Abstract
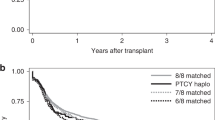
Allogeneic hematopoietic stem cell transplantation (allo-HSCT) is the most important curative method for intermediate- and high-risk adult acute myeloid leukemia (AML) patients. We aimed to identify the clinical outcomes of haploidentical related donor (HID) peripheral blood stem cell transplantation (PBSCT) who receiving peripheral blood (G-PB) harvest, and the patients receiving bone marrow (BM) plus G-PB harvest (BM + PB) as grafts were enrolled as control. The engraftments of neutrophil and platelet in G-PB group were both faster than those in BM + PB group. The cumulative incidences of grade II–IV acute graft-versus-host disease (aGVHD), and moderate to severe chronic GVHD (cGVHD) were all comparable between G-PB and BM + PB groups. The cumulative incidence of relapse and non-relapse mortality at 3 years after HID HSCT was 12.6% versus 13.7% (p = 0.899) and 3.6% versus 7.3% (p = 0.295), respectively, in G-PB and BM + PB group. While the probabilities of GVHD-free/relapse-free survival, leukemia-free survival, and overall survival at 3 years after HID HSCT were 60.6% versus 53.4% (p = 0.333), 83.8% versus 79.0% (p = 0.603), and were 87.3% versus 82.9% (p = 0.670), respectively. We confirmed the safety and efficacy of HID PBSCT in intermediate- and high-risk AML patients in a large cohort.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The dataset supporting the conclusions of this article is available in the clinical data repository of Peking University People’s Hospital. Individual participant data were not shared. For the original data, please contact moxiaodong@pkuph.edu.cn.
References
Lv M, Shen M, Mo X. Development of allogeneic hematopoietic stem cell transplantation in 2022: regenerating “Groot” to heal the world. Innovation. 2023;4:100373. https://doi.org/10.1016/j.xinn.2023.100373.
Zhang XH, Chen J, Han MZ, Huang H, Jiang EL, Jiang M, et al. The consensus from the Chinese Society of Hematology on indications, conditioning regimens and donor selection for allogeneic hematopoietic stem cell transplantation: 2021 update. J Hematol Oncol. 2021;14:145. https://doi.org/10.1186/s13045-021-01159-2.
Xu LP, Lu DP, Wu DP, Jiang EL, Liu DH, Huang H, et al. Hematopoietic stem cell transplantation activity in China 2020-2021 during the SARS-CoV-2 pandemic: a report from the Chinese Blood and Marrow Transplantation Registry Group. Transplant Cell Ther. 2023;29:136.e131–7. https://doi.org/10.1016/j.jtct.2022.11.011.
Xu LP, Lu PH, Wu DP, Sun ZM, Liu QF, Han MZ, et al. Hematopoietic stem cell transplantation activity in China 2019: a report from the Chinese Blood and Marrow Transplantation Registry Group. Bone Marrow Transplant. 2021;56:2940–7. https://doi.org/10.1038/s41409-021-01431-6.
Huang XJ, Zhu HH, Chang YJ, Xu LP, Liu DH, Zhang XH, et al. The superiority of haploidentical related stem cell transplantation over chemotherapy alone as postremission treatment for patients with intermediate- or high-risk acute myeloid leukemia in first complete remission. Blood. 2012;119:5584–90. https://doi.org/10.1182/blood-2011-11-389809.
Wang Y, Liu QF, Xu LP, Liu KY, Zhang XH, Ma X, et al. Haploidentical vs identical-sibling transplant for AML in remission: a multicenter, prospective study. Blood. 2015;125:3956–62. https://doi.org/10.1182/blood-2015-02-627786.
Ma YR, Xu LP, Zhang XH, Liu KY, Chang YJ, Lv M, et al. Allogeneic hematopoietic stem cell transplantation for intermediate-risk acute myeloid leukemia in the first remission: outcomes using haploidentical donors are similar to those using matched siblings. Ann Hematol. 2021;100:555–62. https://doi.org/10.1007/s00277-020-04359-x.
