Abstract
Background Adult inpatients are at risk of developing oral health-related problems during their admission that may require input from their medical team. Doctors have minimal training in oral health which may lead to inappropriate diagnosis and management of oral conditions.
Aim The aim of this survey was to investigate the knowledge of junior doctors in managing oral health conditions in hospitalised patients.
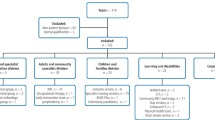
Method A survey was carried out with 146 junior doctors in Kent, Surrey and Sussex who attended oral health training sessions, which included scenario-based questions on diagnosis and management.
Results Ninety-two percent of doctors did not feel confident in diagnosing common oral conditions and 50% did not routinely assess the mouth as part of their overall health assessment. Of those surveyed, 97% expressed that they would like further training in oral health.
Conclusion There is a need to incorporate oral health training into the teaching programme for junior doctors to improve their confidence in the diagnosis and management of oral conditions. This would help improve the management of patients who develop oral problems during their hospital stay.
Similar content being viewed by others
Key points
-
Highlights that older patients in hospital are at risk of poor oral health.
-
Identifies that junior doctors do not feel confident in managing oral health conditions.
-
Suggests there may be a need to provide training in oral health for junior doctors.
Introduction
Doctors are regularly faced with patients that require management for conditions related to their oral cavity. Every year, approximately 600,000 consultations with a general medical practitioner are for patients with dental problems.1 Training and education in oral health for doctors, both at an undergraduate and postgraduate level, is extremely limited.2,3,4 Morgan et al.2 reported that doctors felt they had received insufficient training in examining patients' mouths and, as a result, a high proportion do not routinely carry out an oral assessment, despite the majority recognising the importance of doing so.
In hospitals, it is the responsibility of the medical team to provide first line management for inpatients with oral problems. The King's Fund found that the majority of hospital inpatients are over 75 years old, with the average age being over 80.5 Older patients are now more likely to retain their teeth due to positive changes in oral health over the last few decades. As a result, these patients may be at an increased risk of developing dental diseases that can impact on their overall health.6 Oral health problems are more likely to develop in older patients who make up a significant proportion of the inpatient population.7 Common oral conditions among the ageing population are: tooth loss, dental caries, periodontitis, xerostomia and acute candidiasis.8 Polypharmacy and systemic diseases such as diabetes can contribute to the development of these conditions, which can be debilitating for patients.9 In a hospitalised patient who may already be frail and unwell, oral symptoms can lead to difficulties eating, contributing to nutritional problems that inhibit overall recovery, and can also lead to a lower quality of life.10 Increasing age can also mean that patients are more likely to present with oral pain, soft or hard tissue lesions and oral cancer.11 There is increasing evidence of the links between oral health and systemic conditions including cardiovascular disease and diabetes.12,13
The Faculty of Dental Surgery at the Royal College of Surgeons England estimates that across England, Wales and Northern Ireland at least 1.8 million people aged 65 and over have an urgent dental condition such as dental pain, oral sepsis or extensive decay in untreated teeth.14 These figures suggest that older patients in hospitals may either have existing oral disease before admission, or may develop oral problems during their admission.
As hospitalised patients are at an increased risk of deteriorating oral health, it is important that doctors are aware of the signs and symptoms of common oral problems and how to manage them. Oral health improvement programmes for inpatients have tended to focus on upskilling nursing teams to provide good mouth care for inpatients, and have not specifically included training doctors.15,16
In 2015, Health Education England Kent, Surrey and Sussex developed 'Mouth Care Matters', a training and education programme to improve the oral health of inpatients.17 At the NHS acute trust where Mouth Care Matters was developed, a pathway was established to provide oral health advice for staff with regards to inpatients. Almost a quarter of the referrals in the first six months were from junior doctors for conditions such as dry mouth and suspected thrush, indicating there may be a gap in their knowledge of oral health.
The aim of this survey was to investigate whether the current cohort of junior doctors have had previous oral health training and to explore their confidence in managing common oral problems.
