Abstract
Herein, we describe the clinical and hematological features of three genetically related families predisposed to myeloproliferative neoplasms (MPNs). Using whole-exome sequencing, we identified a c.1367delG mutation(p.Arg456fs) in CHST15 (NM_001270764), a gene encoding a type II transmembraneglycoproteinthat acts as a sulfotransferase and participates in the biosynthesis of chondroitin sulfate E, in germline and somatic cells in familial MPN. CHST15defects caused an increased JAK2V617F allele burden and upregulated p-Stat3 activity,leading to an increase in the proliferative and prodifferentiation potential of transgenic HEL cells. We demonstrated that mutant CHST15 is able to coimmmunoprecipitate the JAK2 protein,suggesting the presence of a CHST15-JAK2-Stat3 signaling axis in familial MPN. Gene expression profiling showed that the FREM1, IFI27 and C4B_2 genes are overexpressed in familial MPN, suggesting the activation of an “inflammatory response-extracellular matrix-immune regulation” signaling network in the CHST15 mutation background.We thus concluded that CHST15 is a novel gene that predisposes to familial MPN and increases the probability of disease development or transformation.
Similar content being viewed by others
Introduction
Myeloproliferative neoplasms (MPNs) are a heterogeneous group of disorders including polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), that manifest, in most instances, in a sporadic form. However,familial clustering of MPN has been reported [1,2,3] and accounts for 5–10% of MPN cases [1, 3, 4]. Familial MPN is clinically indistinguishable fromsporadic MPN, and frequent somatic JAK2 and CALRmutations exist [1, 3, 5]. Mutations in other germline genes, such as TET-2 [6, 7], TERT [8, 9], ATG2B/GSKIP [10], MECOM, HBS1L-MYB [11], and RBBP6 [12], may contribute to a small portion of familial MPN cases. However, the causative germline mutation in the majority of familial MPN cases is unknown. Independent acquisition of several oncogenic mutations in a single patient with MPN suggested that an unidentified germline predisposition locus might be present in some sporadic cases. The JAK2 46/1 haplotype with the JAK2 mutation encoding p.Val617Phe was shown to increase the risk of developing MPN [13, 14]. Overall, the 46/1 haplotype has been estimated to account for 50% of the population attributable risk of developing an MPN in European populations, but it cannot explain and revealthegenetic predisposition factor for familial MPN inpopulations from different ethnic groups and geographical origins.
In the present study,we identified the c.1367delG (pArg456fs) mutation in the carbohydrate sulfotransferase 15(CHST15) gene in three Chinese families with MPN viawhole-exome sequencing. This mutation is responsible for earlier-onset PMF and the tendency toward progressive acceleration or transformation. We demonstrated that thisCHST15 mutation is associated with an increased JAK2V617F allele burden and upregulatedp-Stat3 activity. We also confirmed that this CHST15 mutation endows MPN cells with increased proliferative activity and prodifferentiation potential, suggesting that this CHST15 mutation is a candidate for predisposition to familial MPN.
Materials and methods
Patients and samples
Patients were diagnosed with PMF and ET according to the World Health Organization (WHO) criteria [15]. Familial cases were defined when two or more individuals in the same pedigree were affected with MPNs.Blood samples from familial patients (n = 6), family members (n = 9), patients with sporadic MPN (n = 110) and healthy subjects (n = 160) were collected after informed written consent was obtainedin accordance with the Declaration of Helsinki. This study was approved by the institutional ethics committee of The Second Xiang-Ya Hospital, Central South University. To detect germline mutations in the CHST15 gene,oralmucosacells were retrieved frompatients with familial MPN (n = 6), patients with sporadic MPN (n = 30) and normal controls (n = 30) and were prepared with a Swab Pack (Isohelix, UK) as previouslydescribed [16]. JAK2(V617F) andMPN-specificsomatic mutations (JAK2-V617F, MPL-W515L,CALR-type 1 and JAK2 exon 12 mutation) were screenedin granulocyte DNA as previously described [17].
Whole-exome sequencingof germline and somatic cells
We performed whole-exome sequencing (WES) on germline and somatic cells fromthe threefamily members with MPN (n = 6).Genomic DNA was extracted from freshly peripheral blood mononuclear cells (PBMNCs) andoralmucosacells and was fragmentedand hybridized to capture arrays for enrichment. Exome capture sequencing was performed on the HiSeq 4000 platform by BGI-Tech with the paired-end 150 bp read option according to the manufacturer’s instructions (Wuhan, China). BWA software was used to align paired-end reads to the reference human genome (hg19, downloaded from http://genome.ucsc.edu/) with default parameters. After alignment, only uniquely mapped reads or confidently mapped paired-endreads were retained. Alignment calibration was performedby GATK, and Picard was used to mark duplicate reads from PCR. VarScan and SAM tools were employed to detect somatic variations or insertion/deletions (INDELs), and the data were processed by further filtering to eliminate false positives.
All mutations were annotated with ANNOVAR
Gene expression profiling and data analysis
Blood samples were collected from six patients with familial MPN (PMF, 4; ET, 2), their family members (n = 2 for ET), and four patients with sporadic MPN (PMF, 2; ET, 2), and total RNA wasextracted. Twelve sampleswere analyzedon the BGISEQ-500 platform,and a total of 17,610 genes were assayed. Microarrayhybridization was performed according to the manufacturer’s protocols. Differentially expressed genes between twosamples were identified through fold-change filtering (≥2.0). Pathway analysis was performed with gene mapping to KEGG pathways (P < 0.05). Pathway and GOanalyses were applied to determine the functions of differentially expressed genes in these biological pathways or GO terms. Finally, hierarchical clustering was used to distinguish gene expression among samples.
