Abstract
Background
PTEN loss is a putative driver in histotypes of ovarian cancer (high-grade serous (HGSOC), endometrioid (ENOC), clear cell (CCOC), mucinous (MOC), low-grade serous (LGSOC)). We aimed to characterise PTEN expression as a biomarker in epithelial ovarian cancer in a large population-based study.
Methods
Tumours from 5400 patients from a multicentre observational, prospective cohort study of the Ovarian Tumour Tissue Analysis Consortium were used to evaluate associations between immunohistochemical PTEN patterns and overall survival time, age, stage, grade, residual tumour, CD8+ tumour-infiltrating lymphocytes (TIL) counts, expression of oestrogen receptor (ER), progesterone receptor (PR) and androgen receptor (AR) by means of Cox proportional hazard models and generalised Cochran–Mantel–Haenszel tests.
Results
Downregulation of cytoplasmic PTEN expression was most frequent in ENOC (most frequently in younger patients; p value = 0.0001) and CCOC and was associated with longer overall survival in HGSOC (hazard ratio: 0.78, 95% CI: 0.65–0.94, p value = 0.022). PTEN expression was associated with ER, PR and AR expression (p values: 0.0008, 0.062 and 0.0002, respectively) in HGSOC and with lower CD8 counts in CCOC (p value < 0.0001). Heterogeneous expression of PTEN was more prevalent in advanced HGSOC (p value = 0.019) and associated with higher CD8 counts (p value = 0.0016).
Conclusions
PTEN loss is a frequent driver in ovarian carcinoma associating distinctly with expression of hormonal receptors and CD8+ TIL counts in HGSOC and CCOC histotypes.
Similar content being viewed by others
Background
Ovarian cancer is the fifth leading cause of female cancer mortality and advances in the last decades have not translated into increased survival.1 High-grade serous ovarian cancer (HGSOC) is the most common histotype of ovarian cancer and is characterised by extreme genomic instability and chromosomal rearrangements. HGSOC has ubiquitous TP53 mutation, common mutations of BRCA1 and BRCA2 and amplification of CCNE1, MYC and PIK3CA (reviewed in ref. 2). Other common ovarian cancer histotypes are endometrioid (ENOC), clear cell (CCOC), mucinous (MOC) and low-grade serous (LGSOC) which have specific drivers and different cells of origin.1
Phosphatase and tensin homologue (PTEN) is a potent tumour suppressor classically known for its role in the inhibition of the phosphoinositide-3 kinase (PI3K) pathway. PTEN regulates cell proliferation, migration, survival, genomic stability and metabolism by phosphatase-dependent and phosphatase-independent activities.3 Loss of PTEN was associated with immunoresistance and worse response to programmed cell death protein 1 (PD-1) inhibitors in preclinical murine models of melanoma, by decreasing T cell trafficking into the tumours and T cell-mediated cell death in the tumour. Treatment with selective PI3Kbeta inhibitor improved the efficacy of both anti-PD-1 and anti-cytotoxic T-lymphocyte-associated protein 4 (anti-CTLA-4) antibodies in mouse models.3,4 Even subtle changes of PTEN expression may influence tumour initiation and progression as it is strongly regulated by critical molecular networks in which activation of hormonal receptors seems to have an important role.5
In ovarian cancer, mutation of PTEN has been a reported driver in endometrioid and clear cell subtypes.6,7,8,9,10 Homozygous loss of PTEN is found in 6% of HGSOC11 and loss-of-function mutations of Pten allow for accelerated tumour growth in mouse and in vitro models of HGSOC and ENOC.12,13,14 We previously demonstrated that PTEN loss is prevalent in HGSOC using bioinformatics and image analysis methods that corrected for cellularity in gene expression signatures from The Cancer Genome Atlas.15 PTEN and AR gene expression were significantly correlated and had positive survival effects. However, this and previous studies are limited by modest sample sizes and potential effects of different assay methods. Large-scale analysis of PTEN protein expression has not been carried out across the ovarian histotypes.
Therefore, we hypothesised that accurate estimates of PTEN loss across a large population would reveal histotype-specific associations with clinical and pathological factors using clinically relevant immunohistochemical (IHC) assays for PTEN, CD8 and the hormone receptors oestrogen receptor (ER), progesterone receptor (PR) and androgen receptor (AR).16,17 The prevalence of PTEN loss and the above associations will inform the likelihood of loss of PTEN being a driver.
Methods
Study design and participants
A total of 5400 women with ovarian cancer from 20 participating sites in the Ovarian Tumour Tissue Analysis (OTTA) Consortium with an average length of follow-up of 5.5 years were included in this study. We requested and received institutional review board/ethics board approval from the institutions participating in the OTTA Consortium. Patients were not provided compensation for their participation in the study at any site. Average length of follow-up per histotype were approximately 4.4 years for HGSOC, 7.6 for ENOC, 7.2 for CCOC, 6.6 for MOC and 5.8 for LGSOC (Table 1; Supplementary Table S1). One-third of the patients had delayed entry into the study, and for these cases, the mean enrolment time was 1.4 years post-diagnosis.
