Abstract
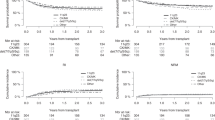
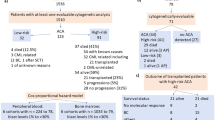
Allogeneic hematopoietic cell transplantation (allo-HCT) remains the best consolidation strategy for acute myeloid leukemia (AML) with complex karyotype (CK). However, CK is a heterogenous and highly diverse entity. Numerical abnormalities have been associated with a controversial prognosis and AML with only multiple numerical abnormalities known as pure hyperdiploid karyotype (HDK) may have a distinct prognosis after allo-HCT compared to non-pure HDK CK AML. A total of 236 patients were identified within the EBMT registry as having HDK comprising 95 pure (pHDK) and 141 with other cytogenetic abnormalities (HDK+). The 2-year probability of leukemia-free survival (LFS) was 50% for pHDK and 31% for HDK+ (p = 0.003). The 2-year probability of overall survival (OS) was 57% for pHDK and 36% for HDK+ (p = 0.007). The 2-year cumulative incidence of relapse (RI) was 22% for pHDK and 44% for HDK+ (p = 0.001). The 2-year probability of graft-versus-host disease (GvHD)-free and relapse-free survival (GRFS) was 36% for pHDK and 21% for HDK+ (p = 0.01). On multivariate analysis, pHDK remained associated with significantly better LFS, OS and GRFS and lower RI (all p-values <0.004). pHDK AML constitutes probably a distinct cytogenetic entity from HDK+ or other non-hyperdiploid CK AML with better outcomes after allo-HCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets analyzed during the current study have been generated from ProMISe (Project Manager Internet Server), the international database coordinated by EBMT.
References
Cornelissen JJ, van Putten WL, Verdonck LF, Theobald M, Jacky E, Daenen SM, et al. Results of a HOVON/SAKK donor versus no-donor analysis of myeloablative HLA-identical sibling stem cell transplantation in first remission acute myeloid leukemia in young and middle-aged adults: benefits for whom? Blood. 2007;109:3658–66. https://doi.org/10.1182/blood-2006-06-025627.
Koreth J, Schlenk R, Kopecky KJ, Honda S, Sierra J, Djulbegovic BJ, et al. Allogeneic stem cell transplantation for acute myeloid leukemia in first complete remission: systematic review and meta-analysis of prospective clinical trials. JAMA. 2009;301:2349–61.
Dohner H, Estey EH, Amadori S, Appelbaum FR, Buchner T, Burnett AK, et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood. 2010;115:453–74. https://doi.org/10.1182/blood-2009-07-235358.
Dohner H, Weisdorf DJ, Bloomfield CD. Acute myeloid leukemia. N Engl J Med. 2015;373:1136–52. https://doi.org/10.1056/NEJMra1406184.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65. https://doi.org/10.1182/blood-2009-11-254441.
Grimwade D, Ivey A, Huntly BJ. Molecular landscape of acute myeloid leukemia in younger adults and its clinical relevance. Blood. 2016;127:29–41. https://doi.org/10.1182/blood-2015-07-604496.
Schoch C, Kern W, Kohlmann A, Hiddemann W, Schnittger S, Haferlach T. Acute myeloid leukemia with a complex aberrant karyotype is a distinct biological entity characterized by genomic imbalances and a specific gene expression profile. Genes Chromosomes Cancer. 2005;43:227–38. https://doi.org/10.1002/gcc.20193.
Baron F, Labopin M, Niederwieser D, Vigouroux S, Cornelissen JJ, Malm C, et al. Impact of graft-versus-host disease after reduced-intensity conditioning allogeneic stem cell transplantation for acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European group for blood and marrow transplantation. Leukemia. 2012;26:2462–8. https://doi.org/10.1038/leu.2012.135.
Schlenk RF, Dohner K, Mack S, Stoppel M, Kiraly F, Gotze K, et al. Prospective evaluation of allogeneic hematopoietic stem-cell transplantation from matched related and matched unrelated donors in younger adults with high-risk acutemyeloid leukemia: German-Austrian trial AMLHD98A. J Clin Oncol. 2010;28:4642–8. https://doi.org/10.1200/JCO.2010.28.6856.
Stelljes M, Beelen DW, Braess J, Sauerland MC, Heinecke A, Berning B, et al. Allogeneic transplantation as post-remission therapy for cytogenetically high-risk acute myeloid leukemia: landmark analysis from a single prospective multicenter trial. Haematologica. 2011;96:972–9. https://doi.org/10.3324/haematol.2011.041004.
Versluis J, Hazenberg CL, Passweg JR, van Putten WL, Maertens J, Biemond BJ, et al. Post-remission treatment with allogeneic stem cell transplantation in patients aged 60 years and older with acute myeloid leukaemia: a time-dependent analysis. Lancet Haematol. 2015;2:e427–436. https://doi.org/10.1016/S2352-3026(15)00148-9.
Bowen D, Groves MJ, Burnett AK, Patel Y, Allen C, Green C, et al. TP53 gene mutation is frequent in patients with acute myeloid leukemia and complex karyotype, and is associated with very poor prognosis. Leukemia. 2009;23:203–6. https://doi.org/10.1038/leu.2008.173.
