Abstract
Background
International guidelines emphasise the role of radiotherapy (RT) for the management of advanced adrenocortical carcinoma (ACC). However, the evidence for this recommendation is very low.
Methods
We retrospectively analysed all patients who received RT for advanced ACC in five European centres since 2000. Primary endpoint: time to progression of the treated lesion (tTTP). Secondary endpoints: best objective response, progression-free survival (PFS), overall survival (OS), adverse events, and the establishment of predictive factors by Cox analyses.
Results
In total, 132 tumoural lesions of 80 patients were treated with conventional RT (cRT) of 50–60 Gy (n = 20) or 20–49 Gy (n = 69), stereotactic body RT of 35–50 Gy (SBRT) (n = 36), or brachytherapy of 12–25 Gy (BT) (n = 7). Best objective lesional response was complete (n = 6), partial (n = 52), stable disease (n = 60), progressive disease (n = 14). Median tTTP was 7.6 months (1.0–148.6). In comparison to cRT20-49Gy, tTTP was significantly longer for cRT50-60Gy (multivariate adjusted HR 0.10; 95% CI 0.03–0.33; p < 0.001) and SBRT (HR 0.31; 95% CI 0.12–0.80; p = 0.016), but not for BT (HR 0.66; 95% CI 0.22–1.99; p = 0.46). Toxicity was generally mild and moderate with three grade 3 events. No convincing predictive factors could be established.
Conclusions
This largest published study on RT in advanced ACC provides clear evidence that RT is effective in ACC.
Similar content being viewed by others
Introduction
Adrenocortical carcinoma (ACC) is a rare malignancy with poor prognosis and 5-year overall survival ranging from about 80 % in patients with ACC stage I to less than 20 % in stage IV disease [1,2,3,4,5,6,7,8]. However, also in stage IV some patients survive many years and even complete responses have been reported [9,10,11].
For the treatment of recurrent and metastatic disease not amenable to complete resection, most international reviews and official guidelines recommend, mitotane alone or in combination with chemotherapy as first-line therapy [1, 8, 12,13,14,15]. Surgery of metastases is usually only performed if all tumoural lesions can be removed and the interval to previous surgery was above 12 months [16]. However, both current international guidelines on ACC emphasise the role of local therapies in advanced disease [1, 2]. The panellists agreed that local therapeutic measures (including radiation therapy (RT)) are of value for therapy of advanced ACC and suggested an individualised decision on which method to choose based on the localisation of the tumour lesion(s), local expertise, prognostic factors and patient’s preference. RT is also indicated for pain, prevention of imminent metastatic complications, severe mass effect or neurological symptoms. Several small studies and reviews suggest an improvement of neurological symptoms and pain relief by RT in ACC [2, 17,18,19,20] similar to other solid tumours [21, 22].
However, if studies focusing only on pain relief are excluded, there are only four retrospective reports including fewer than 60 patients in which 73 treatments with RT are described in unresectable ACC, but only 64 of them could be evaluated [19, 23,24,25].
Ho et al. investigated RT in a small cohort of 12 patients with advanced ACC treated with 18 courses of RT, but only 13 had adequate follow-up imaging to assess a radiographic response. After these 13 courses, 4 lesions decreased in size by 30% or greater, 2 were stable for the documented follow-up of 9.9 and 2.2 months, whereas 7 lesions were initially stable, but progressed after a mean time of 4.8 months [19]. In a study at MD Anderson in Houston, 19 patients were treated with RT due to abdominal disease or local recurrence. RT was described as only moderately effective. Only 3 patients (15.8%) were classified as responders, which was defined as a significant decrease of the lesion or as stabilisation of the lesion for at least 2 years. Combination treatment with mitotane and RT was moderately effective in three of 10 patients (30%) [23]. Magee et al. investigated the efficacy of RT in patients with locally invasive tumour, metastases or recurrent disease after surgery. Treatment response could be evaluated in only six of 10 patients treated by RT. Four experienced partial response assessed by reduction of the size of the primary tumour or metastases, or biochemical response, whereas in two patients no benefit could be demonstrated. However, the documented responses also lasted fewer than 12 months before disease progression [24]. Sabolch et al. evaluated the impact of RT on local tumour control in unresectable disease and local progression occurred only in 1 of 16 cases [25]. In conclusion, the results in these 57 patients were quite heterogeneous, but one has to acknowledge that the majority of these patients have been treated before 2000 and the used techniques are not really comparable anymore with methods offered to patients nowadays. Furthermore, none of these studies could provide any data on prognostic or predictive factors.