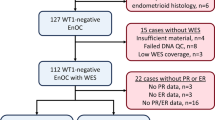
Demographic, clinical and pathological variables, including age at diagnosis, tumour stage and grade, presence or absence of post-operative residual tumour and scores for expression of PTEN, CD8, PR, AR and ER expression were used for the association analysis. Table 1 shows the absolute and relative number of histotype-specific participants with the variables mentioned above. Samples were obtained from pelvic disease and all the histological diagnosis were reviewed by experienced pathologists. Supplementary Table 1 provides information on variable-specific times of follow-up in person-years. Supplementary Fig. 1 summarises the analysis of missing data. Site dependency in missing data pattern was mostly due to different entry times into OTTA for different participant sites. Age at diagnosis was rarely missing (0.5%). The average age at diagnosis was slightly >60 years for HGSOC and around 55 years for other histotypes. Status at last follow-up, time of last follow-up and time of enrolment were mostly present (missed in 2.25, 1.5 and 0.65% of the cases, respectively). In all, 41% of the patients were still alive at the time of last follow-up. Causes of death were disease or treatment in 65.5% of the patients and unknown in 27.8% of the patients.
IHC analysis and scoring
IHC for PTEN was carried out in Cambridge (UK) using tissue microarrays (TMAs) obtained from formalin-fixed, paraffin-embedded tissues and primary antibody for PTEN (Cell Signaling, Danvers, MA, USA; PTEN—Clone 138G6) as previously described.15,18 The PTEN expression assay was previously validated using external positive and negative controls including mouse tissues from a conditional PTEN knockout model.18 PTEN scoring used normal stroma as an internal control. Heat-induced antigen retrieval was carried out in 10 mmol l−1 citric acid (pH 6.0) in a pressure cooker at 120 °C for 10 min. Sections were incubated overnight with PTEN antibody diluted 1:100 in 5% goat serum, followed by a 1-h incubation with anti-rabbit biotinylated secondary antibody and peroxidase-conjugated avidin–biotin complexes (Elite ABC; Vector Laboratories, Burlingame, CA, USA). Formed immunocomplexes were visualised using diaminobenzidine (DAB; DAKO, Glostrup, Denmark, EU), and slides were counterstained with haematoxylin. Sections were rinsed in phosphate-buffered saline between each step. IHC staining for AR was performed in Vancouver using the Ventana Discovery Ultra machine (Ventana Medical Systems Inc., Tuscon, AZ, USA). Sections underwent 36 min of Cell Conditioning 1 (Ventana Medical Systems) before incubation with AR antibody (Santa Cruz sc-815) titrated at 1:50 for 60 min at 37 °C. Antibody expression was detected using the DAB Map Detection Kit (Ventana Medical Systems) with the Universal Secondary Antibody (Ventana Medical Systems). Updated data for CD8, ER and PR staining was obtained from the OTTA Consortium.16,17
IHC samples were stored at room temperature (RT) for at least 48 h before image analysis. For IHC, an Ariol scanning system (Leica, Wetzlar, Germany) was used to obtain the digital images. Scoring was performed according to intensity (using stromal cells as internal positive controls) and the percentage of stained cells. Reproducibility was scored by two independent observers (A.P., F.C.M.) from a randomly assigned data set of 678 cases taken from all TMAs. Cytoplasmic and nuclear staining in the tumour cells was assessed separately. Cytoplasmic staining was scored as negative (no staining in any tumour cell with internal stromal control present), weak positive (all tumour cells with weaker staining compared to stromal cells), positive (all tumour and stromal cells equally stained) or heterogeneous (combination of positive and negative/weak staining) staining. Nuclear staining was scored based on the percentage of cells with positive nuclei for PTEN (0%; 0–10%; 10–50%; >50%).
For AR IHC, positive was defined as nuclear expression in >1% of tumour cells.
Statistical analysis
We used the generalised Cochran–Mantel–Haenszel (gCMH) tests to perform nominal and/or ordinal associations between cytoplasmic PTEN expression and relevant clinical, pathological and demographic variables within each histotype. For ordinal associations, only negative, weak and positive levels of PTEN expression were included.
The gCMH test is equivalent to the Pearson’s Chi-Square test for nominal–nominal associations, to the extended Cochran–Armitage test for nominal–ordinal associations and to the linear-by-linear association test for ordinal–ordinal associations.19 We assigned equidistant scores for ordinal levels. We used Holm’s multiplicity correction, valid under arbitrary assumptions, to achieve a global type I error of 5% per analysis and histotype. All p values presented in the manuscript are adjusted for multiplicity correction.
Significant associations were visualised using mosaic plots, which represent the different contingency table cells, in which the area of the tiles is proportional to the observed frequencies. Each tile is coloured depending on its contribution to the Pearson’s Chi-square statistics. For example, blue and red tiles correspond, respectively, to the cells showing frequencies smaller and greater than expected under the independence assumption. Further tests were performed to describe associations that were significant or clinically relevant.
