Abstract
Introduction With waiting list time increasing in all specialties in the aftermath of the COVID-19 pandemic, it is vital to make sure that patients are receiving treatment in an appropriate setting. Most oral surgery undertaken in secondary care could be successfully carried out in a primary care setting by specialist oral surgeons or general dental practitioners (GDPs) with a special interest in oral surgery.
Aim To investigate reasons for oral surgery referrals to secondary care.
Method A pilot study looking at oral surgery referrals to secondary care was completed to identify key themes for referrals. From this, a questionnaire was designed. An electronic copy of the questionnaire was distributed to all GDPs registered with Health Education and Improvement Wales (HEIW) throughout Wales.
Results Five main themes for referrals, which corresponded with the pilot study findings were: contract limitations; the perception that recently trained dentists do not have the practical skills to undertake oral surgery; limited communication between the oral and maxillofacial surgery departments and GDPs; limited practice resources; and GDPs being less risk averse in undertaking oral surgery in primary care.
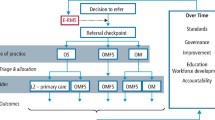
Outcome Following the results from this research, an All-Wales oral surgery referral handbook for general dental practitioners was published, hosted by HEIW, describing oral surgery patient care pathways. Formation of the Oral Surgery Managed Clinical Networks in Wales and the All-Wales Oral Surgery Strategic Advisory Forum will help further develop robust, sustainable patient care pathways, in collaboration with the health boards.
Key points
-
Newly qualified general dental practitioners are perceived by their colleagues to have insufficient oral surgery skills required for general practice.
-
Oral surgery is not adequately remunerated in primary care.
-
Collaboration between oral surgery/oral and maxillofacial surgery departments and primary care need to improve.
Similar content being viewed by others
Introduction
Oral surgery referrals represent the largest volume and cost of all referrals from primary dental care to secondary care.1 Oral surgery referrals are mainly for tooth extractions that may present with surgical or medical complications and may also be supplemented by a request for sedation or general anaesthetic due to patient anxiety and/or the complexity of procedure required.2 Data from health boards on electronic referrals suggest an exponential increase in referrals for oral surgery to secondary care over recent years, with subsequent pressure being placed on hospitals to deliver treatment in a timely, safe and cost-effective manner.3 Several reasons have been put forward to explain this increase in demand: the 2006 UK NHS dental contract may provide unintentional financial incentives for general dental practitioners (GDPs) to refer patients and newly qualified dentists may lack the experience to confidently undertake routine oral surgery procedures.4,5,6
Referral to treatment (RTT) is the total time patients wait from GDP referral to treatment in secondary care. The current RTT in Wales is:
-
95% of all patients should be seen within 26 weeks
-
No patient should wait longer than 36 weeks for treatment.
-
There are different RTT for cancer pathways.7
In Cardiff and Vale University Health Board, a substantial backlog of patients has accrued over the past 12 months and average RTT now stands at 87 weeks (February 2021). There are 2,270 patients awaiting a first appointment and a further 647 patients who have been assessed and are awaiting surgery (February 2021). A pre-pandemic analysis showed that the average monthly referrals exceeded current capacity by about 120 patients per month. The pandemic-induced backlog and lack of clinical space means that demand outstrips capacity. Increase in demand for oral surgery services has been recognised for several years, as well as a rise in the number of referrals from primary to secondary care.
Most oral surgery procedures, which are currently undertaken in secondary care, could be delivered safely by dentists with enhanced skills (DES) and specialist oral surgeons working in primary care. Some health boards and trusts in England and Wales have already established primary care-based oral surgery services, delivered by DES with experience in oral surgery. In this context, an audit of oral surgery referrals to Cardiff Dental Hospital showed that there were a significant proportion of inappropriate referrals, that is, two-thirds of referrals from GDPs registered at Cardiff Dental Hospital in 2019 were deemed suitable to be carried out in primary care. This volume of inappropriate referrals to hospitals undoubtedly puts pressure on waiting times.
The main aims of this national study were to investigate reasons for oral surgery referrals from primary to secondary care.
