Abstract
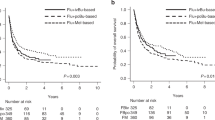
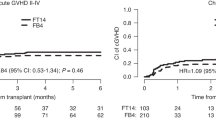
Comparative data of fludarabine, cytarabine and amsacrine (FLAMSA) chemotherapy followed by busulfan (Bu)-based reduced-intensity conditioning (RIC) (FLAMSA-Bu) versus RIC regimens are lacking in patients with active relapsed/refractory (R/R) acute myeloid leukemia (AML) at the time of allogeneic hematopoietic stem cell transplantation (alloSCT). Here, we retrospectively analyzed outcomes after FLAMSA-Bu versus fludarabine/busulfan (FluBu2) conditioning in this patient population. A total of 476 patients fulfilled the inclusion criteria, of whom 257 received FluBu2 and 219 FLAMSA-Bu. Median follow-up was 41 months. Two-year non-relapse mortality (21%), graft-versus-host disease-free, relapse-free survival (24%) and chronic graft-versus-host disease (GVHD) (29%) were not statistically different between cohorts. FLAMSA-Bu was associated with lower 2-year relapse incidence (RI) (38 vs 49% after FluBu2, p = 0.004), and increased leukemia-free survival (LFS) (42 vs 29%, p = 0.001), overall survival (47 vs 39%, p = 0.008) and grades II-IV acute GVHD (36 vs 20%, p = 0.001). In the multivariate analysis, FLAMSA-Bu remained associated with lower RI (HR 0.69, p = 0.042), increased LFS (HR 0.74, p = 0.048) and a higher risk of acute GVHD (HR 2.06, p = 0.005). Notwithstanding the limitations inherent in this analysis, our data indicate that FLAMSA-Bu constitutes a tolerable conditioning strategy, resulting in a long-term benefit in a subset of patients reaching alloSCT with active disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Kurosawa S, Yamaguchi T, Miyawaki S, Uchida N, Sakura T, Kanamori H, et al. Prognostic factors and outcomes of adult patients with acute myeloid leukemia after first relapse. Haematologica. 2010;95:1857–64.
Ravandi F, Cortes J, Faderl S, O’Brien S, Garcia-Manero G, Verstovsek S, et al. Characteristics and outcome of patients with acute myeloid leukemia refractory to 1 cycle of high-dose cytarabine-based induction chemotherapy. Blood. 2010;116:5818–23.
Wattad M, Weber D, Döhner K, Krauter J, Gaidzik VI, Paschka P, et al. Impact of salvage regimens on response and overall survival in acute myeloid leukemia with induction failure. Leukemia. 2017;31:1306–13.
Cortes JE, Khaled S, Martinelli G, Perl AE, Ganguly S, Russell N, et al. Quizartinib versus salvage chemotherapy in relapsed or refractory FLT3-ITD acute myeloid leukaemia (QuANTUM-R): a multicentre, randomised, controlled, open-label, phase 3 trial. Lancet Oncol. 2019;20:984–97.
Perl AE, Martinelli G, Cortes JE, Neubauer A, Berman E, Paolini S, et al. Gilteritinib or chemotherapy for relapsed or refractory FLT3-mutated AML. N Engl J Med. 2019;381:1728–40.
Uy GL, Aldoss I, Foster MC, Sayre PH, Wieduwilt MJ, Advani AS, et al. Flotetuzumab as salvage immunotherapy for refractory acute myeloid leukemia. Blood. 2021;137:751–62.
Stahl M, Menghrajani K, Derkach A, Chan A, Xiao W, Glass J, et al. Clinical and molecular predictors of response and survival following venetoclax therapy in relapsed/refractory AML. Blood Adv. 2021;5:1552–64.
Duval M, Klein JP, He W, Cahn JY, Cairo M, Camitta BM, et al. Hematopoietic stem-cell transplantation for acute leukemia in relapse or primary induction failure. J Clin Oncol. 2010;28:3730–8.
Othus M, Appelbaum FR, Petersdorf SH, Kopecky KJ, Slovak M, Nevill T, et al. Fate of patients with newly diagnosed acute myeloid leukemia who fail primary induction therapy. Biol Blood Marrow Transpl. 2015;21:559–64.