In order to determine disease-specific survival associations with cytoplasmic PTEN expression, we used clinical data censored at 10 years from diagnosis and fitted Cox proportional hazard models stratified by site. With the exception of the cases with LGSOC, which had a small observed sample size, we controlled for age (and age squared), stage (four levels: I/II/III/IV), and post-operative residual tumour (2 levels: Yes/No). Survival times were left-truncated to obtain unbiased parameter estimates with delayed entries (refer to Section 3.5 of ref. 20 for detail), as well as right-censored for patients still alive after 10 years of follow-up or deceased owing to other causes. Deaths due to unknown causes were considered as disease related. We analysed the deviance and Schoenfeld residuals as model checks and performed sensitivity analyses by running the same analyses on data with imputed missing predictors21 and by controlling for the biomarkers CD8, ER, PR and AR independently or jointly (refer to Supplementary Material for detail). All IHC markers investigated were pre-specified before the analysis, and all statistical analyses were corrected for multiple testing. In the survival analyses, we used a multiplicity correction, which takes the dependence between the PTEN parameters of interest into account and allows for a global 5% type I error rate per histotype.22
Cohen’s κ and its weighted variant were, respectively, used to assess inter-rater reliability for categorical and ordinal outcomes, where −1, 0 and 1 represent complete disagreement, agreement by chance and complete agreement, respectively. The strength of association was described as recommended by Landis and Koch.23
Results
PTEN loss is prevalent across all histotypes of ovarian cancer
Classically PTEN acts as a cytoplasmic protein but is also expressed in the nucleus, where it may have several regulatory functions.24 In order to evaluate the reproducibility of both cytoplasmic and nuclear scoring, two observers compared 678 scores randomly assigned across all TMAs evaluated in this study (~4.4% of the original cohort). PTEN cytoplasmic scoring was reproducible between observers (Cohen’s weighted κ = 0.59 for the ‘negative’, ‘weak’ and ‘positive’ ordinal levels; 95% confidence interval (CI) 0.53–0.64) and inter-observer differences were mostly seen when assessing if a core had heterogeneous PTEN expression (Supplementary Fig. 2, Supplementary Table S2). Scoring of PTEN nuclear expression was less reproducible (Cohen’s weighted κ = 0.49 for the ‘0%’, ‘<10%’, ‘10–50%’ and ‘>50%’ ordinal levels; 95% CI 0.43–0.54). As PTEN is also infrequently expressed in the nucleus, only cytoplasmic staining was used for further analyses.
Loss of PTEN IHC cytoplasmic expression was statistically more frequent in endometrioid and clear cell histotypes, with 35% and 32% cases having complete absence of expression, respectively (Fig. 1, Supplementary Figure 3). In HGSOC, the proportion of PTEN loss or downregulation (scored as absent, weak or heterogeneous staining) was very similar to that observed in our previous smaller cohort (75% versus 77%, respectively).15
Mosaic representing the frequency of different scoring for PTEN expression using IHC per histotype with tiles of size proportional to their observed frequencies and colour coded according to their (signed) contributions to the Pearson’s Chi-square statistics. Blue and red tiles, respectively, correspond to cells showing frequencies smaller and greater than expected under the independence assumption. Refer to Supplementary Fig. 3 for the barplots of the absolute and relative frequency of the PTEN scores per histotype.
Early clonal loss of PTEN is a common event and late sub-clonal loss of PTEN is more common in advanced stages in HGSOC
PTEN loss appears in pre-invasive lesions in the fallopian tube and therefore is a putative early driver in HGSOC.25 Our results show that loss of PTEN expression was similar across all stages of HGSOC (with the exception of moderately lower prevalence of PTEN negativity in stage II), consistent with previous evidence that PTEN is commonly lost early in tumour progression (Fig. 2a). Interestingly, heterogeneous expression of PTEN (suggestive of sub-clonal loss of PTEN) was more frequent in more advanced stages of the disease (from 4% in stage I to 8% in stage IV; gCMH p value = 0.0187 for a Cochran–Armitage trend test) and subgroup analysis shows that this association is present only in the context of absent BRCA1/2 pathogenic mutation (see Supplementary Information). In contrast to our previous reported results, loss of PTEN expression was not an adverse prognostic factor and had a modest positive effect on overall survival (hazard ratio (HR) 0.78, 95% CI 0.65–0.94; p value = 0.022 after multiplicity correction; Fig. 2b and Supplementary Table 3). Similar results were obtained with sensitivity analyses controlling for CD8, ER, PR and AR independently or jointly, suggesting that the effect of PTEN is additional to the effect of these biomarkers.
a Mosaic plot corresponding to the association analysis between PTEN expression and stage of disease. b Kaplan–Meier survival curves for PTEN-negative, PTEN-positive, weak or heterogeneous staining for HGSOC from study cohort (multivariate hazard ratio 0.78, 95% CI 0.64–0.93, N = 1842, p = 0.0205 after multiplicity correction, when comparing PTEN negative vs PTEN positive). CI confidence interval. c Mosaic plot for the association between levels of CD8 expression and histotypes of ovarian cancer. Mosaic plots (d, e) summarise the association between PTEN expression and CD8 counts in CCOC and HGSOC, respectively. TIL tumour-infiltrating lymphocytes.
HGSOC and CCOC show distinct associations between PTEN expression and CD8 counts
In HGSOC, CD8 counts were higher than in any other histotype of ovarian cancer (Fig. 2c). In preclinical models of melanoma, loss of PTEN was associated with decreased intra-tumour T cells.4 In this study, higher levels of PTEN expression were associated with lower CD8 counts in CCOC (gCHM test p value < 0.0001 for an ordinal/ordinal association; Fig. 2d and Supplementary Table 4). The average CD8 count per cytoplasmic PTEN level was also different in HGSOC (gCHM test p value = 0.0052 for a nominal/ordinal association, Fig. 2e and Supplementary Table 4). More strikingly, heterogeneous expression of PTEN in HGSOC (suggestive of sub-clonal loss of PTEN) was associated with significantly higher CD8 counts (gCHM test p value = 0.0016 for a binary/ordinal association corresponding to Cochrane–Armitage trend test; Fig. 2e).
