Abstract
The real-world clinical and economic burden of graft-versus-host disease (GVHD) following allogeneic hematopoietic stem cell transplantation has not been comprehensively studied in France. Clinical outcomes, healthcare resource utilization and costs associated with acute GVHD (aGVHD), chronic GVHD (cGVHD), acute plus chronic GVHD (a+cGVHD) versus no GVHD were compared using French administrative claims data. After propensity score matching, 1934, 408, and 1268 matched pairs were retained for the aGVHD, cGVHD, and a+cGVHD cohorts, respectively. Compared with patients with no GVHD, odds of developing severe infection were greater in patients with aGVHD (odds ratio: 1.7 [95% confidence interval: 1.4, 2.1]). Compared with patients with no GVHD, mortality rates were higher in patients with aGVHD (rate ratio (RR): 1.6 [1.4, 1.7]) and with a+cGVHD (RR: 1.1 [1.0, 1.2]) but similar in patients with cGVHD (RR: 0.9 [0.7, 1.1]). Mean overnight hospital admission rates per patient-year were significantly higher in patients with aGVHD and a+cGVHD compared with no GVHD. Total direct costs (range €174,482–332,557) were 1.2, 1.5, and 1.9 times higher for patients with aGVHD, cGVHD, and a+cGVHD, respectively, versus patients with no GVHD. These results highlight the significant unmet need for effective treatments of patients who experience GVHD.
Similar content being viewed by others
Introduction
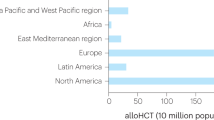
Hematopoietic stem cell transplantation (HSCT) is an effective and, in some cases, the only treatment option for many patients with hematological malignancies [1]. Advances in the field of allogeneic HSCT (allo-HSCT), in which patients receive stem cells from an unrelated donor, have greatly increased the number of transplants performed over the past 3 decades, and now ~20,000 procedures are performed annually across Europe, including more than 2000 in France [2, 3]. Despite such advances, graft-versus-host disease (GVHD) remains the most frequent and potentially fatal complication, occurring in ~40% of allo-HSCT recipients [4].
GVHD is traditionally categorized as either acute (aGVHD), usually presenting within 100 days of transplantation, or chronic (cGVHD), which more frequently occurs 100 days after transplantation [5]. Both aGVHD and cGVHD carry substantial health and economic burdens. Whereas cGVHD is associated with long-term morbidity and mortality, aGVHD is the primary fatal complication within the first few months following allo-HSCT [6]. Compared with patients who do not develop GVHD after allo-HSCT, those with GVHD have been shown to have higher hospital readmission, infection, and associated mortality rates [7, 8]. The clinical implications of GVHD have been shown to translate to an increased economic burden in the United States (US) with higher readmission rates for patients with GVHD compared with no GVHD, and a longer median length of hospital stay as well as higher median total costs for the initial procedure [8,9,10,11].
An unmet need exists for effective therapies to prevent and treat GVHD following allo-HSCT [12]. Treatment options for GVHD are largely limited to systemic corticosteroids and, specifically for patients with cGVHD, immunosuppressants [13]. Currently, there is no standard second-line treatment for patients who become resistant to or dependent on corticosteroids. A full evaluation of the public health burden of patients with GVHD is an important component for understanding the disease and its management. To date, the clinical and economic burden of GVHD has not been comprehensively studied in France. Quantifying the risk of severe disease, mortality, and the economic burden of GVHD is useful for healthcare providers, regulators, and payers. We performed a real-world analysis of the clinical outcomes, healthcare resource utilization (HCRU), and costs associated with aGVHD, cGVHD, and acute plus chronic (a+cGVHD) GVHD in France.
Materials and methods
Data source and study design
This study was a retrospective, nationwide cohort study using administrative claims obtained from the French national health data system, Système National des Données de Santé (SNDS). The SNDS contains health records of an estimated 65 million insured individuals. The French national health system offers universal coverage, so this is a representative sample of the whole population. SNDS data are linked via unique identifiers to primary care, hospital, pharmacy, and death registration databases, allowing for the linkage of patient treatment history, treatment patterns, and hospitalization based on International Classification of Diseases, 10th revision (ICD-10) codes.