Analysis of the JAK2V617F mutational burden and phosphorylation ofStat3/5 as well as p38
DNA was extracted from fresh frozen PBMNCs in samples from 5 patients with familial MPN and 50 patients with sporadic MPN using a TIANamp Genomic DNA Kit (Tiangen, China). The JAK2V617F mutant allele burden was measured by quantitative real-time PCR(qRT-PCR) as previously described [18]. Amplification was performed in a Rotor Gene real-time PCR 6000 system (Corbett Research, Wasserburg, Germany). Genomic DNA (20 ng) was used as the template. Primer sequences flanking the mutated region were employed with TaqMan probes (the sequences are available insupplemental materials (1)). The amount of the JAK2V617F allele was calculated by comparison with serial dilutions of mutant DNA obtained from a PMF patient with amutant allele percentage of 100% and wild-type DNA obtained from healthy individual. The mean of triplicate ΔCT determinations (CT JAK2V617F–CT JAK2WT) was used to calculate the mutant allele percentage. Usingflow cytometry, assays of p-Stat3,p-Stat5 and p-p38 protein abundancesinPBMNCs from patients with familial MPN (n = 5) and sporadic MPN (n = 15) were performed.
Immunoprecipitation
Immunoprecipitation was performed with wild-type CHST15 and mutant CHST15 in HEL cells and PBMNCs from patients with familial MPN (n = 6),sporadic MPN with JAK2V617F mutation (n = 3), MPN with CALR mutation (n = 3), and triple-negative MPN (n = 3). The cells were lysed in RIPA lysis buffer. Before immunoprecipitation, the samples were precleared by adding 20 μL of Protein A/G PLUS-agarose (Santa Cruz,, Texas) and 1 μg of control IgG. Lysates were incubated overnight at 4 °C with anti-JAK2 or anti-Flag-CHST15 antibodies, as well as with anti-Calnexin, anti-Cyclin B1, anti-HCK and anti-IFI27 antibodies. Affinity beads were collected and washed with immunoprecipitation buffer, and bound proteins were eluted. Eluates were resolved by SDS-PAGE and immunoblotted with specific antibodies.
Confocal immunofluorescence microscopy
Flag (3 × Flag)-tagged wild-type CHST15 and mutant CHST15 were cloned into the CV548 vector (Genechem, Shanghai, China). HEL cells were plated and cultured in RPMI 1640 medium supplemented with 10% FCS. Cells were transfected using Liposomal Transfection Reagent (Hanbio, Shanghai, China) with 4.0 µg of 3 × Flag-CHST15WT or 3 × Flag-CHST15 Mut plasmid as well as 2.0 µl of transfection reagent. Transfected cells were selected in medium containing 2 µg/ml puromycin (Thermo Fisher Scientific, USA). After the cells were washed, fixed (4% paraformaldehyde) and permeabilized (0.1% Triton X-100), a blocking step was performed at room temperature (4% bovine serum albumin in PBS). Then, the cells were washed with 1 × PBS and incubated with anti-FLAG (mouse mAb, Sigma–Aldrich) and anti-JAK2 (rabbit mAb, Cell Signaling) antibodies overnight at 4 °C. After washing, the cells were stained with an Alexa Fluor 488-conjugated anti-mouse antibody and an Alexa Fluor 594-conjugated anti-rabbit antibody (Invitrogen) for 1 h and were then incubated in DAPI for 1 h at 37 °C. Finally, the cells were visualized and imaged using a confocal laserscanning microscope (Zeiss, Jena, Germany).
Other methods and materials
The details of the other methods used in this study, i.e. colony formation experiment, RNA extraction, cDNA synthesis, and qRT-PCR of CHST15 mRNA, lentiviral vector constructs and CHST15 gene transfection, differentiation markers analysis of CHST15 mutants, Immunoblotting assay, Wright-Giemsa staining [19]. Additional information concerning the sequences of primers for PCR amplification or Sanger sequencing are available in theOnline Supplementary Materials.
Statistical analyses
Quantitative data are presented as the mean ± standard error ofmean (SEM). Comparisons between groupswere made with one-way ANOVA or a Mann–Whitney Utest. Statistical differences were considered significant at P < 0.05.