PTEN expression was strongly associated with AR, ER and PR expression in HGSOC
In ENOC, PTEN loss was more prevalent in younger (<50 years) than in older patients (gCHM test p value < 0.0001 for an ordinal/ordinal association; Supplementary Table S3 and Fig. 3a), and this was likely related to the previously described hormonal regulation of PTEN expression. We also found that PTEN expression was strongly and positively associated with expression of ER, PR and AR in HGSOC (Supplementary Table 4; Fig. 3b–d).
Discussion
The standard treatment of ovarian cancer has remained the same for the past two decades since the introduction of taxanes to platinum-based therapies, with very modest improvements in survival that are most likely related to improvements in supportive care. In order to define better therapeutic strategies, it is crucial to accurately describe the prevalence of common drivers and how they associate with clinical features and biomarkers of actionable pathways.2
Our large study of 5400 patients with ovarian cancer showed that complete loss of PTEN is highly prevalent across different histotypes of ovarian cancer ranging from 11% in LGSOC and 35% in CCOC, suggesting that it may be a driver of the disease. A small number of molecular alterations are generally sufficient to drive tumour initiation and progression.26 As HGSOC and its pre-cancerous lesions in the fallopian tubes have highly complex genomes27,28,29 and there is marked heterogeneity between patients, the identification of important drivers is challenging. Our results show a similar frequency of complete PTEN loss across all stages of HGSOC, which is consistent with loss of PTEN as a common early step in the progression of HGSOC. In BRCA1-associated breast cancer, which has molecular similarities with HGSOC (e.g., genomic instability, chromosomal complexity, frequent TP53, BRCA1 and BRCA2 mutation), PTEN loss was also the most frequent initiating event.18 Interestingly, we found here that the frequency of HGSOC cases with heterogeneous expression of PTEN (suggestive of a later sub-clonal loss of PTEN) is higher in more advanced disease in patients without any confirmed pathogenic BRCA1/2 mutation. As stage is a surrogate for increased tumour mass, this suggests that PTEN loss confers a proliferative advantage to tumour cells and is positively selected over HGSOC cell expansion. PTEN loss is also one of the most frequent hits for increased cell viability in CRISPR screens.30 Considering the role of the PI3K pathway in the regulation of genomic stability, it is difficult to ascertain if loss of PTEN by chromosomal deletion is a result of baseline genomic instability or if it influences the latter.31 Therefore, despite the clinical and pathological associations we presented, it remains inconclusive if loss of PTEN is a driver of the disease initiation or progression. Previous evidence of PTEN loss in early pre-cancer lesions in the fallopian tubes,25 its role in the mouse models of HGSOC12,13,14 and high focal prevalence of PTEN loss compared to other neighbouring genes (Gistic p value for the likelihood of PTEN loss being a driver: 7.3e−17)11,32 in HGSOC are supportive of the role of PTEN loss in driving progression in HGSOC. Whole-genome characterisation of chemoresistant ovarian tumours also suggested that gene breakage of PTEN and other tumour-suppressor genes also contributes to chemoresistance.33
The majority of ENOC arise from malignant transformation of endometriosis, suggesting that pathways involved in the transformation of this ectopic endometrium into ENOC may overlap with the processes involved in the progression from normal endometrium to endometrial cancer.34 In this context, PTEN loss is commonly lost in the normal endometrium.35 In our study, the frequency of PTEN loss in ENOC was significantly higher in younger premenopausal patients whose higher levels of oestradiol and progesterone induce higher expression and phosphorylation of PTEN in the endometrium.5 This suggests that deletion of PTEN is therefore more likely to be positively selected and to provide a proliferative advantage in the context of a surrounding endometrium with upregulated PTEN than within the endometrium of older postmenopausal patient where lower hormonal levels already condition lower levels of PTEN expression. In this context, we found a strong association between expression of hormonal receptors (AR, ER and PR) and PTEN expression in HGSOC. Activity of the PTEN/PI3K pathway has also been associated with AR expression in prostate cancer,20,36 and mouse models suggest that a functional AR may increase PTEN inactivation-induced uterine cancer.37 These data suggest that PTEN inactivation is positively selected by functional androgen activity in these tumour types.
In a previous study, we found in two smaller cohorts that cases with any type of loss of PTEN expression was associated with shorter overall survival. Although this association was significant, the confidence intervals were relatively wide (N = 439; HR 1.5, 95% CI 1.1–2.0).15 In this much larger cohort, the frequency of loss was similar, but there was an opposite prognostic signal, reinforcing the need to use large cohorts for validation of putative prognostic biomarkers. The association between PTEN negative expression in HGSOC and longer overall survival (HR 0.78 95% CI 0.64–0.93) is counterintuitive considering that activation of the PI3K pathway is generally associated with proliferation and more aggressive tumours. We speculate that further genetic interactions may be important in determining survival. For instance, if PTEN loss appears stochastically in the context of existing homologous recombination deficiency, accelerated proliferation on a background chromosomal instability may increase genomic crisis and cell death. In addition, loss of PTEN may have treatment interactions particularly with platinum-based chemotherapy as higher proliferation and genomic instability predict better response.38
A multi-omics approach also demonstrated that immune-infiltrate of cytotoxic T cells can be recruited to the tumour by cytokines derived from the activation of the DNA damage response protein ATM in tumours that are genomically unstable and therefore enriched for chromosomal copy number alterations (CNAs),39 supporting previous associations between BRCA-like HGSOC (characterised by homologous recombination deficiency) and immune infiltrates.11,40 In previous studies, CD8 counts were indeed highest in HGSOC (the ovarian cancer histotype with higher prevalence of CNAs) as compared to other histotypes, and higher CD8 counts were associated with longer survival in HGSOC and ENOC.16 Despite the associations we found between expression of PTEN and CD8 counts in HGSOC, they seem to have opposite effects on survival. More specifically, PTEN loss and higher CD8 counts seem to have positive effects on prognosis, which may be explained by their association with CNA-enriched, genomically unstable tumours. This is further supported by the fact that the highest CD8 counts were found in tumours with heterogeneous expression of PTEN (and likely late sub-clonal loss of PTEN).