There is more experience for treatment with RT in an adjuvant setting. Until now retrospective studies describing more than 500 cases have been reported [12, 24,25,26,27,28,29,30,31,32], but several publications used the same databases with significantly overlapping cohorts and the true number of patients in large series is probably only around 380. Almost all studies showed that adjuvant RT can reduce the risk of local recurrence. However, data are conflicting regarding overall recurrence-free and overall survival [33]. Nevertheless, these studies suggest that the majority of ACCs are sensitive to RT.
Therefore, the aim of this study was to investigate patients with advanced ACC treated with currently state of the art RTs and to evaluate its efficacy and tolerance, and to identify predictors of response to RT.
Subjects and methods
Study population
This cohort study was part of the ENSAT registry study (www.ensat.org/registry) in five European reference centres for ACC (Berlin, Germany; Munich, Germany; Würzburg, Germany; London, UK and Eindhoven, Netherlands). It was approved by the ethics committees or institutional review boards at all participating institutions and all patients provided written informed consent. Patients with advanced ACC (defined as not completely resectable disease) and treatment with RT were included if they were treated between 2000 and April 2020. Follow-up for this study was closed in July 2022.
Demographic, clinical, and histological parameters sex, age at diagnosis, tumour size, evidence of hormonal excess, ENSAT tumour stage [7], information on local and systemic therapies before RT and details on RT (see below) were retrieved from the ENSAT ACC registry and medical records. All histological diagnoses were confirmed by experienced pathologists. Tumour staging at diagnosis was based on imaging studies and by the findings during surgery and pathological examination. Autonomous cortisol excess was defined as pathological dexamethasone test in the presence of suppressed baseline plasma ACTH.
Patients with lack of relevant information on primary diagnosis or follow-up or newly started concomitant systemic anti-tumour treatment within 12 weeks prior RT (except progressive disease was already documented) were excluded. Ongoing mitotane treatment (started more than 12 weeks prior RT) was permitted and mitotane blood levels were documented. Patients treated with adjuvant RT did not qualify for this study.
Details on radiotherapy
The following information on RT was captured: RT modality classified as conventional RT (cRT) stereotactic body radiotherapy (SBRT), and brachytherapy (BT), first day and duration of RT, number of fractions, and dose per fraction in Gray (Gy). Due to different RT techniques and treatment doses, patients were divided in different groups for statistical analyses. We defined four groups according to modality and dosage: patients treated by cRT with 50–60 Gy (cRT50-60Gy) or 20–49 Gy (cRT20-49Gy), by SBRT (with 35–50 Gy) and by BT (with 12–25 Gy). In addition, we analysed patients according to the equivalent dose in 2 Gy fractions (EQD2) and the biologically effective dose (BED10) using the linear quadratic model for radiobiology with an alpha/beta ratio of 10 Gy for adrenocortical tumours. For EQD2 and BED10 the patients were distributed to three groups according to RT dose. Since this retrospective analysis did not allow the definition in all patients whether a definitive or a palliative approach was intended at the time of RT, we discriminated post hoc two different groups: all procedures applying cRT50-60Gy, SBRT or BT were classified as ‘potentially definitive approach’, whereas cRT20-49Gy was judged as ‘potentially palliative approach’.
Outcome assessment
Prior to any analysis, we defined time to progression of the treated lesion (‘tTTP’) as the most relevant outcome. Each lesion was evaluated separately. We further analysed overall progression-free survival (‘oPFS’) which means that all tumoural lesions were judged independent of treatment with RT. The judgement of treatment response was based on routine radiologic assessment applying RECIST 1.1 criteria as close as possible. Best objective response was defined according to RECIST 1.1 criteria. The first radiological evaluation was performed after 2.6 months (range 1.1–14.6) and the second after 5.6 (1.5–17.8) months.