Method
An initial pilot survey was undertaken in order to explore the appropriate approach to obtaining the information required. This was carried out with a small group of ten foundation doctors at Surrey and Sussex Health Care Trust. Permission to conduct the study was granted by the Kent, Surrey and Sussex postgraduate dental dean. The research and development team at the pilot site, Surrey and Sussex Health Care Trust, was consulted and they advised ethical approval was not necessary as this was an educational survey.
Twelve acute NHS trusts in Kent, Surrey and Sussex were offered an oral health training session for junior doctors. Four medical education centres accepted the invitation and a one-hour training session was carried out by the same consultant in special care dentistry. At the start of the training session the doctors were invited to participate in a survey that included questions (Appendix 1) on:
Their previous oral health training
Whether they regularly assessed the oral cavity
How confident they felt in managing oral health problems
All information was recorded on individual anonymised data collection sheets.
The doctors were then shown a series of five photographs and provided with a short scenario for each (Table 1). They were asked to record their primary diagnosis and what would be their first line management based on the information provided. The scenarios were selected from patient cases that had been referred to the dental department at the Mouth Care Matters pilot trust in the previous six months, and consent to use these images had been obtained. Photographs were selected to represent the clinical case if they were not available. Four scenarios were of oral conditions more commonly seen in inpatients and one was an oral cancer case that had been referred to the dental unit that had developed an urgent referral pathway for hospital staff.
The survey sheets were collected after all scenarios had been provided. A teaching session then followed that included a discussion of the management of each of these cases.
Results
One hundred and forty six participants took part in the survey comprising of 75 female and 71 male foundation year one and two doctors. One of the doctors had previously studied dentistry and their data were not included in the results. Ninety percent of the doctors had qualified within the last three years, with 95% qualifying from a medical school in the United Kingdom.
Scenario one: poor oral hygiene
One third of the doctors correctly identified that the patient had a build-up of dental plaque on their teeth from the scenario and photograph provided. Thirty one percent were able to correctly advise that the plaque needed to be removed with improved oral hygiene. Twenty seven percent of the doctors, however, incorrectly diagnosed this as oral thrush and their primary management was to prescribe antifungal or antibiotic therapy. Seven percent said they would prescribe chlorhexidine as their first line treatment and 28% of the participants left this case unanswered. Four respondents suggested that the patient needed to have their teeth extracted.
Scenario two: dry tongue
Fifty seven percent of the doctors were able to identify that the patient most likely had a dry mouth from the clinical scenario and 14% said they would manage this with some form of dry mouth care. Thirty one percent said their primary diagnosis was glossitis or inflammation of the tongue, while 6% thought the appearance of the tongue was the result of an allergy. There was a range of primary treatment options including checking bloods (14%), administering vitamin B (13%), giving steroids (5%) and administering adrenaline (2%).
Scenario three: denture-related stomatitis
Fifty nine percent of the doctors diagnosed that the patient had a denture-related problem but only three out of 146 correctly diagnosed a fungal infection. Three percent of doctors said they would prescribe an antifungal medication and 5% advised they would recommend improved denture hygiene. Eight percent of the doctors thought the patient had ulcers on the palate. Nineteen percent responded that the first line management would be to advise them to see a dentist to have a new denture made, while 56% left the question unanswered.
Scenario four: ulcer
Eighty-two percent correctly diagnosed an ulcer from the scenario. The most common response for management was to prescribe a topical treatment of a well-known brand of anaesthetic gel (25%), followed by chlorhexidine (8%). Forty seven percent of those who correctly diagnosed an ulcer did not provide a response for the management.
Scenario five: oral carcinoma
Thirty nine percent of the doctors were able to correctly identify a suspected oral carcinoma from the clinical scenario. Other suggestions included thrush (15%) or trauma (8%). Forty two percent of the doctors would have referred the patient for management by the maxillofacial or ears, nose and throat (ENT) team. Seventeen percent said they would prescribe antifungals or antibiotics as their primary management.
Oral health training and confidence in managing oral conditions
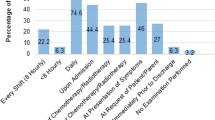
Fifty percent of the doctors said that they did not look into the mouth as part of a routine patient assessment, despite 90% expressing that they recognised it is important to do so. Ninety two percent of the junior doctors expressed they did not feel confident in diagnosing oral conditions with 94% answering they not did not feel confident in managing oral conditions.