Results
Clinical characteristics
Our study cohort included 6 patients with MPN with germline CHST15 mutations from 3 unique families.There were 5 females and 1 male; the age at disease onset ranged from 28 to 55 years, with a median age of 46.3 years. The course of the disease was 6 to 13 years, with a median survival periodof 9.67 years. The patients were followed - upcontinuously for 7–12 years.The patients experienced either malaise with left upperabdominal discomfort (4 PMF patients) or fatigue (2 ET patients). Additional testing revealed the presence of the JAK2V617F mutation in 5 cases and the CALR gene mutation in 1 case. Upon evaluation, 2 patients (Family 1) had moderate anemia (PMF), and 5 patients displayed an increased platelet count (range: 342–1100 × 109/L).All PMF patients were found to have splenomegaly with the spleen tip 3–5 cm below the left umbilical margin. Bone marrow biopsy showed increased megakaryocytes and strong reticulin staining (MF-3). Concurrent cytogenetic analysis revealed normal karyotypes.Six years after diagnosis, doubleframeshift mutations at two loci in ASXL1 (c.1934dup, p.Gly646TrpfsTer12 and c.2428_2431del, p.Asp810MetfsTer7) were found in one patient with PMF (family 2) during screeningfor MPN-related genes. One patient was found to have a mutation in TET2 (p.Asn427ValfsTer4) (family 1) and TP53 (p.Lys164AsnfsTer6) mutation and has gotten into MDS-EB-II, then, transformed into AML and did of severe pneumonia. No patient experiencedthromboembolic events, and 3 (PMF) had an accelerated phase. Leukemic transformation occurredin two patients (family 1:proband 1; duration:12 years; Family 1; proband’s young sister; duration 12 years), proband 1 harbouring EZH2 (c.707delC (p.Thr236fs mutation experienced erythropoietic failure (normoblasts:2%) with severe anemia. Four months after treatment with ruxolitinib, the disease evolvedto myelodysplastic syndrome (MDS-EB-II, 13% myeloblasts) and transformed into acute myeloid leukemia; the patient finally died of infection and bone marrow failure on March 15, 2018. Notably, this case went through a dramaticevolution in that the original PMF transformed into PV and thenreturned to PMF until its evolution into MDS/AML. Another caseof PMF (family 1) has entered MDS-EB-II stage (17% myeloblast) at present. More interestingly, the two sisters suffered from the same MPN subtype, shared the same CHST15 mutation and undergone a similar transforming courses. A patient with ET (family 3) was complicated bycarcinoma of the uterine cervixin May 2019 (Fig. 1A). The characteristics of the CHST15 mutations in 6 patients with MPN are shown in Table 1.
Discovery of mutations through whole-exome sequencing
We captured and sequenced exomes from PBMNCs and oralmucosacellsfrom patients with familial MPN (n = 6). A recurrent germline and somatic mutation in CHST15 (c.1367delG, p.Arg456fs) were found in all six patients and five patients, respectively. The prevalence of this mutation in the general population is 0/60 706 (in Exome Aggregation Consortium database). This mutation was not found in 160 healthy subjects or 110 patients with sporadic MPN. It is noteworthy that most patients (5/6) exhibited a canonical somatic mutation in CHST15 (c.1367delG, p.Arg456fs), except in one patient, who wasthe proband’solder sister in family 2 (germline mutation in CHST15 (c.1367delG, p.Arg456fs) was positive, CHST15somatic mutation wasabsent). Germline and somatic CHST15 mutations were confirmed by Sanger sequencing (Fig. 1B). In addition, family 1’s daughter and son, family 2’s son and daughter, and the proband’s parents in family 3 did not have both germline and somatic mutations. We also detected the germline CHST15pArg456fs mutation in 34 patients with sporadic MPN, and no mutations were found P) (Fig. 1B).
Familial MPN gene expression signatures involved in extracellular matrix and immune responses
Employing gene expression profiling assays, we identified 4 genes whose expression was significantly upregulated or downregulated in familial PMF. Among these genes, ERAS1-related extracellular matrix 1(FREM1) (p = 0.043), interferon alpha inducible protein 27(IFI27) (p = 0.032) and complement component 4B (C4B_2) (p < 0.0001) displayed obviousupregulation; amine oxidase copper domain-containing protein 1(AOC1) (p < 0.0001) was significantly downregulated (Fig. 2A). Relative to their expression in patients with sporadic ET, 12 genes were differentially expressed in 2 familial ET patients (Fig. 2B). These genes were mainly involved in RET signaling (SIGLEC14), ERK signaling, the actin cytoskeleton (TMSB4Y), cytokine receptor interaction signaling (RETN) and metabolism-related signaling (KDM5D, UTY). Gene expression profiles in both familial PMF and familial ET were integrated and compared mutually with those in sporadic PMF or ET. The results indicated that the expression of the neural proliferation differentiation and control protein 1 (NPDC1) gene was upregulated and the expression ofthe AOC1 gene was downregulated in familial MPN (Fig. 2C).
A Heatmap shows hierarchical clustering of expression profiles of 4 differentially expressed CHST15 target genes in familial PMF (red:upregulation;blue:downregulation). Microarray assay of genes with >2.0-fold upregulation or downregulation. B Familial essential thrombocythemia (ET) genes expression profiles. Heatmap shows hierarchical clustering of profiles of 12 differentially expressed genes. C Genes expression profiles both in familial PMF and in familial ET.
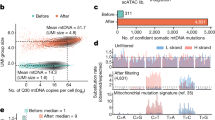
CHST15 mutation is complicated by upregulated JAK2V617F allele burden and enhanced p-STAT3 signaling
We determined the effects of CHST15 mutation on JAK2 mRNA and stat signaling. The JAK2V617F mutant allele burden (\({{{\bar{\mathrm x}}}}\) = 63.48% ± 24.15%)in 5 familial MPN patients (JAK2V617F positive) was significantly higher than that in patients with sporadic MPN (n = 50; \({{{\bar{\mathrm x}}}}\) = 21.84% ± 19.85%) (p = 0.016) (Fig. 3A). Flow cytometric assays showed that thep-Stat3 protein level (MFI: 83.36%) was obviously higher in familial MPN thanin sporadic MPN (n = 15) (MFI: 50.98%) (p < 0.001). There was no significant difference in p-Stat5 and p-p38levels between familial MPN and sporadic MPN (Fig. 3A, B). The western blot results demonstrated that cells harboring theCHET15 mutant had increased levels of p-Stat3 (Figs. 3C, S1).
A1 Histograms show significantly increased JAK2V617F allele burdens in familial MPNs with CHST15 mutation (p = 0.016). A2 Histograms indicate upregulated p-stat3 expression in familial MPNs corresponding to sporadic MPNs (n = 15) (p < 0.001); but no statistic difference is found for p-state5 and p-p38 between familial MPNs and sporadic MPNs. B1/B2: A representative FCM figures for p-stat3 and p-stat5 assays. Data are presented as mean ± s.e.m. ***p < 0.001; *p < 0.05, Student’s t test. C Western blot results show that cells harbouring CHET15 mutation present upregulated expression of p-stat3.
