Abstract
Introduction Socioeconomic and ethnic status have in the past been implicated as possible causes of dental caries. Aims To assess the role that relative social depravation and ethnicity has on dental caries in two- and three-year-olds undergoing DGA in Wolverhampton. Design and methods Retrospective analysis of hospital records of 213 patients over a six-year period (2011-2016). A three-way analysis of variance (ANOVA) and chi-square tests were used to test statistical significance. Results The most significant factor between ethnicity, year and sex, was ethnicity (P = 0.026), with the greatest difference between mean number of teeth extracted per treatment visit for Other Whites (mean = 6.3) compared with White British (mean = 4.0) (difference P = 0.012). The association between the difference in extracted quadrant and year of treatment was significant (P = 0.011), with the greatest frequency of extractions involving three and four quadrants in the later years of 2015 and 2016. Seventy percent of children treated were living in the 20% most deprived areas (deciles one and two) compared with children living in more affluent areas (deciles three to ten) (P <0.001). Conclusion An important public health issue is highlighted which needs to be addressed, both at a national level and locally, through early oral health education for mothers from relatively deprived areas; particularly those of Other White ethnicity.
Similar content being viewed by others
Key points
-
Highlights the relatively high levels of DGA activity reported in very young children of two and three years of age.
-
Discusses how DGA activity is associated with risks of relative social deprivation and ethnicity.
-
Suggests early oral health education is required to increase awareness of the importance of early dental attendance.
Introduction
Despite significant improvements in the oral health of the UK population, there still remains a high prevalence of dental caries in children; with no significant reduction in dental disease of those under five,1 including children as young as two and three having teeth removed due to dental decay. The first national survey of three-year-olds carried out by Public Health England in 20132 has shown that 12% of three-year-olds surveyed had evidence of dental decay, with an average number of 3.07 decayed, missing and filled teeth (d3mft). Due to their young age, any children aged two and three years requiring dental extractions are invariably admitted to hospital for a dental general anaesthetic (DGA). This included 7,926 children under five years in 2015-16, with estimated costs to the National Health Service (NHS) of £7.8 million annually.3 While the risk of mortality is reported to be 1 in 250,000; morbidities are more common, occurring in 40-90% of children receiving a DGA including pain, nausea and bleeding.4 In addition to these physical impacts, recent research5 has shown that anxiety can have an important negative psychological impact from a child's perspective both pre- and peri-operatively; but interestingly children receiving a DGA also reported positive psychological outcomes post-operatively, such as satisfaction that their dental problem had been resolved.
While the cause of the decay can be attributed most commonly to the frequent consumption of sugar in food and drinks,6 a number of other variables are also involved. These include referral pathways, preventive strategies and the demographic profile of children admitted for DGA such as age, sex, ethnicity and socioeconomic background. Studies on these variables can help identify trends which can be used to facilitate future planning of healthcare and target oral health prevention.
The association between dental caries in children and social deprivation is well documented, with children from deprived backgrounds more likely to have experienced tooth decay than those from more affluent areas. The 2013 oral health survey of three-year-olds2 showed that 19% of the prevalence of decay was due to deprivation and the 2017 oral health survey of five-year-olds showed that prevalence among the most deprived children was higher at 33%.7 Children from deprived backgrounds are also more likely to require hospital admissions for dental extractions than children from more affluent areas.8 Inequalities in dental decay prevalence are also known to be associated with ethnicity. Studies have shown that in some ethnic minority groups, it is more pronounced in pre-school children than in any other age group.9
Wolverhampton has a multi-ethnic population of 250,000 and is in the 6% most deprived authorities in the UK.10 Deprivation is disproportionate across the city, with a marked disparity between residents in affluent wards and those from less affluent wards, in the east and south east of the city, where there is high unemployment. Approximately 400-450 children per annum present to New Cross Hospital, Wolverhampton for a DGA due to caries including children as young as two and three years old, which is concerning and raises important public health issues. The aim of this study is to investigate the importance of socioeconomic and ethnicity risk factors in the development of dental caries in young children of two and three years who attended New Cross Hospital, Wolverhampton for dental extractions.