Preclinical murine models of melanoma suggest that PTEN loss promotes resistance to T cell-mediated immunotherapy by decreasing T cell trafficking into the tumours.4 Moreover, trials of PI3Kbeta inhibitor in this model improved the efficacy of both anti-PD-1 and anti-CTLA-4 antibodies. Recent in silico and IHC analysis of human prostate tumours showed that PTEN loss in primary prostate tumours was also associated with lower CD8+ TIL counts and an immunosuppressive tumour environment mediated by infiltrating FoxP3+ T cells.41 However, in the same study, PTEN-deficient metastasis to the lymph nodes showed increased counts of CD8+ T cells. Interestingly, these opposite associations are also demonstrated in our study, since PTEN loss was associated with low counts of CD8+ T cells in HGSOC cases and high counts in CCOC cases, supporting the hypothesis that not only PI3K activation may influence recruitment of cytotoxic T cells but also that these processes may be distinctly regulated in different subtypes of ovarian cancer.
PTEN loss is known to preferentially activate the PI3Kbeta subunit and we show that PTEN loss is a common event in all types of ovarian cancer and can appear in the context of chromosomal instability in HGSOC. These results suggest that combinations of small molecule inhibitors targeting the PI3K/AKT/mammalian target of rapamycin pathway (including inhibitors of the beta subunit), poly ADP-ribose polymerase or apoptotic pathways may have effective results in cases of HGSOC in the clinical setting. Preclinical studies using combinations of those agents have already shown promising results.42,43,44 Moreover, the associations we found between expression of PTEN and hormonal receptors suggest that molecular stratification based on expression of PTEN and hormonal receptors may be informative for tumours that are more likely to respond to hormonal therapies (high expression of PTEN and hormonal receptors) and those that could be preferentially treated with PI3Kbeta inhibitors (low expression of PTEN and hormonal receptors). Finally, future validation in primary cells from patients to assess if and how PTEN regulates recruitment of cytotoxic T cells may inform how the drug combinations above can be used to improve immunotherapy results. In summary, this work will inform future trials in ovarian cancer using combinations of immunotherapy and other targeted therapies and suggests that profiling for PTEN expression should also be done in the context of those trials.
References
Vaughan, S., Coward, J. I., Bast, R. C. Jr., Berchuck, A., Berek, J. S., Brenton, J. D. et al. Rethinking ovarian cancer: recommendations for improving outcomes. Nat. Rev. Cancer 11, 719–725 (2011).
Bowtell, D. D., Bohm, S., Ahmed, A. A., Aspuria, P. J., Bast, R. C. Jr., Beral, V. et al. Rethinking ovarian cancer II: reducing mortality from high-grade serous ovarian cancer. Nat. Rev. Cancer 15, 668–679 (2015).
Lee, Y. R., Chen, M. & Pandolfi, P. P. The functions and regulation of the PTEN tumour suppressor: new modes and prospects. Nat. Rev. Mol. Cell Biol. 19, 547–562 (2018).
Peng, W., Chen, J. Q., Liu, C., Malu, S., Creasy, C., Tetzlaff, M. T. et al. Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov. 6, 202–216 (2016).
Guzeloglu-Kayisli, O., Kayisli, U. A., Al-Rejjal, R., Zheng, W., Luleci, G. & Arici, A. Regulation of PTEN (phosphatase and tensin homolog deleted on chromosome 10) expression by estradiol and progesterone in human endometrium. J. Clin. Endocrinol. Metab. 88, 5017–5026 (2003).
McConechy, M. K., Ding, J., Senz, J., Yang, W., Melnyk, N., Tone, A. A. et al. Ovarian and endometrial endometrioid carcinomas have distinct CTNNB1 and PTEN mutation profiles. Mod. Pathol. 27, 128–134 (2014).
Obata, K., Morland, S. J., Watson, R. H., Hitchcock, A., Chenevix-Trench, G., Thomas, E. J. et al. Frequent PTEN/MMAC mutations in endometrioid but not serous or mucinous epithelial ovarian tumors. Cancer Res. 58, 2095–2097 (1998).
Sato, N., Tsunoda, H., Nishida, M., Morishita, Y., Takimoto, Y., Kubo, T. et al. Loss of heterozygosity on 10q23.3 and mutation of the tumor suppressor gene PTEN in benign endometrial cyst of the ovary: possible sequence progression from benign endometrial cyst to endometrioid carcinoma and clear cell carcinoma of the ovary. Cancer Res. 60, 7052–7056 (2000).
Kurman, R. J. & Shih, Ie. M. Molecular pathogenesis and extraovarian origin of epithelial ovarian cancer–shifting the paradigm. Hum. Pathol. 42, 918–931 (2011).
Hauke, J., Hahnen, E., Schneider, S., Reuss, A., Richters, L., Kommoss, S. et al. Deleterious somatic variants in 473 consecutive individuals with ovarian cancer: results of the observational AGO-TR1 study (NCT02222883). J. Med. Genet. 56, 574–580 (2019).
