Abstract
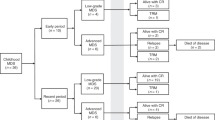
The comparison of haploidentical G-CSF-mobilized peripheral blood and bone marrow transplantation (HBMT) for patients with myelodysplastic syndrome (MDS) and haploidentical G-CSF-primed peripheral blood stem cell transplantation (HPBSCT) remains unclear. We performed a retrospective analysis using a propensity score method on 140 MDS patients who received HPBSCT (n = 46) or HBMT (n = 94) with BU/CY as a conditioning regimen prior to transplantation at our center between June 2016 and June 2021. HBMT recipients were associated with a reduced incidence of grade III-IV acute GVHD (17.22% vs. 30.57%, p = 0.019) within 100 days, reduced 2-year transplant-related mortality (TRM) (14.29% vs. 28.94%, p = 0.045) and superior 2-year overall survival (OS) (81.6% vs. 66.0%, p = 0.027), progression-free survival (PFS) (80.9% vs. 61.2%, p = 0.015), and GVHD relapse-free survival (GRFS) (64.6% vs. 53.3%, p = 0.062) compared with HPBSCT, but 2-year relapse incidence (RI) (5.96% vs. 9.39%, p = 0.445) was not affected. Multivariate analysis revealed that a GPB/GBM mixture was the independent factor for a reduced incidence of grade III-IV acute GVHD (p = 0.018) and TRM (p = 0.048), improved OS (p = 0.029), PFS (p = 0.019) and GRFS (p = 0.072). Collectively, the use of a GPB/GBM mixture as stem cell grafts for haplo-HSCT in patients with MDS appears to be an optimal choice.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Data availability
The datasets used and analyzed during the current study are available from the corresponding author on reasonable request.
References
Cazzola M. Myelodysplastic Syndromes. N. Engl J Med. 2020;383:1358–74.
Mo XD, Qin YZ, Zhang XH, Xu LP, Wang Y, Yan CH, et al. Minimal residual disease monitoring and preemptive immunotherapy in myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation. Ann Hematol. 2016;95:1233–40.
Gragert L, Eapen M, Williams E, Freeman J, Spellman S, Baitty R, et al. HLA match likelihoods for hematopoietic stem-cell grafts in the U.S. registry. N. Engl J Med. 2014;371:339–48.
Kwok J, Guo M, Yang W, Ip P, Chan GCF, Ho J, et al. Estimation of optimal donor number in Bone Marrow Donor Registry: Hong Kong’s experience. Hum Immunol. 2017;78:610–3.
Halagan M, Manor S, Shriki N, Yaniv I, Zisser B, Madbouly A, et al. East Meets West-Impact of Ethnicity on Donor Match Rates in the Ezer Mizion Bone Marrow Donor Registry. Biol Blood Marrow Transpl. 2017;23:1381–6.
van Walraven SM, Brand A, Bakker JN, Heemskerk MB, Nillesen S, Bierings MB, et al. The increase of the global donor inventory is of limited benefit to patients of non-Northwestern European descent. Haematologica. 2017;102:176–83.
Lee SJ, Klein J, Haagenson M, Baxter-Lowe LA, Confer DL, Eapen M, et al. High-resolution donor-recipient HLA matching contributes to the success of unrelated donor marrow transplantation. Blood. 2007;110:4576–83.
Flomenberg N, Baxter-Lowe LA, Confer D, Fernandez-Vina M, Filipovich A, Horowitz M, et al. Impact of HLA class I and class II high-resolution matching on outcomes of unrelated donor bone marrow transplantation: HLA-C mismatching is associated with a strong adverse effect on transplantation outcome. Blood. 2004;104:1923–30.
Luznik L, O’Donnell PV, Symons HJ, Chen AR, Leffell MS, Zahurak M, et al. HLA-haploidentical bone marrow transplantation for hematologic malignancies using nonmyeloablative conditioning and high-dose, posttransplantation cyclophosphamide. Biol Blood Marrow Transpl. 2008;14:641–50.
Brunstein CG, Fuchs EJ, Carter SL, Karanes C, Costa LJ, Wu J, et al. Alternative donor transplantation after reduced intensity conditioning: results of parallel phase 2 trials using partially HLA-mismatched related bone marrow or unrelated double umbilical cord blood grafts. Blood. 2011;118:282–8.