Method
A cross-sectional survey of GDPs throughout Wales, following on from an initial qualitative study, was undertaken. A pilot had already been completed using semi-structured, audio-recorded interviews, with five GDPs working in Cardiff and Vale University Health Board following written consent. Thematic analyses of the transcripts identified five key themes responsible for many oral surgery referrals from primary to secondary care.8 They were:
-
Contract limitations
-
All GDPs interviewed felt that the remuneration for carrying out surgical extractions was insufficient and felt that if they were better remunerated, they would be more likely to attempt the extraction
-
Perception that recently trained dentists do not have the practical skills to undertake oral surgery
-
Communication between the oral surgery/oral and maxillofacial surgery (OMFS) department and GDPs. None of the GDPs interviewed were aware of the current hospital waiting times. All agreed that the OMFS department should contact the GDPs who inappropriately refer patients and GDPs should be encouraged to attend postgraduate courses
-
Limited practice resources
-
GDPs less risk averse in undertaking oral surgery in primary care.
A questionnaire was developed using the key themes identified in the pilot. The questionnaire focused on current oral surgery practice in primary care, oral surgery experience on qualifying, referrals to secondary care and communication between GDPs and oral surgery/OMFS department.
According to the NHS Wales Shared Services Partnership, there are over 430 primary dental care practices in Wales stratified by seven health boards, with over 1,100 GDPs registered to carry out NHS primary care services.
The inclusion and exclusion criteria for GDPs to complete the survey were:
-
Inclusion criteria - dentists working in primary care in Wales who are willing to take part in the study
-
Exclusion criteria - dentists working in primary care who are unwilling to take part in the study.
Ethical approval was obtained from Cardiff Dental School Research Ethics Committee.
Health Education and Improvement Wales (HEIW) have all registered GDP email addresses, place of work and telephone contact details. HEIW forwarded an email with a link to the questionnaire to all GDPs working in Wales, inviting them to participate in the survey. Consent to take part in the study was implicit and anonymous, that is, completing the study questionnaire was taken as implied consent. The data were analysed using Excel and SPSS Statistics.
Questions included in the study related to:
-
Position in practice
-
Years since qualified
-
Primary dental degree-awarding university and how teaching was delivered
-
Confidence when first qualified with simple extractions and surgical procedures
-
Any postgraduate training since qualified and if yes, what type
-
Preference to perform more oral surgery in practice and the barriers to this
-
Oral surgery remuneration in primary care
-
Potential complaints from patients affecting their decision to refer a patient
-
Communication between GDPs and oral surgery/OMFS departments
-
Thoughts on extracting the roots in Figure 1.
Results
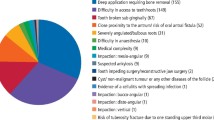
Overall, 236 responses were received (55.1% from associates), some incomplete, equating to 21.5% of GDPs in Wales. Years qualified ranged from 1 to over 31 years and more than one-third (40%) were Cardiff graduates (most common response). Just over two-thirds (67.8%) would like to do more oral surgery in practice. Over half of GDPs agreed that a potential complaint would affect their decision to carry out an extraction in primary care. Over 80% of GDPs agreed/strongly agreed that colleagues are more risk averse and are more likely to refer potentially complicated extractions. In total, 70% of GDPs declared to have had some form of further training post primary dental qualification - the most common format was a simulation course (as part of foundation training or other postgraduate training e.g. pig's head course), followed by training as junior staff in OMFS in secondary care (Fig. 2). Almost half of GDPs who responded (49%) felt they have sufficient oral surgery experience and more than three-quarters (77.5%) strongly agreed/agreed that recently qualified dentists do not have the oral surgery practical skills required to undertake oral surgery in primary care. In this study, over half of GDPs chose 'not confident at all' in performing a surgical extraction when they graduated from dentistry (Fig. 3).