Cancer Genome Atlas Research Network. Integrated genomic analyses of ovarian carcinoma. Nature 474, 609–615 (2011).
Kim, J., Coffey, D. M., Creighton, C. J., Yu, Z., Hawkins, S. M. & Matzuk, M. M. High-grade serous ovarian cancer arises from fallopian tube in a mouse model. Proc. Natl Acad. Sci. USA 109, 3921–3926 (2012).
Perets, R., Wyant, G. A., Muto, K. W., Bijron, J. G., Poole, B. B., Chin, K. T. et al. Transformation of the fallopian tube secretory epithelium leads to high-grade serous ovarian cancer in Brca;Tp53;Pten models. Cancer Cell 24, 751–765 (2013).
Dinulescu, D. M., Ince, T. A., Quade, B. J., Shafer, S. A., Crowley, D. & Jacks, T. Role of K-ras and Pten in the development of mouse models of endometriosis and endometrioid ovarian cancer. Nat. Med. 11, 63–70 (2005).
Martins, F. C., Santiago, I., Trinh, A., Xian, J., Guo, A., Sayal, K. et al. Combined image and genomic analysis of high-grade serous ovarian cancer reveals PTEN loss as a common driver event and prognostic classifier. Genome Biol. 15, 526 (2014).
Goode, E. L., Block, M. S., Kalli, K. R., Vierkant, R. A., Chen, W., Fogarty, Z. C. et al. Dose-response association of CD8+ tumor-infiltrating lymphocytes and survival time in high-grade serous ovarian cancer. JAMA Oncol. 3, e173290 (2017).
Sieh, W., Kobel, M., Longacre, T. A., Bowtell, D. D., deFazio, A., Goodman, M. T. et al. Hormone-receptor expression and ovarian cancer survival: an Ovarian Tumor Tissue Analysis Consortium study. Lancet Oncol. 14, 853–862 (2013).
Martins, F. C., De, S., Almendro, V., Gonen, M., Park, S. Y., Blum, J. L. et al. Evolutionary pathways in BRCA1-associated breast tumors. Cancer Discov. 2, 503–511 (2012).
Agresti, A. Categorical Data Analysis (John Wiley & Sons, 2002).
Carver, B. S., Chapinski, C., Wongvipat, J., Hieronymus, H., Chen, Y., Chandarlapaty, S. et al. Reciprocal feedback regulation of PI3K and androgen receptor signaling in PTEN-deficient prostate cancer. Cancer Cell 19, 575–586 (2011).
Buuren, S. V. Flexible Imputation of Missing Data (Chapman & Hall/CRC, 2012).
Bretz, F., Hothorn, T. & Westfall, P. Multiple Comparisons Using R (Chapman & Hall/CRC, 2010).
Landis, J. R. & Koch, G. G. The measurement of observer agreement for categorical data. Biometrics 33, 159–174 (1977).
Shen, W. H., Balajee, A. S., Wang, J., Wu, H., Eng, C., Pandolfi, P. P. et al. Essential role for nuclear PTEN in maintaining chromosomal integrity. Cell 128, 157–170 (2007).
Roh, M. H., Yassin, Y., Miron, A., Mehra, K. K., Mehrad, M., Monte, N. M. et al. High-grade fimbrial-ovarian carcinomas are unified by altered p53, PTEN and PAX2 expression. Mod. Pathol. 23, 1316–1324 (2010).
Tomasetti, C., Marchionni, L., Nowak, M. A., Parmigiani, G. & Vogelstein, B. Only three driver gene mutations are required for the development of lung and colorectal cancers. Proc. Natl Acad. Sci. USA 112, 118–123 (2015).
Eckert, M. A., Pan, S., Hernandez, K. M., Loth, R. M., Andrade, J., Volchenboum, S. L. et al. Genomics of ovarian cancer progression reveals diverse metastatic trajectories including intraepithelial metastasis to the fallopian tube. Cancer Discov. 6, 1342–1351 (2016).
Labidi-Galy, S. I., Papp, E., Hallberg, D., Niknafs, N., Adleff, V., Noe, M. et al. High grade serous ovarian carcinomas originate in the fallopian tube. Nat. Commun. 8, 1093 (2017).
Gorringe, K. L., Jacobs, S., Thompson, E. R., Sridhar, A., Qiu, W., Choong, D. Y. et al. High-resolution single nucleotide polymorphism array analysis of epithelial ovarian cancer reveals numerous microdeletions and amplifications. Clin. Cancer Res. 13, 4731–4739 (2007).
Chow, R. D., Guzman, C. D., Wang, G., Schmidt, F., Youngblood, M. W., Ye, L. et al. AAV-mediated direct in vivo CRISPR screen identifies functional suppressors in glioblastoma. Nat. Neurosci. 20, 1329–1341 (2017).
Berenjeno, I. M., Pineiro, R., Castillo, S. D., Pearce, W., McGranahan, N., Dewhurst, S. M. et al. Oncogenic PIK3CA induces centrosome amplification and tolerance to genome doubling. Nat. Commun. 8, 1773 (2017).
Gao, J., Aksoy, B. A., Dogrusoz, U., Dresdner, G., Gross, B., Sumer, S. O. et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 6, pl1 (2013).
Patch, A. M., Christie, E. L., Etemadmoghadam, D., Garsed, D. W., George, J., Fereday, S. et al. Whole-genome characterization of chemoresistant ovarian cancer. Nature 521, 489–494 (2015).