The study period ran from January 1, 2011 through December 31, 2019. The index date was defined as the date of the first allo-HSCT procedure between January 1, 2012 and December 31, 2018. The baseline period was defined as the 12 months prior to the index date (as early as January 1, 2011). The follow-up period was a minimum of 12 months after the index date, until the last available information, death, or the end of the study (December 31, 2019), whichever came first.
This study was conducted in accordance with legal and regulatory requirements, as well as with scientific purpose, value, and rigor. The study followed generally accepted research practices described in the Guidelines for Good Pharmacoepidemiology Practices issued by the International Society for Pharmacoepidemiology, Good Epidemiological Practice guidelines issued by the International Epidemiological Association, Good Practices for Outcomes Research issued by the International Society for Pharmacoeconomics and Outcomes Research, International Ethical Guidelines for Epidemiological Research issued by the Council for International Organizations of Medical Sciences, and the European Medicines Agency, as well as the European Network of Centres for Pharmacoepidemiology, and Pharmacovigilance Guide on Methodological Standards in Pharmacoepidemiology. The final protocol was reviewed and approved by a scientific committee and the national data protection agency. All patient data were pseudonymized, which according to applicable legal requirements renders the data exempt from privacy laws; therefore, obtaining informed consent from patients was not required.
Study population
Patients (aged 18 years and above at the index date) who underwent allo-HSCT for any hematological malignancy between January 1, 2012 and December 31, 2018 were eligible for the study. Patients were excluded if they had an allo-HSCT prior to the start of the study or multiple allo-HSCT procedures during the study period. All patients were required to have at least 12 months of baseline data prior to the allo-HSCT and 12 months of possible follow-up data (unless they died). Eligible patients were identified in the database using the common classification of medical procedure codes or, where applicable, diagnosis-related group or ICD-10 codes.
Using ICD-10 codes, patients were divided into 1 of 4 categories by GVHD type: aGVHD, cGVHD, a+cGVHD, or no GVHD (Supplementary Table 1).
Outcome measures
The outcomes measures assessed were rates of severe infection, mortality, HCRU, and healthcare costs. Severe infections were defined as those leading to hospitalization and were identified through ICD-10 discharge codes. Relapse—investigated as an exploratory outcome—was defined as any hospital readmission for the same underlying malignancy, followed by cancer treatment. Mortality was defined as all-cause death.
Statistical analysis
Continuous variables were summarized descriptively with mean, standard deviation (SD), median, minimum and maximum, and lower and upper quartiles (Q1; Q3). Frequencies and percentages were reported for categorical variables. The chi-square test was used for categorical variables.
The crude mortality rate was calculated as a ratio of the number of deaths during the follow-up period divided by the total person-years in the given cohort. The crude rates of HCRU and of severe infections were calculated as the total number of events divided by the person-years. A mean value was then estimated for each cohort.
No imputed data were used for missing values for outcomes assessments. Statistical analyses were conducted using SAS (version 9.4 TS1M4). Percentages were based on available observations (known values), and outliers were included in ranges and percentiles. The rate ratios (RRs) were calculated using the OpenEpi statistical tool [14].
Comparative analysis
For the comparative analysis, separate 1:1 propensity score matching was used to balance covariates between the aGVHD, cGVHD, and a+cGVHD groups versus the no GVHD group. The propensity score, defined as the probability of a patient to develop GVHD conditional on observed baseline covariates, was estimated using a logistic regression model. The baseline covariates explored were hematological condition for the allo-HSCT, age, gender, comorbidities, and preparative regimens. The final model was chosen based on the Akaike information criterion (a mathematical method for evaluating how well a model fits the data it was generated from) and the sample size retained for each comparison. The final covariates were selected based on clinical relevance and/or statistical significance.