Bensinger WI, Martin PJ, Storer B, Clift R, Forman SJ, Negrin R, et al. Transplantation of bone marrow as compared with peripheral-blood cells from HLA-identical relatives in patients with hematologic cancers. N Engl J Med. 2001;344:175–81.
Couban S, Simpson DR, Barnett MJ, Bredeson C, Hubesch L, Howson-Jan K, et al. A randomized multicenter comparison of bone marrow and peripheral blood in recipients of matched sibling allogeneic transplants for myeloid malignancies. Blood. 2002;100:1525–31.
Friedrichs B, Tichelli A, Bacigalupo A, Russell NH, Ruutu T, Shapira MY, et al. Long-term outcome and late effects in patients transplanted with mobilised blood or bone marrow: a randomised trial. Lancet Oncol. 2010;11:331–8.
Jo T, Arai Y, Kondo T, Mizuno S, Hirabayashi S, Inamoto Y, et al. Advantages of peripheral blood stem cells from unrelated donors versus bone marrow transplants in outcomes of adult acute myeloid leukemia patients. Cytotherapy. 2022;24:1013–25. https://doi.org/10.1016/j.jcyt.2022.05.009.
Wang Y, Liu DH, Liu KY, Xu LP, Zhang XH, Han W, et al. Long-term follow-up of haploidentical hematopoietic stem cell transplantation without in vitro T cell depletion for the treatment of leukemia: nine years of experience at a single center. Cancer. 2013;119:978–85. https://doi.org/10.1002/cncr.27761.
Huang XJ, Liu DH, Liu KY, Xu LP, Chen H, Han W, et al. Haploidentical hematopoietic stem cell transplantation without in vitro T-cell depletion for the treatment of hematological malignancies. Bone Marrow Transplant. 2006;38:291–7. https://doi.org/10.1038/sj.bmt.1705445.
Xu LP, Wu DP, Han MZ, Huang H, Liu QF, Liu DH, et al. A review of hematopoietic cell transplantation in China: data and trends during 2008-2016. Bone Marrow Transplant. 2017;52:1512–8. https://doi.org/10.1038/bmt.2017.59.
Zhao X, Gao F, Zhang X, Wang Y, Xu L, Liu K, et al. Improved clinical outcomes of rhG-CSF-mobilized blood and marrow haploidentical transplantation compared to propensity score-matched rhG-CSF-primed peripheral blood stem cell haploidentical transplantation: a multicenter study. Sci China Life Sci. 2016;59:1139–48. https://doi.org/10.1007/s11427-016-0014-8.
Xu LP, Liu KY, Liu DH, Chen H, Han W, Chen YH, et al. The inferiority of G-PB to rhG-CSF-mobilized blood and marrow grafts as a stem cell source in patients with high-risk acute leukemia who underwent unmanipulated HLA-mismatched/haploidentical transplantation: a comparative analysis. Bone Marrow Transplant. 2010;45:985–92. https://doi.org/10.1038/bmt.2009.311.
Ma YR, Zhang X, Xu L, Wang Y, Yan C, Chen H, et al. G-CSF-primed peripheral blood stem cell haploidentical transplantation could achieve satisfactory clinical outcomes for acute leukemia patients in the first complete remission: a registered study. Front Oncol. 2021;11:631625. https://doi.org/10.3389/fonc.2021.631625.
Mo XD, Zhang YY, Zhang XH, Xu LP, Wang Y, Yan CH, et al. The role of collateral related donors in haploidentical hematopoietic stem cell transplantation. Sci Bull. 2018;63:1376–82. https://doi.org/10.1016/j.scib.2018.08.008.
Ma R, Huang XJ, Xu LP, Liu KY, Zhang XH, Yan CH, et al. Comparable outcomes after hematopoietic stem cell transplantation from mother donors and matched unrelated donors in patients with hematopoietic malignancies. Biol Blood Marrow Transplant. 2019;25:1210–7. https://doi.org/10.1016/j.bbmt.2019.01.030.