Documentation of adverse events
Medical records were reviewed for adverse events associated with RT. All adverse events were retrospectively scored according to the toxicity criteria of the radiation therapy oncology group (RTOG) and the common terminology criteria for adverse events (CTCAE v5.0) [34].
Statistical analysis
Time to progression of the treated lesion (tTTP) was defined as the time elapsing from the first day of RT to the first evidence of progression of this lesion or the date of last follow-up. Overall progression-free survival (oPFS) was defined as the time between the start of RT and the date of progression of any lesion or last follow-up. Overall survival (OS) was defined as the time from the date of first RT to the date of death or last follow-up. Patients without progression or death were censored at the date of last follow up. Survival analysis was calculated using the Kaplan-Meier method, and differences between groups were assessed by log-rank statistics.
We performed univariable analysis of factors that could potentially influence outcome after RT: sex, age, RT modality (cRT20-49Gy, cRT50-60Gy, SBRT, BT), time interval between primary diagnosis and RT (≤12 months vs. >12 months), number of therapies (in addition to primary surgery) before RT (≤3 vs. >3), size of the tumoural lesion treated with RT (≤30 mm vs. >30 mm), Ki67 index of the primary tumour (≤15 % vs. >15%), presence of autonomous glucocorticoid excess (yes vs no), localisation of treated lesion, number of lesions ≤5 vs. <5 and concomitant mitotane treatment (maximum plasma level during RT ≤ 14 mg/l vs. >14 mg/l). In a multivariable approach using the Cox proportional hazards model, tTTP, oPFS and OS were adjusted for all factors with p < 0.1 in univariate analysis. As an alternative to RT modality, EQD2 and BED10 were analysed in the same manner.
All reported P values are two-sided and P < 0.05 were considered to indicate statistical significance. Data were analysed using SPSS v.26 (IBM SPSS Statistics).
Results
Patient characteristics
The total cohort consisted of 80 patients with 132 individual lesions treated with RT. Key patients’ characteristics are given in Table 1. All patients suffered from advanced ACC at the time they were treated with RT. Age, sex, glucocorticoid excess, ENSAT stage and resection status at primary diagnosis did not differ significantly between the four groups of RT modality, but median Ki67 index of the primary tumour was higher in the cRT20-49 and ‘brachytherapy’ group compared to the others.
Radiotherapy characteristics
Table 2 provides details of the RT modalities and the treated lesions. Of a total of 132 tumoural lesions, 69 were treated with cRT20-49Gy, 20 with cRT50-60Gy, 36 with SBRT and 7 lesions with BT. Due to the different RT modalities the median number of fractions, the median dose per fraction, the median EQD2 and median BED10 differed significantly between the groups. Furthermore, lesions treated with SBRT were the smallest and lesions treated with brachytherapy were the largest. Median time between start of RT and first or second imaging was not significantly different between groups. Furthermore, the time interval between RT and first and second tumour evaluation were similar between both groups.
Clinical outcome according to treatment groups
57 of 80 patients died during follow-up (all due to progressive disease). Median time of follow-up of alive patients was 21.5 (1.9–132.2) months.
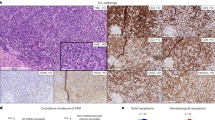
Best objective response of the 132 irradiated lesions was complete response in 6 lesions (4.5%), partial response in 52 lesions (39.4%) and stable disease in 60 (45.5%). Progression in the subsequent imaging was present in only 14 lesions (10.6%). The objective responses were scattered among the different treatment groups (Table 3). However, tTTP was significantly different between groups (Fig. 1). For the cRT50-60 Gy median tTTP was not reached, whereas it was 19.3 months for the SBRT group, 7.9 months for the cRT20-49 Gy group and only 4.6 months in patients treated with BT (p < 0.001).
Second, we compared treatment efficacy depending on the location of the treated tumoural lesions. In all soft tissue lesions, objective response rate was about 50% (Supplementary Table 1). However, tTTP varied slightly between the different locations (median tTTP for local recurrence 9.8 months, 17.5 months for bone lesions, 17.2 months for pulmonary lesions and 13.5 months for liver lesions, p = 0.81).