Binary and continuous demographics
All binary outcomes were described using frequencies. The excess number of infections (viral, fungal, bacterial, or other infection), the excess number of deaths, and the excess number of HCRUs were assessed using conditional logistic regression stratified by the paired identifier. Odds ratios (ORs) with the associated 95% confidence intervals (CIs) and two-sided p values were estimated.
Time-to-event outcomes
The effect of GVHD on each time-to-event outcome of interest (time to first severe infection and time to death) was summarized using Kaplan–Meier (KM) methodology on the matched population. The assumption of proportional hazards was evaluated by visually inspecting the KM plot and confirmed by testing the significance of interactions between treatment and the log of time. Hazard ratios (HRs) were used to assess excess time to death (or end of study follow-up, whichever came first), and excess time to severe infections.
Cost outcomes
Actual costs reimbursed were considered (without inflation to a standard cost year). Cost data were not normally distributed. The effect of GVHD on costs was investigated in the propensity score-matched populations using the generalized linear models with gamma distribution and log-link function. Excess cost was assessed using mean differences and cost ratios, together with the associated 95% CIs and p values.
Results
A total of 10,579 patients were identified in the SNDS database as recipients of allo-HSCT during the study period. After applying inclusion and exclusion criteria, 6385 patients were included in the study population (Fig. 1). The mean age of the overall study population was 51.1 years and 57.9% were male. A total of 2002 patients (31.4%) experienced aGVHD, 411 patients (6.4%) had cGVHD, and 1304 patients (20.4%) had a+cGVHD. The remaining 2668 patients (41.8%) had no recorded diagnosis code for GVHD (Supplementary Table 2).
aGVHD acute GVHD, a+cGVHD acute and chronic GVHD, allo-HSCT allogeneic hematopoietic stem cell transplantation, cGVHD chronic GVHD, FU follow-up, GVHD graft-versus-host disease, ICD-10 International Classification of Diseases, 10th revision, SNDS Système National des Données de Santé. *Includes patients with both an episode of acute and chronic GVHD at some point during follow-up. Identified using ICD-10 codes.
Patients with GVHD had lower rates of relapse than those with no GVHD. Overall, 16.3% of the total study population (1043 patients) had a relapse (aGVHD 276 patients [13.7%]; cGVHD 61 patients [14.8%]; a+cGVHD 220 patients [16.8%]; no GVHD 486 patients [18.2%]). Among all patients who had a relapse, the median time to relapse was 1.2 (range 0.1–56.5) months.
The final covariates selected to pair for propensity score matching for all groups were age at allo-HSCT, gender, year of allo-HSCT, and preparative regimen (use of clofarabine). Additional covariates for each GVHD type included related donor, other preparative regimen (use of carmustine), and the presence of diabetes for aGVHD and a+cGVHD; lymphoid leukemia, acute myeloblastic leukemia, and total body irradiation for aGVHD; congestive heart failure and connective tissue disorder for cGVHD; and cerebrovascular disease and any tumor (including lymphoma and leukemia except for malignant neoplasm of the skin) for a+cGVHD.
After propensity score matching, 1934 matched pairs were retained for the aGVHD cohort; 408 matched pairs were retained for the cGVHD cohort and 1268 matched pairs were retained for the a+cGVHD cohort (Table 1). The median ages of each of the matched cohorts versus no GVHD were 55.0 (range 18.0–77.0) for the aGVHD cohort (54.0 [range 18.0–78.0] no GVHD); 54.0 (range 18.0–75.0) for the cGVHD cohort (52.5 [range 18.0–78.0] no GVHD); and 53.0 (range 18.0–76.0) for the a+cGVHD cohort (54.0 [range 18.0–78.0] no GVHD).