Wang Y, Liu QF, Lin R, Yang T, Xu YJ, Mo XD, et al. Optimizing antithymocyte globulin dosing in haploidentical hematopoietic cell transplantation: long-term follow-up of a multicenter, randomized controlled trial. Sci Bull. 2021;66:2498–505. https://doi.org/10.1016/j.scib.2021.06.002.
Mo XD, Hong SD, Zhao YL, Jiang EL, Chen J, Xu Y, et al. Basiliximab for steroid-refractory acute graft-versus-host disease: a real-world analysis. Am J Hematol. 2022;97:458–69. https://doi.org/10.1002/ajh.26475.
Shen MZ, Hong SD, Lou R, Chen RZ, Zhang XH, Xu LP, et al. A comprehensive model to predict severe acute graft-versus-host disease in acute leukemia patients after haploidentical hematopoietic stem cell transplantation. Exp Hematol Oncol. 2022;11:25. https://doi.org/10.1186/s40164-022-00278-x.
Fan S, Hong HY, Dong XY, Xu LP, Zhang XH, Wang Y, et al. Machine learning algorithm as a prognostic tool for Epstein-Barr virus reactivation after haploidentical hematopoietic stem cell transplantation. Blood Sci. 2023;5:51–9. https://doi.org/10.1097/bs9.0000000000000143.
Shen MZ, Hong SD, Wang J, Zhang XH, Xu LP, Wang Y, et al. A predicted model for refractory/recurrent cytomegalovirus infection in acute leukemia patients after haploidentical hematopoietic stem cell transplantation. Front Cell Infect Microbiol. 2022;12:862526. https://doi.org/10.3389/fcimb.2022.862526.
Chang YJ, Wang Y, Liu YR, Xu LP, Zhang XH, Chen H, et al. Haploidentical allograft is superior to matched sibling donor allograft in eradicating pre-transplantation minimal residual disease of AML patients as determined by multiparameter flow cytometry: a retrospective and prospective analysis. J Hematol Oncol. 2017;10:134. https://doi.org/10.1186/s13045-017-0502-3.
Mo XD, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, et al. Salvage chemotherapy followed by granulocyte colony-stimulating factor-primed donor leukocyte infusion with graft-vs.-host disease control for minimal residual disease in acute leukemia/myelodysplastic syndrome after allogeneic hematopoietic stem cell transplantation: prognostic factors and clinical outcomes. Eur J Haematol. 2016;96:297–308. https://doi.org/10.1111/ejh.12591.
Shen MZ, Zhang XH, Xu LP, Wang Y, Yan CH, Chen H, et al. Preemptive interferon-α therapy could protect against relapse and improve survival of acute myeloid leukemia patients after allogeneic hematopoietic stem cell transplantation: long-term results of two registry studies. Front Immunol. 2022;13:757002. https://doi.org/10.3389/fimmu.2022.757002.
Fan S, Pan TZ, Dou LP, Zhao YM, Zhang XH, Xu LP, et al. Preemptive interferon-α therapy could prevent relapse of acute myeloid leukemia following allogeneic hematopoietic stem cell transplantation: a real-world analysis. Front Immunol. 2023;14:1091014. https://doi.org/10.3389/fimmu.2023.1091014.
Döhner H, Wei AH, Appelbaum FR, Craddock C, DiNardo CD, Dombret H, et al. Diagnosis and management of AML in adults: 2022 recommendations from an international expert panel on behalf of the ELN. Blood. 2022;140:1345–77. https://doi.org/10.1182/blood.2022016867.
Schoemans HM, Lee SJ, Ferrara JL, Wolff D, Levine JE, Schultz KR, et al. EBMT-NIH-CIBMTR Task Force position statement on standardized terminology & guidance for graft-versus-host disease assessment. Bone Marrow Transplant. 2018;53:1401–15. https://doi.org/10.1038/s41409-018-0204-7.
Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695–706. https://doi.org/10.1002/(sici)1097-0258(19990330)18:63.0.co;2-o.
Bashey A, Zhang MJ, McCurdy SR, St Martin A, Argall T, Anasetti C, et al. Mobilized peripheral blood stem cells versus unstimulated bone marrow as a graft source for T-cell-replete haploidentical donor transplantation using post-transplant cyclophosphamide. J Clin Oncol. 2017;35:3002–9. https://doi.org/10.1200/jco.2017.72.8428.
