. Symmetrical mutant phenotypes of the receptor EphB4 and its specific transmembrane ligand ephrin-B2 in cardiovascular development. Mol Cell. 1999;4:403–14.
Matsuo K, Otaki N. Bone cell interactions through Eph/ephrin: bone modeling, remodeling and associated diseases. Cell Adh Migr. 2012;6:148–56.
Pennisi A, Ling W, Li X, Khan S, Shaughnessy JD Jr, Barlogie B, et al. The ephrinB2/EphB4 axis is dysregulated in osteoprogenitors from myeloma patients and its activation affects myeloma bone disease and tumor growth. Blood. 2009;114:1803–12.
Zhao C, Irie N, Takada Y, Shimoda K, Miyamoto T, Nishiwaki T, et al. Bidirectional ephrinB2-EphB4 signaling controls bone homeostasis. Cell Metab. 2006;4:111–21.
Li Y, Chen Y, Tan L, Pan JY, Lin WW, Wu J, et al. RNAi-mediated ephrin-B2 silencing attenuates astroglial-fibrotic scar formation and improves spinal cord axon growth. CNS Neurosci Ther. 2017;23:779–89.
Ren Z, Chen X, Yang J, Kress BT, Tong J, Liu H, et al. Improved axonal regeneration after spinal cord injury in mice with conditional deletion of ephrin B2 under the GFAP promoter. Neuroscience. 2013;241:89–99.
Yue Y, Widmer DA, Halladay AK, Cerretti DP, Wagner GC, Dreyer JL, et al. Specification of distinct dopaminergic neural pathways: roles of the Eph family receptor EphB1 and ligand ephrin-B2. J Neurosci. 1999;19:2090–101.
Chalmers KA, Love S. Neurofibrillary tangles may interfere with Smad 2/3 signaling in neurons. J Neuropathol Exp Neurol. 2007;66:158–67.
Logan A, Berry M, Gonzalez AM, Frautschy SA, Sporn MB, Baird A. Effects of transforming growth factor beta 1 on scar production in the injured central nervous system of the rat. Eur J Neurosci. 1994;6:355–63.
Ueberham U, Ueberham E, Gruschka H, Arendt T. Altered subcellular location of phosphorylated Smads in Alzheimer’s disease. Eur J Neurosci. 2006;24:2327–34.
Yamagata H, Matsuzaki K, Mori S, Yoshida K, Tahashi Y, Furukawa F, et al. Acceleration of Smad2 and Smad3 phosphorylation via c-Jun NH(2)-terminal kinase during human colorectal carcinogenesis. Cancer Res. 2005;65:157–65.
Khalil H, Kanisicak O, Prasad V, Correll RN, Fu X, Schips T, et al. Fibroblast-specific TGF-beta-Smad2/3 signaling underlies cardiac fibrosis. J Clin Invest. 2017;127:3770–83.
Joko M, Osuka K, Usuda N, Atsuzawa K, Aoyama M, Takayasu M. Different modifications of phosphorylated Smad3C and Smad3L through TGF-beta after spinal cord injury in mice. Neurosci Lett. 2013;549:168–72.
Hellal F, Hurtado A, Ruschel J, Flynn KC, Laskowski CJ, Umlauf M, et al. Microtubule stabilization reduces scarring and causes axon regeneration after spinal cord injury. Science. 2011;331:928–31.
Lagord C, Berry M, Logan A. Expression of TGFbeta2 but not TGFbeta1 correlates with the deposition of scar tissue in the lesioned spinal cord. Mol Cell Neurosci. 2002;20:69–92.
Rhett JM, Ghatnekar GS, Palatinus JA, O’Quinn M, Yost MJ, Gourdie RG. Novel therapies for scar reduction and regenerative healing of skin wounds. Trends Biotechnol. 2008;26:173–80.
Faulkner JR, Herrmann JE, Woo MJ, Tansey KE, Doan NB, Sofroniew MV. Reactive astrocytes protect tissue and preserve function after spinal cord injury. J Neurosci. 2004;24:2143–55.
Herrmann JE, Imura T, Song B, Qi J, Ao Y, Nguyen TK, et al. STAT3 is a critical regulator of astrogliosis and scar formation after spinal cord injury. J Neurosci. 2008;28:7231–43.
Wanner IB, Anderson MA, Song B, Levine J, Fernandez A, Gray-Thompson Z, et al. Glial scar borders are formed by newly proliferated, elongated astrocytes that interact to corral inflammatory and fibrotic cells via STAT3-dependent mechanisms after spinal cord injury. J Neurosci. 2013;33:12870–86.
Hamers FP, Koopmans GC, Joosten EA. CatWalk-assisted gait analysis in the assessment of spinal cord injury. J Neurotrauma. 2006;23:537–48.
Funding
This work was supported by the following funding: National Natural Science Foundation of China (Project Number: 81772342, 82072439), Key Program of Natural Science Foundation of Tianjin (19JCZDJC36300), International Cooperation Program of National Natural Science Foundation of China (81620108018).
Author information
Authors and Affiliations
Contributions
DP, GN, and SF conceived of the presented idea. DP, YL, and FY carried out the experiment. SZ verified the analytical methods and assembled the figures. DP wrote the manuscript with support from FY All authors discussed the results and contributed to the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Mice were involved in this study, and the statement on ethics approval has been included in our manuscript.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article has been retracted. Please see the retraction notice for more detail: https://doi.org/10.1038/s41420-022-01159-2"
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Pan, D., Yang, F., Zhu, S. et al. RETRACTED ARTICLE: Inhibition of TGF-β repairs spinal cord injury by attenuating EphrinB2 expressing through inducing miR-484 from fibroblast. Cell Death Discov. 7, 319 (2021). https://doi.org/10.1038/s41420-021-00705-8
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41420-021-00705-8
This article is cited by
-
Serum microRNA as a potential biomarker for the activity of thyroid eye disease
Scientific Reports (2023)