Method
This retrospective study examined hospital records of two- and three-year-olds who received a DGA at New Cross Hospital, Wolverhampton over a six-year period, 2011-2016. Data relating to the child's age, sex, and teeth extracted were obtained from the theatre register and details of postcodes of residence and ethnicity from the electronic patient notes. The DGA service at New Cross offers only an exodontia service, under inhalational GA, accepting children from 2-16 years of age, referred mainly from general dental practitioners (GDPs), general medical practitioners (GMPs), and also from the special care dental service, with a few patients referred from the paediatric department within the hospital.
Children were seen for a pre-operative assessment by a senior dental officer (NS), who shares the role of operating dentist with another senior dental officer (RH). Although neither dentist is a specialist in paediatric dentistry, both are very experienced clinicians and have been undertaking DGA activity for many years. At the pre-assessment appointment, administrative and clinical details relating to each patient were recorded. ASA I patients and ASA II patients with controlled medical conditions were treated as outpatients. Patients with complex medical conditions were referred to the maxillofacial department at New Cross or to Birmingham Children's Hospital.
The teeth were examined visually, using a mouth mirror and operating light, for clinical caries. Intra-oral radiographs were used whenever possible, although this was not generally tolerated by the two- and three-year-olds treated. To avoid repeat GAs, all carious and symptomatic teeth were extracted as recommended in the 'Guidelines for the use of general anaesthesia in paediatric dentistry'.11 Parents were advised on their child's oral health before and after the DGA, and of the importance of seeking regular dental care following the DGA. Although the service accepts some referrals for patients living outside the city of Wolverhampton, these were excluded from the study, which included a total of 213 two- and three-year-olds from Wolverhampton. The index of multiple deprivation (IMD) 201512 was used to determine the relative deprivation of the child's area of residence, using small area geographies known as lower super output areas (LSOAs), containing individual post codes. Using the IMD index, LSOAs were ranked into deciles according to the level of relative deprivation (that is, 1 to 10, where 1 = 10% most deprived area).
The number of teeth extracted was analysed using a three-way analysis of variance (ANOVA), with the three factors being 'ethnicity', 'year' and 'sex'. The number of quadrants involving extractions was recorded and monitored by year (2011-2016). The association between the quadrants involved by year was analysed using a chi-square test of independence. Statistical significance was set at the P value of 0.05. The number of children treated by deprivation decile was analysed using a chi-square goodness of fit test (the null hypothesis was assumed to take a uniform distribution).
Results
Table 1 demonstrates the demographic characteristics of the two- and three-year-olds treated, by sex and year of treatment. Of the 213 treated from 2011-2016, 111 (53.3%) were boys and 102 (46.7%) were girls. The majority of those treated were White British (57%) with South Asian accounting for 14.5%, Other Whites (white persons not English, Scottish, Welsh or Irish) 13%, Black 5.1%, and Mixed Race and Other Ethnic Groups both 4.7%. The ethnicity of two children (0.9%) was not stated.
The three-way ANOVA identified no high-order interactions (between ethnicity, year and sex) and the only significant main effect was due to ethnicity (P = 0.026); see the mean numbers of deciduous teeth extracted by ethnicity in Figure 1. Bonferroni multiple comparisons identified the greatest difference was predominately between the mean number of deciduous teeth extracted for those of White British ethnicity (mean = 4.00) compared with Other Whites (mean = 6.3) (difference = -2.3, P = 0.012; with 95% CI -4.3 to -0.28).
The association between the extracted quadrants by year was significant, with the chi-square test of independence χ2 = 30.3 with 15 df (P = 0.011), see Table 2. The significant association confirms a trend of children's teeth being extracted from one and two quadrants in the earlier years (2011 and 2012) but being extracted more frequently from three and four quadrants in more recent years (2015 and 2016).