Ruggeri A, Labopin M, Bacigalupo A, Gülbas Z, Koc Y, Blaise D, et al. Bone marrow versus mobilized peripheral blood stem cells in haploidentical transplants using posttransplantation cyclophosphamide. Cancer. 2018;124:1428–37. https://doi.org/10.1002/cncr.31228.
Zhao X, Zhao X, Huo M, Fan Q, Pei X, Wang Y, et al. Donor-specific anti-human leukocyte antigen antibodies predict prolonged isolated thrombocytopenia and inferior outcomes of haploidentical hematopoietic stem cell transplantation. J Immunol Res. 2017;2017:1043836. https://doi.org/10.1155/2017/1043836.
Champlin RE, Schmitz N, Horowitz MM, Chapuis B, Chopra R, Cornelissen JJ, et al. Blood stem cells compared with bone marrow as a source of hematopoietic cells for allogeneic transplantation. IBMTR Histocompatibility and Stem Cell Sources Working Committee and the European Group for Blood and Marrow Transplantation (EBMT). Blood. 2000;95:3702–9.
Zhao XS, Chen Y, Zhao XY, Liu DH, Xu LP, Wang Y, et al. Improved outcomes using G-CSF-mobilized blood and bone marrow grafts as the source of stem cells compared with G-PB after HLA-identical sibling transplantation in patients with acute leukemia. Clin Transplant. 2013;27:844–51. https://doi.org/10.1111/ctr.12225.
Mielcarek M, Storer B, Martin PJ, Forman SJ, Negrin RS, Flowers ME, et al. Long-term outcomes after transplantation of HLA-identical related G-CSF-mobilized peripheral blood mononuclear cells versus bone marrow. Blood. 2012;119:2675–8. https://doi.org/10.1182/blood-2011-12-396275.
Mo XD, Xu LP, Zhang XH, Liu DH, Wang Y, Chen H, et al. Chronic GVHD induced GVL effect after unmanipulated haploidentical hematopoietic SCT for AML and myelodysplastic syndrome. Bone Marrow Transplant. 2015;50:127–33. https://doi.org/10.1038/bmt.2014.223.
Xiao-Jun H, Lan-Ping X, Kai-Yan L, Dai-Hong L, Yu W, Huan C, et al. Partially matched related donor transplantation can achieve outcomes comparable with unrelated donor transplantation for patients with hematologic malignancies. Clin Cancer Res. 2009;15:4777–83. https://doi.org/10.1158/1078-0432.CCR-09-0691.
Acknowledgements
We sincerely thank all participating patients, The authors appreciate Dr. Qi Wen, Feng-Ting Dao, Dao-Xing Deng, Shuang Fan, Ze Guo, and Meng-Zhu Shen for their help in data collection.
Funding
This work was supported by the National Key Research and Development Program of China (2022YFA1103300, 2022YFC2502606), Major Program of the National Natural Science Foundation of China (82293630), the Key Program of the National Natural Science Foundation of China (81930004), the National Natural Science Foundation of China (82170208, 82200239), and CAMS Innovation Fund for Medical Sciences (2019-I2M-5-034, 2022-I2M-C&T-B-121), Peking University People’s Hospital Research and Development Funds (RZ2022-02), and the Fundamental Research Funds for the Central Universities.
Author information
Authors and Affiliations
Contributions
X-DM and X-JH conceived and designed the study. L-QC and W-XH collected and analyzed data as well as drafted the manuscript. All the authors contributed to samples collected and provided feedback on the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval and consent to participate
The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Institutional Review Board of Peking University People’s Hospital.
Consent for publication
Consent for publication was obtained from the patient.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Cao, LQ., Huo, WX., Zhang, XH. et al. Peripheral blood stem cell transplantation from haploidentical related donor could achieve satisfactory clinical outcomes for intermediate- or high-risk adult acute myeloid leukemia patients. Bone Marrow Transplant 59, 203–210 (2024). https://doi.org/10.1038/s41409-023-02117-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02117-x