Over half of GDPs agreed/strongly agreed that complexity Level 1 and 2 extractions should be carried out in a hospital setting and an overwhelming majority of GDPs (94%) declared that they had not heard of the Welsh Health Circular The future development of oral surgery and oral medicine services in Wales (WHC/2015/041). Furthermore, 70% of GDPs were neutral/disagreed/strongly disagreed that they knew the difference between complexity Level 1 and 2 extractions. Over half of GDPS (58%) agreed/strongly agreed that if oral surgery/OMFS departments sent out guidance on referrals to secondary care, GDPs would send fewer referrals. In reference to the retained roots shown in Figure 1, 51.3% felt they were 'completely confident' in being able to extract the roots.
The most common reasons for referring patients to secondary care were impacted third molars, anxious patients, and patients who have had previous radiotherapy to the head and neck region. Barriers to performing surgical extractions in practice included inadequate remuneration and lack of experience (Fig. 4).
Discussion
Contract limitations and limited practice resources
Units of dental activity (UDA) are essentially the value given to a course of treatment.9 UDA value can range from over £100 in parts of London to £11 in the West Midlands, with the average value being £25. The value of a UDA can differ in different local health boards throughout Wales. An associate working in the practice would then get a 'share of that value of the UDA', for example, £10 a UDA. Extractions and surgical extractions currently sit in Band 2 - the equivalent of three UDAs. If a patient required a restoration and an extraction on different teeth, they would get three UDAs. However, if they completed the restoration on one tooth and referred the patient for the extraction of another to secondary care, they would also receive three UDAs. With increased demands on GDPs' time, most GDPs felt that it was simply not worth their time to carry out difficult extractions. Most GDPs felt that oral surgery wasn't a good 'practice builder' due to the post-operative swelling, bruising and infection associated with an extraction. If the UDA value of oral surgery was increased or given a 'fee structure' this could encourage those GDPs to undertake more oral surgery in primary care or attend courses to upskill/expand their skill set so they are able to perform oral surgery in primary care.
Risk averse
Of those surveyed, 82.6% agreed/strongly agreed that practitioners are more risk averse and therefore, likely to refer extractions deemed to be complicated. Non-surgical extractions (those not requiring raising a flap or bone removal) carry a risk of pain, bruising, swelling and infection, like most surgical procedures; therefore, dental extractions are not seen as a 'general dental practice builder'. GDPs are concerned about litigation because it is in the press more frequently and can increase their indemnity.
A dental protection survey carried out in 2018 found that 89% of dentists are fearful of being sued by a patient and 64% of respondents felt that the fear of being sued has resulted in them making more referrals.10
Communication between the oral surgery/OMFS department and GDPs
Of the participants, over three-quarters (76.3%) felt there wasn't enough communication between primary care and their local oral surgery/OMFS department.
When asked how to improve the communication between oral surgery/OMFS departments and GDPs:
-
71% wanted more feedback on referrals
-
41.5% wanted the guidelines hospitals worked to
-
73.7% wanted a point of contact for verbal advice
-
71.2% wanted advice on what waiting list times are.
It is important to let GDPs know current waiting times for procedures so they are able to give the correct information to patients, enabling the patient to make an informed decision about being referred.
Following on from this research, and led by the South East Wales Oral Surgery and Oral Medicine Managed Clinical Network, the All Wales oral surgery referral guidelines for general dental practitioners has been developed and published for GDPs - the document is hosted by HEIW on their primary care platform. An update to the e-referral software in Cardiff and Vale University Health Board to display RTT times on the referral platform will allow GDPs to see and inform patients in real time the wait time to be seen in secondary care. In addition, a 'hotline' to the oral surgery/OMFS department for GDPs to contact if they have questions regarding a patient being treated in primary care would be beneficial. This could be either via telephone or web-based query, answered within 24 hours by a senior clinician within the department. This could encourage GDPs to contact with medical queries for oral surgery patients treated in primary care.
Of note, almost all of the participants in this survey had not heard of the Welsh Health Circular Future development of oral surgery and oral medicine service in Wales (WHC/2015/041). This is a large document that GDPs may feel is irrelevant to them; however, it does contain the difference between Level 1/Level 2 extractions and where it is appropriate for these procedures to be carried out. A new oral surgery Welsh Health Circular - Role and provision of oral surgery in Wales (WHC/2021/033) - was released in December 2021.