In univariable analysis the following factors were associated with improved outcome: modality of RT, male sex, Ki67 index of the primary tumour ≤15%, absence of autonomous cortisol secretion, size of the treated lesion ≤30 mm, and, a time interval between primary diagnosis and RT > 12 months (Table 4). Using a multivariable model (with the ‘cRT 20-49 Gy’ group as reference), time to local progression was significantly longer for cRT50-60Gy (HR 0.01; 95% CI 0.03–0.33; p < 0.001) and for SBRT (HR 0.31; 95% CI 0.12–0.80; p = 0.016), but not for BT (HR 0.66; 95% CI 0.22–1.99; p = 0.46). Among the other variables, only glucocorticoid excess remained significant (Table 4).
Median overall PFS in the cRT50-60Gy group was 15.7 months, in the cRT20-49 Gy group 5.6 months, in the SBRT group 3.2 months and in the BT group 2.9 months (p = 0.058). However, when adjusted in a multivariable analysis (with the ‘cRT20-49 Gy’ group as reference) these differences were not longer significant (cRT50-60Gy HR 0.50; 95% CI 0.25–1.01; p = 0.054); SBRT HR 1.21; 95% CI 0.73–2.0; p = 0.47; and BT (HR 1.60; 95% CI 0.66–3.91; p = 0.29) (Supplementary Table 2). Again only the presence of glucocorticoid excess correlated with a significantly shorter oPFS (p = 0.012).
At last follow-up, 8 (40%) patients in the cRT50-60Gy group, 9 (13%) patients in the cRT20-49Gy group, 9 (25%) patients in the SBRT group and 3 (42%) patients in the BT group were still alive. Median overall survival in the cRT50-60Gy group was 67.5 months, for cRT20-49Gy 13.5 months, in the SBRT group 60.7 months and in the BT group 16.3 months (p < 0.001). After multivariate analysis overall survival in comparison to cRT20-49Gy was significantly longer for cRT50-60Gy (HR 0.36; 95% CI 0.16–0.83; p = 0.017), but not for SBRT (HR 0.45; 95% CI 0.18–1.12; p = 0.09) and BT group (HR 0.92; 95% CI 0.26–3.28; p = 0.91). Furthermore, Ki67 index >15% led to a significantly shorter OS (p = 0.014) (Supplementary Table 3).
Clinical outcomes according to EQD2 and BED10
We analysed clinical outcomes in another approach distributing the lesions according to EQD2 and BED10. EQD2 was calculated for each RT treatment and the lesions were distributed in three groups EQD2<40Gy (n = 48), EQD240-50Gy (n = 36), EQD2>51Gy (n = 48). For BED10 lesions were distributed the cases in the following three groups <50 Gy (n = 51), 50–60 Gy (n = 39), >61 Gy (n = 42).
With regard to best objective response, EQD2 seems to represent a quite useful predictor, because 5 of 6 patients with complete response were treated with an EQD2 > 51 Gy. In addition, none of the 48 patients in this group experienced an immediate progress of the treated lesion. This was also reinforced by the multivariable adjusted Cox regression model (Supplementary Table 4 and Supplementary Fig. 1).
Using EQD2<40Gy as reference group, time to local progression was significantly longer in the EQD2>51Gy and EQD240-50Gy group (62.6 months vs. 19.2 months vs. 7.9 months; p < 0.001). After multivariable adjustment the corresponding HR were 0.24; 95% CI 0.09–0.64; p = 0.004 and 0.33; 95% CI 0.12–0.89; p = 0.029. Surprisingly male sex correlated with a significantly longer tTTP (HR 0.46; 95% CI 0.22–0.98; p = 0.045).
Regarding overall survival, patients with higher EQD2 had a significant longer OS in comparison to EQD2<40 Gy (EQD250-60Gy HR 0.39; 95% CI 0.17–0.88; p = 0.023; EQD2>61Gy HR 0.35; 95% CI 0.15–0.81; p = 0.014; multivariate analysis with the same variables as for overall survival in treatment groups). Among the other evaluated variables, only Ki67index > 15 % correlated with a shorter OS (p = 0.015).