Grimwade D, Walker H, Oliver F, Wheatley K, Harrison C, Harrison G, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1612 patients entered into the MRC AML 10 trial. The medical research council adult and children’s leukaemia working parties. Blood. 1998;92:2322–33.
Breems DA, Van Putten WL, De Greef GE, Van Zelderen-Bhola SL, Gerssen-Schoorl KB, Mellink CH, et al. Monosomal karyotype in acute myeloid leukemia: a better indicator of poor prognosis than a complex karyotype. J Clin Oncol. 2008;26:4791–7. https://doi.org/10.1200/JCO.2008.16.0259.
Haferlach C, Alpermann T, Schnittger S, Kern W, Chromik J, Schmid C, et al. Prognostic value of monosomal karyotype in comparison to complex aberrant karyotype in acute myeloid leukemia: a study on 824 cases with aberrant karyotype. Blood. 2012;119:2122–5. https://doi.org/10.1182/blood-2011-10-385781.
Poire X, Labopin M, Cornelissen JJ, Volin L, Richard Espiga C, Veelken JH, et al. Outcome of conditioning intensity in acute myeloid leukemia with monosomal karyotype in patients over 45 year-old: a study from the acute leukemia working party (ALWP) of the European group of blood and marrow transplantation (EBMT). Am J Hematol. 2015;90:719–24. https://doi.org/10.1002/ajh.24069.
Poire X, Labopin M, Polge E, Forcade E, Ganser A, Volin L, et al. Allogeneic stem cell transplantation using HLA-matched donors for acute myeloid leukemia with deletion 5q or monosomy 5: a study from the Acute Leukemia Working Party of the EBMT. Haematologica. 2020;105:414–23. https://doi.org/10.3324/haematol.2019.216168.
Poire X, Labopin M, Polge E, Volin L, Finke J, Ganser A, et al. The impact of concomitant cytogenetic abnormalities on acute myeloid leukemia with monosomy 7 or deletion 7q after HLA-matched allogeneic stem cell transplantation. Am J Hematol. 2020;95:282–94. https://doi.org/10.1002/ajh.25714.
Chilton L, Hills RK, Harrison CJ, Burnett AK, Grimwade D, Moorman AV. Hyperdiploidy with 49–65 chromosomes represents a heterogeneous cytogenetic subgroup of acute myeloid leukemia with differential outcome. Leukemia. 2014;28:321–8. https://doi.org/10.1038/leu.2013.198.
Bacigalupo A, Ballen K, Rizzo D, Giralt S, Lazarus H, Ho V, et al. Defining the intensity of conditioning regimens: working definitions. Biol Blood Marrow Transplant. 2009;15:1628–33. https://doi.org/10.1016/j.bbmt.2009.07.004.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1. https://doi.org/10.1038/bmt.2015.305.
Dohner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood. 2022;140:1345–77. https://doi.org/10.1182/blood.2022016867.
Luquet I, Lai JL, Barin C, Baranger L, Bilhou-Nabera C, Lippert E, et al. Hyperdiploid karyotypes in acute myeloid leukemia define a novel entity: a study of 38 patients from the Groupe Francophone de Cytogenetique Hematologique (GFCH). Leukemia. 2008;22:132–7. https://doi.org/10.1038/sj.leu.2404974.
Lazarevic V, Rosso A, Juliusson G, Antunovic P, Rangert-Derolf A, Lehmann S, et al. Prognostic significance of high hyperdiploid and triploid/tetraploid adult acute myeloid leukemia. Am J Hematol. 2015;90:800–5. https://doi.org/10.1002/ajh.24091.
Lazarevic VL, Rosso A, Juliusson G, Antunovic P, Derolf AR, Deneberg S, et al. Incidence and prognostic significance of isolated trisomies in adult acute myeloid leukemia: a population-based study from the Swedish AML registry. Eur J Haematol. 2017;98:493–500. https://doi.org/10.1111/ejh.12861.
Farag SS, Archer KJ, Mrozek K, Vardiman JW, Carroll AJ, Pettenati MJ, et al. Isolated trisomy of chromosomes 8, 11, 13 and 21 is an adverse prognostic factor in adults with de novo acute myeloid leukemia: results from Cancer and Leukemia Group B 8461. Int J Oncol. 2002;21:1041–51.
Wolman SR, Gundacker H, Appelbaum FR, Slovak ML.Southwest Oncology G. Impact of trisomy 8 (+8) on clinical presentation, treatment response, and survival in acute myeloid leukemia: a Southwest Oncology Group study. Blood. 2002;100:29–35. https://doi.org/10.1182/blood.v100.1.29. e-pub ahead of print 2002/06/19.
Schoch C, Haase D, Fonatsch C, Haferlach T, Loffler H, Schlegelberger B, et al. The significance of trisomy 8 in de novo acute myeloid leukaemia: the accompanying chromosome aberrations determine the prognosis. German AML Cooperative Study Group. Br J Haematol. 1997;99:605–11. https://doi.org/10.1046/j.1365-2141.1997.4473257.x.