Only 6% of the doctors reported that they had received previous training on the management of oral health conditions in their medical career at either an undergraduate or postgraduate level. Ninety seven percent said that they would like to receive additional training in the management or oral health conditions (Table 2).
Discussion
In recent years there has been an increased awareness that poor oral health is linked to several systemic health conditons.12,13 A failure by the medical team to assess the oral cavity or correctly manage oral conditions can result in patients experiencing oral pain and infection and contribute to difficulties eating and drinking; this will have an impact on their overall recovery.10
Morgan et al. carried out a study of two hospitals in Merseyside in 2001 to assess the views and knowledge of hospital doctors in general and geriatric medicine on oral health in older people.2 Results showed that out of the 70 doctors questioned, only 19% carried out an examination of the patients' mouth as part of their assessment, despite 84% feeling it was important to do so. The study reported several doctors were also unable to diagnose common oral mucosal lesions. In this survey, 50% of doctors said they regularly assessed the oral cavity but this is still a relatively low number.
Training in oral health
Oral health training is limited or non-existent for doctors both at an undergraduate and postgraduate level. This will have an impact on the care of inpatients who present with oral health-related problems. A survey found only eleven out of twenty-six medical schools in the United Kingdom included oral anatomy teaching in their curriculum.3 Ninety-four percent of doctors in this survey had no previous oral health training and this is reflected in the fact that, although they are aware of its importance, only half said they regularly look in the mouth when assessing a patient. Just six percent of the group felt confident in managing oral conditions, which is concerning as doctors are regularly faced with adult inpatients with oral problems that require a diagnosis and management.14 In the study by Morgan et al., 30% of doctors said that they would prescribe nystatin if asked to by nursing staff without first directly looking in the mouth.2 Furthermore, not only can inappropriate prescribing negatively impact the patient, it also contributes to the financial burden of the NHS.15
Doctors should be able to manage common oral conditions that develop in hospitalised patients such as candida infection, xerostomia and mucosal ulceration. For acute dental problems such as severe dental pain or very loose teeth, ideally there should be commissioned pathways in place to refer to local dental professionals, but in reality this is a rarity. In some trusts there are maxillofacial units who may accept referrals for inpatients who require management for severe dental infections but in many hospitals there are no links to onsite or domiciliary dental services for inpatients who require urgent dental care.
Impact of hospitalisation on oral health
Research has shown that hospitalisation is associated with a deterioration in oral health and this in turn may lead to hospital-acquired infections, poor nutritional intake, longer hospital stays and increased care costs.18 The most common oral conditions among the ageing population are tooth loss, dental decay, periodontitis, xerostomia and acute candida infection.19 Poisson et al.20 found that poor oral health is strongly associated with malnutrition and this can affect a patient's recovery.21 Patients with disabilities who are frail and medically unwell may not be able to directly communicate that they are not eating as a result of problems with their mouth, and there may be other signs such as visible poor dentition, ulceration, swelling or changes in behaviour including hitting or tugging at their face.22 These patients will depend on their medical and nursing teams recognising these signs, to assess their oral cavity and appropriately manage the condition until they can access dental care. Raising awareness of oral health among medical teams may help to improve inpatient care and contribute to reducing the length of hospital admissions.
Discussion of the scenarios used in this survey
We used scenarios in this survey to provide an indication of the knowledge of the junior doctors in diagnosis and management of oral conditions. Consideration needs to be taken into account that the scenarios and photographs provide limited information compared to a real life assessment and this will influence the answers provided. The aim of this survey was to get an overall idea of the level of knowledge of the doctors.
