Abstract
Conditioning protocols for patients undergoing allogeneic hematopoietic cell transplantation (allo-HCT) are being developed continuously to improve their anti-leukemic efficacy and reduce their toxicity. In this study, we compared the conditioning protocol of fludarabine with melphalan 140 mg/m2 (FluMel) with conditioning protocols based on this same backbone but with an additional alkylating agent i.e., either fludarabine/BCNU (also known as carmustine)/melphalan (FBM), or fludarabine/thiotepa/melphalan (FTM) 110 mg/m2. We included 1272 adult patients (FluMel, n = 1002; FBM/FTM, n = 270) with acute myeloid leukemia (AML) with intermediate/poor cytogenetic risk in first complete remission (CR) from the registry of the EBMT Acute Leukemia Working Party. Despite patients in the FBM/FTM group were older (64.1 years vs. 59.8 years, p < 0.001) and had a worse Karnofsky performance score (KPS < 90, 33% vs. 24%, p = 0.003), they showed a better overall survival (OS) (2 y OS: 68.3% vs. 58.1%, p = 0.02) and less non-relapse mortality (NRM) (2 y NRM: 15.8% vs. 22.2%, p = 0.009) compared to patients treated with FluMel. No significant differences were observed in relapse incidence (RI) (2 y RI: 24.9% vs. 23.7%, p = 0.62). In conclusion, the addition of a second alkylating agent (BCNU/carmustine or thiotepa) to FluMel as FBM/FTM conditioning, improves OS in AML patients in first CR with intermediate/poor risk cytogenetics after allo-HCT.
Similar content being viewed by others
Introduction
Conditioning protocols for patients undergoing allogeneic hematopoietic cell transplantation (allo-HCT) are developing continuously and are assessed for efficacy and toxicity. Conditioning regimens have been intensified for increased killing of leukemia cells, but this has increased the risk of short- and long-term toxicities and high-intensity regimens cannot be tolerated by older patients [1]. The conditioning intensity has been shown to be a continuum in previous studies and a novel transplant conditioning intensity (TCI) score has been established [2]. In this study we compared from the ‘intermediate’ TCI score the conditioning protocol of fludarabine with the single alkylating agent melphalan (FluMel) with conditioning protocols based on this same backbone but with an additional alkylating agent i.e., either fludarabine/BCNU (also known as carmustine)/melphalan (FBM), or fludarabine/thiotepa/melphalan (FTM).
Conditioning with FluMel is a standard conditioning protocol in many centers and has been showed to have moderate toxicity and good anti-leukemic activity [3, 4]. Patients treated with FluMel have a similar relapse incidence than patients treated with classical myeloablative ablative conditioning (MAC) protocols Bu4Cy and FluBu4 and they show a lower relapse incidence than reduced intensity conditioning (RIC) protocol FluBu2 [4]. Lower relapse incidence and higher non-relapse mortality (NRM) was shown for patients receiving FluMel compared to patients treated with the lower-intensity conditioning protocol fludarabine/busulfan (FluBu2), although similar rates of leukemia-free survival (LFS) and overall survival (OS) were observed in patients with AML [5]. However, improved LFS and OS were observed in patients with MDS treated with FluMel compared to FluBu2 [6]. Using the registry of the Acute Leukemia Working Party (ALWP) from the European Society for Blood and Marrow Transplantation (EBMT), it was previously shown that FluMel had conferred a lower relapse rate, but higher NRM compared to patients conditioned with fludarabine/treosulfan (FluTreo) in patients with AML in complete remission (CR). However, patients had similar outcomes regarding OS and LFS [7].