Pearce, C. L., Templeman, C., Rossing, M. A., Lee, A., Near, A. M., Webb, P. M. et al. Association between endometriosis and risk of histological subtypes of ovarian cancer: a pooled analysis of case-control studies. Lancet Oncol. 13, 385–394 (2012).
Suda, K., Nakaoka, H., Yoshihara, K., Ishiguro, T., Tamura, R., Mori, Y. et al. Clonal expansion and diversification of cancer-associated mutations in endometriosis and normal endometrium. Cell Rep. 24, 1777–1789 (2018).
Mulholland, D. J., Tran, L. M., Li, Y., Cai, H., Morim, A., Wang, S. et al. Cell autonomous role of PTEN in regulating castration-resistant prostate cancer growth. Cancer Cell 19, 792–804 (2011).
Choi, J. P., Desai, R., Zheng, Y., Yao, M., Dong, Q., Watson, G. et al. Androgen actions via androgen receptor promote PTEN inactivation induced uterine cancer. Endocr. Relat. Cancer 22, 687–701 (2015).
Dillon, L. M. & Miller, T. W. Therapeutic targeting of cancers with loss of PTEN function. Curr. Drug Targets 15, 65–79 (2014).
McGrail, D. J., Federico, L., Li, Y., Dai, H., Lu, Y., Mills, G. B. et al. Multi-omics analysis reveals neoantigen-independent immune cell infiltration in copy-number driven cancers. Nat. Commun. 9, 1317 (2018).
Press, J. Z., De Luca, A., Boyd, N., Young, S., Troussard, A., Ridge, Y. et al. Ovarian carcinomas with genetic and epigenetic BRCA1 loss have distinct molecular abnormalities. BMC Cancer 8, 17 (2008).
Vidotto, T., Saggioro, F. P., Jamaspishvili, T., Chesca, D. L., Picanco de Albuquerque, C. G., Reis, R. B. et al. PTEN-deficient prostate cancer is associated with an immunosuppressive tumor microenvironment mediated by increased expression of IDO1 and infiltrating FoxP3+ T regulatory cells. Prostate 79, 969–979 (2019).
Zhang, J., Gao, X., Schmit, F., Adelmant, G., Eck, M. J., Marto, J. A. et al. CRKL mediates p110beta-dependent PI3K signaling in PTEN-deficient cancer cells. Cell Rep. 20, 549–557 (2017).
Zervantonakis, I. K., Iavarone, C., Chen, H. Y., Selfors, L. M., Palakurthi, S., Liu, J. F. et al. Systems analysis of apoptotic priming in ovarian cancer identifies vulnerabilities and predictors of drug response. Nat. Commun. 8, 365 (2017).
Philip, C. A., Laskov, I., Beauchamp, M. C., Marques, M., Amin, O., Bitharas, J. et al. Inhibition of PI3K-AKT-mTOR pathway sensitizes endometrial cancer cell lines to PARP inhibitors. BMC Cancer 17, 638 (2017).
Author information
Authors and Affiliations
Contributions
F.C.M., R.C., M.J.L., S.D., D.H., M.K., S.R., P.D.P.P. and J.D.B. designed, established and supervised the study. F.C.M., R.C. and J.D.B. obtained funding for the work. F.C.M. performed the laboratory work related to PTEN staining and F.C.M. and A.P. scored the cores. C.C. performed the laboratory work related to AR staining and A.N.K. and T.M.N. scored the cores. F.C.M., D.-L.C., P.D.P.P. and J.D.B. performed the data analysis and have drafted the manuscript; D.-L.C., supervised by P.D.P.P., led the statistical analysis and developed the R code presented as Supplementary Material. F.C.M., D.-L.C., A.P., A.N.K., C.C., T.M.N., A.O., A.G.-M., A.V., A.H., A.T., A.O., A.D.H., A.B.-W., A.D.F., A.F., A.H., B.Y.H., B.M.M., C.K., C.B.S., C.H., D.G.T., E.H., F.A.T., F.M., G.K., G.N., H. Steed, H. Song, H.L., J.B., J.A., J.M.K., J.L., J.H.R., J.M.d.A., L.L., L.P.-A., L.R.-D., L.R.W., M.J.G., M.P.I., M.-L.A., M.A.B., M.W.B., M.J.-L., M.A., M.E.C., M.S., N.T., N.P., N.S., N.L., P.S., P.G., R. Erber, R. Edwards, R.V., R.B.N., S.L., S.O., S.Y.B., S.K., S.F., S.G., S.J.W., S.K., T.P., T.A.L., V.M.G., V.R., W.S., Y.B.S., A.S.W., A.S., B.Y.K., C.R.-A., D.D.B., E.L.G., E.H., F.J.C.d.R., J.G., J.C.-C., K.B.M., L.E.K., L.S.C., M.T.G., P.A.F., R.C., S.D., U.M., D.G.H., M.K., S.J.R., P.D.P.P. and J.D.B. have contributed for the acquisition of data and materials, have critically revised the manuscript, have approved the published version and agreed to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the Declaration of Helsinki. All institutions participating in the Ovarian Tumour Tissue Analysis Consortium got institutional review board/ethics board approval. In most studies, patients consented to participate. In five studies, the need for informed consent was waived by the ethics board (Supplementary Material).
Data availability
The R markdown document containing the entire data set and allowing for reproducing all analyses performed in this manuscript is available as supplementary files.