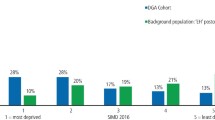
Concerning socioeconomic trends this can be seen in Table 3, with more children being treated who lived in relatively deprived areas compared to more affluent ones. The chi-squared goodness of fit test for the 'observed' and 'expected' number of children (assuming a uniform distribution under a null hypothesis) shows this confirming that more children were treated from areas of greatest deprivation (deciles one and two) in contrast with those living in more affluent areas (deciles three to ten). The imbalance is clearly illustrated in Table 3 and Figure 2.
The results of the chi-square goodness of fit test was χ2 = 318.4 with nine degrees of freedom (df) (P <0.001). This imbalance can be seen in Figure 2.
Discussion
The results of this study show that socioeconomic and ethnic status are risk factors in dental caries for some two- and three-year-olds living in Wolverhampton involving the need for a DGA. The association between deprivation and ethnicity was not measured but the data show a clear relationship between risks of caries experience and relative deprivation (see Table 3, Figure 2); with more episodes of care required by children living in relatively deprived areas in the east and south east of the city. Seventy percent of children receiving a DGA resided in the 20% most deprived areas (deciles one and two) in Wolverhampton. The results also reveal a disproportionate percentage of children treated from some ethnic groups based on data from the last census,13 involving 5.3% Other Whites compared with 1.39% White British, 1.29% Other Ethnicities, 0.44% South Asians, 0.42% Black and 0.24% Mixed Race. The association between loss of deciduous teeth and increased numbers of quadrants, involving three or four quadrants, increased in later years (2015 and 2016), including loss of deciduous second molars. This is concerning, as the loss of this tooth increases the risk of crowding and impaction of the permanent second premolar due to mesial movement of the permanent first molar.
The association between caries and socioeconomic status is well established.14 Evidence for this has also been shown in oral health surveys of three- and five-year-olds.2,7 A study in Glasgow showed caries in the most deprived areas to be 32% compared with 16% in the least deprived areas.15 Admissions to hospital primarily for dental caries is also more likely to involve children from deprived areas compared with more affluent areas. Data from HES (Hospital Episodes Statistics) 1997-2006, showed that this was the case and that 80% of all admissions involved extractions.16 Studies have also revealed that ethnic disparities in caries experience is more likely to depend on the population studied and so comparisons are limited. Studies in the UK have shown significantly higher caries experience among pre-school children from South Asian backgrounds.17 There is little published information concerning caries experience in White Eastern Europeans, although a study concerning the oral health of pre-school children in East London showed White Eastern European, Bangladeshi and Pakistani children had significantly poorer oral health than their White British counterparts.18 The 2017 oral health survey of five-year-olds found that Eastern European and Chinese children had significantly higher decay rates than those in other groups.7
Our study suggests further evidence of oral health inequalities experienced by pre-school children in more deprived groups and among some ethnic groups, in particular Other White communities. It also underlines the value of routine collected data in informing local strategies. Caries is a preventable disease and it is very concerning that children as young as two and three years are being admitted to New Cross Hospital for elective extractions, often involving posterior deciduous molars. There is evidence that dental caries, once established, continue to rise throughout childhood into adulthood, which reinforces the case for oral health prevention or in establishing early intervention to stop the disease as soon as possible. This could be achieved through culturally sensitive oral health programmes, in addition to following general evidence-based preventive approaches, as recommended in the Department of Health's 'Delivering better oral health: an evidence-based toolkit for prevention'.19 This document provides guidance for primary care teams on oral health assessments, age-appropriate preventive advice and the importance of supervised toothbrushing with fluoride toothpaste, and would be appropriate for use with pre-school children from deprived areas and some ethnic groups, including Other White communities. Other health improvement programmes such as Public Health England's 'sugar smart' initiative and the government's sugar levy, primarily aimed at reducing obesity through reductions in sugar consumption, would also help reduce levels of dental decay. At local and national level, dental commissioners are being encouraged to support the UK-wide 'dental check by one' (DCby1) campaign launched by the British Society for Paediatric Dentistry with the Office of the Chief Dental Officer, which aims to increase awareness of the importance of early dental attendance for children aged zero to two years.20
