Abstract
Background
Increasing data indicate that HER2-positive (HER2 + ) breast cancer (BC) subtypes exhibit differential responses to targeted anti-HER2 therapy. This study aims to investigate these differences and the potential underlying molecular mechanisms.
Methods
A large cohort of BC patients (n = 7390) was utilised. The clinicopathological characteristics and differential gene expression (DGE) of HER2+ immunohistochemical (IHC) subtypes, specifically HER2 IHC 3+ and IHC 2 + /Amplified, were assessed and correlated with pathological complete response (pCR) and survival in the neoadjuvant and adjuvant settings, respectively. The role of oestrogen receptor (ER) status was also investigated.
Results
Compared to HER2 IHC 3+ tumours, BC patients with IHC 2 + /Amplified showed a significantly lower pCR rate (22% versus 57%, P < 0.001), shorter survival regardless of HER2 gene copy number, were less classified as HER2 enriched, and enriched for trastuzumab resistance and ER signalling pathway genes. ER positivity significantly decreased response to anti-HER2 therapy in IHC 2 + /Amplified, but not in IHC 3 + BC patients.
Conclusion
In HER2 + BC, overexpression of HER2 protein is the driver of the oncogenic pathway, and it is the main predictor of response to anti-HER2 therapy. ER signalling pathways are more dominant in BC with equivocal HER2 expression. personalised anti-HER2 therapy based on IHC classes should be considered.

Similar content being viewed by others
Introduction
Human epidermal growth factor receptor 2 positive (HER2 + ) breast cancer (BC) accounts for 13–15% of BC [1]. HER2 positivity is defined either by protein overexpression as defined by immunohistochemical score (IHC) 3+ or equivocal protein expression (IHC 2 + ), with evidence of HER2 gene amplification (defined here as IHC 2 + /Amplified) [1,2,3,4]. To date, BCs with HER2 IHC 3+ or IHC 2 + /Amplified are equally considered candidates for anti-HER2 therapy [5]. However, the response rate in HER2 + BC patients is not uniform, and predictors of response are variables and complex, including protein expression level, HER2 gene copy number level and others [6,7,8].
A meta-analysis of response rates to neoadjuvant therapy showed that the pathologic complete response (pCR) in HER2 + BC was 46% when targeted anti-HER2 therapy (trastuzumab) was used, compared to 25% in the chemotherapy alone group [9]. In the latter group, the pCR rates varied from 16 to 33% within the hormone receptor (HR) positive and negative groups, respectively [9]. Other studies have confirmed these findings [10, 11], and have also shown substantial variability in the response rate among HER2 + BC patients treated with the same anti-HER2 therapies. This variability raises a concern about whether HER2 protein overexpression or HER2 gene amplification is the key driver of response. Some studies have shown that pCR rates are significantly higher in HER2 IHC 3 + BC patients compared to those with IHC 2 + /Amplified [12,13,14,15,16,17]. Furthermore, patients with HER2 IHC 3+ were reported to have longer survival than those with IHC 2 + /Amplified, when treated with anti-HER2 therapy [18]. In studies comparing the response rate in relation to HER2 gene amplification levels, some studies have indicated that the therapeutic response to anti-HER2 therapy correlates with the level of HER2 gene amplification [19,20,21,22,23]. However, no association between HER2 gene copy number and survival was identified [11, 23,24,25]. In the NeoALTTO Phase III clinical trial, a significant association between HER2 gene copy number and pCR was reported [26], but the effect of HER2 gene amplification status ceased to have predictive value when HER2 protein expression level was considered [26]. Within the HER2 IHC 2 + /Amplified class, Dowsett et al. [27] found no association between HER2 gene copy number or HER2/CEP17 ratio and outcome.
The crosstalk between the oestrogen receptor (ER) and HER2 signalling has also attracted a great deal of attention and has been studied in several clinical trials [7, 8, 11, 28, 29]. Both HER2 and ER drive BC proliferation by a complex network of molecular signalling processes [30]. The complexity of response to anti-HER2 therapy varies among the different ER expression groups, as reported in the literature. ER-negative (ER-)/HER2+ tumours have shown higher response rates compared to ER + /HER2- tumours [9]. However, some studies suggest that ER+ tumours also exhibit a good response to anti-HER2-targeted therapy [30, 31]. On the other hand, some studies found no relationship between ER status and response to anti-HER2 therapy [12]. Furthermore, the impact of ER status on the response to anti-HER2 therapy within each HER2 + IHC class has not been fully addressed.
In this study, we hypothesised that the level of HER2 protein expression, rather than HER2 gene amplification level, is the key determinant in predicting response to anti-HER2 therapy. We aimed to decipher the clinical, biological, and molecular signatures of HER2 + IHC classes of BC with a particular emphasis on the difference in pCR and outcome as well as the role of ER expression within these two categories.
Materials and methods
Study cohort
A total of 10,139 invasive BC cases were initially included in this study and comprise multiple large cohorts:
-
The first cohort comprised Nottingham University Hospitals (NUH) BC patients (n = 7485).
-
The second cohort was available from the publicly available BC datasets (PABCD) including The Cancer Genome Atlas (TCGA, https://identifiers.org/cbioportal:brcatcga) BC cohort (n = 855), a subset of the Molecular Taxonomy of BC International Consortium (METABRIC, https://identifiers.org/cbioportal:brca_metabric) (n = 289) and Gene Expression Omnibus (GEO, https://www.ncbi.nlm.nih.gov/gds) (n = 136). NUH, TCGA and METABRIC had available clinicopathological data, including age at diagnosis, tumour size, histological tumour grade, axillary lymph node (LN) status, histologic tumour type, lymphovascular invasion (LVI), Nottingham prognostic index (NPI), HER2 IHC scores (0–3), HER2 gene amplification, HR status (including ER and progesterone receptors (PR) in addition to long term follow up data. Data about treatment regimens (chemotherapy and anti-HER2) in the adjuvant settings were available from the NUH cohort, while intrinsic molecular subtypes were available through the PAM50 classification and integrative cluster subtypes in TCGA and METABRIC cohorts, respectively.
-
The third cohort was derived from the previously published multicentre (MC) study of HER2 + BC patients [6] (n = 1374). From that cohort, data about neoadjuvant therapy, pCR, HER2 IHC scores, HER2 gene amplification, HER2/CEP17 ratio, HR status, histologic tumour grade on the core biopsy and histologic tumour type were available. That cohort was enriched for HER2 IHC 2 + /Amplified cases to assess the differential response between both HER2+ categories in the neoadjuvant settings.
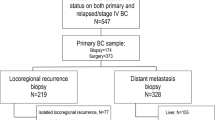
Cases without HER2 IHC score and/or gene amplification status were excluded, and the final number of cases enrolled in this study was 7390 patients, of which 1052 received neoadjuvant therapy and 751 had data on pCR (Fig. 1). In addition, data from six studies with differential response of HER2 + BC patients to therapy [12,13,14,15,16, 32] were considered in this study and the average response of HER2+ classes to anti-HER2 therapy was calculated (Supplementary Table 1A).
