Abstract
Objectives A study of hospital admissions for diseases of pulp and periapical tissues in NHS Grampian and the effects of socioeconomic, geographic location and primary dental care availability on hospital admissions.
Design Retrospective analysis of hospitalisation data from NHS Grampian Health Intelligence database for the five-year period (1 January 2011 to 31 December 2015), if their primary diagnosis was disease of the pulp or periapical tissues. The influence of the Scottish Index of Multiple Deprivation (SIMD) scores on hospital admissions for pulp or periapical diseases were assessed and compared. Data from general dental practitioners (GDPs) providing primary care were obtained from the National Services Scotland practitioner services board.
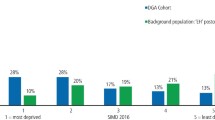
Results There were 963 admissions to NHS Grampian hospitals over the five-year period. The most frequent hospitalisation admission code was K047 'periapical abscess without sinus', accounting for 59.3% of all admissions. Hospital admissions decreased from 185 in 2011 to 122 in 2015, and coincided with a 50% rise in the number of GDPs providing primary care dentistry within the region (171 in 2011 to 256 in 2015). SIMD 5 (least deprived) had the greatest number of admissions (68) in 2011 compared with the most deprived (11). In 2015, SIMD 4 had the most admissions (41) compared to SIMD 1 (12).
Conclusion A reduction in hospital admissions for pulp/periapical abscesses appears to coincide with an increase in GDPs providing primary care dental services. Barriers to providing dental treatment in primary care should be minimised to reduce the burden of care on NHS hospitals for preventable dental diseases such as periapical abscesses.
Similar content being viewed by others
Key points
-
Highlights the socioeconomic impact of dental disease according to the Scottish Index of Multiple Deprivation and its link to hospitalisations for pulp/periapical disease in the NHS Grampian region.
-
Highlights the extensive burden on NHS secondary care resources in treating what is an entirely preventable dental disease and therefore requiring intervention in the form of education and prevention for patients.
-
Discusses the link in a decrease in hospitalisations for pulp/periapical diseases over a five-year period with the increase in the number of GDPs providing primary care services in NHS Grampian.
Introduction
NHS Grampian serves a population of half a million patients, stretching over a huge geographic area of over 3,000 square miles. Issues regarding access to dentistry are unique and incomparable to many other regions of the UK. Provision of preventative dentistry and quality endodontic care is vital to prevent and reduce the incidence of dento-alveolar infections, facial cellulitis and the associated sequelae including hospitalisation and general anaesthetic surgical treatment. In England, recent data have suggested a worrying trend of increased incidence of such admissions and it has been suggested that the current NHS dentistry funding system may have an element of responsibility for this.1
The Scottish Dental Access Initiative was introduced in 2000 in order to address the poor availability of NHS primary care dentistry in Scotland. Grants were offered to European Union dentists to set up new, and take over current, dental practices in order to increase registrations of NHS patients. This has seen a huge increase in the number of NHS dentists in previously 'barren' areas such as Aberdeen City, Shire and Moray.
Rural communities face difficulties in not only a lack of general dental practitioners (GDPs) and increased distances to reach dental practices, but travel and public transport issues may lead to a reduced level of primary care dental service. This is especially pertinent in a region such as NHS Grampian. Distance and transport can also be a barrier when it comes to the provision of specialist referral services, making secondary care potentially more difficult to access for a rural demographic of patients. Knowledge of the geographic source of patients undergoing hospitalisation could benefit future planning for regionalised, specialist-led endodontic services as part of a managed clinical network in NHS Grampian.
Socioeconomic factors have previously been shown to influence the incidence of hospitalisation of paediatric patients for dental care.2 The most deprived quintile of children in England were shown to be twice as likely to be hospitalised for dental care as the least deprived. The Grampian region has significant variation in socioeconomic status and, therefore, data assessing the influence of the Scottish Index of Multiple Deprivation (SIMD) score on incidence of hospitalisations would be a useful comparison with previously reported data.
The World Health Organisation International Classification of Diseases (ICD) provides a system of disease classification, to promote international comparability in collection and processing of epidemiological data.
Shah et al.3 have previously investigated the trends of hospitalisation for primary diagnosis of periapical abscess with/without sinus involvement (K046/7), across the USA from 2000-2008. This study demonstrated an increasing burden on hospital services, with over 61,000 hospitalisations and 66 deaths over the time period, highlighting the severity of the issue.
