Abstract
Aims Since it is known that oral problems affect various medical diseases, the effects of restrictions on visits for dental treatment on exacerbations of various systemic medical diseases were examined.
Method and materials The data were used from the Japan COVID-19 and Society Internet Survey, a large-scale internet survey conducted in 2021 (n = 28,175). The questionnaires were distributed to 33,081 candidates who were selected to represent the Japanese population regarding age, sex and residential prefecture using a simple random sampling procedure. Patients currently undergoing treatment for diabetes mellitus, hypertension, asthma, cardiocerebrovascular disease, hyperlipidemia, atopic dermatitis, and mental illness, such as depression, were extracted from the total participants. Then, whether discontinuation of dental treatment affected the exacerbation of their systemic disease was examined.
Results Overall, 50-60% of patients with each systemic disease had continued to receive dental treatment, and 4-8% of them had discontinued dental treatment. On univariate and multivariate analyses, discontinuation of dental treatment is a risk factor in the exacerbation of diabetes mellitus, hypertensive conditions, asthma, cardiocerebrovascular disease and hyperlipidemia.
Conclusion The present epidemiological study showed the relationship between oral health and systemic health, which can provide meaningful insights regarding future medical-dental collaboration in Japan.
Key points
-
Discontinuation of dental treatment is a risk factor for the exacerbation of diabetes mellitus, hypertensive conditions, asthma, cardiocerebrovascular disease and hyperlipidemia.
-
Dental check-ups and treatment could prevent worsening of systemic diseases.
-
Understanding the relationship between oral health and systemic health could provide meaningful insights for medical-dental collaboration.
Similar content being viewed by others
Introduction
Oral diseases, especially periodontal disease, are associated with various systemic diseases. The association, for example, between periodontal disease and diabetes mellitus, has been well-evidenced. Diabetes mellitus is a metabolic disease caused by abnormal glucose metabolism and it is known to affect many patients in Japan.1 Periodontal disease has been widely recognised as a major complication of diabetes mellitus and many epidemiological studies have shown that diabetic patients have a higher tendency to develop periodontal disease. In addition, periodontal dental treatment in diabetic patients with periodontal disease improves the control of the diabetes mellitus, suggesting that there is a bidirectional relationship.2 Moreover, it has been reported that periodontal disease is associated with various other systemic diseases, such as heart disease, chronic kidney disease, and hypertension, although some of these associations have insufficient evidence.3,4,5,6,7
The Japan COVID-19 and Society Internet Survey (JACSIS) was a survey of the actual conditions of residents' lives, health and social and economic activities, including the issue of COVID-19. The purpose of this survey was to provide information to plan and implement realistic measures for socioeconomic relief and health promotion for 'protecting and promoting health and social activities'. This survey took a sample that matched the population distribution of Japan. The aspects evaluated included items related to consultations and medical conditions for various medical diseases, including oral diseases. These data clarify the general health status of the Japanese people.
Due to measures imposed to mitigate SARS-CoV-2 infection, social activities were restricted in Japan, and as a result, various health concerns have surfaced. With regard to these restrictions, problems of refraining from dental treatment have also arisen. Since it is known that oral problems affect various medical diseases, the effects of restrictions on visits for dental treatment on exacerbations of various systemic medical diseases were examined using JACSIS data (n = 28,175).
Materials and methods
Study participants and setting
A cross-sectional study was conducted by analysing data from the JACSIS study. The ethics committee of Osaka International Cancer Institute approved the study protocol (approval number: 20084). From 27 September 2021 to 30 October 2021, questionnaires were distributed to 33,081 candidates who were selected from the panellists of a Japanese internet research company (Rakuten Insight, Inc) to represent the Japanese population regarding age, sex and residential prefecture using a simple random sampling procedure. All participants provided web-based informed consent at registration. Respondents who had provided invalid responses to the questionnaire were excluded and the data of 27,185 respondents (age range: 15-79 years; 49.7% male) were included in the analysis.
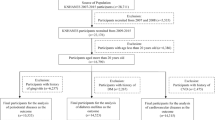
Patients currently undergoing treatment for diabetes mellitus, hypertension, asthma, cardiocerebrovascular disease, hyperlipidemia, atopic dermatitis, and mental illness, such as depression, were picked from the total participants. Then, whether their systemic disease worsened was examined. For instance, Figure 1 shows the participant extraction process for diabetes mellitus.