HER2 staining was completed on the Ventana Benchmark ULTRA immunohistochemistry automated staining system using the Ventana PATHWAY anti-HER-2/neu (4B5) rabbit monoclonal ready-to-use primary antibody in combination with Ventana detection kits. ER IHC staining was carried out following a standard protocol, the 4-µm sections were prepared, and slides were processed through pre-diluted Tris-based buffer with a basic pH (Roche, Ventana) for 64 min at 95 °C for antigen retrieval, an anti ER rabbit monoclonal antibody SP1 clone (Roche) was applied and incubated for 16 min. ER and PR positivity were assessed according to ASCO/CAP guidelines if ≥1% of the invasive tumour cell nuclei are immunoreactive [33]. HER2 IHC was scored in all included cohorts as positive (IHC 3 + ), equivocal (score 2 + ) or negative (score 1 + /0). IHC score 2+ patients were tested for HER2 gene amplification by fluorescence in situ hybridisation (FISH) or chromogenic in situ hybridisation (CISH) [2, 5]. HER2 cases with equivocal protein expression were considered positive if HER2 gene copy number was ≥6.0 and/or HER2/CEP17 ratio was ≥2.0 [5]. HER2-negative BC cases defined as HER2 IHC score 2 + /non-amplified and those with IHC scores 1+ and 0 were used as control groups. The sample size for this study was determined based on a power analysis, considering the primary research objectives, desired effect size, statistical significance level (0.05), power level of 0.95 and expected variability in the data and to ensure robust and reliable statistical analysis and meaningful interpretation of the study findings.
Correlation between HER2 classes and response to therapy in the neoadjuvant settings
The response to neoadjuvant therapy was evaluated. pCR was defined as no residual invasive carcinoma in both breast and axillary lymph nodes regardless of the presence of residual ductal carcinoma in situ (DCIS) (ypT0/is ypN0) [14]. Differences in pathologic response were evaluated according to HER2 protein expression level, HER2 gene amplification level, ER status and whether patients received anti-HER2 targeted therapy with the neoadjuvant chemotherapy (NACT). To investigate the impact of the levels of HER2 gene amplification on the pathologic response in tumours with equivocal protein expression, cases were stratified into; low (HER2 gene copy number ≥6.0 to <9.0, and/or HER2/CEP17 ratio ≥2.0 to <4.0) [5] and high (HER2 gene copy number ≥9.0 and or HER2/CEP17 ratio ≥4.0) amplification status. These cut-offs were based on the median of HER2 gene copy number or HER2/CEP17 ratio within the HER2 IHC 3+ group, which was used as a benchmark for gene amplification level in this study.
Correlation between HER2 + BC classes and patients’ outcome in the adjuvant settings
The correlation between HER2 + BC classes and the outcome was assessed in the combined NUH, TCGA and METABRIC cohorts in BC patients who received adjuvant anti-HER2 therapy using BC-specific survival (BCSS), defined as the time from the initial diagnosis to the time of BC-related death, and distant metastasis-free survival (DMFS) defined as the time from surgery to development of distant metastasis.
Differential gene expression (DGE) analysis
The molecular characteristics of both HER2+ classes were analysed using gene set enrichment (GSEA) and pathway analysis to understand the related mechanisms of differential response to therapy. For that, the PABCD cohort was used.
RNA-seq counts were obtained from the TCGA-BRCA RNAseqV2 dataset [34]. We also accessed the METABRIC cohort on cBioPortal website [35, 36] for gene expression and clinical data. Five independent gene expression datasets (GSE136300, GSE55005, GSE161420, GSE121105 and GSE60182), were downloaded from the GEO database and exploited as discovery cohorts to identify DEGs involved in HER2 signalling pathway, trastuzumab response and resistance. Briefly, raw reads were obtained from NCBI-GEO, adaptors removed, and low-quality reads (phred <30) were removed using TrimGalore, with resultant reads aligned to the GRCh38 version of the human reference genome using STAR, and gene expression was quantified using FeatureCounts. Detailed information on datasets is listed in (Supplementary Table 2). The DESeq2 tool in R software (version 3.4.3; https://cran.r-project.org/) was used for differential analysis of gene expression using matrices defining trastuzumab treatment in both drug-sensitive and drug-resistant samples, as well as between HER2 siRNA knockdown and control groups. The significantly differentiated expressed genes were defined as log2 fold change (≥±1) and false discovery rate (FDR) < 0.05 between high and low score groups and common DEGs between conditions were identified using Venn diagrams. The web-based gene set enrichment analysis tool (WebGestalt) [37] was used to explore significantly enriched pathways based on the identified DEGs in IHC 2 + /Amplified samples. ER related genes from the Reactome pathway website reactome.org, were identified within the DEG among HER2+ classes. Detailed methodology is mentioned in Supplementary Materials 1.
Statistical analysis
Statistical package of social science (IBM-SPSS) statistical software v. 27.0 (SPSS, Chicago, IL, USA) was used to carry out the statistical analysis. Correlations between HER2 IHC scores, pCR and clinicopathologic parameters were analysed using Chi-square (χ2) test, Fisher’s exact test, Kruskal–Wallis where appropriate. Univariate and multivariable logistic regression analyses were performed to investigate the association of each variable with pCR and the effect of other confounders. Odds ratios (ORs) and 95% CIs were calculated for each variable. Outcome analysis was assessed using Kaplan–Meier curves and the log-rank test. The difference between gene expression among two groups was calculated through t test or ANOVA using GraphPad software. For all analyses, a P value of <0.05 (two-tailed) was considered statistically significant.
Results
Table 1 summarises the demographic and pathological characteristics of the included cohorts. In the whole cohort, the median value of HER2 gene copy number was 2.0 (range 0.8–440) and HER2/CEP17 ratio was 1.5 (range 0.42–32). When HER2 + BC was stratified based on IHC classes, in the HER2 IHC 3 + , the median HER2 gene copy number was 9.0 (range 2–440) and the median HER2/CEP17 ratio was 4.0. In HER2 IHC 2 + /Amplified, the median HER2 gene copy number was 4.4 (range 1.7–370) and HER2/CEP17 ratio was 2.3, respectively. Eighty percent of HER2 IHC 2+ were ER-positive compared to 60% in HER2 IHC 3 + .
There was a significant correlation between HER2 IHC 3+ and features characteristic of aggressive tumour behaviour, including larger tumour size, higher tumour grade, high NPI risk group, positive LN status and ER and PR negativity (P < 0.001). These associations were maintained when IHC 3+ tumours were compared to IHC 2 + /Amplified BC (Table 2).
HER2 IHC 3+ tumours showed significant association with HER2 enriched (HER2-E) molecular subtype as compared to 2 + /Amplified (64% versus 25% respectively; P < 0.001). Contrasting this, when HER2 gene copy number or HER2/CEP17 ratio were considered, no correlation with HER2-E molecular subtype was detected (Supplementary Fig. 1). Moreover, when HER2 IHC 2+ with high HER2 gene amplification level (≥9.0 copies) is compared to HER2 IHC 3 + , HER2-E molecular subtypes and HR negativity continue to exhibit a statistically significant association with the HER2 IHC 3+ category (P = 0.01, P = 0.03 and P = 0.008 for ER and PR, respectively).
Differential response of HER2+ classes to therapy in the neoadjuvant setting
Overall, the pCR rate in the whole neoadjuvant BC cohort was 26%, while in HER2+ tumours it was 36%. When stratified based on HER2 classes, HER2 IHC 3+ tumours had significantly higher pCR than IHC 2 + /Amplified (57% vs 22%) (P < 0.001). In the whole HER2+ tumour cohort, no significant difference in pCR rates between BC patients with low (< 9.0) and high (≥ 9.0) HER2 gene copy number levels was identified (P = 0.13). The same was found for patients with HER2/CEP17 ratios ≥2.0 to <4.0 or ≥4.0. Moreover, patients with HER2 IHC 2+ tumours and high HER2 gene amplification level had lower pCR rate when compared with all HER2 IHC 3+ tumours regardless of their gene amplification levels (17% vs 57%, P = 0.001). Considering the whole spectrum of HER2 expression, there was a significant positive association between pCR and HER2/CEP17 ratio (P = 0.0.03), however, significance was lost within patients with IHC 2 + /Amplified tumours (P = 0.5). Supplementary Fig. 2A summarises pCR at different HER gene copy number amplification levels scenarios).