Clinical outcomes
Overall, patients with any GVHD type were more likely to develop infections than those with no GVHD (Fig. 2). Among patients with aGVHD, 88.9% (1720 patients) developed at least one severe infection, compared with 82.2% (1589 patients) in the no GVHD cohort (OR 1.7 [95% CI 1.4, 2.1], p < 0.001), and 30.6% (592 patients) had four or more severe infections, compared with 18.5% (357 patients) in the no GVHD cohort (OR 1.9 [95% CI 1.7, 2.3], p < 0.001). Although a numerically greater proportion of patients with cGVHD than no GVHD developed severe infection (85.3% versus 81.9%, respectively), the difference was not statistically significant (OR 1.3 [95% CI 0.9, 1.9], p = 0.179). Significantly more patients with cGVHD had four or more infections compared with no GVHD (33.6% versus 18.4%, respectively; OR 2.2 [95% CI 1.6, 3.0], p < 0.001). Significantly more patients with a+cGVHD had severe infection compared with no GVHD (94.2% versus 81.4%; OR 4.0 [95% CI 3.0, 5.4], p < 0.001), and significantly more patients with a+cGVHD had four or more infections compared with no GVHD (50.5% versus 20.0%, respectively; OR 4.0 [95% CI 3.3, 4.9], p < 0.001). The most common infections were bacterial, recorded in >70% of all patients; and viral infections recorded in 47.4%, 44.9%, 59.1%, and 27.5–31.9% of patients with aGVHD, cGVHD, a+cGVHD, and no GVHD, respectively. The most frequent viral infection was CMV, reported in 28.6%, 23.5%, 36% of patients with aGVHD, cGVHD, a+cGVHD respectively versus 12.5%–13.7% of patients with no GVHD (Supplementary Table 3).
Patients with aGVHD and a+cGVHD had an increased rate of hospitalization for severe infection, with an RR of 1.3 (95% CI 1.2, 1.4) and 1.1 (95% CI 1.1, 1.2), respectively, versus no GVHD. The rate of hospitalization for severe infection was similar for patients with cGVHD compared with no GVHD (RR 1.0 [95% CI 0.8, 1.1], p > 0.05).
The mean time to first infection for patients with aGVHD was 10.0 (SD 0.5) months, compared with 15.6 (SD 0.7) months for patients with no GVHD (HR 2.5 [95% CI 1.9, 3.3], p < 0.001, for patients who had their first infection recorded after 2 months), and 10.1 (SD 0.1) months for a+cGVHD compared with 16.4 (SD 0.8) months for no GVHD (HR 2.5 [95% CI 1.7, 3.8], p < 0.001, for patients who had their first infection recorded after 6 months). The mean time to first infection was not statistically different for patients with cGVHD compared with no GVHD (16.0 [SD 1.3] months versus 16.4 [SD 1.4] months, respectively; HR 0.9 [95% CI 0.8, 1.1], p = 0.292). KM curves in Fig. 3 illustrate the time to first severe infection for each GVHD type versus no GVHD.
Patients with aGVHD had an increased mortality rate (RR 1.6 [95% CI 1.4, 1.7], p < 0.05) versus patients with no GVHD; the mortality rate was slightly higher, although not statistically significant, for the a+cGVHD versus no GVHD groups (RR 1.1 [95% CI 1.0, 1.2], p > 0.05) and similar between patients with cGVHD and patients with no GVHD (RR 0.9 [95% CI 0.7, 1.1], p > 0.05). KM curves in Fig. 4 illustrate the time to death for each GVHD type versus no GVHD.
Resource and cost implications of GVHD
Patients with aGVHD and a+cGVHD had significantly more overnight hospitalizations per patient-year than patients with no GVHD (mean admission rates aGVHD 4.3 versus 3.3 no GVHD, p < 0.001; a+cGVHD 4.2 versus 3.2 no GVHD, p < 0.001). Mean overnight hospitalizations per patient-year were similar for patients with cGVHD compared with no GVHD (3.0 versus 3.0, respectively, p = 0.044) (Table 2).