To improve the anti-leukemic effect of conditioning without increasing toxicity, protocols combining two alkylating agents had been developed in the last few decades. For example, the FBM conditioning protocol was developed by adding BCNU to FluMel conditioning and by reducing the melphalan dose [8]. The conditioning protocol FBM has shown low toxicity and remarkable anti-leukemic activity not only in AML patients with active disease, but also in the second transplantation setting and in patients with multiple comorbidities [9,10,11]. Similarly, the FTM conditioning protocol was established by adding thiotepa to the FluMel backbone. Haplo-identical allo-HCT after conditioning with the FTM protocol has been well tolerated and effective for patients with AML/myelodysplastic syndromes (MDS) with low tumor burden [12, 13] and as a conditioning protocol for patients with multiple myeloma [14]. Hence, previous studies have shown that both conditioning protocols based on two alkylating agents (FBM or FTM) have adequate anti-leukemic activity and were suitable for older patients or those with co-morbidities including impaired lung function. Hence, both protocols were comparable regarding adjusted OS [15, 16].
In this registry-based study, we hypothesized that patients treated with conditioning based on the fludarabine and melphalan backbone with the addition of a second alkylating agent as BCNU (FBM) or thiotepa (FTM) and undergoing allo-HCT for AML with intermediate/poor cytogenetics in first CR would have better outcomes than patients receiving FluMel as conditioning.
Patient and methods
Study design
In this retrospective multicenter analysis, data were provided by the ALWP of the EBMT, a scientific society representing >600 transplant centers, mainly in Europe who report annually all consecutive allo-HCTs after patient authorization via informed consent, and approval of the study by the general assembly of the ALWP of the EBMT. We focused on (1) adult (aged >18 years) patients who received conditioning with FluMel (fludarabine, median 150 mg/m2; melphalan 140 mg/m2) or with FBM (fludarabine, median 150 mg/m2; BCNU 300–400 mg/m2 and melphalan 110 mg/m2) or with FTM (fludarabine, median 150 mg/m2; thiotepa 5–10 mg/kg and melphalan 110 mg/m2), (2) first allo-HCT from a matched sibling donor (MSD) or unrelated donor for patients with AML including secondary AML (secAML) in first CR, (3) AML with intermediate/poor cytogenetics risk, (4) transplantation date between January 1st, 2009 and December 31st, 2020, (5) with an unmanipulated peripheral blood graft (no in vitro T-cell depletion (TCD) and no bone marrow grafts). Patients undergoing haploidentical allo-HCT were excluded. Three hundred eighteen (25%) of the patients received an unrelated donor for which the HLA was incomplete or low resolution making impossible to calculate the high resolution mismatches on A, B, C, DRB1 and DQB1.
In previous single-center-based studies, it was shown that FBM and FTM protocols are comparable after adjusting for variables influencing mortality in multivariate analysis [16]. This was confirmed using EBMT registry-based data in a preliminary analysis of the present study. For this reason and knowing that BCNU and thiotepa are both alkylating agents, we decided to include FBM- and FTM-treated patients in the same group.
Statistical analysis
Outcome variables were defined following internal consensus guidelines [17]. Patient-, disease- and treatment-related characteristics were compared using the chi-square test for categorical data or the Mann–Whitney test for continuous data. Baseline characteristics were summarized using median, interquartile range (IQR), and range, for continuous data, and frequency and percentage for categorical data. OS was defined as the time from allo-HCT until death from any cause. LFS was defined as the time from allo-HCT to death from any cause, or relapse/progression, whichever occurred first. Relapse was defined as detection of disease via cytological and histological assessment after allo-HCT; death without prior relapse was considered as a competing risk for relapse and was denoted as NRM. For cumulative incidence of acute graft-versus-host disease (aGvHD) and chronic GvHD (cGvHD), death without aGvHD/cGvHD and relapse were considered as competing events. GvHD-free, relapse-free survival (GRFS) was defined as being alive with neither grade III–IV aGVHD nor severe cGVHD, relapse, or death from any cause post-HCT. Patients with no event were censored at the date of last follow-up. To allow for the difference in follow-up period between the 2 conditioning regimen groups, outcome was censored at 2 years post transplantation for all comparisons.