Scenario one: poor oral hygiene
Only one third of doctors recognised that the patient with learning disabilities had a build-up of dental plaque. There are many inpatients including those with cognitive or physical disabilities who may need help from staff or carers to maintain good oral hygiene. There is an increasing amount of evidence of the association between oral bacteria in the mouth and aspiration pneumonia,23 and so the mechanical removal of plaque with a toothbrush is very important. Hospital-acquired pneumonia is a common infection in hospitals with high morbidity and mortality rates; there are many causes including aspiration of oral bacteria, so awareness among the hospital team about the importance of removing plaque is very important. Although supporting patients with mouth care may be perceived as the role of nursing staff, it is important for doctors and allied healthcare professionals to also have it on their radar and to provide consistent messages. One in four doctors thought this patient had oral thrush and would prescribe antifungal treatment. If we extrapolate these figures to all hospitals in the UK, incorrect antifungal prescribing will be a significant cost burden to the NHS.15
Scenario two: xerostomia (dry mouth)
Although over half the doctors recognised that the most common reason for the sore mouth was a dry mouth, only 14% of those who correctly diagnosed would advise dry mouth care as first line management. Xerostomia is very common problem in hospitalised patients as a result of polypharmacy, dehydration, oxygen therapy, mouth breathing and being nil by mouth.
An absence of saliva can make the mouth very dry and sore. This can make it painful to clean, cause difficulty when chewing and swallowing food and medication, lead to problems with speech and difficulties wearing dentures. All of these factors can contribute to poor nutrition and lead to weight loss and poor recovery.9 Due to the implications xerostomia can have on a patient's quality of life, it is important hospital staff are able to recognise the signs of a dry mouth. Although nursing staff are responsible for supporting patients with regular dry mouth care, doctors can prescribe dry mouth gels and sprays for patients with advanced xerostomia that can help with the symptoms during a hospital admission.
Scenario three: denture stomatitis
Only 2% of the doctors recognised that the area of redness in the photograph was most likely a fungal infection as a consequence of not removing the denture for a long period of time. Three percent of doctors would prescribe antifungals and 13% did recognise that there was a need to improve denture hygiene.
Patients in hospitals and care homes often have high rates of denture stomatitis due to poor practice of good denture hygiene.24 This often comes down to poor understanding and training of staff. Denture stomatitis is a common finding among denture wearers, especially those who wear dentures at night and those who have difficulties keeping their dentures clean. Colonisation of the denture by causative organisms, primarily Candida albicans, causes inflammation and erythema in the underlying mucosal tissues.25 Again, the importance of removing and cleaning dentures at night and storing them safely to avoid them being lost should be a consistent message from all healthcare professionals.
Scenario four: ulceration
This was the most correctly answered scenario with 82% recording that the patient has an ulcer. However, almost half the respondents left the management response blank, suggesting that the doctors may not be aware of first line management for mouth ulcers such as saline rinses, anti-inflammatory mouth rinses or low-dose topical steroids.
Scenario five: oral cancer
Only 39% of those surveyed recognised that the large red and white speckled swelling in the mouth was likely an oral cancer and only 42% said they would refer to a specialist as their first line management. It is concerning that 13% of the doctors in this situation said they would prescribe antifungal medication as first line management. The incidence of oral cancer is rising. In the UK, oral cancer is the fourth most common cancer among men and the twelfth most common cancer among women.26 Early detection of squamous cell carcinoma can improve the five-year survival rate by 50-80%.26 In this case, the patient was diagnosed with a late stage squamous carcinoma and the lesion was discovered on the day she was about to be discharged from hospital after a two week stay.27 The results from the survey demonstrate the importance of the medical team looking into the mouth as part of inpatient assessment on admission.
Statement of the problem
The main focus of the 'Mouth Care Matters' programme is to raise awareness of the importance of oral health for hospital patients and upskill staff to enable them to provide good mouth care.28 Much of the initial training was directed at nursing staff, who began to assess the mouths of all vulnerable patients admitted to hospital for more than 24 hours. This led to nursing staff identifying more issues with the mouth and asking junior doctors to diagnose and manage oral conditions. At the pilot trust, hospital staff were able to refer patients for whom they had specific oral health concerns to a dentist. One in four of these referrals in the first six months were from junior doctors for advice on managing and diagnosing conditions such as thrush and dry mouth. To address this issue the Mouth Care Matters team developed training sessions for doctors focused on common oral conditions found in hospitalised patients. This involved the incorporation of oral health training into the medical training programme through:
An annual oral health teaching session for foundation year one and two doctors
Four oral health presentations at grand rounds (lunchtime teaching session for hospital doctors) each year
The development of a pathway for oral health advice for junior doctors which is managed by supervised dental core trainees.