Nagler A, Savani BN, Labopin M, Polge E, Passweg J, Finke J, et al. Outcomes after use of two standard ablative regimens in patients with refractory acute myeloid leukaemia: A retrospective, multicentre, registry analysis. Lancet Haematol. 2015;2:e384–92.
Loke J, Malladi R, Moss P, Craddock C. The role of allogeneic stem cell transplantation in the management of acute myeloid leukaemia: a triumph of hope and experience. Br J Haematol. 2020;188:129–46.
Schmid C, Schleuning M, Ledderose G, Tischer J, Kolb HJ. Sequential regimen of chemotherapy, reduced-intensity conditioning for allogeneic stem-cell transplantation, and prophylactic donor lymphocyte transfusion in high-risk acute myeloid leukemia and myelodysplastic syndrome. J Clin Oncol. 2005;23:5675–87.
Schmid C, Schleuning M, Schwerdtfeger R, Hertenstein B, Mischak-Weissinger E, Bunjes D, et al. Long-term survival in refractory acute myeloid leukemia after sequential treatment with chemotherapy and reduced-intensity conditioning for allogeneic stem cell transplantation. Blood. 2006;108:1092–9.
Malard F, Labopin M, Stuhler G, Bittenbring J, Ganser A, Tischer J, et al. Sequential intensified conditioning regimen allogeneic hematopoietic stem cell transplantation in adult patients with intermediate- or high-risk acute myeloid leukemia in complete remission: a study from the acute leukemia working party of the European Group for Blood and Marrow Transplantation. Biol Blood Marrow Transpl. 2017;23:278–84.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: An ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows JTE. 1994 consensus conference on acute GVHD grading. Bone Marrow Transpl. 1995;15:825–8.
Lee SJ, Vogelsang G, Flowers MED. Chronic graft-versus-host disease. Biol Blood Marrow Transpl. 2003;9:215–33.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–66.
Hougaard P. Frailty models for survival data. Lifetime Data Anal. 1995;1:255–73.
Andersen P, Klein J, Zhang M. Testing for centre effects in multi-centre survival studies: a Monte Carlo comparison of fixed and random effects tests. Stat Med. 1999;18:1489–500.
Craddock C, Jackson A, Loke J, Siddique S, Hodgkinson A, Mason J, et al. Augmented reduced-intensity regimen does not improve postallogeneic transplant outcomes in acute myeloid leukemia. J Clin Oncol. 2021;39:768–78.
Ruggeri A, Battipaglia G, Labopin M, Ehninger G, Beelen D, Tischer J, et al. Unrelated donor versus matched sibling donor in adults with acute myeloid leukemia in first relapse: An ALWP-EBMT study. J Hematol Oncol. 2016;9:1–8.
Rodríguez-Arbolí E, Labopin M, Tischer J, Brecht A, Ganser A, Finke J, et al. FLAMSA-based reduced-intensity conditioning versus myeloablative conditioning in younger patients with relapsed/refractory acute myeloid leukemia with active disease at the time of allogeneic stem cell transplantation: an analysis from the acute leukemia. Biol Blood Marrow Transpl. 2020;26:2165–73.
Spyridonidis A, Labopin M, Savani BN, Niittyvuopio R, Blaise D, Craddock C, et al. Redefining and measuring transplant conditioning intensity in current era: a study in acute myeloid leukemia patients. Bone Marrow Transpl. 2020;55:1114–25.
Hourigan CS, Dillon LW, Gui G, Logan BR, Fei M, Ghannam J, et al. Impact of conditioning intensity of allogeneic transplantation for acute myeloid leukemia with genomic evidence of residual disease. J Clin Oncol. 2020;38:1273–83.
Craddock C, Nagra S, Peniket A, Brookes C, Buckley L, Nikolousis E, et al. Factors predicting long-term survival after T-cell depleted reduced intensity allogeneic stem cell transplantation for acute myeloid leukemia. Haematologica. 2010;95:989–95.