Univariate analyses were performed using Gray’s test for cumulative incidence functions and the log-rank test for OS, GRFS, and LFS. The Cox proportional-hazards model was used for multivariable regression analysis and included variables with unbalanced distribution between the two groups or factors known to predict outcomes. To allow for center differences, a random effect or frailty was introduced for each center into the models. Results were expressed as the hazard ratio (HR) with the 95% confidence interval (95% CI).
All tests were two sided. The Type I error was fixed at 0.05 for factors associated with time-to-event outcomes. Statistical analyses were performed with R 3.6.1 (R Development Core Team, Vienna, Austria) software packages.
Results
Patient and transplant characteristics
The patient and transplant characteristics of the 1272 AML patients are shown in Table 1. Prior to allo-HCT, 1002 (79%) patients received a conditioning with FluMel, and 270 (21%) patients received FBM/FTM. Before censoring at 2 years, the median follow-up was 2.6 years (95% CI, 2.2–2.9) in the FluMel and 2.0 years (95%CI, 1.6–2.2 years) in the FBM/FTM group, respectively. Patients in the FBM/FTM group were older compared to patients in the FluMel group (median age of 64.1 years vs. 59.8 years, p < 0.001). Compared with FluMel patients, those conditioned with FBM/FTM showed a significantly worse performance, with KPS < 90 (33% vs. 24% in FluMel, p = 0.003). Additional transplant characteristics such as secondary AML (21% vs. 14% in FluMel, p = 0.003), donor type (81% vs. 66% unrelated in FluMel, p < 0.0001) varied significantly between the groups. GvHD prophylaxis based on in vivo T-cell depletion (TCD) was similar between both groups (91% vs 92% in FluMel, p = 0.39) but the type of in vivo TCD differed significantly (82% ATG in FBM/FTM and 74% alemtuzumab in FluMel, p < 0.0001) (Table 1).
Analysis of outcomes in patients conditioned with FluMel compared to FBM/FTM
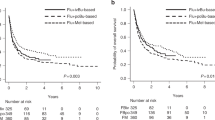
Results are shown in Tables 2–3 and Fig. 1. According to the univariate analysis (Table 2 and Fig. 1), patients conditioned with FBM/FTM had compared to patients treated with FluMel a better OS (2 y 68.3% vs. 58.1%, HR 0.7, 95%CI 0.52–0.94, p = 0.02), improved LFS (2 y: 59.4% vs. 54.1%, HR 0.78, 95%CI 0.61–0.99, p = 0.04) and decreased NRM (2 y: 15.8% vs. 22.2%, HR 0.56, 95%CI 0.36–0.86, p = 0.009) (Table 3). Several clinical parameters adversely influenced OS such as age (per 10 years) at allo-HCT (HR 1.19, 95%CI 1.05–1.35, p = 0.006), unrelated donor (HR 1.61, 95%CI 1.27–2.04, p < 0.001), poor cytogenetics (HR 1.71, 95%CI 1.39–2.1, p < 0.001) and KPS (HR for KPS < 90 1.43, 95%CI 1.13–1.79, p = 0.002) (Table 3).
Kaplan–Meier curves represent (a) overall survival and (b) leukemia-free survival by conditioning protocol. Cumulative incidences of (c) non-relapse mortality and (d) relapse by conditioning protocol. FluMel, fludarabine/melphalan; FBM, fludarabine/BCNU/melphalan; FTM, fludarabine/thiotepa/melphalan; Pts, patients; allo-HCT, allogeneic hematopoietic cell transplantation.