From all 28,175 participants, 1,999 people with current diabetes mellitus were picked up. Of these 1,999 people, those who had not received medical treatment because of their neglected disease were excluded. The 1,802 people who were currently receiving medical treatment were picked up and of the 1,802 people currently with diabetes mellitus, those who had interrupted and discontinued diabetes treatment in the last two months were excluded. Thus, 1,719 people who were able to continue diabetes treatment were picked up. These 1,719 people were analysed as the final verified subjects.
Then, whether their diabetes mellitus exacerbated between those who continued dental treatment and those who discontinued was examined epidemiologically. The survey asked the questions below regarding the underlying two behaviours:
-
1.
Has your systemic disease condition worsened in the last two months?
-
2.
Have you been able to have dental treatment within the last two months?
The answers for question one were 'yes, my disease condition worsened' or 'no, my disease condition has not worsened'. The answers for question two were 'yes, I have continued the dental treatment', 'no, I discontinued the dental treatment' and 'N/A (this question does not apply)'.
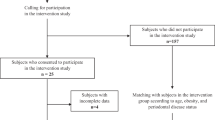
Subjects with hypertension, asthma, cardiocerebrovascular disease, hyperlipidemia, atopic dermatitis, and mental illness, such as depression, were extracted in the same manner as above. Of these final verified subjects, the exacerbation of each systemic disease condition was compared between those who continued to receive dental treatment and those who discontinued dental treatment. The outcome index used in this study was the respondents' exacerbation of each systemic disease condition. If an individual chose the answer 'my disease condition has worsened in the past two months', that individual was assigned to the exacerbation group, and this was used as the primary outcome variable. Next, explanatory variables were added. Model 1 was an initial crude model that examined the presence or absence of dental treatment as a univariate. Model 2 added age, sex, smoking and living alone or not as socioeconomic factors. Factors such as owning a home, educational background and income were added as economic factors in Model 3.
To compare the two groups, the Mann-Whitney U test and the chi-squared test were used for continuous variables and categorical variables, respectively. Data were collected and analysed with a combination of software packages (Microsoft Excel [Microsoft, Redmond, WA, USA], SigmaPlot [Systat Software, Palo Alto, CA, USA] and EZR [Saitama Medical Centre and Jichi Medical University, Saitama, Japan]). Results are reported as means ± standard deviation, unless otherwise indicated.
All procedures performed in this study were in accordance with the Ethical Guidelines for Medical and Health Research Involving Human Subjects of the Ministry of Health, Labour and Welfare, Government of Japan, and with the 1964 Helsinki Declaration and its later amendments.
Results
The final validated subjects examined in this study had diabetes mellitus (n = 1,719), hypertension (n = 5,130), asthma (n = 677), cardiocerebrovascular disease (n=833), hyperlipidemia (n = 2,998), atopic dermatitis (n = 792), and mental illness, such as depression (n=1,638). As shown in Table 1, 50-60% of patients with each disease had continued to receive dental treatment and 4-8% of them had discontinued dental treatment. The percentage of patients with worsening of their disease condition was higher in the group who discontinued dental treatment than in those who continued dental treatment for all diseases. The proportion of those with exacerbated conditions was high in atopic dermatitis and mental illness, accounting for more than 20%, whereas less than 5% of those with hypertension and hyperlipidemia showed exacerbation of the condition.
For diabetes mellitus, there were 1,719 final verified subjects (average age: 61.2 ± 14.8 years; 1,241 men, 478 women). Of these final verified subjects, 88 discontinued dental treatment in the last two months and 1,043 continued to receive dental treatment. There were 588 individuals who had no prior dental treatment. Of those who discontinued dental treatment, 16/88 (18.2%) had worsening diabetes mellitus, whereas 58/1,043 (5.6%) of those who continued dental treatment had worsening diabetes mellitus. Univariate analysis with Model 1 showed a significant difference (p <0.0001), suggesting that discontinuing dental treatment significantly affected the worsening of diabetes mellitus. The results of Models 2 and 3 (the multivariate analyses with socioeconomic factors added) are shown in Table 2 and the online Supplementary Information, respectively. In all Models, 1, 2 and 3, the presence or absence of dental treatment was a significant factor in the exacerbation of diabetes mellitus.