Of the GDPs asked if they would refer the following patient for treatment in secondary care, the following responses were received:
-
Warfarin - 6.4%
-
Head and neck radiotherapy - 68.6%
-
Novel anticoagulants - 8.9%
-
Bisphosphonates - 29.2%
-
Diabetic patient - 0.8%.
This was a positive outcome, as GDPs are expected to be able to manage patients on warfarin, on novel anticoagulants, and diabetic patients within the primary care setting. Patients who have undergone head and neck radiotherapy or patients taking bisphosphonates could be managed within primary care; however, it is understandable why GDPs would refer these patients into secondary care, as they have the potential to have significant complications following oral surgery.
Perception that recently trained dentists do not have the practical skills to undertake oral surgery
Over three-quarters of responders agreed/strongly agreed that recently qualified dentists do not have sufficient oral surgery practical skills. Previously, an undergraduate dental student would have been expected to obtain a minimum number of extractions in combination with written and oral examinations. However, this has largely been replaced in the majority of dental schools with a 'competency-based assessment', where students are required to demonstrate the achievement of a number of learning outcomes defined by the General Dental Council. Graduation marks the end of formal teaching; however, it does not signify an end to learning, as the dentist has a responsibility to learn and develop throughout their career 'to update and develop professional knowledge' (General Dental Council Standard 7.3).11,12 Gilmour et al.12 carried out a study looking at fifth year students' confidence at carrying out clinical procedures. The procedures that they felt least confident in were surgical extractions involving a flap and simple surgical procedures. Macluskey et al.13 reported that forceps exodontia and surgical extractions have a high discrepancy in confidence, shown by a survey that recorded the number of surgical extractions undertaken by UK dental undergraduates. Gilmour et al.'s14 study of foundation trainers in England and Northern Ireland found that nearly 40% of trainers felt that new graduates were unable to undertake a surgical extraction on their own, and a further 30% felt that new graduates would need advice before attempting the procedure. This is likely to be higher in the aftermath of the COVID-19 pandemic and the effect that this has had on recent graduates' clinical experience.
Furthermore, 70.8% of respondents had carried out some form of further training post primary dental qualification; the most common was simulation followed by completing a senior house officer (SHO) job (Fig. 2). Those who had carried out a simulation course or completed a SHO post felt they had the necessary skills in completing oral surgery and were generally more confident in oral surgery than those who hadn't.
When cross-tabulating 'how confident were you in performing a surgical extraction when you first graduated?' with the university qualified from, Barts and the London had the best response, with 66.7% of those who answered feeling fairly confident, in comparison to Cardiff, where 62.1% felt they 'weren't confident at all'.
Currently, in Wales, as part of the study days for foundation dental trainees and dental core trainees (DCTs), an informative simulation training day is held annually with two senior oral surgeons, which is well-received by trainees. Scaling up these hands-on training course, in collaboration with HEIW, would help upskill junior dental trainees in oral surgery. Such courses could also be offered to GDPs who have been identified as consistently making inappropriate surgical referrals to secondary care. An 'e-package' has been considered to help practitioners struggling with oral surgery; however, without a clinical element, the authors are unsure how successful this would be in upskilling GDPs. Cross tabulation of the ability to extract retained roots (Fig. 1) with year qualified showed a strong positive association between confidence in extracting roots and years qualified.
There are approximately 40 oral surgery speciality trainees across the UK and 755 registrants on the oral surgery specialist list (including some OMFS surgeons).15 If a GDP is seen to be referring a large number of inappropriate referrals, they could be allocated an oral surgery mentor who is on the oral surgery specialist list to help them develop their skills and therefore limiting referrals to secondary care.
Conclusion
Following the results from this research, the All-Wales referral guidelines for general dental practitioners have been developed for GDPs defining care pathways for patients with the most common oral surgery needs and medical conditions. Plans to develop a (Once for Wales) DES pathway in oral surgery are underway, in collaboration with HEIW, Oral Surgery Managed Clinical Networks, and the All-Wales Oral Surgery Strategic Advisory Forum.