Familial PMF patients and HEL cells harboring the CHST15 mutant display downregulated CHST15 protein and mRNA expression
To test whether theCHST15 mutation influences the protein and mRNA expression of CHST15, western blotting and quantitative real-time PCR(qRT-PCR) were performed. The results showed that compared with sporadic PMF patients, patients with familial PMFexhibited significantly decreased CHST15 expression (Figs. 4A, S2), consistent with HEL cells harboring mutant CHST15 (Figs. 4B, S3). The qRT-PCR results indicated that CHST15 mRNA expression was obviously decreased in patients with familial MPN compared with patients with sporadic MPN and normal subjects and there were significant difference between familial MPN and sporadic MPN or normal controls (p < 0.05) (Fig. 4C).
A from left to right, CHST15 blotting bands represent sporadic MPN patients; healthy controls and familial MPN, respectively. B CHST15 protein expression on HEL cells with wild-type CHST15 (WT) and mutant CHST15 gene(Mut) and non - transfected HEL cells (HEL). C Quantitative RT-PCR analysis of CHST15 mRNA. Left panel: from left to right, F1-1, F1-2, F2-1, F2-2 indicate familial PMF; S1, S2, S3 indicate sporadic PMF; N1, N2, N3 indicate normal individuals. Results are means of three independent experiments. Right panel: when the mRNA expression levels were compared by pairwise comparison, the results showed that there was significantly depressed expression on CHST15 mRNA in familial MPN (p < 0.05).
The CHST15 variant confers a proliferative advantage and triggers the differentiation of HEL cells
We then sought to determine whether the CHST15 variant was associated with the disease phenotype. HEL cells, a human erythroleukemia cell line harboring the JAK2V617F mutation, were used as a cellular model, and cultured in the presence or absence of GM-CSF, G-CSF, EPO, SCF, and IL-3.The clone forming experiments showed that bothCHST15-WT and CHST15-Mut cells displayed cytokine-dependent growth,In the absence of growth factors, CHST15-Mutcells had stronger proliferative activity (p < 0.001), suggesting the growth manner was cytokine-independent (Fig. 5A). Cell cycle analysis showed that in the absence of cytokines, CHST15-Mut cells displayed an increase in proliferative index (S- and G2/M-phase populations) (p < 0.05) compared to those populations of CHST15-WT cells (Fig. 5B, C), implying that the CHST15 mutation overcomes G1 phase cell cycle block, resulting in enhanced growth potential.
A CHST15 mutant promotes HEL cells proliferation with cytokine-independent fashion (colony-forming tests): HEL cells harbouring CHST 15 mutant (1 × 105) or wild-type CHST15 (1 × 105) were plated under semisolid condition and colonies were counted 14 d after cultured. Shown are average colonies ± s.e.m; The experiment performed in triplicate. ***p < 0.001. B Analysis of cell cycle distribution: HEL cells with CHST15 mutant (MU) or CHST15 mutation-negative (WT) in the presence (WTC or MUC) or absence of cytokine were cultured in 1640 medium; cells were harvested at day 7 and were analyzed by flow cytometry. Compared with WT, HEL cells with CHST15 mutant showed an increased proliferative index (S phase plus G2/M phase%) (***p < 0.001), and independent of growth factors. C A representative image for cells cycle analysis. D Detection of differentiation markers by flow cytometry. demonstrated upregulation of cell surface markers CD14, CD15 and CD61 in HEL cells with CHST15 mutant in the presence of cytokines; whereas there was no effecton CD235a expression. Data are shownas the mean ± s.e.m of three independent experiments. E Morphological changes associated with differentiation of HEL cells were evidenced by Wright-Giemsa staining (100×). Upper panel: A2, A4 showed characteristics of myeloid differentiated in CHST15 mutant with shrunken cell nucleus and decreased the nuclear/cytoplastic ratio (N:C ratio) (A1-WT; A2-MU; A3-WT plus cytokine; A4-MU plus cytokine); Middle panel: B1, B4 represented monocytic differentiation with alleviated nuclear- folded and regular cellular outline in CHST15 mutant cells. (B1-WT; B2-MU; B3-WT plus cytokine; B4-MU plus cytokine); Lower panel: C1, C4 represents megakaryocytic differentiation (C1-WT; C2-MU; C3-WT plus cytokine; C4-MU plus cytokine).
We then investigated whether CHST15 mutation contributes to HEL cell differentiation.We measured the expression of myeloid (CD15, CD14), erythroid (CD235a) and megakaryocytic lineage (CD61) markers by flow cytometry. Notably, the results showed that CHST15 mutation enhanced the expression of CD15, CD14 and CD61, and this enhancementwas more evident in the presence of cytokines (Fig. 5D), suggesting that the CHST15 mutant endows HEL cells with increased differential potential toward the myeloid or megakaryocytic lineage. Wright-Giemsa staining confirmed that CHST15 mutation strikingly reduced the nuclear:cytoplasmic ratio (N:C ratio) compared to that of control HEL cells (Fig. 5E).