The average pCR from the current study and previously published reports [12,13,14,15,16, 32] was 46% with an average of 56 and 23% in HER2 IHC 3+ and IHC 2 + /Amplified, respectively (Supplementary Table 1A).
ER+ tumours were significantly associated with a lower rate of pCR among HER2+ patients (33% with pCR vs 67% with no response). Within HER2 IHC 3 + BC patients, there was no statistically significant association between ER status and pCR rates, unlike BC patients with HER2 IHC 2 + /Amplified where negative ER status were significantly associated with increased pCR rates (P < 0.001) (Supplementary Fig. 2B and Supplementary Table 3).
Among IHC 2 + /Amplified tumours, the pCR following NACT alone was 13% compared to 39% for HER2 IHC 3+ tumours. Following anti-HER2 therapy the pCR in HER2 IHC 3+ patients was augmented (57%) compared to 21% in IHC 2 + /Amplified patients (Supplementary Fig. 2B).
Multivariate logistic regression model for factors affecting pathologic response among BC patients with over and equivocal HER2 protein expression revealed that HER2 IHC 3+ is an independent predictor of pCR over HER2 gene amplification level; (OR, 18.00; 95%CI, 89.07–2.66; P = 0.004). Also, histologic tumour grade and ER status were an independent predictor of pCR (OR, 3.12; 95% CI, 1.60–6.00; P = 0.001), (OR, 0.35; 95%CI, 0.18–0.67; P = 0.001, for grade 3 and ER+ tumours, respectively) (Fig. 2).
HER2+ groups and patients’ survival
In the non-treated (anti-HER2 therapy-naive) patients, HER2 IHC 3 + BC patients had significantly shorter BCSS (mean value 84 months) compared to patients with IHC 2 + /Amplified tumours (mean value 119 months), (P = 0.01). Following anti-HER2 therapy, the mean BCSS of HER2 IHC 3+ increased to 110 months close to IHC 2 + /Amplified patients (P = 0.23) (Supplementary Fig. 3).
Among HER2 3 + BC patients, administration of adjuvant anti-HER2 in addition to chemotherapy significantly increased 10-year survival (P < 0.001 and P = 0.006, for BCSS and DMFS, respectively). However, in patients with HER2 IHC 2 + /Amplified tumours, no significant difference in survival was observed (P = 0.08 and P = 0.14, respectively) (Fig. 3).
When cases were stratified based on ER expression, patients with ER- and HER2 IHC 2 + /Amplified BC showed improved outcome upon treatment with anti-HER2 therapy (BCSS P = 0.02). However, no similar improvement in the outcome was observed in the ER + HER2 IHC 2 + /Amplified BC patients’ group after receiving of anti-HER2 therapy (BCSS P = 0.47) (Fig. 3). Contrasting this, IHC 3 + BC patients the association between longer survival and anti-HER2 therapy was observed in both ER- and ER+ groups (BCSS P < 0.001 and P = 0.005, for ER- and ER + , respectively). Supplementary Table 1B summarises data about the differential response of HER2+ patients to anti-HER2 therapy in the adjuvant settings from previously published reports.
Molecular profile of HER2+ classes and its impact on response to therapy
We next performed an analysis to identify genes responsible for HER2 oncogenic signalling pathway and response to trastuzumab therapy among the 2 HER2 IHC classes (HER2 IHC 3+ and 2 + /Amplified) as well as in the 2 + /non-amplified tumours. HER2 oncogenic signalling pathway genes were significantly enriched in HER2 IHC 3+ compared to HER2 2 + /Amplified (Fig. 4 and Supplementary Tables 4 and 5). However, the differential expression of these genes was not as significant between the two classes of equivocal HER2 protein expression (2 + /Amplified and 2 + /non-amplified).
a The row data was extracted from GEO dataset and the bioinformatics analysis was carried out to identify genes responsible for the HER2 oncogenic pathway and response to therapy. b The mean values of the normalised reads of HER2 signalling genes were significantly enriched in HER2 IHC 3+ tumours compared to HER2 IHC 2+ tumours regardless of the amplification status. c, d Unsupervised clustering analysis and heatmap illustrating the expression of HER2 oncogenic pathway genes among HER2+ classes.
Differential analysis of genes responsible for resistance to trastuzumab therapy between HER2 IHC 3+ and 2 + /Amplified groups revealed 82 genes; of them, 50 genes were significantly upregulated in IHC 2 + /Amplified (Supplementary Fig. 4). The predictive validity of those genes was tested through the online database; rocplot.org. Twelve genes were significantly associated with no pathologic response to anti-HER2 therapy in HER2 + BC (Supplementary Fig. 5 and Supplementary Table 6).
ER signalling pathway genes were significantly enriched in HER2 IHC 2 + /Amplified class compared to HER2 IHC 3+ (P = 0.008) (Fig. 5). Supplementary Table 7 summarises the mean values of ER signalling pathway genes between BC patients with over and equivocal protein expression. Further details are mentioned in Supplementary Materials 2.
a Heatmap demonstrating the unsupervised clustering and distribution of ER signalling genes among HER2 IHC 3+ and IHC 2 + /Amplified with significant expression in IHC 2 + /Amplified class (P = 0.008). b Principal component analysis (PCA) showing that most of ER-positive tumours are within the HER2 2 + /Amplified category. c A visual diagram delineates the significance of ER positivity in both HER2 + IHC categories. HER2 IHC 3+ predominantly hinges on the HER2 oncogenic signalling pathway, rendering the efficacy of anti-HER2 therapy contingent upon obstructing this pathway (depicted on the left side). Conversely, in HER2 IHC 2 + /Amplified tumours (depicted on the right side), the ER signalling pathway remains active. Here, cancer cells elude the suppressive effects of anti-HER2 interventions, sustaining their proliferation.
Discussion
The response of HER2 + BC patients to anti-HER2 therapy is variable [7, 9, 11, 38,39,40,41,42,43,44] and whether the protein expression or the gene amplification levels, when considered together, are the key driver remains to be confirmed. Although most anti-HER2 targeted therapy exerts their action on HER2 protein and no response is observed in IHC scores 0 or 1 + BC patients, there is high concordance between IHC and HER2 gene copy number [45] and no response is observed in ISH-negative cases. Moreover, there is an excellent correlation between HER2 IHC 3+ and high HER2 gene amplification level [46, 47], which may explain why most cases with high amplification levels respond well to anti-HER2 therapy. The main discrepancy is among HER2 IHC 2+ tumours, which typically show borderline gene amplification [1, 16, 45]. These results together with the finding that 4% of cases with HER2 IHC scores 0 and 1+ show evidence of gene amplification [45], argue against using ISH alone as a predictive of response to anti-HER2 therapy. In addition, the differential response based on interactions between IHC classes and ISH status and the molecular characteristics of these HER2 + IHC classes are not well-defined. In this study, we aimed to decipher the clinical, biological, and molecular mechanisms involved in anti-HER2 therapy response among these classes.