Total direct costs (including hospitalizations, outpatient visits, and pharmacy costs) were 1.2, 1.5, and 1.9 times higher (p < 0.001) for patients with aGVHD, cGVHD, and a+cGVHD, respectively, compared with no GVHD. Total indirect costs (including sick leave and transportation) were similar for patients with aGVHD versus patients with no GVHD, 1.3 times higher for patients with cGVHD (p = 0.017), and 1.3 times higher for patients with a+cGVHD than those with no GVHD (p < 0.001) (Table 3). Mean total cost within 100 days from allo-HSCT was 1.2 times higher for patients with aGVHD (€124,136) compared with no GVHD (€103,173). Hospital cost, including drugs dispensed during hospitalization, was the primary driver of increased HCRU and costs among patients with GVHD (Fig. 5).
aGVHD acute GVHD, a+cGVHD acute and chronic GVHD, cGVHD chronic GVHD, GVHD graft-versus-host disease. Mean costs per patient are computed among patients with at least one reimbursement for each individual component (the number of patients in the individual component costs can vary). They are presented here as layers; their sum is very close to the total direct cost.
Discussion
The clinical and economic impacts of GVHD were demonstrated in this real-world analysis of patients who had an allo-HSCT in France. Compared with patients with no GVHD, those with any type of GVHD were more likely to develop infections and patients with aGVHD had an increased mortality rate. More specifically, patients with aGVHD and a+cGVHD had an increased rate of hospitalizations for severe infections and a shorter time to first infection.
Although numerous changes in transplant practices have improved allo-HSCT results, opportunistic infections remain a serious complication associated with significant morbidity and mortality [15,16,17,18]. Beyond financial and economic burden, these potentially life-threatening infections also have important clinical burden and result in poor quality of life [15, 19, 20]. In the current study, 85.3–94.2% patients who presented with GVHD (depending on GVHD type) developed at least one severe infection (versus 81.4–82.2% patients in the matched no GVHD cohorts). In particular, 50.5% patients with a+cGVHD developed four or more severe infections (versus 20.0% patients in the matched no GVHD cohort). These results, in line with previous findings [21], highlight the critical importance of preventing and managing infection for patients receiving allo-HSCT. Indeed, in addition to the prevention, diagnosis, and treatment of the broad range of potential opportunistic infections that may occur after allo-HSCT, decreasing the amount of GVHD with a concomitant improvement of immune responses is key to achieve long-term GVHD and severe infection-free survival [15, 22].
Patients who experienced GVHD, regardless of the GVHD type, had higher HCRU and costs compared with patients who did not experience GVHD. These findings are consistent with previous research [8, 23, 24]. Furthermore, our results were maintained after controlling for key baseline characteristics including age at allo-HSCT, gender, hematological malignancy, type of donor, and type of preparative regimen. These findings are consistent with previous research in the US, which found the clinical and economic burden of GVHD extended for at least a year after transplantation [25].
Patients with GVHD had a longer mean initial length of hospital of stay and a significantly higher number of subsequent hospital stays, including intensive care unit (ICU) visits during these subsequent hospitalizations, compared with patients with no GVHD. During the follow-up period, total direct costs were 1.2, 1.5, and 1.9 times higher for patients with aGVHD, cGVHD, and a+cGVHD, respectively, than for those with no GVHD (p < 0.001). These costs were primarily driven by subsequent hospitalizations and drug costs. Patients with aGVHD had a significantly higher number of documented hospitalizations for severe infection as well as a higher rate of mortality than patients with no GVHD. These results are aligned with other studies conducted in Europe [26] and in the US [8,9,10,11] which showed increased costs for aGVHD when compared with no GVHD, although the costs differ between these regions. In this study, the mean total costs within 100 days from allo-HSCT were lower than in a similar US study [10], considering an exchange rate of $1.18 = €1. The cost of aGVHD in our study represented 46% of the reported cost for the US study (aGVHD: €124,136 in this study versus US reported cost of $316,458). Similarly, the cost of no GVHD in our study represented 57% of the reported cost for the US study (no GVHD: €103,173 in this study versus US reported cost of $215,229). The difference in costs between the two studies likely reflects country-specific healthcare practice patterns, labor and supply costs.