The oral health knowledge that the junior doctors gain will be useful in whichever area of medicine they end up pursuing. Although the public are encouraged to see a dentist with oral conditions, many patients end up at accident and emergency or at their general medical practitioners with dental problems.29 The training sessions have also been a good experience for the dental core trainees who have the opportunity to develop their teaching skills. It is envisioned that Health Education England will continue to support this model of training.
This survey was of a relatively small sample and the findings encourage research into the oral health knowledge of not only foundation doctors but also speciality trainees and consultant and general medical practitioners.
There is an opportunity through training initiatives like Mouth Care Matters for collaboration between the dental and medical professionals to help to continue to raise awareness that oral health is an integral part of general health.
Conclusion
Poor oral health is a significant problem for inpatients and education and training for nursing staff can help to improve standards of mouth care in a hospital. However, the lack of education and training for doctors can impact on patient care as oral conditions may not be managed appropriately. Serious oral conditions can be missed as a consequence of a failure to look in the mouth. It is important that oral health is recognised as an important element of general health and that poor oral health may extend inpatient admissions.
The results from this survey suggest that junior doctors are not able to manage common oral health conditions and that this may be the result of a lack of training in oral health. The junior doctors that participated in this survey recognised the importance of assessing the oral cavity as part of patient care, but did not feel confident to do so. More evidence is needed so that it can be used to support the need for undergraduate and postgraduate oral health training for doctors. The study should be repeated on a larger scale and with wider target groups including consultants and general medical practitioners. Providing doctors with training in oral health has the potential to directly improve patient care.
References
Cope A L, Chestnutt I G, Wood F, Francis N A. Dental consultations in UK general practice and antibiotic prescribing rates: a retrospective cohort study. Br J Gen Pract 2016; 66: 329-336.
Morgan R, Tsang J, Harrington N, Fook L. Survey of hospital doctors' attitudes and knowledge of oral conditions in older patients. Postgrad Med J 2001; 77: 392-394.
Joint Royal Colleges of Physicians Training Board. Speciality training curriculum for geriatric medicine curriculum. 2010. Available at https://www.jrcptb.org.uk/sites/default/files/2010%20Geriatric%20Medicine%20Curriculum%20%28AMENDMENTS%202016%29.pdf (accessed August 2019).
McCann P J, Sweeney M P, Gibson J, Bagg J. Training in oral disease, diagnosis and treatment for medical students and doctors in the United Kingdom. Br J Oral Maxillofac Surg 2005; 43: 61-64.
Ewbank L, Thompson J, McKenna H. NHS hospital bed numbers: past, present, future. 2017. Available at https://www.kingsfund.org.uk/publications/nhs-hospital-bed-numbers (accessed August 2019).
Steele J G, Treasure E T, O'Sullivan I, Morris J, Murray J J. Adult Dental Health Survey 2009: transformations in British oral health 1968-2009. Br Dent J 2012; 213: 523-527.
Bilder L, Yavnai N, Zini A. Oral health status among long-term hospitalized adults: a cross sectional study. PeerJ 2014; 2: e423.
Avcu N, Ozbek M, Kurtoglu D, Kurtoglu E, Kansu O, Kansu H. Oral findings and health status among hospitalized patients with physical disabilities, aged 60 or above. Arch Gerontol Geriatr 2005; 41: 69-79.
Sousa L L, e Silva Filho W L, Mendes R F, Moita Neto J M, Prado Junior R R. Oral health of patients under short hospitalization period: observational study. J Clin Periodontol 2014; 41: 558-563.
Gil-Montoya J A, Subirá C, Ramón J M, González-Moles M A. Oral health-related quality of life and nutritional status. J Public Health Dent 2008; 68: 88-93.
McGurk M, Chan C, Jones J, O'Regan E, Sherriff M. Delay in diagnosis and its effect on outcome in head and neck cancer. Br J Oral Maxillofac Surg 2005; 43: 281-284.
D'Aiuto F, Gable D, Syed Z et al. Evidence summary: the relationship between oral diseases and diabetes. Br Dent J 2017; 222: 944-948.