JAK2/CHST15 complex formation
We performed coimmunoprecipitation experiment on bothprimary PBMNCs from patients with familial MPN and HEL cells. The results showed that JAK2 coimmunoprecipitated with CHST15 in HEL cells (Fig. 6A, left); conversely, CHST15 directly interacted with JAK2 (Fig. 6A, right, Fig. S4). However, CHST15 could not be coimmunoprecipitated with calnexin, cyclin B1, HckorIFI27 (data not shown). In PBMNCs from patients with MPN, JAK2 interacted with CHST15. However, there were some differences in the strength of the interaction, The abundance of CHST15 in familial MPN harboringthe CHST15 mutation was lower than that in sporadic MPN. In addition, the abundance of JAK2 in familial MPN washigher than that in sporadic MPN (Figs. 6B, S5), suggesting an attenuated inhibitory effect of the CHST15 mutant on JAK2. The interaction between CHST15 and JAK2 was also confirmed by the acquisition of fluorescence images using a confocal laser scanning microscope, showing that JAK2 was mainly distributed on the plasma membrane and in the cytosol and nucleus, while CHST15 was mainly located onthe plasma membrane and in the cytosol. Compared with its location in wild-type cells, the JAK2/CHST15 complex was mainly localized on the inner side of the cell membrane in cells expressing the CHST15 mutant (Fig. 6C).
A Coimmunoprecipitation between JAK2 and CHST15 on HELcells harbouring CHET15 mutation (CHST15R456fs) or wild-type CHST15. left panel:anti-JAK2 antibody; right panel:anti- Flag-CHST15 antibody. Input, non-immunoprecipitated cell lysates; IgG, control IP with isotype antibody. B Coimmunoprecipitation between JAK2 and CHST15 on primary PBMNCs of patients with familial MPN (left panel: 1, 2, Familial 1. PMF: 3, 4. Familial 3. ET; 5,6. Familial 2, PMF.) or sporadic MPN (right panel: 1’, 2’, 3’: sporadic MPN with JAK2V617F; 4’, 5’, 6’: MPN with CALR mutation; 7’,8’,9’: MPN without mutation- triple negative). C Immunofluorescent colocalization of FLAG-tagged-CHST15 and JAK2. 4′,6-diamidino-2-phenylindole (DAPI) wasused for nuclear staining. The results show that both JAK2 and CHST15 are mainly found on cytomembrane and cytoplasm, and form co-precipitatation with granular shape between CHET15 and JAK2, suggesting exists in physical interaction both JAK2 and CHST15 (wild type) especially CHST15R456fs mutant.
Discussion
We identified CHST15 germline mutationscoexisting with somatic mutations that predispose to PMF and ET in three Chinese families. Our familial MPN cases had the same geographical origin, with an earlier MPN onset in comparison to sporadic cases (46.3 years versus 58.5 years [6]), an obvious female predominance and a tendency toward progressive transformation to an accelerated phase of PMF or acute myeloid leukemia. Consistent with theclinical features, our results showed that patients with the CHST15 mutation exhibited an increased JAK2V617F allele burden and activated p-stat3 signaling, suggesting that the CHST15 mutation cooperateswith the classical JAK2 V617F mutation to trigger the MPN phenotype. To explore the consequences of CHST15 mutation, we also established transgenic cell models. The subsequent results indicated that HEL cells harboring the CHST15 mutation displayed overt proliferative activity with a cytokine-independent pattern, implying that this mutation increases the sensitivity of myeloid or erythroid progenitors to hematopoietic growth factors. More importantly, we observed that the CHST15 mutation might induce HEL cell differentiation toward myeloid, monocytic and megakaryocytic lineages, which mimicked the bone marrow morphologic characterization ofPMF or ET, showing an enhancing effect of CHST15 mutation on MPN development (Fig. 7). Notably, when additional epigenetic events were detected during follow-up, 3 patients with PMF were found to have mutations in IDH1,
EZH2, ASXL1, TET2 and,TP53 mutation. Consistent with these changes, in the 3 patients with coexisting germline and somatic CHST15 mutations, the disease converted to acute myeloid leukemia or accelerated PMF, illustrating that CHST15 mutation can enhance the transformation potential of PMF.
Familial segregation of hematological malignancies supports the role of inherited factors in disease etiology [20, 21]. Direct evidence for a predisposition to MPNs is provided by the increased risk related to MPNs [11]. The Sud A group reported that first-degree relatives ofthe majority of patients with hematological malignancies exhibited increased familial relative risks(FRRs) for the same tumor type; the FRRs for MPN were >4.0, suggesting an inter relationship between FRRs and MPNs [22]. In our patients, CHST15 mutation occurred with low frequencyin the same family member and was present in both germline and somatic cells, suggesting that CHST15 germline mutation may be a founder lesion and is not accidental but instead is substantially interconnected. At the population level, a number of germline predisposition alleles have been identified for MPN, including rs2736100 in the TERT gene [8, 9], the JAK2 46/1haplotype [13, 14], andRBBP6 germline mutation [12]. However, these data mainly came from Caucasian populations, and the universality of the mutations still remains to be evaluated, especially in Chinese populations. In the present study, we identified the c.1367delG, p.Arg456fsmutation in the CHST15 gene as a predisposing genefor familial MPN. This conclusion was based on the following evidence: (i) the mutation is not found in the Exome Aggregation Consortium (ExAC) database (0/60, 706), indicating that it is very rare; (ii) there were no CHST15 mutations in 110 patients with sporadic MPN and 160 healthy subjects from the same geographicalarea, excluding the possibility of polymorphism; and (iii) the previous generation (family 3, ET) and the subsequent generation (all three families) of the probands lacked the CHST15 mutation (a total of 8 unaffected individuals), indicating that CHST15 variant doesn’t follow a atavistic heredity models at multigenerational pedigree levels, and may be a de novo mutation.