Aoudjhane M, Labopin M, Gorin NC, Shimoni A, Ruutu T, Kolb HJ, et al. Comparative outcome of reduced intensity and myeloablative conditioning regimen in HLA identical sibling allogeneic haematopoietic stem cell transplantation for patients older than 50 years of age with acute myeloblastic leukaemia: a retrospective survey. Leukemia. 2005;19:2304–12.
Luger SM, Ringdén O, Zhang M-J, Perez WS, Bishop MR, Bornhäuser M, et al. Similar outcomes using myeloablative versus reduced intensity allogeneic transplant. Bone Marrow Transpl. 2012;47:203–11.
Ringdén O, Labopin M, Ehninger G, Niederwieser D, Olsson R, Basara N, et al. Reduced intensity conditioning compared with myeloablative conditioning using unrelated donor transplants in patients with acute myeloid leukemia. J Clin Oncol. 2009;27:4570–7.
Couriel DR, Saliba RM, Giralt S, Khouri I, Andersson B, de Lima M, et al. Acute and chronic graft-versus-host disease after ablative and nonmyeloablative conditioning for allogeneic hematopoietic transplantation. Biol Blood Marrow Transpl. 2004;10:178–85.
Bornhäuser M, Kienast J, Trenschel R, Burchert A, Hegenbart U, Stadler M, et al. Reduced-intensity conditioning versus standard conditioning before allogeneic haemopoietic cell transplantation in patients with acute myeloid leukaemia in first complete remission: a prospective, open-label randomised phase 3 trial. Lancet Oncol. 2012;13:1035–44.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
Schmid C, Labopin M, Schaap N, Veelken H, Schleuning M, Stadler M, et al. Prophylactic donor lymphocyte infusion after allogeneic stem cell transplantation in acute leukaemia—a matched pair analysis by the Acute Leukaemia Working Party of EBMT. Br J Haematol. 2019;184:782–7.
Burchert A, Bug G, Fritz LV, Finke J, Stelljes M, Röllig C, et al. Sorafenib maintenance after allogeneic hematopoietic stem cell transplantation for acute myeloid leukemia with FLT3-internal tandem duplication mutation (SORMAIN). J Clin Oncol. 2020;38:2993–3002.
Xuan L, Wang Y, Huang F, Fan Z, Xu Y, Sun J, et al. Sorafenib maintenance in patients with FLT3-ITD acute myeloid leukaemia undergoing allogeneic haematopoietic stem-cell transplantation: an open-label, multicentre, randomised phase 3 trial. Lancet Oncol. 2020;21:1201–12.
Bug G, Burchert A, Wagner EM, Kröger N, Berg T, Güller S, et al. Phase I/II study of the deacetylase inhibitor panobinostat after allogeneic stem cell transplantation in patients with high-risk MDS or AML (PANOBEST trial). Leukemia. 2017;31:2523–5.
Acknowledgements
ERA is a recipient of a Río Hortega academic clinical fellowship (CM19/00194) from the Instituto de Salud Carlos III, Spain. We thank all the patients included in the study and their families, as well as the investigators and data managers from the participating EBMT sites.
Author information
Authors and Affiliations
Contributions
ERA and MM conceived and designed the study. ML performed the statistical analyses. ERA wrote the draft version of the manuscript. BS, AS, AB, SG, EB, CS, AN, and MM reviewed the manuscript and contributed to its final version. ME, AB, IWB, AH, EF, JT, WB, SB, MV, CEB, HE, and FS were the principal investigators at the centers recruiting the highest number of patients for the study. All authors critically reviewed the manuscript and approved its final version.
Corresponding author
Ethics declarations
Competing interests
ERA and CS have received speaker fees from Eurocept Pharmaceuticals. The remaining authors declare no competing financial interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Rodríguez-Arbolí, E., Labopin, M., Eder, M. et al. Augmented FLAMSA-Bu versus FluBu2 reduced-intensity conditioning in patients with active relapsed/refractory acute myeloid leukemia: an EBMT analysis. Bone Marrow Transplant 57, 934–941 (2022). https://doi.org/10.1038/s41409-022-01611-y
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01611-y