References
O'Neil E, Gallagher J E, Kendall N. A baseline audit of ereferral and treatment delivered to patients in the intermediate minor oral surgery service in Croydon PCT. Prim Dent Care 2012; 19: 23-28.
Kendall N. Development of oral surgery services in primary care. Oral Surg 2011; 4: 57-64.
Kendall N. Improving access to oral surgery services in primary care. Prim Dent Care 2009; 16: 137-142.
Medical Education England. Review of Oral Surgery Services and Training. 2010. Available at https://www.baos.org.uk/resources/MEEOSreview.pdf (accessed January 2023).
Goldthorpe J, Sanders C, Gough L et al. Implementing and evaluating a primary care service for oral surgery: a case study. BMC Health Serv Res 2018; 18: 636.
Welsh Government. Improving access to specialist dental services delivered in primary care. 2015. Available at https://www.gov.wales/sites/default/files/publications/2019-07/guidance-for-health-boards-on-improving-access-to-dental-services-for-vulnerable-patients.pdf (accessed January 2023).
Welsh Parliament. Hospital waiting times - What do you need to know? 2019. Available at https://senedd.wales/media/ycspv5fr/hospital-waiting-times.pdf (accessed January 2023).
Sivarajasingam V, Athwal J, Lewis K, Mort J, Emmanuel C, Morgan M. Oral surgery referrals at a UK dental hospital in the context of a managed clinical network: a mixed-methods study. Oral Surg 2020; 13: 212-220.
Watson M. What is a UDA? Vital 2010; 7: 13.
Dental Protection. Dental Protection survey reveals 9 in 10 dentists fear being sued by patients. 2018. Available at https://www.dentalprotection.org/uk/articles/dental-protection-survey-reveals-9-in-10-dentists-fear-being-sued-by-patients (accessed January 2023).
General Dental Council. Standards for the Dental Team. 2013. Available at https://standards.gdc-uk.org/Assets/pdf/Standards%20for%20the%20Dental%20Team.pdf (accessed January 2023).
Gilmour A, Welply A, Cowpe J G, Bullock A, Jones R J. The undergraduate preparation of dentists: Confidence levels of final year dental students at the School of Dentistry in Cardiff. Br Dent J 2016; 221: 349-354.
Macluskey M, Durham J, Bell A et al. A national survey of UK final years students' opinions of undergraduate oral surgery teaching. Eur J Dent Educ 2012; 16: 205-212.
Cardiff University. Dental Foundation Trainers' Expectations of a Dental Graduate. 2012. Available at https://www.cardiff.ac.uk/__data/assets/pdf_file/0007/26566/Dental-Foundation-Trainers-expections-of-new-graduates.pdf (accessed January 2023).
Health Education England. Oral Surgery. Available at https://dental.hee.nhs.uk/dental-trainee-recruitment/dental-specialty-training/oral-surgery (accessed January 2023).
Acknowledgements
The authors would like to acknowledge Health Education and Improvement Wales in helping to distribute the questionnaire.
Author information
Authors and Affiliations
Contributions
Kim Lewis: carried out the pilot study, designed and arranged distribution of the questionnaire, wrote the first draft of the article, and proofread and edited the article. Vas Sivarajasingham: highlighted the need for research, was supervisor throughout the project, and proofread and edited the article. Maria Morgan: public health specialist, contributed to survey design, analysed results and edited the paper.
Corresponding author
Ethics declarations
The authors declare no conflicts of interest.
Ethical approval was obtained from Cardiff Dental School Research Ethics Committee.
Consent to take part in the study was implicit and anonymous, that is, completing the study questionnaire taken as implied consent.
Rights and permissions
About this article
Cite this article
Lewis, K., Sivarajasingam, V. & Morgan, M. An investigation into oral surgery referrals in Wales. Br Dent J (2023). https://doi.org/10.1038/s41415-023-5505-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41415-023-5505-6