The aim of this study was to compare the pattern of hospital admissions in NHS Grampian between 2011-2015 and the effect of quintile deprivation and geographic location on admissions. These data were compared to the level of primary care services provided by GDPs in the region to determine if there was any form of relationship between the data.
UK hospitalisations have been assessed in children, also using the same ICD coding system.2 This paper looked at data for the time period 1997-2006 using the inclusive ICD codes K00 to K14: a dental condition. It demonstrated the huge frequency of childhood hospitalisation for caries and extractions. Over 470,000 children were hospitalised over the time period for dental issues across England. The code K04 represents diagnosis of disease of the pulp and periapical tissues; directly linked to endodontic disease and preventable by successful hygiene advice, conservation therapy and high-quality endodontic treatment. This category would represent the sequelae of inadequate or incomplete endodontic management of the dentition.
Method
Data on hospital activity were extracted from the NHS Grampian Health Intelligence database for the five-year period from 1 January 2011 to 31 December 2015. For the purpose of this investigation, data were extracted if the following inclusion criteria were fulfilled:4
- 1.
The patient was admitted to an NHS Grampian hospital
- 2.
Their primary diagnosis was disease of the pulp or periapical tissues (International Classification of Diseases tenth revision, ICD-10, code K04).
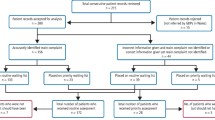
Once extracted, these data underwent validation checks and duplicate records were removed. The temporal change between each year was assessed to determine any pattern developing. The data relating to the number of primary care GDPs in the NHS Grampian region were obtained from the practitioner services board, for the time period of the study.
The data were assessed and compared not only for any temporal change but also for the effect of SIMD quintile deprivation score and geographic location (determined by postcode). In order to compare incidence fairly between highly populous postcodes and remote regions, a value was obtained which represented the relative risk per population in each area; for example, one in 300 people were admitted in AB10 (Aberdeen City) over the time period, versus one in 600 in AB37 (Aberdeenshire).
Results
General characteristics
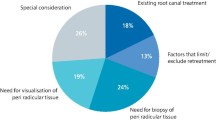
There were 963 admissions to NHS Grampian hospitals between 2011 and 2015 (five-year period) under the code K04 (diseases of the pulp and periapical tissues). Of the various diagnosis codes within the K04, the most frequent admission code was K047 'periapical abscess without sinus', accounting for 59.3% of all admissions within this category.
Temporal changes
Over the five-year time period between 2011 and 2015, admissions to NHS Grampian hospitals for disease of the pulp or periapical tissues (primary diagnosis) decreased from 185 in 2011 to 122 in 2015. This reduction has coincided with a 50% rise in the number of GDPs providing primary care dentistry within the region (171 in 2011 to 256 in 2015). Figure 1 indicates how the reduction in hospital admissions appears to follow the significant year-by-year increase in GDP numbers.
Relative deprivation
The data were obtained and different SIMD groups were compared for admission rates for each year of the study. The group contributing the greatest number of admissions in 2011 was SIMD 5 (least deprived) which had 68 admissions in 2011 compared with 11 from the most deprived. The data were grouped more closely in 2015 with the highest contributor, the fourth least deprived quintile with 41 compared to the SIMD 1 with 12 admissions.
Geographical analysis (2011-2015 inclusive)
Analysis of geographic locations of home addresses of patients admitted allowed a map to be developed. This allowed the calculation of risk per population per postcode area for admission to hospital for disease of pulp/periapical abscesses. For ease of visibility, this was a split between Aberdeen City and the rural regions.
Population figures were obtained for each postcode within the Grampian region and, therefore, a calculation was undertaken to assess the relative risk per population. This was important due to the high variations in population; for example, AB15 postcode: 35,616 residents versus AB36: 500 residents. The areas at the highest risk for admission due to disease of pulp/periapical tissues were city centre postcodes AB11, 12, 23 and 24, along with rural areas AB34 and AB54 (Figs 2 and 3). The southern part of Aberdeenshire shows a high risk of admission with a risk of one per 400-500 people.
Discussion
The data can be interpreted but caution should be applied when making assumptions.
Clearly, in NHS Grampian, in the population assessed in this study (462,786), there is a high incidence of hospital admissions for disease of the pulp/periapical tissues; 976 over the period 2011-2015. This represents an overall risk of one admission per 810 of the population. This level of admission to hospital will place a high burden on NHS services and economic resources, for what generally should be a preventable condition. Promisingly, there appears to be a temporal reduction in the incidence of admissions between the time period 2011-2015. This has coincided with a huge increase in the number of primary care independent GDPs within the region. The increase in primary care dental services, the ideal place for prevention and treatment of such conditions, may have reduced the need for unregistered patients to rely on hospital A&E services along with oral and maxillofacial surgery (OMFS) departments. This may be unsubstantiated however, with future assessment required to confirm a stable reduction in numbers and upkeep of GDP provision.