Carbohydrate sulfotransferase 15 (CHST15) is a type II transmembrane glycoprotein that acts as a sulfotransferase and participates in chondroitin sulfate E (CS-E) biosynthesis [23]. CS-E plays a pivotal role in tumor progression [24] and tissue fibrosis formation [25, 26]. KatagiriBM T et al. assessed the effects of CS on hematopoiesis using a CS-reduced mouse model, in which a gene encoding the CS-synthesizing enzyme, CS N-acetylgalactosaminyltransferase-1 (CSGalNAcT1) was desrupted (T1KO), and BM levels of CS disaccharides in T1KO mice (930 pmol/mg acetone powder) were approximately two-thirds of those in WT mice (1400 pmol/mg acetone powder) while the expression level of CSGalNAcT1 in BM LSK cells (RT-qPCR) was very high, suggesting that immature hematopoietic cells are richer in CS disaccharides than mature ones. The hematopoietic stem and progenitor cells (HSPCs) from T1KO mice showed significantly impaired repopulation in WT recipient mice on serial transplantation., suggesting that CS is also important for HSC self-renewal, differentiation and homeostasis maintance in BM [27, 28]. Based on the impact of CSGalNAcT1 gene defect on hematopoietic, we speculate that CHST15 gene mutation might be involved in an insufficient CS-E synthesis, and participated in the abnormal hematopoietic in familial MPNs.
In addition, overexpression of CHST15 may account for the prognosis of pancreatic cancer [29], invasive activity of breast cancer cells [30] and enhanced proliferation and sensitization to apoptosis of esophageal squamous cell carcinoma cells [31], suggesting the possibility that CHST15 is a functional oncogene. Our results showed that familial MPN exhibited downregulated expression of both CHST15 mRNA and CHST15 protein. These characteristics suggest that the CHST15 mutation endows MPN cells with increased proliferative activity and differentiation potential.
Coimmunoprecipitation experiment results indicated that CHST15 may interact with JAK2 both in HEL cells and in PBMNCs from familial MPN. The interaction was also confirmed by acquisition of immunofluorescence images, revealing for the first time that the physical interaction of CHST15 with JAK2 occurs in MPN cells, and suggested that a regulatory signaling axis, the CHST15/JAK2/p-Stat3 axis, is involved in the pathogenesis of familial MPN.
To gain deeper insight into the molecular mechanisms and signaling pathways of CHST15 mutation in familial MPN, gene expression profiling was performed. The results showed that CHST15-mutant cells had significant overexpression of the FREM1,IFI27 and C4B_2 genesand downregulated AOC1 gene expression. These genes are mainly involved in the control of the inflammatory response, extracellular matrix formation and immune regulation,which contribute to a regulatory network supporting the generation of the inflammatory bone marrow microenvironment in PMF [32, 33]. An alternatively spliced FREM1 transcript variant, named Toll-like/interleukin-1 receptor regulator (TILRR), is a coreceptor for members of the interleukin 1 receptor family. TILRR signaling contributes to the control of inflammation and amplifies IL-1-induced activation of NF-κB [34]. The IFI27 gene is related to innate immune and interferon gamma signaling. In sporadic PMF patients, IFI27 was overexpressed, reflecting the facilitation of PMF activity and enhancement of the tumor burden [35]. Although the IFI27 gene was overexpressed in familial PMF, our coimmunoprecipitation did not confirm a direct interaction between CHST15 and IFI27, suggesting both might exist in a signaling crosstalk. Complement signaling can influence both innate and adaptive immunity [36, 37], and both are involved in the development of inflammation-induced immune injury and stromareconstruction. We demonstrated that the C4B_2 gene exhibited upregulated expression in familial PMF, implying thatC4B_2 may participate inthe development of local inflammatory lesions and the formation of extracellular matrix. AOC1 may catalyze the degradation of putrescine and histamine. Polyaminesand their diamine precursor putrescine perform pivotal functions in cell growth. Kirschner et al. suggest that Aoc1gene expression contributes to the homeostasis of polyaminelevels in embryonic kidneys. Downregulation of AOC1 is predicted to disturb the delicate balance of growth promotion and differentiation signals, thereby favoring a proliferative phenotype [38]. When the mRNA expression profiles of all six familial MPN pateints were integrated and hierarchical clustering analysis was performed, only two differentially expressed genes (AOC1 and NPDC1) were identified. The NPDC1 gene is able to suppress oncogenic transformation in neural and nonneural cells and overexpressed in intraductal papillary mucinous neoplasms of the pancreas [39] and soft tissue sarcoma [40]. Our patients exhibited upregulated NPDC1 expression, suggesting the existence of signaling communication between CHST15 and NPDC1. When differentially expressed genes and proteins were integrated, we generated a signaling network related to the regulation of cell proliferation, differentiation, extracellular matrix formation and inflammatory responses associated with CHST15 mutation in familial MPN, which was conducive to our understanding of the molecular mechanism of CHST15 mutation-driven MPN.
In summary, analysis of three families with the same geographical origin identified a mutant locus in CHST15 that is associated with the development of familial MPN. Further insights into the underlying mechanism of CHST15 mutation-related MPN may lead to not only the identification of novel biomarkers but also the development of new therapeutic targets for MPN.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary materials.
References
Rumi E, Passamonti F, Della Porta MG, Elena C, Arcaini L, Vanelli L, et al. Familial chronic myeloproliferative disorders: clinical phenotype and evidence of disease anticipation. J Clin Oncol. 2007;25:5630–5.
