Abstract
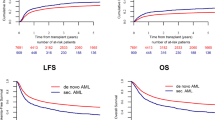
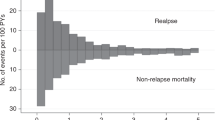
We report the results from a multicentre retrospective study of 220 adult patients who underwent allogeneic hematopoietic stem cell transplantation (alloHSCT) for therapy-related acute myeloid leukaemia (t-AML). Median age at t-AML diagnosis was 56 years, with a prior history of haematological (45%) or breast (34%). Median time from cytotoxic exposure to t-AML diagnosis was 54.7 months. At transplant, around 20% of patients had measurable residual disease and 3% of patients were not in complete remission. The median follow-up was 21.4 months (Q1–Q3, 5.9–52.8). At 12 months, overall survival (OS), event-free survival (EFS), and graft-versus-host-disease (GVHD)-free-relapse-free survival (GRFS) were 60.7% (95% CI 54.6–67.5), 52.8% (95% CI 46.5–68.4), and 44.1% (95% CI 37.6–51.8), respectively. At 5 years, OS, EFS, and GRFS were 44.1% (95% CI 37.4–52.1), 40.4% (95% CI 33.9–48.1), and 35.3% (95% CI 28.8–43.3), respectively. At last follow-up, 44% of patients were in complete remission (n = 96) and transplant-related mortality accounted for 21% of all deaths (n = 119). Multivariable analysis revealed that uncontrolled t-AML at transplant was associated with lower EFS (HR 1.94, 95% CI 1.0–3.7, p = 0.041). In conclusion, alloHSCT for t-AML shows encouraging results and offers additional opportunity with the emergence of novel pre-graft therapies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
McNerney ME, Godley LA, Le Beau MM. Therapy-related myeloid neoplasms: when genetics and environment collide. Nat Rev Cancer. 2017;17:513–27.
Wong TN, Ramsingh G, Young AL, Miller CA, Touma W, Welch JS, et al. The role of TP53 mutations in the origin and evolution of therapy-related AML. Nature. 2015;518:552–5.
Allan JM, Travis LB. Mechanisms of therapy-related carcinogenesis. Nat Rev Cancer. 2005;5:943–55.
Larson RA. Etiology and management of therapy-related myeloid leukemia. Hematology. 2007;2007:453–9.
Nenova I, Grudeva-Popova J. Carcinogenic potential of antitumor therapies - is the risk predictable? J BUON. 2017;22:1378–84.
Morton LM, Dores GM, Tucker MA, Kim CJ, Onel K, Gilbert ES, et al. Evolving risk of therapy-related acute myeloid leukemia following cancer chemotherapy among adults in the United States, 1975-2008. Blood. 2013;121:2996–3004.
Borthakur G, Estey EE. Therapy-related acute myelogenous leukemia and myelodysplastic syndrome. Curr Oncol Rep. 2007;9:373–7.
Cancer Survivorship --- United States, 1971–2001. https://www.cdc.gov/mmwr/preview/mmwrhtml/mm5324a3.htm (accessed 20 Sep2021).
Miller KD, Nogueira L, Mariotto AB, Rowland JH, Yabroff KR, Alfano CM, et al. Cancer treatment and survivorship statistics, 2019. CA Cancer J Clin. 2019;69:363–85.
Nilsson C, Linde F, Hulegårdh E, Garelius H, Lazarevic V, Antunovic P, et al. Characterization of therapy-related acute myeloid leukemia: increasing incidence and prognostic implications. Haematologica. 2022. https://doi.org/10.3324/haematol.2022.281233.
Granfeldt Østgård LS, Medeiros BC, Sengeløv H, Nørgaard M, Andersen MK, Dufva IH, et al. Epidemiology and clinical significance of secondary and therapy-related acute myeloid leukemia: a national population-based cohort study. JCO. 2015;33:3641–9.
Churpek JE, Larson RA. The evolving challenge of therapy-related myeloid neoplasms. Best Pract Res Clin Haematol. 2013;26:309–17.
Hulegårdh E, Nilsson C, Lazarevic V, Garelius H, Antunovic P, Derolf ÅR, et al. Characterization and prognostic features of secondary acute myeloid leukemia in a population-based setting: a report from the Swedish Acute Leukemia Registry. Am J Hematol. 2015;90:208–14.