A similar analysis showed that 17/211 (8.1%) of those with hypertension who discontinued dental treatment had worsening of their hypertension condition, and of those who continued dental treatment, 76/3.126 (2.4%) had exacerbated hypertension. Univariate and multivariate analyses showed significant differences, suggesting that discontinuing dental treatment significantly affected the exacerbation of hypertensive conditions in Models 1, 2 and 3 (Table 2). The presence or absence of dental treatment was a significant factor related to the condition of hypertension.
Asthma, cardiocerebrovascular disease and hyperlipidemia were similarly examined in a similar manner. Significant differences were also observed in all models. The absence of dental treatment was a significant factor in the exacerbation of each disease. Conversely, in atopic dermatitis and mental illness, no significant difference was observed in all Models.
Discussion
This is the first epidemiological study to suggest that the discontinuation of dental treatment is a risk factor for worsening of various systemic diseases in Japan. This study showed whether discontinuation of dental treatment was related to worsening of seven systemic diseases within one research survey, showing the importance of continuation of dental treatment.
The outcome index used in the present study was exacerbation of systemic disease. Participants diagnosed with each systemic disease were assigned to the exacerbation and non-exacerbation groups and this was used as the primary outcome variable. Explanatory variables were added and analysed with socioeconomic factors. The observation period was from 27 September 2021 to 29 October 2021, which corresponded to the period of the fifth domestic COVID-19 pandemic surge in Japan.
In recent years, various reports have suggested that oral disease adversely affects systemic health, and that oral disease is strongly related to the health of the whole body has been found to be a reliable observation. Much useful information about the effects of periodontal disease on various systemic diseases, including diabetes mellitus, has permeated through the entire medical community. In addition, the relationship between oral disease and systemic diseases other than diabetes mellitus has also been reported, although the evidence is not yet clear.
Periodontal disease and systematic disease
There have been various reports of the relationships between periodontal disease and systemic diseases. A cross-sectional study of adult Japanese people showed that individual components of metabolic syndrome, including obesity, hypertension, lipid abnormalities and hyperglycaemia, were associated with periodontal diseases.8 A significant correlation has been reported between the severity of periodontal disease and the deterioration of hemoglobin A1c (HbA1c), and its subanalysis showed that this association was more pronounced in subjects with high-sensitivity C-reactive protein (CRP) levels >1.0 mg/L. It has been suggested that the inflammatory reaction due to periodontal disease could be involved in the deterioration of HbA1c.9,10
The relationship between periodontal disease and coronary artery disease is currently receiving a great deal of attention. The leading cause of death in Japan is malignant neoplasm and the second and the fourth causes are heart disease and cerebrovascular disease, respectively. Cardiocerebrovascular diseases together account for about 25% of the total number of deaths in Japan each year. Recently, it has been reported that the enhancement of the systemic inflammatory response due to periodontal disease is involved in the onset and progression of vascular disorders.11 Histologically, Porphyromonas gingivalis has been shown to invade vascular endothelial cells12 and arteriosclerosis and periodontal diseases have common pathologies, such as elevations of inflammatory cytokines and CRP.13,14,15
Cariogenic bacteria and systemic disease
A study of the molecular basis linking Streptococcus mutans, which is a major cariogenic bacterium, to arteriosclerosis, has been reported. In a study that investigated the presence of oral bacteria in human atherosclerotic plaques using the polymerase chain reaction method, the detection rate of S. mutans was 74%.16 Another study also showed that S. mutans was detected in atherosclerotic plaques of 23% of young patients and 44% of elderly patients.17 In addition, it was confirmed that arterial endothelial cells invaded by oral streptococci produced an inflammatory cytokine (interleukin-6).18 These studies showed the relationship between metabolic syndrome, including hypertension and hyperlipidemia, and dental caries.