In the neoadjuvant setting, the overall pCR rate of HER2 + BC patients to NACT with anti-HER2 therapy in our study was 36%. However, when the cases were stratified based on the IHC classes, the pCR rate was significantly higher in HER2 IHC 3+ compared to HER2 IHC 2 + /Amplified BC patients. High HER2 gene amplification status was significantly associated with high pCR when all HER2 IHC categories were compared. However, when HER2 + IHC subgroups were considered, such association between HER2 gene amplification levels and pCR rate was lost. In the current study, HER2 protein overexpression (IHC 3 + ), was also an independent predictor of pCR, while different levels of HER2 gene amplification were not. These results are similar to the HERA and N9831 trials, which concluded that HER2/CEP17 ratio and HER2 gene copy number were not associated with patient outcome [25, 27, 48]. These results also are consistent with several previous studies, which demonstrated that HER2 protein overexpression is a strong predictor of response to anti-HER2 therapy [12,13,14,15,16, 18, 25, 32, 49]. Other studies have also indicated that the rate of pCR in the subset of patients with evidence of HER2 gene amplification in the absence of HER2 protein overexpression was significantly lower (17% vs 66%) [16, 32].
The stronger correlation between HER2 protein overexpression and response to anti-HER2 therapy is likely to reflect the fact that HER2 oncogenic pathways are driven by HER2 protein overexpression and not merely by HER2 gene copy number independent of the HER2 protein level as is the case in HER2 IHC 2 + /Amplified tumours. Therefore, the response of these patients with equivocal HER2 protein expression to therapies that target the HER2 oncogenic pathways is limited and the clinical response of these patients to chemotherapy combined with anti-HER2 therapies is not significantly different from that of HER2 IHC 2+ without evidence of HER2 gene amplification to chemotherapy alone.
Some studies have shown that the therapeutic response to anti-HER2 therapy is correlated with the level of HER2 gene amplification [19, 20, 22]. Singer an colleagues [22] evaluated the HER2/CEP17 ratio and response to therapy but they did not consider HER2 IHC protein expression in the analysis. Also, Arnold and colleagues [19] compared the response rate between cases with medium and high levels of gene amplification, yet only 1 case was HER2 IHC 2 + /Amplified, and the rest of the cases were IHC 3 + . Salmon et al. [18] demonstrated that trastuzumab efficacy of trastuzumab was consistently observed in both IHC and ISH HER2+ groups. However, in their study patients with HER2 protein overexpression experienced better survival than those with HER2 gene amplification but equivocal protein expression.
In the CLEOPATRA Phase III trial, HER2 IHC 3+ was associated with improved survival [49]. This is consistent with our study where patients with HER2 IHC 3+ benefited from adjuvant anti-HER2 therapy in terms of prolonged BCSS and DMFS compared to HER2 IHC 2 + /Amplified BC patients. Previous studies have demonstrated that the level of HER2 gene amplification is not a prognostic factor in patients with HER2 + BC treated with anti-HER2 therapy [24, 27]. The N9831 Phase III trial assessed disease-free survival of patients on adjuvant trastuzumab according to protein expression, HER2 gene copy number and HER2/CEP17 ratio. It reported that patients with normal HER2 protein-expressing tumours (0,1,2 + ) and ISH amplified had no improvement in survival with additional trastuzumab, while patients with IHC 3+ had a significant response to treatment [25].
Some authors have indicated that the level of HER2 protein expression in HER2+ tumours has no role in clinical management with anti-HER2 therapy [50]. However, that study was not based on a dichotomised classification (IHC 3+ versus 2 + ), but rather on a spectrum of HER2 staining. Other reports have suggested that the optimum strategy for choosing individuals for anti-HER2 therapy is to measure HER2 gene amplification by ISH testing [51, 52]. This was based on studies that included tumours with IHC scores of 3+ and 2+ and the ISH-negative group included only IHC 2+ tumours, resulting in an overemphasis of the value of ISH testing [51, 52].
Unlike conventional anti-HER2 therapies, which inhibit HER2 oncogenic pathways, HER2-based antibody-drug conjugates (ADCs) such as T-DM1 and DS-8201 mainly uses HER2 as a target to facilitate internalisation of the cytotoxic agent into HER2-expressing cells and their response is not proportional to the amount of HER2 protein [53]. The differential response of HER2+ tumours to T-DM1 was reported in Phase III KATHERINE trial of adjuvant T-DM1 versus Trastuzumab for residual invasive disease after neoadjuvant therapy for HER2 + BC. In the subgroups of patients defined by HER2 status, there was less pronounced treatment benefit in HER2 IHC 2+ compared to IHC 3+ in the trastuzumab arm, while in the T-DM1 arm, the 3-year invasive disease-free survival (IDFS) rate was not statistically significant between the two HER2+ classes (89% in the IHC 3+ subgroup and 85% in the IHC 2+ subgroup. Further supporting evidence in the same trial is that the IDFS of patients with heterogenous HER2 expression, mostly evident in HER2 IHC 2+ cases, was too close to homogenous expression, mostly in HER2 IHC 3+ in the T-DM1 arm (89 and 88%, respectively) compared to the trastuzumab arm where less benefit was seen in tumours with heterogenous HER2 expression [54].
In vitro studies that compared trastuzumab and T-DM1 in HER2+ cell lines revealed that T-DM1 is more efficacious in trastuzumab-sensitive as well as in trastuzumab-insensitive HER2+ cell lines. Using trastuzumab-resistant xenograft tumour models, it was also demonstrated that T-DM1 can induce both apoptosis and mitotic catastrophe in vivo [55, 56]. However, the focality of HER2 expression might attenuate T-DM1 activity, which was unable to induce a bystander effect for surrounding HER2-negative cells due to a non-cleavable linker [54]. This issue was resolved through T-Dxd (DS-8201) that proved to overrate T-DM1 in HER2+ as well as in HER2 low BC (HER2 IHC 1+ or 2+ without HER2 gene amplification according to results of DESTINY-Breast04 trial [57, 58]. In that trial, the clinical outcome was similar in patients with a score of 1+ on IHC analysis and those with a score of 2+ [58].
Based on the previously mentioned experimental and clinical trial evidence, our evidence support that the differential response of HER2 + IHC classes to anti-HER2 therapy should be considered in treatment decision-making and that further trials to explore the differential response of HER2 IHC 2 + /Amplified to T-Dxd or T-DM1 compared to trastuzumab or other anti-HER2 targeting agents are warranted.