Nampoothiri RV, Law AD, Lam W, Chen C, Al-Shaibani Z, Loach D, et al. Predictors of outcomes of therapy-related acute myeloid leukemia after allogeneic hematopoietic stem cell transplantation. Hematol Oncol Stem Cell Ther. 2022;15:27–35.
Grimwade D, Hills RK, Moorman AV, Walker H, Chatters S, Goldstone AH, et al. Refinement of cytogenetic classification in acute myeloid leukemia: determination of prognostic significance of rare recurring chromosomal abnormalities among 5876 younger adult patients treated in the United Kingdom Medical Research Council trials. Blood. 2010;116:354–65.
Döhner H, Estey E, Grimwade D, Amadori S, Appelbaum FR, Büchner T, et al. Diagnosis and management of AML in adults: 2017 ELN recommendations from an international expert panel. Blood. 2017;129:424–47.
McDonald GB, Sandmaier BM, Mielcarek M, Sorror M, Pergam SA, Cheng G-S, et al. Survival, nonrelapse mortality, and relapse-related mortality after allogeneic hematopoietic cell transplantation: comparing 2003–2007 versus 2013–2017 cohorts. Ann Intern Med. 2020;172:229.
Metheny L, Callander NS, Hall AC, Zhang M-J, Bo-Subait K, Wang H-L, et al. Allogeneic transplantation to treat therapy-related myelodysplastic syndrome and acute myelogenous leukemia in adults. Transplant Cell Ther. 2021;27:923.e1–923.e12.
Döhner H, Wei AH, Löwenberg B. Towards precision medicine for AML. Nat Rev Clin Oncol. 2021;18:577–90.
Lee CJ, Labopin M, Beelen D, Finke J, Blaise D, Ganser A, et al. Comparative outcomes of myeloablative and reduced‐intensity conditioning allogeneic hematopoietic cell transplantation for therapy‐related acute myeloid leukemia with prior solid tumor: a report from the acute leukemia working party of the European society for blood and bone marrow transplantation. Am J Hematol. 2019;94:431–8.
Bastida JM, Cabrero M, Lopez-Godino O, Lopez-Parra M, Sanchez-Guijo F, Lopez-Corral L, et al. Influence of donor age in allogeneic stem cell transplant outcome in acute myeloid leukemia and myelodisplastic syndrome. Leuk Res. 2015;39:828–34.
Tomizawa D, Tanaka S, Kondo T, Hashii Y, Arai Y, Kudo K, et al. Allogeneic hematopoietic stem cell transplantation for adolescents and young adults with acute myeloid leukemia. Biol Blood Marrow Transplant. 2017;23:1515–22.
Goyal SD, Zhang M-J, Wang H-L, Akpek G, Copelan EA, Freytes C, et al. Allogeneic hematopoietic cell transplant for AML: no impact of pre-transplant extramedullary disease on outcome. Bone Marrow Transpl. 2015;50:1057–62.
Yokohama Cooperative Study Group for Hematology (YACHT), Ando T, Fujisawa S, Teshigawara H, Ogusa E, Ishii Y, et al. Impact of treatment-related weight changes from diagnosis to hematopoietic stem-cell transplantation on clinical outcome of acute myeloid leukemia. Int J Hematol. 2019;109:673–83.
Schmaelter A-K, Labopin M, Socié G, Itälä-Remes M, Blaise D, Yakoub-Agha I, et al. Inferior outcome of allogeneic stem cell transplantation for secondary acute myeloid leukemia in first complete remission as compared to de novo acute myeloid leukemia. Blood Cancer J. 2020;10:26.
Salas MQ, Chen S, Lam W, Pasic I, Gerbitz A, Michelis FV, et al. Less is more: superior graft-versus-host disease-free/relapse-free survival with reduced-intensity conditioning and dual T cell depletion in acute myelogenous leukemia. Biol Blood Marrow Transplant. 2020;26:1511–9.
Gatwood KS, Labopin M, Savani BN, Finke J, Socie G, Beelen D, et al. Transplant outcomes for patients with therapy-related acute myeloid leukemia with prior lymphoid malignancy: an ALWP of EBMT study. Bone Marrow Transpl. 2020;55:224–32.