We have limited information about the numbers of this highly selective group of patients that were born and lived in Wolverhampton or of those that might have lived elsewhere before moving to the area prior to their DGA. Population estimates for the years 2013-2016 show that the numbers of two- and- three-year-olds living in Wolverhampton was fairly stable at around 7,000 per annum, with a slight increase in numbers from 2014.21 We also have limited information about the dental care the children received before their DGA which would be valuable information for future planning of services in Wolverhampton. However, it is very unlikely that many will have visited a dentist before they were seen as an emergency by a GDP in Wolverhampton prior to a referral for a DGA. It is reported that less than 12% of children attend a dentist before their second birthday.3 It is surprising that such high levels of caries were seen in these patients, in view of the fact that Wolverhampton has a fluoridated water supply beneficial for dental health and such high rates are contrary to that seen in the general three-year-old population in Wolverhampton, where prevalence of decay is 15% (England = 12%) and the d3mft is 2.06 (England = 3.07). There are likely to be several reasons for this, including the fact that many children may not have received tap water routinely or had moved to Wolverhampton from non-fluoridated areas before referral. Another reason could be due to cultural practices, including prolonged use of feeding bottles containing cariogenic fruit juices or milk sweetened with sugar or honey, as has been reported in a study in Greater Manchester.22 Unfortunately in our study, no data were collected with regards to weaning and drinking habits to assess whether parents were aware of safe baby drinks and food. This emphasises the importance of applying culturally sensitive programmes as recommended in the toolkit on 'Delivering better oral health', including advice on the use of free-flow cups from one year of age and weaning foods that are sugar free.19 A further limitation concerns the small numbers of children treated in some of the 17 ethnic groups used at New Cross. These were collapsed down to seven broader ethnic groups to improve statistical powers, but in doing so, any disparities existing among the different sub-groups could be missed, which might have an effect on caries experience due to cultural, religious or educational status.
Conclusion
Significant numbers of two- and three-year-olds required general anaesthetic for dental extractions due to caries in Wolverhampton. High caries levels were associated with relative social deprivation and ethnicity. Reducing oral health inequalities may be considered with culturally sensitive oral health programmes educating mothers of very young children in relation to dental caries and the need to undergo regular dental assessment.
References
Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2015. A report on the prevalence and severity of dental decay. 2016. Available at https://www.gov.uk/government/statistics/oral-health-survey-of-5-year-old-children-2014-to-2015 (accessed February 2019).
Public Health England. Dental public health epidemiology programme: Oral Health survey of three-year-old children 2013. A report on the prevalence and severity of dental decay. 2014. Available at https://www.gov.uk/government/publications/oral-health-survey-of-3-year-old-children-2013 (accessed February 2019).
Public Health England. Health matters: child dental health. 2017. Available at https://www.gov.uk/government/publications/health-matters-child-dental-health/health-matters-child-dental-health (accessed February 2019).
Knapp R, Marshman Z, Rodd H. Treatment of dental caries under general anaesthetic in children. BDJ Team 2017; 4: 17116.
Rodd H, Hall M, Deery C, Gilchrist F, Gibson B J, Marshman Z. 'I felt weird and wobbly'. Child-reported impacts associated with a dental general anaesthetic. Br Dent J 2014; 216: E17.
Selwitz R H, Ismail A I, Pitts N B. Dental caries. Lancet 369: 51-59.