There is increasing evidence that response to anti-HER2 targeted therapy is closely related to intrinsic molecular subtypes. A study of the intrinsic molecular classes of HER2 + BC revealed that BC assigned to the HER2-E subtype by RNA-seq analysis is more likely to achieve a pCR compared to other intrinsic subtypes [17]. Recent systematic review and meta-analysis studies [17, 59,60,61,62] concluded that HER2-E biomarker identifies patients with increased likelihood of achieving a pCR following neoadjuvant anti-HER2-based therapy. Furthermore, in the PAMELA Phase 2 trial, they concluded that HER2-E subtype is the predictor of pCR following trastuzumab and lapatinib without chemotherapy in early-stage HER2 + BC [63]. Not all clinically HER2+ tumours are of the HER2-E intrinsic molecular subtype and only ∼50% of clinically HER2+ tumours fall into this category. Also, HER2 protein overexpressing tumours showed significantly higher expression of several receptor tyrosine kinases (RTKs) including FGFR4, EGFR, HER2 itself, as well as genes within the HER2 amplified region on Chr17q12-q21 (including GRB7). Our study supports such data as we found that HER2-E subtype is significantly associated with HER2 IHC 3+ rather than IHC 2 + / Amplified. In the same context, differential expression of genes responsible for HER2 oncogenic signalling pathway was more significant in HER2 IHC 3+ compared to HER2 IHC 2 + /Amplified unlike both classes of equivocal HER2 protein expression. Moreover, DGE analysis of genes responsible for resistance to trastuzumab therapy in HER2 + BC revealed that 60% of them are upregulated in HER2 IHC 2 + /Amplified tumours. ER status is also emerging as a robust predictive marker within HER2+ disease. Several clinical trials and studies highlighted the bidirectional crosstalk between HER2 and ER when both receptors are expressed in BC cells, where the main role of ER signalling in those tumours is to act as a mechanism of resistance to HER2 inhibition [7, 8, 11, 28, 29, 64,65,66]. However, the differential expression of ER within each HER2 + IHC class and its impact on response to therapy within that class is not clear. In our study ER positivity was a significant predictor of poorer response to therapy in the whole cohort and in IHC 2 + /Amplified, but not in HER2 IHC 3+ patients both in the neoadjuvant and adjuvant settings. These results are similar to Harbeck et al. [31] study which showed that in HER2 protein overexpression HR-positive patients had high pCR rates close to HR negative patients [31]. In a secondary analysis of the HERA trial, the largest of the adjuvant trastuzumab trials, the role of ER IHC status levels combined with HER2 levels, in predicting the magnitude of benefit from adjuvant trastuzumab was investigated. The trial showed that patients with ER-positive and HER2+ with low HER2 gene copy number derived less benefit from adjuvant trastuzumab with all of these patients received endocrine therapy [67]. Also, in a second analysis of NeoALTTO clinical trial which aimed to quantify gene expression levels of ESR1 and HER2 and their relation to pCR, it was revealed that high levels of HER2 and low levels of ESR1 were associated with higher pCR rates [68] They explained these findings based on the increasing amount of genomic and clinical data reporting that HER2-overexpressing tumours have distinct molecular and clinical profiles [67] and that the HER2-E subtype, which is predominantly ER-negative, achieved higher response to HER2-directed therapy [69]. Conversely, the luminal B subtype (HER2+ and ER + ) showed higher expression of the luminal cluster of genes, including GATA3, BCL2 and ESR1. Therefore, a larger proportion of these tumours are driven by the ER pathways with a limited impact of HER2 oncogenic signalling pathways [70].
Furthermore, the DGE analysis performed in this study revealed that HER2 IHC 2 + /Amplified tumours are more frequently ER + , more enriched with ER signalling pathways and its associated genes like ESR1 and BCL2 and less likely to include tumours with HER2-E molecular subtype.
Treating HER2 + /ER + BC is complex, particularly in the HER2 2 + /Amplified group. There is no single treatment or combination of treatments that is most effective or suited to all patients with this subtype. Identifying what is the biological driver of the individual tumour can be of great help (i.e., whether ER or HER2 signalling is dominating and driving the growth and progression of the tumour), though pathway interaction and crosstalk can cause the cancer to change course throughout treatment.
In the preclinical setting, it has been shown that the expression of ER and its downstream targets are increased in cells with acquired resistance to anti-HER2 therapy [71, 72]. Reactivation of ER expression and signalling, including a switch from ER-negative to ER-positive status, were observed in clinical HER2+ tumours after neoadjuvant lapatinib treatment [71].
Furthermore, HER2 overexpression affects endocrine therapy responsiveness both to tamoxifen and to oestrogen deprivation by aromatase inhibitors (AI) and ovarian suppression in premenopausal women [71, 73,74,75,76,77,78,79].
Combining hormone therapy with an anti-HER2 agent has proven beneficial to some specific HER2+ patients [80, 81], particularly those who have high ER expression. While some ER + /HER2+ tumours behave more like the luminal A subtype (i.e., ER-driven cancer) and others as HER2-E tumour (HER2-driven cancer) or a combination of both which require a multipronged targeted blockade of both ER and HER2 pathways.
Young premenopausal women with HR-positive BC are mostly treated with oestrogen modulators, such as Tamoxifen, ovarian function suppression alone or in combination with AI [82]. Moreover, preclinical data supported the idea that PI3K inhibitors and CDK4/6 could be attractive target that functions downstream of both ER and HER2 pathways. PATRICA trial which assessed palbociclib in combination with trastuzumab with or without endocrine therapy in patients with HER2+ advanced BC revealed promising survival outcomes of patients with ER + /HER2 + BC with a PAM50 Luminal A or B subtype treated with trastuzumab [83]. MonarcHER Phase II trial also demonstrated that the combination of abemaciclib, fulvestrant, and trastuzumab significantly improved progression-free survival versus standard-of-care chemotherapy plus trastuzumab [84].
This study has some limitations, as it was performed on multiple retrospective datasets with variable treatment options.
Conclusion
BC with HER2 protein overexpression (IHC 3 + ) appear to be driven by HER2 oncogenic signalling pathway, more HER2-E, which may explain their better response to anti-HER2. Patients with HER2 IHC 2 + /Amplified tumours have limited response to anti-HER2 therapy regardless of the HER2 gene amplification status, particularly those with ER+ tumours. Further comparative studies between conventional anti-HER2 therapy and HER2-directed antibody-drug conjugate therapy in patients with IHC 2 + /Amplified BC could be warranted.
Data availability
All data used in this study are available and can be accessed upon reasonable request. The following publicly available datasets were used on https://identifiers.org/cbioportal:brca_tcga; https://identifiers.org/cbioportal:brca_metabric;https://www.ncbi.nlm.nih.gov/gds.
References
Dodson A, Parry S, Ibrahim M, Bartlett JM, Pinder S, Dowsett M, et al. Breast cancer biomarkers in clinical testing: analysis of a UK national external quality assessment scheme for immunocytochemistry and in situ hybridisation database containing results from 199 300 patients. J Pathol Clin Res. 2018;4:262–73.
Rakha EA, Pinder SE, Bartlett JM, Ibrahim M, Starczynski J, Carder PJ, et al. Updated UK recommendations for HER2 assessment in breast cancer. J Clin Pathol. 2015;68:93–9.
Wolff AC, Hammond ME, Hicks DG, Dowsett M, McShane LM, Allison KH, et al. Recommendations for human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline update. J Clin Oncol. 2013;31:3997–4013.
Loibl S, Gianni L. HER2-positive breast cancer. Lancet. 2017;389:2415–29.
Wolff AC, Hammond MEH, Allison KH, Harvey BE, Mangu PB, Bartlett JM, et al. Human epidermal growth factor receptor 2 testing in breast cancer: American Society of Clinical Oncology/College of American Pathologists clinical practice guideline focused update. Arch Pathol Lab Med. 2018;142:1364–82.
Katayama A, Miligy IM, Shiino S, Toss MS, Eldib K, Kurozumi S, et al. Predictors of pathological complete response to neoadjuvant treatment and changes to post-neoadjuvant HER2 status in HER2-positive invasive breast cancer. Mod Pathol. 2021;34:1271–81.
Schneeweiss A, Chia S, Hickish T, Harvey V, Eniu A, Hegg R, et al. Pertuzumab plus trastuzumab in combination with standard neoadjuvant anthracycline-containing and anthracycline-free chemotherapy regimens in patients with HER2-positive early breast cancer: a randomized phase II cardiac safety study (TRYPHAENA). Ann Oncol. 2013;24:2278–84.
Swain S, Ewer M, Viale G, Delaloge S, Ferrero J-M, Verrill M, et al. Pertuzumab, trastuzumab, and standard anthracycline-and taxane-based chemotherapy for the neoadjuvant treatment of patients with HER2-positive localized breast cancer (BERENICE): a phase II, open-label, multicenter, multinational cardiac safety study. Ann Oncol. 2018;29:646–53.
Houssami N, Macaskill P, von Minckwitz G, Marinovich ML, Mamounas E. Meta-analysis of the association of breast cancer subtype and pathologic complete response to neoadjuvant chemotherapy. Eur J Cancer. 2012;48:3342–54.