Bilmon IA, Kwan J, Gottlieb D, Kerridge I, McGurgan M, Huang G, et al. Haploidentical bone marrow transplants for haematological malignancies using non-myeloablative conditioning therapy and post-transplant immunosuppression with cyclophosphamide: results from a single Australian centre. Intern Med J. 2013;43:191–6.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transplant. 2006;38:291–7.
Lv M, Huang X. Fighting against hematological malignancy in China: from unique system to global impact. Sci China Life Sci. 2015;58:1183–90.
Apperley J, Niederwieser D, Huang XJ, Nagler A, Fuchs E, Szer J, et al. Haploidentical Hematopoietic Stem Cell Transplantation: A Global Overview Comparing Asia, the European Union, and the United States. Biol Blood Marrow Transpl. 2016;22:23–6.
Xu LP, Liu KY, Liu DH, Chen H, Han W, Chen YH, et al. The inferiority of G-PB to rhG-CSF-mobilized blood and marrow grafts as a stem cell source in patients with high-risk acute leukemia who underwent unmanipulated HLA-mismatched/haploidentical transplantation: a comparative analysis. Bone Marrow Transpl. 2010;45:985–92.
Zhao X, Gao F, Zhang X, Wang Y, Xu L, Liu K, et al. Improved clinical outcomes of rhG-CSF-mobilized blood and marrow haploidentical transplantation compared to propensity score-matched rhG-CSF-primed peripheral blood stem cell haploidentical transplantation: a multicenter study. Sci China Life Sci. 2016;59:1139–48.
Haukoos JS. LR. The Propensity Score. JAMA. 2015;314:1637–8.
Morgan CJ. Reducing bias using propensity score matching. J Nucl Cardiol. 2018;25:404–6.
Ruggeri A, Labopin M, Ciceri F, Mohty M, Nagler A. Definition of GvHD-free, relapse-free survival for registry-based studies: an ALWP-EBMT analysis on patients with AML in remission. Bone Marrow Transpl. 2016;51:610–1.
Przepiorka D, Weisdorf D, Martin P, Klingemann HG, Beatty P, Hows J, et al. 1994 Consensus Conference on Acute GVHD Grading. Bone Marrow Transplant. 1995;15:825–8.
Kunacheewa C, Ungprasert P, Phikulsod P, Issaragrisil S, Owattanapanich W. Comparative Efficacy and Clinical Outcomes of Haploidentical Stem Cell Transplantation to Other Stem Sources for Treatment in Acute Myeloid Leukemia and Myelodysplastic Syndrome Patients: A Systematic Review and Meta-Analysis. Cell Transpl. 2020;29:963689720904965.
Grunwald MR, Zhang M-J, Elmariah H, Johnson MH, St. Martin A, Bashey A, et al. Alternative donor transplantation for myelodysplastic syndromes: haploidentical relative and matched unrelated donors. Blood Adv. 2021;5:975–83.
Luznik L, Jalla S, Engstrom LW, Iannone R, Fuchs EJ. Durable engraftment of major histocompatibility complex-incompatible cells after nonmyeloablative conditioning with fludarabine, low-dose total body irradiation, and posttransplantation cyclophosphamide. Blood. 2001;98:3456–64.
Sengsayadeth S, Savani BN, Blaise D, Mohty M. Haploidentical transplantation: selecting optimal conditioning regimen and stem cell source. Semin Hematol. 2016;53:111–4.
Passweg JR, Baldomero H, Peters C, Gaspar HB, Cesaro S, Dreger P, et al. Hematopoietic SCT in Europe: data and trends in 2012 with special consideration of pediatric transplantation. Bone Marrow Transpl. 2014;49:744–50.
Stem Cell Trialists’ Collaborative G. Allogeneic peripheral blood stem-cell compared with bone marrow transplantation in the management of hematologic malignancies: an individual patient data meta-analysis of nine randomized trials. J Clin Oncol. 2005;23:5074–87.
Mielcarek M, Storer B, Martin PJ, Forman SJ, Negrin RS, Flowers ME, et al. Long-term outcomes after transplantation of HLA-identical related G-CSF-mobilized peripheral blood mononuclear cells versus bone marrow. Blood. 2012;119:2675–8.