Conditioning with FluMel or FBM/FTM did not significantly influence either the cumulative incidence of relapse (2 y: 24.9% vs. 23.7%,HR 1.09, 95%CI 0.78–1.52, p = 0.62) (Table 3), aGvHD II–IV (100d: 36.9% vs. 22.3%, HR 1.42, 95%CI 0.94–2.15, p = 0.09), aGvHD III–IV (100d: 14.4% vs. 7.5%, HR 1.59, 95%CI 0.89–2.84, p = 0.11) or cGvHD (2 y: 34.5% vs. 32.3%, HR 0.82, 95%CI 0.61–1.11, p = 0.19) (Supplementary Table 1) in multivariable analysis. Cause of death was not significantly different in patients undergoing allo-HCT conditioned with FluMel compared to FBM/FTM (Supplementary Table 2).
Discussion
Due to the increasing age (and associated comorbidities) of patients undergoing allo-HCT, conditioning protocols are in continuous development to increase their anti-leukemic effect whilst not increasing toxicity [18]. Besides the success of unrelated donor and haploidentical allo-HCT as well as the rise in cellular therapy, the use of RIC in older patients is one of the most notable developments in allo-HCT field during the last decade [19, 20]. The most frequently used conditioning protocols are based on a purine analogue with immunosuppressive effects combined with an alkylating agent with myelosuppressive properties and stem cell toxicity. Some examples based on this combination are fludarabine/busulfan with a high TCI score [21,22,23], and fludarabine/treosulfan [24] and fludarabine/melphalan [25] with an intermediate TCI score.
One approach to improve the anti-leukemic effect (without adversely affecting toxicity) is to add a second alkylating agent and decrease the dosage of the first alkylating substance. With this approach, an additive/synergistic effect can be expected and several modern conditioning protocols have been developed such as thiotepa (8–15 mg/kg b.w.)/fludarabine (3–4 × 40 mg/m2)/treosulfan (3 × 12–14 mg/m2) [TFTreo] [26,27,28] as well as thiotepa (1–2 × 5 mg/kg b.w.)/busulfan (1–3 × 3.2 mg/kg b.w.)/fludarabine (3 × 50 mg/m2) [TBF] [29,30,31] as RIC and MAC protocols. Recent data show that patients treated with two alkylating agent chemotherapies (TBF) have less relapse incidence but the same NRM as patients treated with one alkylating agent chemotherapy (BuFlu or BF) [32]. In a registry-based EBMT study, TBF-MAC and TBF-RIC showed better anti-leukemic activity but higher NRM compared to BF-MAC and BF-RIC, resulting in similar OS [33]. However, intensification of RIC conditioning protocols as FLAMSA-Bu has not resulted in reduction of cumulative incidence of relapse or improved OS and disease-free survival compared to other fludarabine-based conditioning (FluMel + alemtuzumab, FluBu2 + alemtuzumab, FluBu2 + ATG) in randomized controlled clinical trials [34].
Using FluMel as a backbone, two conditioning protocols based on a two-alkylating agent approach have been developed by adding BCNU (carmustine) (FBM) [9] or by adding thiotepa (FTM) [12]. Both protocols have been shown to have good anti-leukemic activity and lower toxicity. However, they have not been compared to FluMel conditioning in clinical trials or in large registry-based studies to demonstrate improved outcome and similar toxicity.
In this study, we analyzed patient characteristics, outcomes, and cause of death in a large registry-based study on behalf of the ALWP of the EBMT including 1272 patients with AML with intermediated/poor cytogenetics in first CR. Patients conditioned with FBM/FTM showed better OS and LFS, and lower NRM despite the patients being older, having a worse KPS and receiving a graft from unrelated donors. All these features were associated with worse OS on multivariable analysis. We only included patients receiving standard melphalan dose in FluMel of 140 mg/m2 and in FBM/FTM of 110 mg/m2. So, we did not just compare the addition of a second alkylating agent to FluMel in our study but also the reduction of melphalan dose, which probably contributed to reducing the toxicity of the FBM/FTM conditioning protocols, while the addition of the second alkylating agent maintains the anti-leukemic activity, as seen by similar relapse incidence in both conditioning groups.