Compared with patients with no GVHD, patients with cGVHD had a significantly higher number of subsequent hospitalizations, and a higher number of ICU visits during subsequent hospitalizations. Total median indirect and direct costs were significantly higher for patients with cGVHD than no GVHD; these results were also observed for costs per patient-year. Although there was no statistically significant difference between the cGVHD and no GVHD cohorts in the number of patients with severe infection, the proportion of patients with severe infection was numerically higher in the cGVHD cohort. Mortality was similar between patients with cGVHD and those with no GVHD.
Significantly more patients with a+cGVHD had at least one subsequent hospitalization and a higher number of ICU visits during the subsequent hospitalizations, compared with those with no GVHD. Both total median indirect and direct costs as well as costs per patient-year were significantly higher for patients with a+cGVHD compared with those with no GVHD. The number of patients with severe infection was significantly higher for patients with a+cGVHD compared with those with no GVHD, resulting in a higher rate of severe infection. Patients with a+cGVHD had a slightly higher rate of mortality during the study follow-up.
Limitations
As with all database analyses, this study has limitations. The cohorts were defined using diagnosis codes. Patients may have been misidentified because of coding errors or changes in coding procedures during the course of the study, or some patients with GVHD may not have been identified, such as if the patient died during the index allo-HSCT hospitalization. To offset this, multiple checks were performed to ensure that all patients were adequately captured. The nature of aGVHD versus cGVHD may lead to inherent biases in observed outcomes. While it is difficult to conclude the reason patients with no GVHD, compared with those with cGVHD, had higher mortality, one possible explanation is that patients who survive are more likely to be coded with cGVHD at some point; thus, the mortality outcome is biased on this reasoning. This was not observed for those with aGVHD or a+cGVHD. Relapse-related mortality, as well as relapse-related costs in the no GVHD subgroup, would be interesting to explore further. Finally, the French SNDS database and linked datasets are claims and hospital practice datasets where missing data are possible and difficult to quantify. In particular, GVHD prophylaxis data was not fully captured.
In conclusion, in this nationwide population of French recipients of allo-HSCT, GVHD (in particular, aGVHD and a+cGVHD) was associated with significant clinical and economic burden, including higher rates of infection and mortality as well as increased hospitalizations and direct costs, compared with no GVHD. The results of this study highlight the significant unmet need for effective prophylaxis and treatment options for GVHD, which could reduce or prevent the clinical burden borne by patients experiencing GVHD of all types (in particular severe infections, and thus the need for GVHD treatments that do not further increase the risk of infection), the increased cost of allo-HSCT procedure due to aGVHD, and the potential development of cGVHD, itself leading to further increase in HCRU and costs. Recent advances in allo-HSCT technology, especially in the area of GVHD prevention and treatment, could add to the drug cost; however, it should also reduce the risk of complications and hence the overall clinical and economic burden.
Data availability
The patient-level data used for this study are not publicly available due to privacy restrictions. The aggregated data generated during the current study are available from the corresponding author on reasonable request.
References
Passweg JR, Baldomero H, Bregni M, Cesaro S, Dreger P, Duarte RF, et al. Hematopoietic SCT in Europe: data and trends in 2011. Bone Marrow Transplant. 2013;48:1161–7. https://doi.org/10.1038/bmt.2013.51.
Transplant Activity Survey. The European Society for Blood and Marrow Transplantation Web site. https://www.ebmt.org/registry/transplant-activity-survey Accessed 15 Mar 2022.
Passweg JR, Baldomero H, Chabannon C, Basak GW, Corbacioglu S, Duarte R, et al. The EBMT activity survey on hematopoietic-cell transplantation and cellular therapy 2018: CAR-T’s come into focus. Bone Marrow Transplant. 2020;55:1604–13. https://doi.org/10.1038/s41409-020-0826-4.
Thiebaut A, Lafuma A, Bureau I, Boyaval G, Bensoussan C, Godard C. Allogeneic stem cell transplant with graft versus host disease in France in 2012 based on national hospital databases (Pmsi). Value Health. 2014;17:A524. https://doi.org/10.1016/j.jval.2014.08.1647.