Dietrich T, Webb I, Stenhouse L et al. Evidence summary: the relationship between oral and cardiovascular disease. Br Dent J 2017; 222: 381-385.
Royal College of Surgeons: Faculty of Dental Surgery. Improving older people's oral health. 2017. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/media-gov/fds-improving-older-peoples-oral-health-2017.pdf (accessed August 2019).
Kent Surrey Sussex Academic Health Science Network. Cost benefit analysis of the Mouth Care Matters programme. 2017. Available at http://www.mouthcarematters.hee.nhs.uk/wp-content/uploads/2017/08/Mouth-Care-Matters-Health-Economic-Report-FInal-draft-20170710-clean....pdf (accessed August 2019).
Salamone K, Yacoub E, Mahoney A M, Edward K L. Oral care of hospitalised older patients in the acute medical setting. Nurs Res Pract 2013; 827670. DOI: 10.1155/2013/827670.
Health Education England. Mouth Care Matters - Improving Oral Health. Available at http://www.mouthcarematters.hee.nhs.uk (accessed August 2019).
Terezakis E, Needleman I, Kumar N, Moles D, Agudo E. The impact of hospitalization on oral health: a systematic review. J Clin Periodontol 2011; 38: 628-636.
Thomson W M, Ma S. An ageing population poses dental challenges. Singapore Dent J 2014; 35: 3-8.
Poisson P, Laffond T, Campos S, Dupuis V, Bourdel-Marchasson I. Relationships between oral health, dysphagia and undernutrition in hospitalised elderly patients. Gerodontology 2016; 33: 161-168.
Walls A W, Steele J G, Sheiham A, Marcences W, Moynihan P J. Oral health and nutrition in older people. J Public Health Dent 2000; 60: 304-307.
Alzheimer's Society. How to tell if someone has dental problems. Available at https://www.alzheimers.org.uk/get-support/daily-living/how-tell-if-someone-has-dental-problems#content-start (accessed August 2019).
Manger D, Walshaw M, Fitzgerald R et al. Evidence summary: the relationship between oral health and pulmonary disease. Br Dent J 2017; 222: 527-533.
Atashrazm P, Sadri D. Prevalence of oral mucosal lesions in a group of Iranian dependent elderly complete denture wearers. J Contemp Dent Pract 2013; 14: 174-178.
Gendreau L, Lowery Z G. Epidemiology and etiology of denture stomatitis. J Prosthodont 2011; 20: 251-260.
Cancer Research UK. Head and neck cancer statistics. Available at http://www.cancerresearchuk.org/health-professional/cancer-statistics/statistics-by-cancer-type/oral-cancer (Accessed August 2019).
Doshi M, Patel J. Putting the mouth back into the body. Br J Hosp Med 2017; 78: 244-245.
Binks C, Doshi M, Mann J. Standardising the delivery of oral health care practice in hospitals. Nursing Times 2017; 113: 11-18.
Ahluwalia A, Crossman T, Smith H. Current training provision and training needs in oral health for UK general practice trainees: survey of General Practitioner Training Programme Directors. BMC Med Educ 2016; 16: 142.
Acknowledgements
The authors would like to thank Professor Stephen Lambert-Humble, Past Postgraduate Dental Dean of Kent, Surrey and Sussex.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Health Education England is funding the Mouth Care Matters initiative in trusts in England.
Rights and permissions
About this article
Cite this article
Doshi, M., Weeraman, M. & Mann, J. A survey of the knowledge of junior doctors in managing oral conditions in adult inpatients. Br Dent J 227, 393–398 (2019). https://doi.org/10.1038/s41415-019-0666-z
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0666-z
This article is cited by
-
The rosetta stone of successful ageing: does oral health have a role?
Biogerontology (2023)
-
Hospital Dental Services to Reduce Hospital-Acquired Pneumonia
Current Oral Health Reports (2023)
-
Who and what you know - making the most of our contacts to vulnerable patients
British Dental Journal (2022)
-
Oral health ambassador scheme: training needs analysis in the community setting
British Dental Journal (2022)
-
Dental care pathways for adult inpatients in an acute hospital: a five-year service evaluation
British Dental Journal (2020)