The use of primary care 'out of hours' dental emergency services has not been considered in the present study. A trend in the region over the studied time period has been for a region-wide service provided by the public dental services (PDS) in Aberdeen City and Shire for patients to access 'out of hours' emergency care, rather than independent practices providing their own service. This expanded PDS service may have also impacted the figures, providing a reduced burden on the hospital admissions in A&E and OMFS.
Another potential factor within the region may be a reduction in transient working population, linked to the oil and gas sector, who may not seek primary care dental services in the case of an acute dental emergency (perhaps due to residential links to other parts of the UK). The downturn in the industry may have reduced this demographic and perhaps meant a reduction in the use of secondary medical care for acute dental emergencies.
Previous research on hospital admissions for dental care in children has shown an increased risk for admission for the most deprived quintiles of society, with a reduction in risk association with reduced deprivation. The numbers obtained in this study are at odds with this as (all ages), in 2011, a significantly higher number of SIMD 5 and 4 were being admitted for diseases of pulp and periapical tissues compared to SIMD 1 (Fig. 4). The Aberdeen City and Shire has, in recent decades, been a prosperous and financially successful region with high employment due to the oil and gas industry. There may be higher representation of the least deprived quintiles within the region, thereby skewing the incidence of hospitalisations. Data on admissions for specific age groups were not available; therefore, it was not possible to determine which age groups are most at risk, and potentially need to be targeted for prevention and treatment. The Scottish 'Childsmile' scheme has been rolled out over the past decade and beyond, and this may be influencing the incidence of childhood caries as well as potentially reducing emergency admissions such as those presented in this study.
Geographic distribution of the patients undergoing hospitalisation showed a number of regions with a higher risk of admission for endodontic-related issues. Perhaps unsurprisingly, inner city regions showed above average risk, while western and southern Aberdeenshire showed greater risk also. The regional plan for the provision of secondary care endodontic services includes improving geographic accessibility to care, via a network of dentists with enhanced skills (DwES) in suitable remote locations, for the widespread population.
Comparative data show that the incidence of admissions for periapical abscess with or without sinus (K046/47) in NHS Grampian is relatively higher than data obtained in the USA over an eight-year period by Shah et al.3 Six hundred and twenty-five admissions were recorded for a population of 500,000 in Grampain, whereas in the USA (population of over 320,000,000) there were 61,439 over eight years. This suggests that the population in the UK is over six times more likely to be hospitalised due to periapical abscesses. However, consideration has to be given to the fact that there may be different systems and costs associated with deterring the use of hospitals in 'borderline' cases in the USA compared to the UK.
Conclusion
An entirely preventable condition such as a periapical abscess should ideally be managed in primary care. Prevention, caries management, endodontic services, and oral surgery from GDPs should be able to prevent or manage the vast majority of cases. Improved access to secondary care endodontic services will provide an undoubted benefit and may reduce the economic and resource burden on NHS hospitals due to periapical abscesses and related conditions. In the current climate, patients are less likely to undergo extractions of teeth when compared with two or three decades ago. This factor further emphasises the need for minimising barriers to primary care and specialist-led secondary care endodontic services.
References
Thomas S J, Atkinson C, Hughes C, Revington P, Ness A R. Is there an epidemic of admissions for surgical treatment of dental abscesses in the UK? BMJ 2008; 336: 1219-1220.
Moles D R, Ashley P. Hospital admissions for dental care in children: England 1997-2006. Br Dent J 2009; 206: E14.
Shah A C, Leong K K, Lee M K, Allareddy V. Outcomes of hospitalizations attributed to periapical abscess from 2000 to 2008: a longitudinal trend analysis. J Endod 2013; 39: 1104-1110.
World Health Organisation. International Classification of Diseases: Version 10. 2016. Available at https://icd.who.int/browse10/2016/en (accessed May 2019).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Anderson, W., Ahmed, H. A retrospective analysis of hospitalisation for diseases of the pulp and periapical tissues in NHS Grampian 2011-2015: geographic, socioeconomic and increased primary care availability effects. Br Dent J 226, 951–954 (2019). https://doi.org/10.1038/s41415-019-0383-7
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41415-019-0383-7
This article is cited by
-
Childhood caries and hospital admissions in England: a reflection on preventive strategies
British Dental Journal (2021)