As mentioned above, it has been reported that the two major oral diseases, dental caries and periodontitis, are related to various lifestyle diseases in various studies. Thus, this makes the result of the present research, indicating that the discontinuation of dental treatment is a risk factor for worsening of diabetes mellitus, hypertension, hyperlipidemia and cardiocerebrovascular disease, to be believable. On the other hand, there are a few reports showing that periodontitis is related to asthma. The number of reports is very small compared to those reporting the relationships among diabetes mellitus, hypertension, hyperlipidemia, and cardiovascular and cerebrovascular disorders.19,20 Interestingly, the present results showed that the discontinuation of dental treatment was significantly related to exacerbation of asthma. We consider this is an important epidemiological result showing the relationship between dental treatment and asthma. Furthermore, there is a report showing no positive association between atopic dermatitis and periodontitis.21 The present study also showed no positive association between discontinuation of dental treatment and exacerbation of atopic dermatitis. Moreover, no positive association between discontinuation of dental treatment and exacerbation of mental illness, such as depression, was similarly shown.
The present study has limitations. Firstly, given the cross-sectional study design, the temporality between variables is not guaranteed. It is difficult to elucidate the causal relationship between the discontinuation of dental treatment and worsening of systemic diseases. Secondly, although participants were recruited to represent the Japanese population in terms of age, sex and residential prefecture, the respondents of a web-based survey might not fully represent the Japanese population, using self-reported information. The survey was developed to cover broad topics rather than focusing on dental health-related issues, which led to some difficulties. The observation period was from 27 September 2021 to 29 October 2021, which corresponded to the period of the third, fourth and fifth domestic COVID-19 pandemic surges in Japan. We could not capture the perfect data of all the participants at the time of the survey. Thus, the association between oral health and systemic health might be underestimated. In the general population, it is difficult to set up prospective studies of situations in which dental treatment is interrupted. The present study showed a very important result because it verified how people's health deteriorates due to the social activity restriction in the presence of COVID-19 infection, when oral dental care was not available. This study showed that discontinuing dental treatment worsened several systemic diseases. The key concept underlying the integrated common risk approach is that the promotion of general health by controlling a small number of risk factors may have a major impact on a large number of diseases at a lower cost and greater efficacy and effectiveness than disease-specific approaches.22 Specific dental check-ups and treatment could be demonstrated to be effective for the early detection and treatment of oral diseases. Therefore, dental treatment could prevent worsening of systemic diseases. The present epidemiological study showed the relationship between oral health and systemic health, and this is believed to provide meaningful insights regarding future medical-dental collaboration in Japan.
Conclusion
The presence or absence of dental treatment was a significant factor in the exacerbation of diabetes mellitus, hypertensive conditions, asthma, cardiocerebrovascular disease and hyperlipidemia. The present epidemiological study showed the relationship between oral health and systemic health, which can provide meaningful insights regarding future medical-dental collaboration in Japan.
References
Kawabata Y, Ekuni D, Miyai H et al. Relationship Between Prehypertension/Hypertension and Periodontal Disease: A Prospective Cohort Study. Am J Hypertens 2016; 29: 388-396.
Salvi G E, Carollo-Bittel B, Lang N P. Effects of diabetes mellitus on periodontal and peri-implant conditions: update on associations and risks. J Clin Periodontol 2008; 35: 398-409.
Sharma P, Fenton A, Dias I H K et al. Oxidative stress links periodontal inflammation and renal function. J Clin Periodontol 2021; 48: 357-367.
D'Aiuto F, Sabbah W, Netuveli G et al. Association of the metabolic syndrome with severe periodontitis in a large U S. population-based survey. J Clin Endocrinol Metab 2008; 93: 3989-3994.
Del Pinto R, Pietropaoli D, Munoz-Aguilera E et al. Periodontitis and Hypertension: Is the Association Causal? High Blood Press Cardiovasc Prev 2020; 27: 281-289.
Muñoz Aguilera E, Suvan J, Orlandi M, Miró Catalina Q, Nart J, D'Aiuto F. Association Between Periodontitis and Blood Pressure Highlighted in Systemically Healthy Individuals: Results From a Nested Case-Control Study. Hypertension 2021; 77: 1765-1774.
Van Dyke T E, Kholy K E, Ishai A et al. Inflammation of the periodontium associates with risk of future cardiovascular events. J Periodontol 2021; 92: 348-358.