Broglio KR, Quintana M, Foster M, Olinger M, McGlothlin A, Berry SM, et al. Association of pathologic complete response to neoadjuvant therapy in HER2-positive breast cancer with long-term outcomes: a meta-analysis. JAMA Oncol. 2016;2:751–60.
Gianni L, Pienkowski T, Im Y-H, Roman L, Tseng L-M, Liu M-C, et al. Efficacy and safety of neoadjuvant pertuzumab and trastuzumab in women with locally advanced, inflammatory, or early HER2-positive breast cancer (NeoSphere): a randomised multicentre, open-label, phase 2 trial. lancet Oncol. 2012;13:25–32.
Chen H-L, Chen Q, Deng Y-C. Pathologic complete response to neoadjuvant anti-HER2 therapy is associated with HER2 immunohistochemistry score in HER2-positive early breast cancer. Medicine. 2021;100:e27632.
Rakha EA, Miligy IM, Quinn CM, Provenzano E, Shaaban AM, Marchiò C, et al. Retrospective observational study of HER2 immunohistochemistry in borderline breast cancer patients undergoing neoadjuvant therapy, with an emphasis on Group 2 (HER2/CEP17 ratio ≥ 2.0, HER2 copy number< 4.0 signals/cell) cases. Br J cancer. 2021;124:1836–42.
Yan H, Xiao H, Zhu J, Zhang J, Liu Z. Association between the HER2 protein expression level and the efficacy of neoadjuvant chemotherapy in HER2-positive breast cancer. Cancer Manag Res. 2020;12:12715.
Zhao J, Krishnamurti U, Zhang C, Meisel J, Wei Z, Suo A, et al. HER2 immunohistochemistry staining positivity is strongly predictive of tumor response to neoadjuvant chemotherapy in HER2 positive breast cancer. Pathol-Res Pract. 2020;216:153155.
Krystel-Whittemore M, Xu J, Brogi E, Ventura K, Patil S, Ross DS, et al. Pathologic complete response rate according to HER2 detection methods in HER2-positive breast cancer treated with neoadjuvant systemic therapy. Breast cancer Res Treat. 2019;177:61–6.
Lesurf R, Griffith OL, Griffith M, Hundal J, Trani L, Watson MA, et al. Genomic characterization of HER2-positive breast cancer and response to neoadjuvant trastuzumab and chemotherapy-results from the ACOSOG Z1041 (Alliance) trial. Ann Oncol. 2017;28:1070–7.
Slamon DJ, Leyland-Jones B, Shak S, Fuchs H, Paton V, Bajamonde A, et al. Use of chemotherapy plus a monoclonal antibody against HER2 for metastatic breast cancer that overexpresses HER2. N Engl J Med. 2001;344:783–92.
Arnould L, Arveux P, Couturier J, Gelly-Marty M, Loustalot C, Ettore F, et al. Pathologic complete response to trastuzumab-based neoadjuvant therapy is related to the level of HER-2 amplification. Clin Cancer Res. 2007;13:6404–9.
Kim J-W, Kim JH, Im S-A, Kim YJ, Han H-S, Kim J-S, et al. HER2/CEP17 ratio and HER2 immunohistochemistry predict clinical outcome after first-line trastuzumab plus taxane chemotherapy in patients with HER2 fluorescence in situ hybridization-positive metastatic breast cancer. Cancer Chemother Pharmacol. 2013;72:109–15.
Li F, Ju Q, Gao C, Li J, Wang X, Yan M, et al. Association of HER-2/CEP17 ratio and HER-2 copy number with pCR rate in HER-2-positive breast cancer after dual-target neoadjuvant therapy with trastuzumab and pertuzumab. Front Oncol. 2022;12:819818.
Singer CF, Tan YY, Fitzal F, Steger GG, Egle D, Reiner A, et al. Pathological complete response to neoadjuvant trastuzumab is dependent on HER2/CEP17 ratio in HER2-amplified early breast cancer. Clin Cancer Res. 2017;23:3676–83.
Guiu S, Gauthier M, Coudert B, Bonnetain F, Favier L, Ladoire S, et al. Pathological complete response and survival according to the level of HER-2 amplification after trastuzumab-based neoadjuvant therapy for breast cancer. Br J Cancer. 2010;103:1335–42.
Xu QQ, Pan B, Wang CJ, Zhou YD, Mao F, Lin Y, et al. HER2 amplification level is not a prognostic factor for HER2-positive breast cancer with trastuzumab-based adjuvant treatment: a systematic review and meta-analysis. Oncotarget. 2016;7:63571–82.
Perez EA, Reinholz MM, Hillman DW, Tenner KS, Schroeder MJ, Davidson NE, et al. HER2 and chromosome 17 effect on patient outcome in the N9831 adjuvant trastuzumab trial. J Clin Oncol. 2010;28:4307–15.
Venet D, Rediti M, Maetens M, Fumagalli D, Brown DN, Majjaj S, et al. Copy number aberration analysis to predict response to neoadjuvant anti-HER2 therapy: results from the neoALTTO phase III clinical trialcopy number aberrations predict pCR in HER2+ breast cancer. Clin Cancer Res. 2021;27:5607–18.
Dowsett M, Procter M, McCaskill-Stevens W, De Azambuja E, Dafni U, Rueschoff J, et al. Disease-free survival according to degree of HER2 amplification for patients treated with adjuvant chemotherapy with or without 1 year of trastuzumab: the HERA trial. J Clin Oncol. 2009;27:2962.
Beitsch P, Whitworth P, Baron P, Rotkis MC, Mislowsky AM, Richards PD, et al. Pertuzumab/trastuzumab/CT versus trastuzumab/CT therapy for HER2+ breast cancer: results from the prospective neoadjuvant breast registry symphony trial (NBRST). Ann Surg Oncol. 2017;24:2539–46.
Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014;384:164–72.
Giuliano M, Trivedi MV, Schiff R. Bidirectional crosstalk between the estrogen receptor and human epidermal growth factor receptor 2 signaling pathways in breast cancer: molecular basis and clinical implications. Breast Care). 2013;8:256–62.
Harbeck N, Gluz O, Christgen M, Kates RE, Braun M, Küemmel S, et al. De-escalation strategies in human epidermal growth factor receptor 2 (HER2)-positive early breast cancer (BC): final analysis of the West German Study Group adjuvant dynamic marker-adjusted personalized therapy trial optimizing risk assessment and therapy response prediction in early BC HER2- and hormone receptor–positive phase II randomized trial—efficacy, safety, and predictive markers for 12 weeks of neoadjuvant trastuzumab emtansine with or without endocrine therapy (ET) versus trastuzumab plus ET. J Clin Oncol. 2017;35:3046–54.
Xu B, Shen J, Zhang L, Zhao W, Wang L. HER2 protein expression level is positively associated with the efficacy of neoadjuvant systemic therapy in HER2-positive breast cancer. Pathol-Res Pract. 2022;234:153900.
Allison KH, Hammond MEH, Dowsett M, McKernin SE, Carey LA, Fitzgibbons PL, et al. Estrogen and progesterone receptor testing in breast cancer: ASCO/CAP guideline update. J Clin Oncol. 2020;38:1346–66.
Hoadley KA, Yau C, Wolf DM, Cherniack AD, Tamborero D, Ng S, et al. Multiplatform analysis of 12 cancer types reveals molecular classification within and across tissues of origin. Cell. 2014;158:929–44.
Gao J, Aksoy BA, Dogrusoz U, Dresdner G, Gross B, Sumer SO, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci Signal. 2013;6:pl1–pl.