Paulsson K, Johansson B. Trisomy 8 as the sole chromosomal aberration in acute myeloid leukemia and myelodysplastic syndromes. Pathol Biol. 2007;55:37–48. https://doi.org/10.1016/j.patbio.2006.04.007.
Schoch C, Kohlmann A, Dugas M, Kern W, Schnittger S, Haferlach T. Impact of trisomy 8 on expression of genes located on chromosome 8 in different AML subgroups. Genes Chromosomes Cancer. 2006;45:1164–8. https://doi.org/10.1002/gcc.20380.
Arber DA, Orazi A, Hasserjian RP, Borowitz MJ, Calvo KR, Kvasnicka HM, et al. International consensus classification of myeloid neoplasms and acute leukemias: integrating morphologic, clinical, and genomic data. Blood. 2022;140:1200–28. https://doi.org/10.1182/blood.2022015850.
Alpermann T, Haferlach C, Eder C, Nadarajah N, Meggendorfer M, Kern W, et al. AML with gain of chromosome 8 as the sole chromosomal abnormality (+8sole) is associated with a specific molecular mutation pattern including ASXL1 mutations in 46.8% of the patients. Leuk Res. 2015;39:265–72. https://doi.org/10.1016/j.leukres.2014.11.026.
Bhatnagar B, Eisfeld AK, Kohlschmidt J, Mrozek K, Nicolet D, Papaioannou D, et al. Clinical and molecular characterization of patients with acute myeloid leukemia and sole trisomies of chromosomes 4, 8, 11, 13 or 21. Leukemia. 2020;34:358–68. https://doi.org/10.1038/s41375-019-0560-3.
Liu J, Han W, Cai X, Wang Z, Cao L, Hua H, et al. Molecular genetic and clinical characterization of acute myeloid leukemia with trisomy 8 as the sole chromosome abnormality. Hematology. 2022;27:565–74. https://doi.org/10.1080/16078454.2022.2071799.
Zong X, Yao H, Wen L, Ma L, Wang Q, Yang Z, et al. ASXL1 mutations are frequent in de novo AML with trisomy 8 and confer an unfavorable prognosis. Leuk Lymphoma. 2017;58:204–6. https://doi.org/10.1080/10428194.2016.1179296.
Dicker F, Haferlach C, Kern W, Haferlach T, Schnittger S. Trisomy 13 is strongly associated with AML1/RUNX1 mutations and increased FLT3 expression in acute myeloid leukemia. Blood. 2007;110:1308–16. https://doi.org/10.1182/blood-2007-02-072595.
Herold T, Metzeler KH, Vosberg S, Hartmann L, Rollig C, Stolzel F, et al. Isolated trisomy 13 defines a homogeneous AML subgroup with high frequency of mutations in spliceosome genes and poor prognosis. Blood. 2014;124:1304–11. https://doi.org/10.1182/blood-2013-12-540716.
Silva FP, Lind A, Brouwer-Mandema G, Valk PJ, Giphart-Gassler M. Trisomy 13 correlates with RUNX1 mutation and increased FLT3 expression in AML-M0 patients. Haematologica. 2007;92:1123–6. https://doi.org/10.3324/haematol.11296.
Kuwatsuka Y, Miyamura K, Suzuki R, Kasai M, Maruta A, Ogawa H, et al. Hematopoietic stem cell transplantation for core binding factor acute myeloid leukemia: t(8;21) and inv(16) represent different clinical outcomes. Blood. 2009;113:2096–103. https://doi.org/10.1182/blood-2008-03-145862.
Poire X, Labopin M, Polge E, Blaise D, Chevallier P, Maertens J, et al. Hematopoietic stem cell transplantation for adult patients with isolated NPM1 mutated acute myeloid leukemia in first remission. Am J Hematol. 2019;94:231–9. https://doi.org/10.1002/ajh.25355.
Potdar R, Varadi G, Fein J, Labopin M, Nagler A, Shouval R. Prognostic scoring systems in allogeneic hematopoietic stem cell transplantation: where do we stand? Biol Blood Marrow Transpl. 2017;23:1839–46. https://doi.org/10.1016/j.bbmt.2017.07.028.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9. https://doi.org/10.1182/blood-2005-05-2004.
Sorror ML, Storb RF, Sandmaier BM, Maziarz RT, Pulsipher MA, Maris MB, et al. Comorbidity-age index: a clinical measure of biologic age before allogeneic hematopoietic cell transplantation. J Clin Oncol. 2014;32:3249–56.
Author information
Authors and Affiliations
Contributions
XP, AN, JE and MM wrote the manuscript; XP, ML, AN, JE and MM designed the study; XP, ML, AN, JE and MM analysed the data; EP, AG, GS, TGD, EF, JF, YC, CEB, IYA, MA, NK and IWB provide the data and reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Poiré, X., Labopin, M., Polge, E. et al. Allogeneic hematopoietic cell transplantation for acute myeloid leukemia with hyperdiploid complex karyotype. Bone Marrow Transplant 59, 264–269 (2024). https://doi.org/10.1038/s41409-023-02167-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02167-1