Bellanne-Chantelot C, Chaumarel I, Labopin M, Bellanger F, Barbu V, De Toma C, et al. Genetic and clinical implications of the Val617Phe JAK2 mutation in 72 families with myeloproliferative disorders. Blood. 2006;108:346–52.
Rumi E, Harutyunyan AS, Pietra D, Milosevic JD, Casetti IC, Bellini M, et al. CALR exon 9 mutations are somatically acquired events in familial cases of essential thrombocythemia or primary myelofibrosis. Blood. 2014;123:2416–9.
Harutyunyan AS, Kralovics R. Role of germline genetic factors in MPN pathogenesis. Hematol Oncol Clin North Am. 2012;26:1037–51.
Lundberg P, Nienhold R, Ambrosetti A, Cervantes F, Perez-Encinas MM, Skoda RC. Somatic mutations in calreticulin can be found in pedigrees with familial predisposition to myeloproliferative neoplasms. Blood. 2014;123:2744–5.
Shen XH, Sun NN, Yin YF, Liu SF, Liu XL, Peng HL, et al. A TET2 rs3733609 C/T genotype is associated with predisposition to the myeloproliferative neoplasms harboring JAK2(V617F) and confers a proliferative potential on erythroid lineages. Oncotarget. 2016;7:9550–60.
Olcaydu D, Rumi E, Harutyunyan A, Passamonti F, Pietra D, Pascutto C, et al. The role of the JAK2 GGCC haplotype and the TET2 gene in familial myeloproliferative neoplasms. Haematologica. 2011;96:367–74.
Oddsson A, Kristinsson SY, Helgason H, Gudbjartsson DF, Masson G, Sigurdsson A, et al. The germline sequence variant rs2736100_C in TERT associates with myeloproliferative neoplasms. Leukemia. 2014;28:1371–4.
Jager R, Harutyunyan AS, Rumi E, Pietra D, Berg T, Olcaydu D, et al. Common germline variation at the TERT locus contributes to familial clustering of myeloproliferative neoplasms. Am J Hematol. 2014;89:1107–10.
Saliba J, Saint-Martin C, Di Stefano A, Lenglet G, Marty C, Keren B, et al. Germline duplication of ATG2B and GSKIP predisposes to familial myeloid malignancies. Nat Genet. 2015;47:1131–40.
Tapper W, Jones AV, Kralovics R, Harutyunyan AS, Zoi K, Leung W, et al. Genetic variation at MECOM, TERT, JAK2 and HBS1L-MYB predisposes to myeloproliferative neoplasms. Nat Commun. 2015;6:6691.
Harutyunyan AS, Giambruno R, Krendl C, Stukalov A, Klampfl T, Berg T, et al. Germline RBBP6 mutations in familial myeloproliferative neoplasms. Blood. 2016;127:362–5.
Olcaydu D, Harutyunyan A, Jager R, Berg T, Gisslinger B, Pabinger I, et al. A common JAK2 haplotype confers susceptibility to myeloproliferative neoplasms. Nat Genet. 2009;41:450–4.
Jones AV, Chase A, Silver RT, Oscier D, Zoi K, Wang YL, et al. JAK2 haplotype is a major risk factor for the development of myeloproliferative neoplasms. Nat Genet. 2009;41:446–9.
Tefferi A, Thiele J, Orazi A, Kvasnicka HM, Barbui T, Hanson CA, et al. Proposals and rationale for revision of the World Health Organization diagnostic criteria for polycythemia vera, essential thrombocythemia, and primary myelofibrosis: recommendations from an ad hoc international expert panel. Blood. 2007;110:1092–7.
Peng HL, Zhang Y, Sun NN, Yin YF, Wang YW, Cheng Z, et al. A gain-of-function mutation in TNFRSF13B is a candidate for predisposition to familial or sporadic immune thrombocytopenia. J Thromb Haemost. 2017;15:2259–69.
Klampfl T, Gisslinger H, Harutyunyan AS, Nivarthi H, Rumi E, Milosevic JD, et al. Somatic mutations of calreticulin in myeloproliferative neoplasms. N. Engl J Med. 2013;369:2379–90.
Antonioli E, Guglielmelli P, Poli G, Bogani C, Pancrazzi A, Longo G, et al. Influence of JAK2V617F allele burden on phenotype in essential thrombocythemia. Haematologica. 2008;93:41–48.
Sykes DB, Kfoury YS, Mercier FE, Wawer MJ, Law JM, Haynes MK, et al. Inhibition of dihydroorotate dehydrogenase overcomes differentiation blockade in acute myeloid leukemia. Cell. 2016;167:171–86. e115
Fallah M, Kharazmi E, Pukkala E, Tretli S, Olsen JH, Tryggvadottir L, et al. Familial risk of non-Hodgkin lymphoma by sex, relationship, age at diagnosis and histology: a joint study from five Nordic countries. Leukemia. 2016;30:373–8.
Sud A, Chattopadhyay S, Thomsen H, Sundquist K, Sundquist J, Houlston RS, et al. Familial risks of acute myeloid leukemia, myelodysplastic syndromes, and myeloproliferative neoplasms. Blood. 2018;132:973–6.
Sud A, Chattopadhyay S, Thomsen H, Sundquist K, Sundquist J, Houlston RS, et al. Analysis of 153 115 patients with hematological malignancies refines the spectrum of familial risk. Blood. 2019;134:960–9.
Ohtake S, Ito Y, Fukuta M, Habuchi O. Human N-acetylgalactosamine 4-sulfate 6-O-sulfotransferase cDNA is related to human B cell recombination activating gene-associated gene. J Biol Chem. 2001;276:43894–900.