Older patients and with reduced performance score received two-alkylating based protocols FBM/FTM in our cohort than the one-alkylating based protocol FluMel. We interpret these data as center- or region-dependent. Of note, there were regional differences in the use of conditioning protocols, which might reflect differences in patient populations and transplantation procedures. Patients conditioned with FluMel were treated in the United Kingdom (74.9%), Belgium (9.4%), Germany (4.7%) and Czech Republic (3.8%). However, patients conditioned with FBM/FTM were treated predominantly in Germany (99.3%).
This study has several limitations. We analyzed data from patients conditioned with FluMel and FBM/FTM, included in the EBMT registry. Due to the retrospective nature of the study, patient cohorts were not balanced with respect to patient characteristics and transplant conditions, which could have influenced on outcomes despite the adjustment in multivariable models. Although a randomized controlled trial would be the gold standard to elucidate which conditioning protocol is the most suitable for which patient population, such studies are very challenging to perform due to the relatively small number of patients. In another hand, the registry nature of this analysis reflects the real practice of the centers. Nevertheless, although patients transplanted with FBM/FTM were older and had a worse KPS, which frequently negatively influences outcomes, they showed prolonged OS. Differences in GvHD prophylaxis were observed in both cohorts, which might have influenced GvHD incidence and, hence, patient outcomes. There were no differences in the use of in vivo TCD between groups (92% in FluMel and 91% in FBM/FTM, p = 0.39). However, patients conditioned with FluMel more often received an in vivo TCD based on alemtuzumab (74%) compared with patients conditioned with FBM/FTM, who received more frequently ATG (82%, p < 0.001). No statistically significant differences were observed in the incidence of aGvHD II–IV and III–IV and cGvHD. However, we cannot exclude that differences on the substances employed (alemtuzumab or ATG) for in vivo TCD may have had an impact on OS influencing other post allo-HCT complications. It has been described that in vivo TCD as GvHD prophylaxis with alemtuzumab in combination FluMel-based conditioning is associated with higher likelihood of infectious complications as well as mixed chimerism, for which a proportion of these patients received DLI [35, 36]. In addition, data about gene mutations or MRD status, which might have impacted patient outcome, were not available in the EBMT registry for the statistical analysis. Other variables influenced by regional differences and not included in our EBMT registry as patient selection or supportive care modalities may have impacted the outcome of patients after conditioning with FluMel or FBM/FTM. Therefore, our data should be interpreted with caution in the absence of randomized controlled clinical trials.
In conclusion, despite older age, worse KPS and receiving more often grafts from unrelated donors, the addition of a second alkylating agent (BCNU/carmustine or thiotepa) to FluMel as FBM/FTM conditioning improves OS in patients with AML with intermediate/poor risk cytogenetics in first CR.
Data availability
The datasets generated during and/or analyzed during the current study are available upon reasonable request from the corresponding authors.
References
Granot N, Storb R. History of hematopoietic cell transplantation: challenges and progress. Haematologica. 2020;105:2716–29.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transpl. 2020;55:1114–25.
Ciurea SO, Kongtim P, Varma A, Rondon G, Chen J, Srour S, et al. Is there an optimal conditioning for older patients with AML receiving allogeneic hematopoietic cell transplantation? Blood. 2020;135:449–52.
Eapen M, Brazauskas R, Hemmer M, Perez WS, Steinert P, Horowitz MM, et al. Hematopoietic cell transplant for acute myeloid leukemia and myelodysplastic syndrome: conditioning regimen intensity. Blood Adv. 2018;2:2095–103.
Baron F, Labopin M, Peniket A, Jindra P, Afanasyev B, Sanz MA, et al. Reduced-intensity conditioning with fludarabine and busulfan versus fludarabine and melphalan for patients with acute myeloid leukemia: a report from the Acute Leukemia Working Party of the European Group for Blood and Marrow Transplantation. Cancer. 2015;121:1048–55.