Public Health England. National Dental Epidemiology Programme for England: oral health survey of five-year-old children 2017. A report on the inequalities found in prevalence and severity of dental decay. 2018. Available at https://www.gov.uk/government/statistics/oral-health-survey-of-5-year-old-children-2017 (accessed February 2019).
Hosey M T, Bryce J, Harris P, McHugh S, Campbell C. The behaviour, social status and number of teeth extracted in children under general anaesthesia: a referral centre revisited. Br Dent J 2006; 200: 331-334.
Watt R, Sheiham A. Inequalities in oral health: a review of the evidence and recommendations for action. Br Dent J 1999; 187: 6-12.
Wolverhampton City Council. Research and Information Briefing Note: 2011 Census 4th Release-Wolverhampton Results. 2011.
Royal College of Surgeons. UK National Clinical Guidelines in Paediatric Dentistry. Guidelines for the Use of General Anaesthesia (GA) in Paediatric Dentistry. 2008. Available at https://www.rcseng.ac.uk/-/media/files/rcs/fds/publications/guideline-for-the-use-of-ga-in-paediatric-dentistry-may-2008-final.pdf (accessed February 2019).
Department for Communities and Local Government. The English Index of Multiple Deprivation (IMD) 2015-Guidance. 2015. Available at https://www.gov.uk/government/statistics/english-indices-of-deprivation-2015 (accessed February 2019).
Office for National Statistics. DC2101EW-Ethnic group by sex by age (Wolverhampton). 2011. Available at https://www.nomisweb.co.uk/census/2011/dc2101ew (accessed February 2019).
Tickle M, Moulding G, Milsom K, Blinkhorn A. Dental caries, contact with dental services and deprivation in young children: their relationship at a small area level. Br Dent J 2000; 189: 376-379.
McMahon A D, Blair Y, McCall D R, Macpherson L M. The dental health of three-year-old children in Greater Glasgow, Scotland. Br Dent J 2010; 209: E5.
Moles D R, Ashley P. Hospital admissions for dental caries in children: England 1997-2006. Br Dent J 2009; 206: E14.
Grey M, Morris A J, Davies J. The oral health of South Asian five-year-old children in deprived areas of Dudley compared with White children of equal deprivation and fluoridation status. Community Dent Health 2000; 17: 243-245.
Delgado-Angulo E K, Bernabé E, Marcenes W. Ethnic inequalities in dental caries among adults in East London. J Public Health 2016; 38: e55-e62.
Public Health England. Delivering better oral health: an evidence based toolkit for prevention. Third edition. 2017. Available at https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/605266/Delivering_better_oral_health.pdf (accessed February 2019).
British Society of Paediatric Dentistry. Dental Check by One. Available at https://www.bspd.co.uk/Resources/Dental-Check-by-One (accessed February 2019).
Office for National Statistics. Population estimates: analysis tool. 2017. Available at https://www.ons.gov.uk/peoplepopulationandcommunity/populationandmigration/populationestimates/datasets/populationestimatesanalysistool (accessed February 2019).
Davies G M, Blinkhorn F A, Duxbury J T. Caries among 3-year-olds in Greater Manchester. Br Dent J 2001; 190: 381-384.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harper, R., Nevill, A., Senghore, N. et al. Socioeconomic and ethnic status of two- and three-year-olds undergoing dental extractions under general anaesthesia in Wolverhampton, 2011-2016. Br Dent J 226, 349–353 (2019). https://doi.org/10.1038/s41415-019-0029-9
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0029-9
This article is cited by
-
Do paediatric patient-related factors affect the need for a dental general anaesthetic?
British Dental Journal (2022)
-
Providing sealants at the general anaesthetic assessment visit for children requiring caries-related dental extractions under general anaesthetic: a pilot randomised controlled trial
British Dental Journal (2021)
-
Childhood caries and hospital admissions in England: a reflection on preventive strategies
British Dental Journal (2021)
-
A rapid review of variation in the use of dental general anaesthetics in children
British Dental Journal (2020)