Similar results were achieved if we dived the group using BED10. In comparison with BED10<50Gy, tTTP was significantly longer for BED1050-60Gy (multivariable adjusted HR 0.25; 95% CI 0.09–0.68; p = 0.007) and for BED10>61Gy (HR 0.29; 95% CI 0.12–0.77; p = 0.012) corresponding with a median tTTP of 28.6, 19.3, and 7.9 months (p = 0.001). Again, male sex was associated significantly with longer tTTP (p = 0.046). For overall survival, patients with higher BED had a significantly prolonged OS in comparison to BED<50Gy (BED1050-60Gy HR 0.41; 95% CI 0.18–0.93; p = 0.033; BED10>61Gy HR 0.34; 95% CI 0.16–0.77; p = 0.009) (Supplementary Table 5 and Supplementary Fig. 1).
Clinical outcomes according to the potential intention of treatment
We defined definitive intention corresponding treatment group cRT50-60Gy, SBRT and BT (n = 63) and treatment with cRT20-49Gy (n = 69) as palliative treatment.
In the 63 lesions treated with ‘potentially definitive approach’, only 22 progressed during follow-up (34.9%), whereas this was the case in 40 of 69 lesions in ‘potentially palliative approach’ (58.0%). Accordingly, median tTTP was significantly different in these groups (62.3 months vs. 7.9 months; p < 0.001) and this difference was confirmed in the multivariable Cox regression model (HR 0.24; 95% CI 0.11–0.52; p < 0.001). We did not find any predictive factor among the other variables tested (Supplementary Fig. 2).
Overall survival was also significantly longer in the definitive treatment group (HR 0.44; 95% CI 0.22–0.89; p = 0.022). Similarly to the analysis for OS above, Ki67 index >15% led to a shorter OS (HR 0.41; 95% CI 0.20–0.84; p = 0.015) (Supplementary Fig. 2).
Adverse events in patients with radiotherapy
The documented adverse events associated with RT were mostly mild or moderate and typical for RT (Table 5). The most frequent toxicities were low grade intestinal and pulmonary adverse events. One grade 3 intestinal adverse event with diarrhoea occurred after a conventional RT with 55 Gy, and two pulmonary grade 3 events with pneumonitis were documented after the conventional treatment with 43 Gy each, respectively.
Discussion
This retrospective study represents the largest cohort of patients with advanced ACC treated with RT. Our data indicate that RT (especially when applied in adequate dosage) is of benefit for selected patients confirming what previous small studies [19, 23,24,25, 32] suggested and what the recent guideline panels [1, 8] concluded mainly based on expert opinion. In most of the treated lesions stable disease or partial responses could be documented; in 6 out of 132 lesions even complete response was achieved. Overall, in only 11% of lesions immediate progression was diagnosed. The reported toxicity was moderate and within the expected range of RT of solid tumoural lesions.
The comparison of the different RT modalities suggests that conventional RT with more than 50 Gy is more efficient than the other methods, as expected. However, the small number of patients in this group (n = 20) and especially in the brachytherapy group (n = 7) calls for caution. To allow a better comparability of the different fractionation schemes we applied the concept of the linear quadratic model and calculated the corresponding EQD2 and BED10 values. These two approaches reinforced our findings of longer tTTP with higher radiation dosage. Of note, patients treated with an EQD2 > 40 Gy or BED10 > 50 Gy experienced a median time to local progression of 62.6 and 28.6 months respectively. Thus, one could also conclude that SBRT might be the preferred option if feasible and the achievable EQD2 and BED10 are above these cutoffs. Furthermore, patient preference is likely in favour of SBRT because of the shorter overall treatment period.