Oran B, Ahn KW, Fretham C, Beitinjaneh A, Bashey A, Pawarode A, et al. Fludarabine and melphalan compared with reduced doses of busulfan and fludarabine improve transplantation outcomes in older patients with myelodysplastic syndromes. Transpl Cell Ther. 2021;27:921.e1–921.e10.
Duque-Afonso J, Finke J, Labopin M, Craddock C, Protheroe R, Kottaridis P, et al. Comparison of fludarabine-melphalan and fludarabine-treosulfan as conditioning prior to allogeneic hematopoietic cell transplantation-a registry study on behalf of the EBMT acute leukemia working party. Bone Marrow Transpl. 2022;57:1269–76.
Wäsch R, Reisser S, Hahn J, Bertz H, Engelhardt M, Kunzmann R, et al. Rapid achievement of complete donor chimerism and low regimen-related toxicity after reduced conditioning with fludarabine, carmustine, melphalan and allogeneic transplantation. Bone Marrow Transpl. 2000;26:243–50.
Bertz H, Potthoff K, Finke J. Allogeneic stem-cell transplantation from related and unrelated donors in older patients with myeloid leukemia. J Clin Oncol. 2003;21:1480–4.
Spyridonidis A, Bertz H, Ihorst G, Grüllich C, Finke J. Hematopoietic cell transplantation from unrelated donors as an effective therapy for older patients (> or = 60 years) with active myeloid malignancies. Blood. 2005;105:4147–8.
Marks R, Potthoff K, Hahn J, Ihorst G, Bertz H, Spyridonidis A, et al. Reduced-toxicity conditioning with fludarabine, BCNU, and melphalan in allogeneic hematopoietic cell transplantation: particular activity against advanced hematologic malignancies. Blood. 2008;112:415–25.
Ciurea SO, Saliba R, Rondon G, Pesoa S, Cano P, Fernandez-Vina M, et al. Reduced-intensity conditioning using fludarabine, melphalan and thiotepa for adult patients undergoing haploidentical SCT. Bone Marrow Transpl. 2010;45:429–36.
Ciurea SO, Saliba RM, Hamerschlak N, Karduss Aurueta AJ, Bassett R, Fernandez-Vina M, et al. Fludarabine, melphalan, thiotepa and anti-thymocyte globulin conditioning for unrelated cord blood transplant. Leuk Lymphoma. 2012;53:901–6.
Majolino I, Davoli M, Carnevalli E, Locasciulli A, Di Bartolomeo P, Scimè R, et al. Reduced intensity conditioning with thiotepa, fludarabine, and melphalan is effective in advanced multiple myeloma. Leuk Lymphoma. 2007;48:759–66.
Duque-Afonso J, Ihorst G, Waterhouse M, Zeiser R, Wäsch R, Bertz H, et al. Impact of lung function on bronchiolitis obliterans syndrome and outcome after allogeneic hematopoietic cell transplantation with reduced-intensity conditioning. Biol Blood Marrow Transpl. 2018;24:2277–84.
Duque-Afonso J, Ihorst G, Waterhouse M, Zeiser R, Wäsch R, Bertz H, et al. Comparison of reduced-toxicity conditioning protocols using fludarabine, melphalan combined with thiotepa or carmustine in allogeneic hematopoietic cell transplantation. Bone Marrow Transpl. 2021;56:110–20.
Kanate AS, Nagler A, Savani B. Summary of scientific and statistical methods, study endpoints and definitions for observational and registry-based studies in hematopoietic cell transplantation. Clin Hematol Int. 2019;2:2–4.
Nagler A, Shimoni A Conditioning. In: Carreras E, Dufour C, Mohty M, Kröger N, editors. The EBMT Handbook: Hematopoietic Stem Cell Transplantation and Cellular Therapies 2019. 7th edition. Cham (CH): Springer. Chapter 13.