Curtis C, Shah SP, Chin S-F, Turashvili G, Rueda OM, Dunning MJ, et al. The genomic and transcriptomic architecture of 2,000 breast tumours reveals novel subgroups. Nature. 2012;486:346–52.
Liao Y, Wang J, Jaehnig EJ, Shi Z, Zhang B. WebGestalt 2019: gene set analysis toolkit with revamped UIs and APIs. Nucleic acids Res. 2019;47:W199–w205.
Bria E, Carbognin L, Furlanetto J, Pilotto S, Bonomi M, Guarneri V, et al. Impact of neoadjuvant single or dual HER2 inhibition and chemotherapy backbone upon pathological complete response in operable and locally advanced breast cancer: sensitivity analysis of randomized trials. Cancer Treat Rev. 2014;40:847–56.
Carey LA, Berry DA, Ollila D, Harris L, Krop IE, Weckstein D, et al. Clinical and translational results of CALGB 40601: A neoadjuvant phase III trial of weekly paclitaxel and trastuzumab with or without lapatinib for HER2-positive breast cancer. J Clin Oncol. 2013;31(15_suppl):500-500.
Gianni L, Dafni U, Gelber RD, Azambuja E, Muehlbauer S, Goldhirsch A, et al. Treatment with trastuzumab for 1 year after adjuvant chemotherapy in patients with HER2-positive early breast cancer: a 4-year follow-up of a randomised controlled trial. lancet Oncol. 2011;12:236–44.
Guarneri V, Frassoldati A, Bottini A, Cagossi K, Bisagni G, Sarti S, et al. Preoperative chemotherapy plus trastuzumab, lapatinib, or both in human epidermal growth factor receptor 2–positive operable breast cancer: results of the randomized phase II CHER-LOB study. J Clin Oncol. 2012;30:1989–95.
Pierga J-Y, Delaloge S, Espié M, Brain E, Sigal-Zafrani B, Mathieu M-C, et al. A multicenter randomized phase II study of sequential epirubicin/cyclophosphamide followed by docetaxel with or without celecoxib or trastuzumab according to HER2 status, as primary chemotherapy for localized invasive breast cancer patients. Breast cancer Res Treat. 2010;122:429–37.
Robidoux A, Tang G, Rastogi P, Geyer CE Jr, Azar CA, Atkins JN, et al. Lapatinib as a component of neoadjuvant therapy for HER2-positive operable breast cancer (NSABP protocol B-41): an open-label, randomised phase 3 trial. lancet Oncol. 2013;14:1183–92.
Jacobs SA, Robidoux A, Abraham J, Pérez-Garcia JM, La Verde N, Orcutt JM, et al. NSABP FB-7: A phase II randomized neoadjuvant trial with paclitaxel+ trastuzumab and/or neratinib followed by chemotherapy and postoperative trastuzumab in HER2+ breast cancer. Breast Cancer Res. 2019;21:1–11.
Dybdal N, Leiberman G, Anderson S, McCune B, Bajamonde A, Cohen RL, et al. Determination of HER2 gene amplification by fluorescence in situ hybridization and concordance with the clinical trials immunohistochemical assay in women with metastatic breast cancer evaluated for treatment with trastuzumab. Breast Cancer Res Treat. 2005;93:3–11.
Middleton LP, Price KM, Puig P, Heydon LJ, Tarco E, Sneige N, et al. Implementation of American Society of Clinical Oncology/College of American Pathologists HER2 Guideline Recommendations in a tertiary care facility increases HER2 immunohistochemistry and fluorescence in situ hybridization concordance and decreases the number of inconclusive cases. Arch Pathol Lab Med. 2009;133:775–80.
Sui W, Ou M, Chen J, Wan Y, Peng H, Qi M, et al. Comparison of immunohistochemistry (IHC) and fluorescence in situ hybridization (FISH) assessment for Her-2 status in breast cancer. World J Surg Oncol. 2009;7:83.
Gullo G, Bettio D, Torri V, Masci G, Salvini P, Santoro A. Level of HER2/neu gene amplification as a predictive factor of response to trastuzumab-based therapy in patients with HER2-positive metastatic breast cancer. Investig N Drugs. 2009;27:179–83.
Swain SM, Miles D, Kim S-B, Im Y-H, Im S-A, Semiglazov V, et al. Pertuzumab, trastuzumab, and docetaxel for HER2-positive metastatic breast cancer (CLEOPATRA): end-of-study results from a double-blind, randomised, placebo-controlled, phase 3 study. Lancet Oncol. 2020;21:519–30.
Zabaglo L, Stoss O, Rüschoff J, Zielinski D, Salter J, Arfi M, et al. HER2 staining intensity in HER2-positive disease: relationship with FISH amplification and clinical outcome in the HERA trial of adjuvant trastuzumab. Ann Oncol. 2013;24:2761–6.
Mass RD, Press MF, Anderson S, Cobleigh MA, Vogel CL, Dybdal N, et al. Evaluation of clinical outcomes according to HER2 detection by fluorescence in situ hybridization in women with metastatic breast cancer treated with trastuzumab. Clin Breast Cancer. 2005;6:240–6.
Press MF, Sauter G, Buyse M, Fourmanoir H, Quinaux E, Tsao-Wei DD, et al. HER2 gene amplification testing by fluorescent in situ hybridization (FISH): comparison of the ASCO-College of American Pathologists Guidelines with FISH scores used for enrollment in breast cancer international research group clinical trials. J Clin Oncol. 2016;34:3518–28.
Modi S, Park H, Murthy RK, Iwata H, Tamura K, Tsurutani J, et al. Antitumor activity and safety of trastuzumab deruxtecan in patients with HER2-low-expressing advanced breast cancer: results from a phase Ib study. J Clin Oncol. 2020;38:1887–96.
Denkert C, Lambertini C, Fasching PA, Pogue-Geile KL, Mano MS, Untch M, et al. Biomarker data from the phase III KATHERINE study of adjuvant T-DM1 versus trastuzumab for residual invasive disease after neoadjuvant therapy for HER2-positive breast cancer. Clin Cancer Res. 2023;29:1569–81.
Barok M, Tanner M, Köninki K, Isola J. Trastuzumab-DM1 causes tumour growth inhibition by mitotic catastrophe in trastuzumab-resistant breast cancer cells in vivo. Breast Cancer Res: BCR. 2011;13:R46.
Lewis Phillips GD, Li G, Dugger DL, Crocker LM, Parsons KL, Mai E, et al. Targeting HER2-positive breast cancer with trastuzumab-DM1, an antibody–cytotoxic drug conjugate. Cancer Res. 2008;68:9280–90.
Cortés J, Kim S-B, Chung W-P, Im S-A, Park YH, Hegg R, et al. Trastuzumab deruxtecan versus trastuzumab emtansine for breast cancer. N Engl J Med. 2022;386:1143–54.
Modi S, Jacot W, Yamashita T, Sohn J, Vidal M, Tokunaga E, et al. Trastuzumab deruxtecan in previously treated HER2-low advanced breast cancer. N Engl J Med. 2022;387:9–20.
Schettini F, Pascual T, Conte B, Chic N, Brasó-Maristany F, Galván P, et al. HER2-enriched subtype and pathological complete response in HER2-positive breast cancer: a systematic review and meta-analysis. Cancer Treat Rev. 2020;84:101965.
Davey MG, Kerin E, O’Flaherty C, Maher E, Richard V, McAnena P, et al. Clinicopathological response to neoadjuvant therapies and pathological complete response as a biomarker of survival in human epidermal growth factor receptor-2 enriched breast cancer–a retrospective cohort study. Breast. 2021;59:67–75.