RT in ACC is traditionally used as a palliative therapy especially in symptomatic bone, brain or inferior vena cava involvement [35]. However, our data clearly indicate its important role in selected patients with ACC and non-resectable lesions beyond palliation. Nevertheless, a relevant proportion of patients of our cohort has been treated with a palliative concept not primarily aiming at long-term disease control. Therefore, it appears to be important to adjust for possible prognostic or predictive factors. However, even with this approach, conventional RT with more than 50 Gy seemed to be the most efficient therapy. Unfortunately, our search for predictive factors was not very successful. Overall, there was some indication that patients without glucocorticoid excess and with a Ki67 ≤ 15% of the primary tumour might benefit more than others. However, we would be reluctant to use these factors as strong selection criteria. Similarly, we are not yet convinced that male patients have a better outcome to RT, although this finding might deserve future research.
Although RT cannot prevent progression of other lesions or further metastatic spread, it has clearly the power to reach long-term disease control in many patients with limited numbers of tumoural lesions. Therefore, it seems likely that this local effect also translates to an overall clinical benefit in a relevant subset of patients, although we cannot prove this in this retrospective analysis. Furthermore, RT could have additional positive effects in patients treated with immunotherapy due to potential abscopal effects. However, this has never been demonstrated for patients with ACC.
Our study has obvious limitations including the retrospective nature, the still low number of patients, and the lack of a control group. However, due to the absence of published evidence on RT in advanced ACC, this study currently represents the best data available. Due to the rarity of the disease, it is unlikely that a much larger cohort will be recruited in the near future. Another limitation is the heterogeneity of RT modalities and the different group sizes. In addition, we have to acknowledge that the decision for RT was made by local treating physicians and was not based on any defined criteria. Therefore, a selection bias is possible. Smaller lesions and lesions with lower Ki67 index were treated in most of the cases with higher doses of RT, which might have affect the response to RT. Furthermore, RT was not applied according to a standardised protocol nor was this the case for co-treatment with mitotane. However, the number of patients treated with mitotane was quite similar between the four groups and the documented mitotane plasma levels were in the same range. Neither the treatment with mitotane nor the mitotane plasma level had any relevant influence on the efficacy of RT.
In conclusion, our study clearly suggests that RT is associated with beneficial effects on clinical outcome in selected patients with advanced ACC when applied in adequate dosage. These results provide the strongest evidence so far for the use of RT in advanced ACC and it provides a good basis for prospective studies to reduce the uncertainties and limitations of retrospective cohort studies. We would hope that our study will raise interest in considering RT more frequently as a treatment option in advanced disease, where it should not be limited to palliation.
Data availability
The datasets generated and /or analysed during this study are not publicly available due to privacy issues of the patients with a very rare disease but are available in an anonymized fashion from the corresponding author on reasonable request.
References
Fassnacht M, Assie G, Baudin E, Eisenhofer G, de la Fouchardiere C, Haak HR, et al. Adrenocortical carcinomas and malignant phaeochromocytomas: ESMO-EURACAN Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2020;31:1476–90.
Megerle F, Kroiss M, Hahner S, Fassnacht M. Advanced adrenocortical carcinoma - what to do when first-line therapy fails? Exp Clin Endocrinol Diabetes. 2019;127:109–16.
Vaidya A, Nehs M, Kilbridge K. Treatment of adrenocortical carcinoma. Surg Pathol Clin. 2019;12:997–1006.
Berruti A, Fassnacht M, Haak H, Else T, Baudin E, Sperone P, et al. Prognostic role of overt hypercortisolism in completely operated patients with adrenocortical cancer. Eur Urol. 2014;65:832–8.
Baudin E. Endocrine tumor board of Gustave R. Adrenocortical carcinoma. Endocrinol Metab Clin North Am. 2015;44:411–34.
Datta J, Roses RE. Surgical management of adrenocortical carcinoma: an evidence-based approach. Surg Oncol Clin N. Am. 2016;25:153–70.
Fassnacht M, Johanssen S, Quinkler M, Bucsky P, Willenberg HS, Beuschlein F, et al. Limited prognostic value of the 2004 International Union Against Cancer staging classification for adrenocortical carcinoma: proposal for a Revised TNM Classification. Cancer 2009;115:243–50.