Ferrara J, Levine J, Reddy P, Holler E. Graft-versus-host disease. Lancet. 2009;373:1550–61. https://doi.org/10.1016/S0140-6736(09)60237-3.
Moreno DF, Cid J. Graft-versus-host disease. Med Clin. 2019;152:22–8. https://doi.org/10.1016/j.medcli.2018.07.012.
Socie G, Salooja N, Cohen A, Rovelli A, Carreras E, Locasciulli A, et al. Nonmalignant late effects after allogeneic stem cell transplantation. Blood. 2003;101:3373–85. https://doi.org/10.1182/blood-2002-07-2231.
Yu J, Judy JT, Parasuraman S, Sinha M, Weisdorf D. Inpatient healthcare resource utilization, costs, and mortality in adult patients with acute graft-versus-host disease, including steroid-refractory or high-risk disease, following allogeneic hematopoietic cell transplantation. Biol Blood Marrow Transplant. 2020;26:600–5. https://doi.org/10.1016/j.bbmt.2019.10.028.
Johnson BH, Taylor A, Kim G, Drahos J, Yang J, Akbari M, et al. Clinical outcomes and healthcare resource utilization for gastrointestinal acute graft-versus-host disease after allogeneic transplantation for hematologic malignancy: a retrospective US administrative claims database analysis. Biol Blood Marrow Transplant. 2019;25:834–41. https://doi.org/10.1016/j.bbmt.2018.12.839.
Yu J, Lal L, Anderson A, DuCharme M, Parasuraman S, Weisdorf D. Healthcare resource utilization and costs associated with acute graft-versus-host disease following allogeneic hematopoietic cell transplantation. Support Care Cancer. 2020;28:5491–9. https://doi.org/10.1007/s00520-020-05382-4.
Yu J, Parasuraman S, Shah A, Weisdorf D. Mortality, length of stay and costs associated with acute graft-versus-host disease during hospitalization for allogeneic hematopoietic stem cell transplantation. Curr Med Res Opin. 2019;35:983–8. https://doi.org/10.1080/03007995.2018.1551193.
Hooker DS, Grabe-Heyne K, Henne C, Bader P, Toumi M, Furniss SJ. Improved therapeutic approaches are needed to manage graft-versus-host disease. Clin Drug Investig. 2021;41:929–39.
Penack O, Marchetti N, Ruutu T, Aljurf M, Bacigalupo A, Bonifazi F, et al. Prophylaxis and management of graft versus host disease after stem-cell transplantation for haematological malignancies: updated consensus recommendations of the European Society for Blood and Marrow Transplantation. Lancet Haematol. 2020;7:e157–67.
Chao NJ. Clinical manifestations, diagnosis, and grading of acute graft-versus-host disease. In: Negrin RS, editor. UpToDate; 2020.
Garcia-Cadenas I, Rivera I, Martino R, Esquirol A, Barba P, Novelli S, et al. Patterns of infection and infection-related mortality in patients with steroid-refractory acute graft versus host disease. Bone Marrow Transplant. 2017;52:107–13. https://doi.org/10.1038/bmt.2016.225.
Matsumura-Kimoto Y, Inamoto Y, Tajima K, Kawajiri A, Tanaka T, Hirakawa T, et al. Association of cumulative steroid dose with risk of infection after treatment for severe acute graft-versus-host disease. Biol Blood Marrow Transplant. 2016;22:1102–7. https://doi.org/10.1016/j.bbmt.2016.02.020.
Singh AK, McGuirk JP. Allogeneic stem cell transplantation: a historical and scientific overview. Cancer Res. 2016;76:6445–51. https://doi.org/10.1158/0008-5472.CAN-16-1311.
Small TN, Papadopoulos EB, Boulad F, Black P, Castro-Malaspina H, Childs BH, et al. Comparison of immune reconstitution after unrelated and related T-cell-depleted bone marrow transplantation: effect of patient age and donor leukocyte infusions. Blood. 1999;93:467–80.