Passweg JR, Baldomero H, Chabannon C, Basak GW, de la Cámara R, Corbacioglu S, et al. Hematopoietic cell transplantation and cellular therapy survey of the EBMT: monitoring of activities and trends over 30 years. Bone Marrow Transplant. 2021;56:1651–64.
Saraceni F, Scortechini I, Fiorentini A, Dubbini MV, Mancini G, Federici I, et al. Conditioning regimens for frail patients with acute leukemia undergoing allogeneic stem cell transplant: how to strike gently. Clin Hematol Int. 2021;3:153–60.
Rambaldi A, Grassi A, Masciulli A, Boschini C, Micò MC, Busca A, et al. Busulfan plus cyclophosphamide versus busulfan plus fludarabine as a preparative regimen for allogeneic haemopoietic stem-cell transplantation in patients with acute myeloid leukaemia: an open-label, multicentre, randomised, phase 3 trial. Lancet Oncol. 2015;16:1525–36.
Russell JA, Tran HT, Quinlan D, Chaudhry A, Duggan P, Brown C, et al. Once-daily intravenous busulfan given with fludarabine as conditioning for allogeneic stem cell transplantation: study of pharmacokinetics and early clinical outcomes. Biol Blood Marrow Transpl. 2002;8:468–76.
de Lima M, Couriel D, Thall PF, Wang X, Madden T, Jones R, et al. Once-daily intravenous busulfan and fludarabine: clinical and pharmacokinetic results of a myeloablative, reduced-toxicity conditioning regimen for allogeneic stem cell transplantation in AML and MDS. Blood. 2004;104:857–64.
Beelen DW, Stelljes M, Reményi P, Wagner-Drouet EM, Dreger P, Bethge W, et al. Treosulfan compared with reduced-intensity busulfan improves allogeneic hematopoietic cell transplantation outcomes of older acute myeloid leukemia and myelodysplastic syndrome patients: final analysis of a prospective randomized trial. Am J Hematol. 2022;97:1023–34.
Shimoni A, Hardan I, Shem-Tov N, Rand A, Herscovici C, Yerushalmi R, et al. Comparison between two fludarabine-based reduced-intensity conditioning regimens before allogeneic hematopoietic stem-cell transplantation: fludarabine/melphalan is associated with higher incidence of acute graft-versus-host disease and non-relapse mortality and lower incidence of relapse than fludarabine/busulfan. Leukemia. 2007;21:2109–16.
Bernardo ME, Zecca M, Piras E, Vacca A, Giorgiani G, Cugno C, et al. Treosulfan-based conditioning regimen for allogeneic haematopoietic stem cell transplantation in patients with thalassaemia major. Br J Haematol. 2008;143:548–51.
Bernardo ME, Piras E, Vacca A, Giorgiani G, Zecca M, Bertaina A, et al. Allogeneic hematopoietic stem cell transplantation in thalassemia major: results of a reduced-toxicity conditioning regimen based on the use of treosulfan. Blood. 2012;120:473–6.
Finke J, Schmoor C, Stelljes M, Burchert A, Dreger P, Hegenbart U, et al. Thiotepa-fludarabine-treosulfan conditioning for 2nd allogeneic HCT from an alternative unrelated donor for patients with AML: a prospective multicenter phase II trial. Bone Marrow Transpl. 2022;57:1664–70.
Sanz J, Boluda JC, Martín C, González M, Ferrá C, Serrano D, et al. Single-unit umbilical cord blood transplantation from unrelated donors in patients with hematological malignancy using busulfan, thiotepa, fludarabine and ATG as myeloablative conditioning regimen. Bone Marrow Transpl. 2012;47:1287–93.
Di Bartolomeo P, Santarone S, De Angelis G, Picardi A, Cudillo L, Cerretti R, et al. Haploidentical, unmanipulated, G-CSF-primed bone marrow transplantation for patients with high-risk hematologic malignancies. Blood. 2013;121:849–57.