Fassnacht M, Dekkers OM, Else T, Baudin E, Berruti A, de Krijger R, et al. European Society of Endocrinology Clinical Practice Guidelines on the management of adrenocortical carcinoma in adults, in collaboration with the European Network for the Study of Adrenal Tumors. Eur J Endocrinol. 2018;179:G1–G46.
Pommier RF, Brennan MF. An eleven-year experience with adrenocortical carcinoma. Surgery. 1992;112:963–70. discussion 70-1
Schulick RD, Brennan MF. Long-term survival after complete resection and repeat resection in patients with adrenocortical carcinoma. Ann Surg Oncol. 1999;6:719–26.
Elhassan YS, Altieri B, Berhane S, Cosentini D, Calabrese A, Haissaguerre M, et al. S-GRAS score for prognostic classification of adrenocortical carcinoma: an international, multicenter ENSAT study. Eur J Endocrinol. 2021;186:25–36.
Fassnacht M, Hahner S, Polat B, Koschker AC, Kenn W, Flentje M, et al. Efficacy of adjuvant radiotherapy of the tumor bed on local recurrence of adrenocortical carcinoma. J Clin Endocrinol Metab. 2006;91:4501–4.
Else T, Kim AC, Sabolch A, Raymond VM, Kandathil A, Caoili EM, et al. Adrenocortical carcinoma. Endocr Rev. 2014;35:282–326.
Kiseljak-Vassiliades K, Bancos I, Hamrahian A, Habra M, Vaidya A, Levine AC, et al. American association of clinical endocrinology disease state clinical review on the evaluation and management of adrenocortical carcinoma in an adult: a practical approach. Endocr Pr. 2020;26:1366–83.
Altieri B, Ronchi CL, Kroiss M, Fassnacht M. Next-generation therapies for adrenocortical carcinoma. Best Pr Res Clin Endocrinol Metab. 2020;34:101434.
Erdogan I, Deutschbein T, Jurowich C, Kroiss M, Ronchi C, Quinkler M, et al. The role of surgery in the management of recurrent adrenocortical carcinoma. J Clin Endocrinol Metab. 2013;98:181–91.
King DR, Lack EE. Adrenal cortical carcinoma: a clinical and pathologic study of 49 cases. Cancer. 1979;44:239–44.
Polat B, Fassnacht M, Pfreundner L, Guckenberger M, Bratengeier K, Johanssen S, et al. Radiotherapy in adrenocortical carcinoma. Cancer 2009;115:2816–23.
Ho J, Turkbey B, Edgerly M, Alimchandani M, Quezado M, Camphausen K, et al. Role of radiotherapy in adrenocortical carcinoma. Cancer J. 2013;19:288–94.
Pin Y, Paix A, Le Fevre C, Antoni D, Blondet C, Noel G. A systematic review of palliative bone radiotherapy based on pain relief and retreatment rates. Crit Rev Oncol Hemat. 2018;123:132–7.
Sharma S, Hertan L, Jones J. Palliative radiotherapy: current status and future directions. Semin Oncol. 2014;41:751–63.
Williams GR, Manjunath SH, Butala AA, Jones JA. Palliative radiotherapy for advanced cancers: indications and outcomes. Surg Oncol Clin N. Am. 2021;30:563–80.
Venkatesh S, Hickey RC, Sellin RV, Fernandez JF, Samaan NA. Adrenal cortical carcinoma. Cancer 1989;64:765–9.
Magee BJ, Gattamaneni HR, Pearson D. Adrenal cortical carcinoma: survival after radiotherapy. Clin Radio. 1987;38:587–8.
Sabolch A, Feng M, Griffith K, Hammer G, Doherty G, Ben-Josef E. Adjuvant and definitive radiotherapy for adrenocortical carcinoma. Int J Radiat Oncol. 2011;80:1477–84.
Habra MA, Ejaz S, Feng L, Das P, Deniz F, Grubbs EG, et al. A retrospective cohort analysis of the efficacy of adjuvant radiotherapy after primary surgical resection in patients with adrenocortical carcinoma. J Clin Endocrinol Metab. 2013;98:192–7.