Castagna L, Crocchiolo R, Furst S, Bramanti S, El Cheikh J, Sarina B, et al. Bone Marrow Compared with Peripheral Blood Stem Cells for Haploidentical Transplantation with a Nonmyeloablative Conditioning Regimen and Post-transplantation Cyclophosphamide. Biol Blood Marrow Transplant. 2014;20:724–9.
Salas MQ, Law AD, Lam W, Al-Shaibani Z, Loach D, Kim DDH, et al. Safety and Efficacy of Haploidentical Peripheral Blood Stem Cell Transplantation for Myeloid Malignancies Using Post-transplantation Cyclophosphamide and Anti-thymocyte Globulin as Graft-versus-Host Disease Prophylaxis. Clin Hematol Int. 2019;1:105–13.
Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Chen YH, et al. Superior graft-versus-leukemia effect associated with transplantation of haploidentical compared with HLA-identical sibling donor grafts for high-risk acute leukemia: an historic comparison. Biol Blood Marrow Transpl. 2011;17:821–30.
Wang Y, Liu DH, Xu LP, Liu KY, Chen H, Chen YH, et al. Haploidentical/mismatched hematopoietic stem cell transplantation without in vitro T cell depletion for T cell acute lymphoblastic leukemia. Biol Blood Marrow Transpl. 2012;18:716–21.
Huang XJ, Chang YJ. Unmanipulated HLA-mismatched/haploidentical blood and marrow hematopoietic stem cell transplantation. Biol Blood Marrow Transpl. 2011;17:197–204.
Wang HX, Yan HM, Wang ZD, Xue M, Liu J, Guo ZK. Haploidentical hematopoietic stem cell transplantation in hematologic malignancies with G-CSF mobilized bone marrow plus peripheral blood stem cells grafts without T cell depletion: a single center report of 29 cases. Leuk Lymphoma. 2012;53:654–9.
Chen XH, Zhang C, Zhang X, Gao L, Gao L, Kong PY, et al. Role of antithymocyte globulin and granulocyte-colony stimulating factor-mobilized bone marrow in allogeneic transplantation for patients with hematologic malignancies. Biol Blood Marrow Transpl. 2009;15:266–73.
Chen Y, Liu K, Xu L, Chen H, Liu D, Zhang X, et al. HLA-mismatched hematopoietic SCT without in vitro T-cell depletion for myelodysplastic syndrome. Bone Marrow Transpl. 2010;45:1333–9.
Beatty PG, Clift RA, Mickelson EM, Nisperos BB, Flournoy N, Martin PJ, et al. Marrow transplantation from related donors other than HLA-identical siblings. N. Engl J Med. 1985;313:765–71.
Guinan EC, Boussiotis VA, Neuberg D, Brennan LL, Hirano N, Nadler LM, et al. Transplantation of anergic histoincompatible bone marrow allografts. N. Engl J Med. 1999;340:1704–14.
Goldman FD, Rumelhart SL, DeAlacron P, Holida MD, Lee NF, Miller J, et al. Poor outcome in children with refractory/relapsed leukemia undergoing bone marrow transplantation with mismatched family member donors. Bone Marrow Transpl. 2000;25:943–8.
Chang YJ, Huang XJ, Zhao XY. In vivo induction of T-cell hyporesponsiveness and alteration of immunological cells of bone marrow grafts using granulocyte colony-stimulating factor. Haematologica. 2004;89:1517–24.
Chang YJ, Huang XJ, Zhao XY. A direct comparison of immunological characteristics of granulocyte colony-stimulating factor (G-CSF)-primed bone marrow grafts and G-CSF-mobilized peripheral blood grafts. Haematologica. 2005;90:715–6.
Rutella S, Zavala F, Danese S, Kared H, Leone G. Granulocyte colony-stimulating factor: a novel mediator of T cell tolerance. J Immunol. 2005;175:7085–91.
Zhao XY, Xu LL, Lu SY, Huang XJ. IL-17-producing T cells contribute to acute graft-versus-host disease in patients undergoing unmanipulated blood and marrow transplantation. Eur J Immunol. 2011;41:514–26.
Zhao XY, Lv M, Xu LL, Qian X, Huang XJ. Donor Th17 cells and IL-21 may contribute to the development of chronic graft-versus-host disease after allogeneic transplantation. Eur J Immunol. 2013;43:838–50.