Atilla E, Atilla PA, Toprak SK, Demirer T. A review of late complications of allogeneic hematopoietic stem cell transplantations. Clin Transplant. 2017;31. https://doi.org/10.1111/ctr.13062.
Yu ZP, Ding JH, Wu F, Liu J, Wang J, Cheng J, et al. Quality of life of patients after allogeneic hematopoietic stem cell transplantation with antihuman thymocyte globulin. Biol Blood Marrow Transplant. 2012;18:593–9. https://doi.org/10.1016/j.bbmt.2011.08.009.
Young JH, Logan BR, Wu J, Wingard JR, Weisdorf DJ, Mudrick C, et al. Infections after transplantation of bone marrow or peripheral blood stem cells from unrelated donors. Biol Blood Marrow Transplant. 2016;22:359–70. https://doi.org/10.1016/j.bbmt.2015.09.013.
Stemberger C, Graef P, Odendahl M, Albrecht J, Dossinger G, Anderl F, et al. Lowest numbers of primary CD8(+) T cells can reconstitute protective immunity upon adoptive immunotherapy. Blood. 2014;124:628–37. https://doi.org/10.1182/blood-2013-12-547349.
Grubb W, Samuel Huse S, Alam N, Dychter S, Wingard R, Maihail S, et al. Economic burden of acute graft-versus-host disease (GvHD) following allogeneic hematopoietic cell transplant (HCT). Blood. 2016;128:22.
Schain F, Batyrbekova N, Liwing J, Baculea S, Webb T, Remberger M, et al. Real-world study of direct medical and indirect costs and time spent in healthcare in patients with chronic graft versus host disease. Eur J Health Econ. 2021;22:169–80. https://doi.org/10.1007/s10198-020-01249-x.
Farhadfar N, Leather HL, Wang S, Burton N, IrizarryGatell V, Itzler R, et al. Severity of acute graft-versus-host disease and associated healthcare resource utilization, cost, and outcomes. Transplant Cell Ther. 2021;27:1007.e1001–8.
Dignan FL, Potter MN, Ethell ME, Taylor M, Lewis L, Brennan J, et al. High readmission rates are associated with a significant economic burden and poor outcome in patients with grade III/IV acute GvHD. Clin Transplant. 2013;27:E56–63. https://doi.org/10.1111/ctr.12065.
Acknowledgements
This study was funded by CSL Behring and conducted independently by Certara Evidence & Access. Data were provided by the French Caisse Nationale d’Assurance Maladie (CNAM) and its staff involved in the project, in particular the DEMEX team. Support during the data application process was provided by the Health Data Hub, the Ethics and Scientific Committee for Health Research, Studies and Evaluations (CESREES), and the French Commission Nationale de l’Informatique et des Libertés (CNIL) governing data access and data privacy laws. Medical writing was provided by Cheryl Jones from Certara Synchrogenix, and editorial support was provided by Synergy Medical Communications. Both were funded by CSL Behring in accordance with Good Publications Practice (GPP 2022) guidelines (https://www.ismpp.org/gpp-2022).
Author information
Authors and Affiliations
Contributions
All authors contributed to writing this manuscript. DM, NQ, HJ, AB, KT, and MM contributed to the conception and/or design of this study, data analysis and interpretation. DR, MK and XZ also contributed to data analysis and interpretation.
Corresponding author
Ethics declarations
Competing interests
DM: Honoraria for consultancies: CSL Behring. MM: Honoraria for consultancies: CSL Behring. NQ and HJ: Consulting fees paid to Certara: CSL Behring. DR, MK, XZ and KT: employment: CSL Behring. AB: Consulting fees: CSL Behring, Neumentum, Healx.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Michonneau, D., Quignot, N., Jiang, H. et al. Clinical and economic burden associated with graft-versus-host disease following allogeneic hematopoietic cell transplantation in France. Bone Marrow Transplant 58, 514–525 (2023). https://doi.org/10.1038/s41409-023-01930-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-01930-8