Nelson DW, Chang SC, Bandera BC, Fischer TD, Wollman R, Goldfarb M. Adjuvant radiation is associated with improved survival for select patients with non-metastatic adrenocortical carcinoma. Ann Surg Oncol. 2018;25:2060–6.
Gharzai LA, Green MD, Griffith KA, Else T, Mayo CS, Hesseltine E, et al. Adjuvant radiation improves recurrence-free survival and overall survival in adrenocortical carcinoma. J Clin Endocrinol Metab. 2019;104:3743–50.
Zhu J, Zheng Z, Shen J, Lian X, Miao Z, Shen J, et al. Efficacy of adjuvant radiotherapy for treatment of adrenocortical carcinoma: a retrospective study and an updated meta-analysis. Radiat Oncol. 2020;15:118.
Ginsburg KB, Chandra AA, Schober JP, Handorf EA, Uzzo RG, Greenberg RE, et al. Identification of oncological characteristics associated with improved overall survival in patients with adrenocortical carcinoma treated with adjuvant radiation therapy: Insights from the National Cancer Database. Urol Oncol. 2021;39:791 e1–e7.
Thomas JJ, Tward JD. Stage presentation, care patterns, treatment outcomes, and impact of radiotherapy on overall survival for adrenocortical carcinoma. Clin Genitourin Cancer. 2021;19:417–24.
Hermsen IG, Groenen YE, Dercksen MW, Theuws J, Haak HR. Response to radiation therapy in adrenocortical carcinoma. J Endocrinol Invest. 2010;33:712–4.
Terzolo M, Fassnacht M. Our experience with the management of patients with non-metastatic adrenocortical carcinoma. Eur J Endocrinol. 2022;187:R27–40.
Cox JD, Stetz J, Pajak TF. Toxicity criteria of the Radiation Therapy Oncology Group (RTOG) and the European Organization for Research and Treatment of Cancer (EORTC). Int J Radiat Oncol Biol Phys. 1995;31:1341–6.
Milgrom SA, Goodman KA. The role of radiation therapy in the management of adrenal carcinoma and adrenal metastases. J Surg Oncol. 2012;106:647–50.
Acknowledgements
This study was made possible by the ACC database of the European Network for the Study of Adrenal Tumours (ENSAT). We are thankful for continuous help in data documentation from Michaela Haaf.
Funding
This study was supported by the Clinician Scientist programme RISE funded by the Else Kröner-Fresenius-Stiftung & the Eva Luise und Horst Köhler Stiftung and the German Research Foundation (DFG) project 314061271 (TRR-CRC 205), and the European Reference networks Endo-ERN and EuRanCan. Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
OK: Conceptualization; Data curation; Formal analysis; Visualization; Writing—original draft. PS: Data curation; review & editing. LS-P: Data curation; review & editing. BA: Data curation; review & editing. MQ: Data curation; review & editing. JP: Data curation; review & editing. HH: Data curation; review & editing. FM: Data curation; review & editing UD: Data curation; review & editing. MK: Data curation; review & editing. KM: Data curation; review & editing. BP: Conceptualization; Data curation; Writing—review & editing, Supervision MF: Conceptualization; Data curation; Formal analysis; Funding acquisition; Writing—review & editing, Supervision. All authors approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
MK received travel cost reimbursement, speaker honoraria, and research support from Ipsen Pharma. MF has served in an advisory board of HRA Pharma on the management of adrenocortical carcinoma. Remunerations paid to his university hospital. OK received speaker honoraria from HRA Pharma. PS, LSP, BA, MQ, JP, HH, UD, KM, BP declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Ethics approval and consent to participate
This cohort study was part of the ENSAT registry study (www.ensat.org/registry) in five European reference centres for ACC (Würzburg, Germany; Berlin, Germany; Munich, Germany; London, UK; Eindhoven, Netherlands). It was approved by the ethics committees/institutional review boards at all participating institutions and all patients provided written informed consent.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kimpel, O., Schindler, P., Schmidt-Pennington, L. et al. Efficacy and safety of radiation therapy in advanced adrenocortical carcinoma. Br J Cancer 128, 586–593 (2023). https://doi.org/10.1038/s41416-022-02082-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-022-02082-0