Takakura K, Shibazaki Y, Yoneyama H, Fujii M, Hashiguchi T, Ito Z, et al. Inhibition of cell proliferation and growth of pancreatic cancer by silencing of carbohydrate sulfotransferase 15 in vitro and in a Xenograft Model. PLoS ONE. 2015;10:e0142981.
Suzuki K, Arumugam S, Yokoyama J, Kawauchi Y, Honda Y, Sato H, et al. Pivotal role of carbohydrate sulfotransferase 15 in fibrosis and mucosal healing in mouse colitis. PLoS ONE. 2016;11:e0158967.
Kai Y, Tomoda K, Yoneyama H, Kitabatake M, Nakamura A, Ito T, et al. Silencing of carbohydrate sulfotransferase 15 hinders murine pulmonary fibrosis development. Mol Ther Nucleic Acids. 2017;6:163–72.
Katagiri T, Shun Uemura S, Ushiki T, Yaeko NT, Motohiko O, Tadahisa M, et al. Distinct effects of chondroitin sulfate on hematopoietic cells and the stromal microenvironment in bone marrow hematopoiesis. Exp Hematol. 2021;96:52–62.
Gasimli L, Hickey AM, Yang B, Guoyun L, Mitche dela R, Alison VN, et al. Changes in glycosaminoglycan structure on differentiation of human embryonic stem cells towards mesoderm and endoderm lineages. Biochim Biophys Acta. 2014;1840:1993–2003.
Ito Z, Takakura K, Suka M, Kanai T, Saito R, Fujioka S, et al. Prognostic impact of carbohydrate sulfotransferase 15 in patients with pancreatic ductal adenocarcinoma. Oncol Lett. 2017;13:4799–805.
Liu LC, Wang YL, Lin PL, Zhang X, Cheng WC, Liu SH, et al. Long noncoding RNA HOTAIR promotes invasion of breast cancer cells through chondroitin sulfotransferase CHST15. Int J Cancer. 2019;145:2478–87.
Wang X, Cheng G, Zhang T, Deng L, Xu K, Xu X, et al. CHST15 promotes the proliferation of TE1 cells via multiple pathways in esophageal cancer. Oncol Rep. 2020;43:75–86.
Kramann R, Schneider RK. The identification of fibrosis-driving myofibroblast precursors reveals new therapeutic avenues in myelofibrosis. Blood. 2018;131:2111–9.
Schepers K, Pietras EM, Reynaud D, Flach J, Binnewies M, Garg T, et al. Myeloproliferative neoplasia remodels the endosteal bone marrow niche into a self-reinforcing leukemic niche. Cell Stem Cell. 2013;13:285–99.
Zhang X, Pino GM, Shephard F, Kiss-Toth E, Qwarnstrom EE. Distinct control of MyD88 adapter-dependent and Akt kinase-regulated responses by the interleukin (IL)-1RI co-receptor, TILRR. J Biol Chem. 2012;287:12348–52.
Skov V, Larsen TS, Thomassen M, Riley CH, Jensen MK, Bjerrum OW, et al. Whole-blood transcriptional profiling of interferon-inducible genes identifies highly upregulated IFI27 in primary myelofibrosis. Eur J Haematol. 2011;87:54–60.
Dunkelberger JR, Song WC. Role and mechanism of action of complement in regulating T cell immunity. Mol Immunol. 2010;47:2176–86.
Ricklin D, Hajishengallis G, Yang K, Lambris JD. Complement: a key system for immune surveillance and homeostasis. Nat Immunol. 2010;11:785–97.
Kirschner KM, Braun JF, Jacobi CL, Rudigier LJ, Persson AB, Scholz H. Amine oxidase copper-containing 1 (AOC1) is a downstream target gene of the Wilms tumor protein, WT1, during kidney development. J Biol Chem. 2014;289:24452–62.
Sato N, Fukushima N, Maitra A, Iacobuzio-Donahue CA, van Heek NT, Cameron JL, et al. Gene expression profiling identifies genes associated with invasive intraductal papillary mucinous neoplasms of the pancreas. Am J Pathol. 2004;164:903–14.
Francis P, Namlos HM, Muller C, Eden P, Fernebro J, Berner JM, et al. Diagnostic and prognostic gene expression signatures in 177 soft tissue sarcomas: hypoxia-induced transcription profile signifies metastatic potential. BMC Genomics. 2007;8:73.
Acknowledgements
The authors would like to thank the patients and their familial members for participation and coordination in this study.
Funding
This work was supported in part by the National Natural Science Foundation of China (No. 81470323 and No. 81500171); the Natural Science Foundation of Hunan Province (2019JJ40449); and the Famous Clinical Doctors Program in Xiang-Ya Medical College of Central South University (2012–2014).
Author information
Authors and Affiliations
Contributions
GSZ diagnosed and treated the patients, designed the study, and composed the paper. YC, YZ, and ZC performed main experiments. YWW, WZY, YJL, NNS, SSZ, SFL, and XX performed partly experiments. ZHW, HLP, YXX, and GYH helped with clinic sample collection and case-management. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics statement
Patient samples were collected after informed written consent was obtained in accordance with the Declaration of Helsinki. This study was approved by the institutional ethics committee of The Second Xiang-Ya Hospital, Central South University.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Edited by Boris Zhivotovsky
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Chen, Y., Zhang, Y., Wang, Z. et al. CHST15 gene germline mutation is associated with the development of familial myeloproliferative neoplasms and higher transformation risk. Cell Death Dis 13, 586 (2022). https://doi.org/10.1038/s41419-022-05035-w
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41419-022-05035-w