Shen G, Zhao F, Huo X, Ren D, Du F, Zheng F, et al. Meta-analysis of HER2-enriched subtype predicting the pathological complete response within HER2-positive breast cancer in patients who received neoadjuvant treatment. Front Oncol. 2021;11:632357.
Prat A, Pascual T, De Angelis C, Gutierrez C, Llombart-Cussac A, Wang T, et al. HER2-enriched subtype and ERBB2 expression in HER2-positive breast cancer treated with dual HER2 blockade. J Natl Cancer Inst. 2020;112:46–54.
Llombart-Cussac A, Cortés J, Paré L, Galván P, Bermejo B, Martínez N, et al. HER2-enriched subtype as a predictor of pathological complete response following trastuzumab and lapatinib without chemotherapy in early-stage HER2-positive breast cancer (PAMELA): an open-label, single-group, multicentre, phase 2 trial. Lancet Oncol. 2017;18:545–54.
Brandão M, Caparica R, Malorni L, Prat A, Carey LA, Piccart M. What is the real impact of estrogen receptor status on the prognosis and treatment of HER2-positive early breast cancer? Clin Cancer Res. 2020;26:2783–8.
Pernas S, Tolaney SM. Targeting HER2 heterogeneity in early-stage breast cancer. Curr Opin Oncol. 2020;32:545–54.
von Minckwitz G, Rezai M, Fasching PA, Huober J, Tesch H, Bauerfeind I, et al. Survival after adding capecitabine and trastuzumab to neoadjuvant anthracycline-taxane-based chemotherapy for primary breast cancer (GBG 40–GeparQuattro). Ann Oncol. 2014;25:81–9.
Loi S, Dafni U, Karlis D, Polydoropoulou V, Young BM, Willis S, et al. Effects of estrogen receptor and human epidermal growth factor receptor-2 levels on the efficacy of trastuzumab: a secondary analysis of the HERA trial. JAMA Oncol. 2016;2:1040–7.
Fumagalli D, Venet D, Ignatiadis M, Azim HA Jr., Maetens M, Rothé F, et al. RNA sequencing to predict response to neoadjuvant anti-HER2 therapy: a secondary analysis of the neoALTTO randomized clinical trial. JAMA Oncol. 2017;3:227–34.
Prat A, Bianchini G, Thomas M, Belousov A, Cheang MC, Koehler A, et al. Research-based PAM50 subtype predictor identifies higher responses and improved survival outcomes in HER2-positive breast cancer in the NOAH study. Clin Cancer Res. 2014;20:511–21.
Koboldt DC, Fulton RS, McLellan MD, Schmidt H, Kalicki-Veizer J, McMichael JF, et al. Comprehensive molecular portraits of human breast tumours. Nature 2012;490:61–70.
Vaz-Luis I, Winer EP, Lin NU. Human epidermal growth factor receptor-2-positive breast cancer: does estrogen receptor status define two distinct subtypes? Ann Oncol. 2013;24:283–91.
Wang Y-C, Morrison G, Gillihan R, Guo J, Ward RM, Fu X, et al. Different mechanisms for resistance to trastuzumab versus lapatinib in HER2- positive breast cancers - role of estrogen receptor and HER2 reactivation. Breast Cancer Res. 2011;13:R121.
Lee AV, Cui X, Oesterreich S. Cross-talk among estrogen receptor, epidermal growth factor, and insulin-like growth factor signaling in breast cancer. Clin Cancer Res. 2001;7:4429s–35s.
Osborne CK, Schiff R. Estrogen-receptor biology: continuing progress and therapeutic implications. J Clin Oncol. 2005;23:1616–22.
Schiff R, Massarweh SA, Shou J, Bharwani L, Mohsin SK, Osborne CK. Cross-talk between estrogen receptor and growth factor pathways as a molecular target for overcoming endocrine resistance. Clin Cancer Res. 2004;10:331s–6s.
Zhang H, Berezov A, Wang Q, Zhang G, Drebin J, Murali R, et al. ErbB receptors: from oncogenes to targeted cancer therapies. J Clin Investig. 2007;117:2051–8.
Martin L-A, Farmer I, Johnston SR, Ali S, Marshall C, Dowsett M. Enhanced estrogen receptor (ER) α, ERBB2, and MAPK signal transduction pathways operate during the adaptation of MCF-7 cells to long term estrogen deprivation. J Biol Chem. 2003;278:30458–68.
Shou J, Massarweh S, Osborne CK, Wakeling AE, Ali S, Weiss H, et al. Mechanisms of tamoxifen resistance: increased estrogen receptor-HER2/neu cross-talk in ER/HER2–positive breast cancer. J Natl Cancer Inst. 2004;96:926–35.
Rimawi MF, Mayer IA, Forero A, Nanda R, Goetz MP, Rodriguez AA, et al. Multicenter phase II study of neoadjuvant lapatinib and trastuzumab with hormonal therapy and without chemotherapy in patients with human epidermal growth factor receptor 2-overexpressing breast cancer: TBCRC 006. J Clin Oncol. 2013;31:1726–31.
Montemurro F, Di Cosimo S, Arpino G. Human epidermal growth factor receptor 2 (HER2)-positive and hormone receptor-positive breast cancer: new insights into molecular interactions and clinical implications. Ann Oncol. 2013;24:2715–24.
Lønning PE. Poor-prognosis estrogen receptor-positive disease: present and future clinical solutions. Ther Adv Med Oncol. 2012;4:127–37.
Sella T, Ruddy KJ, Carey LA, Partridge AH. Optimal endocrine therapy in premenopausal women: a pragmatic approach to unanswered questions. JCO Oncol Pract. 2022;18:211–6.
Ciruelos E, Villagrasa P, Pascual T, Oliveira M, Pernas S, Paré L, et al. Palbociclib and trastuzumab in HER2-positive advanced breast cancer: results from the phase II SOLTI-1303 PATRICIA trial. Clin Cancer Res. 2020;26:5820–9.
Tolaney SM, Wardley AM, Zambelli S, Hilton JF, Troso-Sandoval TA, Ricci F, et al. Abemaciclib plus trastuzumab with or without fulvestrant versus trastuzumab plus standard-of-care chemotherapy in women with hormone receptor-positive, HER2-positive advanced breast cancer (monarcHER): a randomised, open-label, phase 2 trial. Lancet Oncol. 2020;21:763–75.
Acknowledgements
The authors are part of the PathLAKE digital pathology consortium. PathLAKE is one of the UK Government’s five AI Centres of Excellence and has received in-kind industry investment from Philips for digital pathology equipment, software, and other services. These new centres are supported by a £50 m investment from the Data to Early Diagnosis and Precision Medicine strand of the government’s Industrial Strategy Challenge Fund, managed and delivered by UK Research and Innovation (UKRI).
Funding
NA is supported and funded by the Egyptian Ministry of Higher Education and Scientific Research.
Author information
Authors and Affiliations
Contributions
Concept and design: NA and ER. Collection of the data: NA, NM and MA. Identifying and reviewing the images: NA and MT. Analysis of the data: NA, NM, MA and ER. Interpretation of the results: all authors. Writing and reviewing manuscript: all authors. All authors reviewed and agreed on the final revision of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
This study was approved by the Yorkshire & the Humber—Leeds East Research Ethics Committee (REC Reference: 19/YH/0293) under the IRAS Project ID: 266925. Data collected were fully anonymised.
Consent for publication
Not applicable.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Atallah, N.M., Alsaleem, M., Toss, M.S. et al. Differential response of HER2-positive breast cancer to anti-HER2 therapy based on HER2 protein expression level. Br J Cancer 129, 1692–1705 (2023). https://doi.org/10.1038/s41416-023-02426-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-023-02426-4