Competing interests
F.C.M. is a Clinical Lecturer for the Experimental Medicine Initiative from the University of Cambridge that is partly funded by AstraZeneca. A.P. was funded by NIHR (Academic Clinical Fellowship). A.D.F. has received a research grant from AstraZeneca, not directly to this work. D.D.B. receives funding from Astra Zeneca and Genentech Roche for the conduct of research studies and clinical trials unrelated to the work described in this article. D.G.H. is a founder and Chief Medical Officer of Contextual Genomics, a somatic mutation testing laboratory; the company’s work and interests do not overlap with the subject of and methodologies used in this article. U.M. has stock ownership and has received research funding from Abcodia. No other disclosures are reported. P.D.P.P. is a member of the British Journal Cancer Editorial Board. All other authors declare no competing interests.
Funding information
F.C.M. is funded by the Experimental Medicine Initiative from the University of Cambridge, by the Academy of Medical Sciences (SGL016_1084), Cancer Research UK (C53876/A24267) and by the Addenbrooke’s Charitable Trust (REF 13/17). Funding was provided by Canadian Institutes for Health Research (MOP-86727); Brazilian National Council for Scientific and Technological Development, grant No. 478416/2009-1; Calgary Laboratory Services Internal Research Competition RS10-533; German Federal Ministry of Education and Research of Germany (01 GB 9401); German Cancer Research Center (DKFZ); US National Cancer Institute K07-CA80668, P50-CA159981, R01CA095023; National Institutes of Health/National Center for Research Resources/General Clinical Research Center grant MO1-RR000056; US Army Medical Research and Materiel Command DAMD17-02-1-0669; NIH (R01-CA122443, P50-CA136393, P30-CA15083, U01-CA71966, U01-CA69417, R01-CA16056, K07-CA143047); Cancer Research UK (C490/A10119, C490/A10123, C490/A16561); UK National Institute for Health Research Biomedical Research Centres at the University of Cambridge and at University College Hospital, ‘Women’s Health Theme’; NIH SFB 685; the Eve Appeal; the Oak Foundation and Deutsche Forschungsgemein-schaft. The Australian Ovarian Cancer Study Group was supported by the US Army Medical Research and Materiel Command under DAMD17-01-1-0729; The Cancer Council Victoria; Queensland Cancer Fund; The Cancer Council, New South Wales; the Tom Baker Cancer Centre Translational Laboratories; The Cancer Council, South Australia; The Cancer Foundation of Western Australia; The Cancer Council Tasmania and the National Health and Medical Research Council of Australia (NHMRC; ID400413, ID400281). The AOCS gratefully acknowledges additional support from the Peter MacCallum Cancer Foundation and Ovarian Cancer Australia (OCA). The Gynaecological Oncology Biobank at Westmead, a member of the Australasian Biospecimen Network-Oncology group, was funded by the National Health and Medical Research Council Enabling grants ID 310670 and ID 628903 and the Cancer Institute NSW grants 12/RIG/1-17 and 15/RIG/1-16. Funding for MALOVA was provided by research grant R01-CA61107 from the National Cancer Institute, Bethesda, Maryland; research grant 94 222 52 from the Danish Cancer Society, Copenhagen, Denmark and the Mermaid I project. A.D.F. is funded by Cancer Institute NSW grant 15/TRC/1-01. B.Y.K. is funded by the American Cancer Society Early Detection Professorship (SIOP-06-258-01-COUN) and the National Center for Advancing Translational Sciences (NCATS), grant UL1TR000124. The samples from the German Ovarian Cancer Study were provided by the tissue bank of the National Center for Tumor Diseases (NCT, Heidelberg, Germany) in accordance with the regulations of the tissue bank and the approval of the ethics committee of Heidelberg University. F.J.C.d.R. is funded by the Brazilian National Council for Scientific and Technological Development – CNPq (427983/2016-9, 303210/2018-4). The UKOPS study was funded by The Eve Appeal (The Oak Foundation) with investigators supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre. A.T. is funded through a Michael Smith Foundation for Health Research Scholar Award. M.A. is funded through a Michael Smith Foundation for Health Research Scholar Award and the Janet D. Cottrelle Foundation Scholars programme managed by the BC Cancer Foundation. D.G.H. receives support from the Dr. Chew Wei Memorial Professorship in Gynecologic Oncology and the Canada Research Chairs programme (Research Chair in Molecular and Genomic Pathology). OVCARE (including the VAN study) receives support through the BC Cancer Foundation and The VGH + UBC Hospital Foundation (relevant for authors A.T., D.G.H, S.L., C.C., A.N.K., and M.A.). J.D.B. acknowledges funding and support from Cancer Research UK (grant numbers A22905, A15601 and A17197). The funding sources had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript and decision to submit the manuscript for publication.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Martins, F.C., Couturier, DL., Paterson, A. et al. Clinical and pathological associations of PTEN expression in ovarian cancer: a multicentre study from the Ovarian Tumour Tissue Analysis Consortium. Br J Cancer 123, 793–802 (2020). https://doi.org/10.1038/s41416-020-0900-0
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41416-020-0900-0
This article is cited by
-
Pten knockout affects drug resistance differently in melanoma and kidney cancer
Pharmacological Reports (2023)
-
Regulation of PTEN and ovarian cancer progression by an E3 ubiquitin ligase RBCK1
Human Cell (2022)
-
Influence of interdisciplinary frailty screening on perioperative complication rates in elderly ovarian cancer patients: results of a retrospective observational study
Archives of Gynecology and Obstetrics (2022)
-
BCL2L1 is identified as a target of naringenin in regulating ovarian cancer progression
Molecular and Cellular Biochemistry (2022)