Morita T, Ogawa Y, Takada K et al. Association between periodontal disease and metabolic syndrome. J Public Health Dent 2009; 69: 248-253.
Demmer R T, Desvarieux M, Holtfreter B et al. Periodontal status and A1C change: longitudinal results from the study of health in Pomerania (SHIP). Diabetes Care 2010; 33: 1037-1043.
Demmer R T, Squillaro A, Papapanou P N et al. Periodontal infection, systemic inflammation, and insulin resistance: results from the continuous National Health and Nutrition Examination Survey (NHANES) 1999-2004. Diabetes Care 2012; 35: 2235-2242.
Nakajima T, Honda T, Domon H et al. Periodontitis-associated upregulation of systemic inflammatory mediator level may increase the risk of coronary heart disease. J Periodontal Res 2010; 45: 116-122.
Dorn B R, Dunn W A Jr, Progulske-Fox A. Invasion of human coronary artery cells by periodontal pathogens. Infect Immun 1999; 67: 5792-5798.
Nissen S E, Tuzcu E M, Schoenhagen P et al. Statin therapy, LDL cholesterol, C-reactive protein, and coronary artery disease. N Engl J Med 2005; 352: 29-38.
Ridker P M, Cannon C P, Morrow D et al. C-reactive protein levels and outcomes after statin therapy. N Engl J Med 2005; 352: 20-28.
Yamazaki K, Ohsawa Y, Itoh H et al. T-cell clonality to Porphyromonas gingivalis and human heat shock protein 60s in patients with atherosclerosis and periodontitis. Oral Microbiol Immunol 2004; 19: 160-167.
Nakano K, Inaba H, Nomura R et al. Detection of cariogenic Streptococcus mutans in extirpated heart valve and atheromatous plaque specimens. J Clin Microbiol 2006; 44: 3313-3317.
Kozarov E, Sweier D, Shelburne C, Progulske-Fox A, Lopatin D. Detection of bacterial DNA in atheromatous plaques by quantitative PCR. Microbes Infect 2006; 8: 687-693.
Nagata E, de Toledo A, Oho T. Invasion of human aortic endothelial cells by oral viridans group streptococci and induction of inflammatory cytokine production. Mol Oral Microbiol 2011; 26: 78-88.
Lopes M P, Cruz A A, Xavier M T et al. Prevotella intermedia and periodontitis are associated with severe asthma. J Periodontol 2020; 91: 46-54.
Arbes S J Jr, Matsui E C. Can oral pathogens influence allergic disease? J Allergy Clin Immunol 2011; 127: 1119-1127.
Tursas L, Ylipalosaari M, Sinikumpu S-P et al. Association between bleeding periodontal pockets and eczemas: Results of the Northern Finland Birth Cohort 1966. J Clin Periodontol 2022; 49: 591-598.
Shigan E N. Integrated programme for noncommunicable diseases prevention and control (NCD). World Health Stat Q 1988; 41: 267-273.
Funding
This work was supported by the Japan Society for the Promotion of Science KAKENHI Grants [grant numbers 18H03062 and 21H04856]. The findings and conclusions of this article are the sole responsibility of the authors and do not represent the official views of the research funders. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript
Author information
Authors and Affiliations
Contributions
Akifumi Enomoto, Atsushi-Doksa Lee, Takeshi Shimoide, Yuto Takada, Yasuhiro Kakiuchi and Takahiro Tabuchi: development of the research study and authorship of initial draft; Akifumi Enomoto and Takahiro Tabuchi: review and contribution to all subsequent drafts of the manuscripts.
Corresponding author
Ethics declarations
The authors declare that they have no conflicts of interest.
The present study was approved by the Bioethics Review Committee of Osaka International Cancer Institute, Japan (approval number: 20084). All participants provided web-based informed consent at registration.
Supplementary Information
Rights and permissions
About this article
Cite this article
Enomoto, A., Lee, AD., Shimoide, T. et al. Is discontinuation of dental treatment related to exacerbation of systemic medical diseases in Japan?. Br Dent J (2023). https://doi.org/10.1038/s41415-023-5690-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-5690-3