Raiola AM, Dominietto A, Ghiso A, Di Grazia C, Lamparelli T, Gualandi F, et al. Unmanipulated haploidentical bone marrow transplantation and posttransplantation cyclophosphamide for hematologic malignancies after myeloablative conditioning. Biol Blood Marrow Transpl. 2013;19:117–22.
Sora F, Grazia CD, Chiusolo P, Raiola AM, Bregante S, Mordini N. et al. Allogeneic hemopoietic stem cell transplants in patients with Acute Myeloid Leukemia (AML) prepared with Busulfan and Fludarabine (BUFLU) or Thiotepa, Busulfan, and Fludarabine (TBF): a retrospective study. Biol Blood Marrow Transpl. 2020;26:698–703.
Saraceni F, Labopin M, Hamladji RM, Mufti G, Socié G, Shimoni A, et al. Acute leukemia working party of the European society for Blood and Marrow Transplantation (EBMT). Thiotepa-busulfan-fludarabine compared to busulfan-fludarabine for sibling and unrelated donor transplant in acute myeloid leukemia in first remission. Oncotarget. 2017;9:3379–93.
Craddock C, Jackson A, Loke J, Siddique S, Hodgkinson A, Mason J, et al. Augmented reduced-intensity regimen does not improve postallogeneic transplant outcomes in acute myeloid leukemia. J Clin Oncol. 2021;39:768–78.
Marsh RA, Lane A, Mehta PA, Neumeier L, Jodele S, Davies SM, et al. Alemtuzumab levels impact acute GVHD, mixed chimerism, and lymphocyte recovery following alemtuzumab, fludarabine, and melphalan RIC HCT. Blood. 2016;127:503–12.
Bertz H, Spyridonidis A, Wäsch R, Grüllich C, Egger M, Finke J. A novel GVHD-prophylaxis with low-dose alemtuzumab in allogeneic sibling or unrelated donor hematopoetic cell transplantation: the feasibility of deescalation. Biol Blood Marrow Transpl. 2009;15:1563–70.
Acknowledgements
The study has been performed on behalf of the Acute Leukemia Working Party of the EBMT. The authors would like to thank the contribution of the ALWP data managers to this work. According to EBMT rules, co-authorship has been offered to the centers contributing most patients to the analysis. However, we would like to thank all the centers for their contribution to this work.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
JD-A, JF, BNS, AS, AN and MM designed the study, interpreted the data, and wrote the manuscript. MN and J-EG performed the statistical analysis. CCrad, BC, AB, EN, ME, OK, TV, JAS, ET, CCraw, MC, KMOW, AG, RP, FC and EMW-D provided patient data. All the authors critically reviewed the final version of the manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests with the publication of this article. JD-A has received speaker’s honoraria from Roche, Amgen, AstraZeneca, Riemser, Lilly, Ipsen and Sobi and travel support from Gilead and Sobi. JF has received research support and speaker’s honoraria from Medac, Neovii, and Riemser. JAS declares advisory board for Medac, and speaker fees from Novartis, Mallinckrodt, Gilead and Jazz. CCrad declares consulting/speakers board fees for Abbvie, JAZZ and Medac.
Ethics approval
This study was approved by the general assembly of the ALWP of the EBMT.
Patient consent
Patient authorization was performed via informed consent to include their data in the EBMT registry.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Duque-Afonso, J., Finke, J., Ngoya, M. et al. Comparison of fludarabine/melphalan (FluMel) with fludarabine/melphalan/BCNU or thiotepa (FBM/FTM) in patients with AML in first complete remission undergoing allogeneic hematopoietic stem cell transplantation – a registry study on behalf of the EBMT Acute Leukemia Working Party. Bone Marrow Transplant 59, 247–254 (2024). https://doi.org/10.1038/s41409-023-02150-w
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02150-w