Wen Q, Kong Y, Zhao HY, Zhang YY, Han TT, Wang Y, et al. G-CSF-induced macrophage polarization and mobilization may prevent acute graft-versus-host disease after allogeneic hematopoietic stem cell transplantation. Bone Marrow Transpl. 2019;54:1419–33.
Zhao XY, Wang YT, Mo XD, Zhao XS, Wang YZ, Chang YJ, et al. Higher frequency of regulatory T cells in granulocyte colony-stimulating factor (G-CSF)-primed bone marrow grafts compared with G-CSF-primed peripheral blood grafts. J Transl Med. 2015;13:145.
Huang XJ, Chang YJ, Zhao XY. Maintaining hyporesponsiveness and polarization potential of T cells after in vitro mixture of G-CSF mobilized peripheral blood grafts and G-CSF primed bone marrow grafts in different proportions. Transpl Immunol. 2007;17:193–7.
Chang YJ, Huang XJ. Haploidentical bone marrow transplantation without T-cell depletion. Semin Oncol. 2012;39:653–63.
Chang YJ, Huang XJ. Use of G-CSF-stimulated marrow in allogeneic hematopoietic stem cell transplantation settings: a comprehensive review. Clin Transpl. 2011;25:13–23.
Chang YJ, Huang XJ. Haploidentical hematopoietic stem cell transplantation with unmanipulated granulocyte colony stimulating factor mobilized marrow and blood grafts. Curr Opin Hematol. 2012;19:454–61.
Korbling M, Anderlini P. Peripheral blood stem cell versus bone marrow allotransplantation: does the source of hematopoietic stem cells matter? Blood. 2001;98:2900–8.
Issa JP. Optimizing therapy with methylation inhibitors in myelodysplastic syndromes: dose, duration, and patient selection. Nat Clin Pr Oncol. 2005;2:S24–9.
Toyota M, Kopecky KJ, Toyota MO, Jair KW, Willman CL, Issa JP. Methylation profiling in acute myeloid leukemia. Blood. 2001;97:2823–9.
Pinto AMM, Attadia V, Zappacosta S, Cimino R. Modulation of HLA-DR antigens expression in human myeloid leukaemia cells by cytarabine and 5-aza-2’-deoxycytidine. Lancet. 1984;2:867–8.
Pinto A, Zagonel V. 5-Aza-2’-deoxycytidine (Decitabine) and 5-azacytidine in the treatment of acute myeloid leukemias and myelodysplastic syndromes: past, present and future trends. Leukemia. 1993;7:51–60.
Acknowledgements
This work was supported in part by grants from the National Natural Science Foundation of China (81730003, 81870120, 82070187, 82020108003, 82000140), the Social Development Project of Jiangsu Province (BE2019655), the Jiangsu Province Key R&D Program (BE2019798), the Suzhou Science Project (SKY2021104), the Priority Academic Program Development of Jiangsu Higher Education Institutions (PAPD), the National Key Research and Development Program (2019YFC0840604), and the Natural Science Foundation of Jiangsu Province (BK20200197).
Author information
Authors and Affiliations
Contributions
Depei Wu and Yang Xu were responsible for the conception of the study and paper revision. Mengqian Chu, Shuhong Hu, and Yifan Shen contributed to performing the research study, analyzing data and writing the manuscript. Danya Shen and Yuchen Zhan helped complete the research study and perform data analysis. Yi Fan, Jia Chen and Xiaowen Tang contributed to the data analysis, manuscript writing and study supervision.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
41409_2022_1862_MOESM3_ESM.docx
Major causes of death after haploidentical hematopoietic cell transplantation in patients who received GPB or GPB/GBM mixed stem cell grafts.
41409_2022_1862_MOESM6_ESM.tif
Survival outcomes for MDS patients undergoing haplo-HSCT according to the use of decitabine bridging BU/CY in the conditioning regimen.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Chu, M., Hu, S., Shen, Y. et al. Comparison of clinical outcomes between peripheral blood stem cells and peripheral blood stem cells plus bone marrow in myelodysplastic syndrome patients with haploidentical transplantation. Bone Marrow Transplant 58, 142–151 (2023). https://doi.org/10.1038/s41409-022-01862-9
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-022-01862-9