Sengsayadeth S, Labopin M, Boumendil A, Finke J, Ganser A, Stelljes M, et al. Transplant outcomes for secondary acute myeloid leukemia: acute leukemia working party of the European Society for blood and bone marrow transplantation study. Biol Blood Marrow Transplant. 2018;24:1406–14.
Sorror ML, Maris MB, Storb R, Baron F, Sandmaier BM, Maloney DG, et al. Hematopoietic cell transplantation (HCT)-specific comorbidity index: a new tool for risk assessment before allogeneic HCT. Blood. 2005;106:2912–9.
ElSawy M, Storer BE, Pulsipher MA, Maziarz RT, Bhatia S, Maris MB, et al. Multi-centre validation of the prognostic value of the haematopoietic cell transplantation- specific comorbidity index among recipient of allogeneic haematopoietic cell transplantation. Br J Haematol. 2015;170:574–83.
Jullien M, Orvain C, Berceanu A, Couturier M, Guillaume T, Peterlin P, et al. Impact of allogeneic stem cell transplantation comorbidity indexes after haplotransplant using post‐transplant cyclophosphamide. Cancer Med. 2021;10:7194–202.
Elsawy M, Storer BE, Milano F, Sandmaier BM, Delaney C, Salit RB, et al. Prognostic performance of the augmented hematopoietic cell transplantation-specific comorbidity/age index in recipients of allogeneic hematopoietic stem cell transplantation from alternative graft sources. Biol Blood Marrow Transplant. 2019;25:1045–52.
D’Angelo CR, Novitsky B, Mee Lee S, Godley LA, Kline J, Larson RA, et al. Characterization of cancer comorbidity prior to allogeneic hematopoietic cell transplantation. Leuk Lymphoma. 2019;60:629–38.
Alfayez M, Kantarjian H, Kadia T, Ravandi-Kashani F, Daver N. CPX-351 (vyxeos) in AML. Leuk Lymphoma. 2020;61:288–97.
Lancet JE, Uy GL, Cortes JE, Newell LF, Lin TL, Ritchie EK, et al. CPX-351 (cytarabine and daunorubicin) liposome for injection versus conventional cytarabine plus daunorubicin in older patients with newly diagnosed secondary acute myeloid. Leuk JCO. 2018;36:2684–92.
Lancet JE, Uy GL, Newell LF, Lin TL, Ritchie EK, Stuart RK, et al. CPX-351 versus 7+3 cytarabine and daunorubicin chemotherapy in older adults with newly diagnosed high-risk or secondary acute myeloid leukaemia: 5-year results of a randomised, open-label, multicentre, phase 3 trial. Lancet Haematol. 2021;8:e481–e491.
Cherry EM, Abbott D, Amaya M, McMahon C, Schwartz M, Rosser J, et al. Venetoclax and azacitidine compared with induction chemotherapy for newly diagnosed patients with acute myeloid leukemia. Blood Adv. 2021;5:5565–73.
DiNardo CD, Jonas BA, Pullarkat V, Thirman MJ, Garcia JS, Wei AH, et al. Azacitidine and venetoclax in previously untreated acute myeloid leukemia. N Engl J Med. 2020;383:617–29.
Author information
Authors and Affiliations
Contributions
Conceptualisation, ET; Methodology, GR, ED, ET; Patients care, GR, RD, NF, EF, MS, PC, MR, FS, JBM, HLW, KB, ED, JOB, AF, CEB, SNQ, AG, CO, PT, ML, XP, GG, YB, NM, JBM, EC, JC, ET; Collected the data, GR, ED, RD, NF, EF, MS, PC, MR, FS, JBM, HLW, KB, ED, JOB, AF, CEB, SNQ, AG, CO, PT, ML, XP, GG, YB, NM, JBM, EC, JC, ET; Analysed data, GR, ED, PB, ET; Writing – original draft, GR, ED, ET; Review and editing, all the authors.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rey, G., Daguenet, E., Bonjean, P. et al. Allogeneic hematopoietic stem cell transplantation for adults with therapy-related acute myeloid leukaemia: a retrospective multicentre study on behalf of the SFGM-TC. Bone Marrow Transplant 58, 1331–1338 (2023). https://doi.org/10.1038/s41409-023-02082-5
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02082-5