Abstract
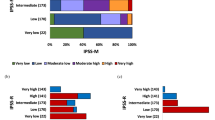
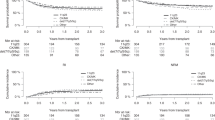
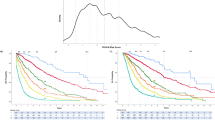
Cytogenetic abnormalities are a major risk factor for relapse after hematopoietic stem cell transplantation (HSCT) for myelodysplastic syndrome (MDS). We aimed to evaluate the value of the five-group cytogenetic classification according to the revised International Prognostic Scoring System (R-IPSS) for predicting the outcome after HSCT in pediatric patients with MDS. We retrospectively analyzed the Japanese registration data of 242 pediatric patients with MDS. According to the R-IPSS classification, 112 (45.5%) patients had good, 55 (22.7%) had intermediate, 64 (26.4%) had poor, and 11 (4.6%) had very poor cytogenetics. The 5-year overall survival (5yOS) was 72%, 69%, 59%, and 30% in the good, intermediate, poor, and very poor cytogenetic subgroups (p = 0.026), respectively. The very good, good, and intermediate subgroups were grouped into a “standard” subgroup and reclassified into three subgroups (standard, poor, and very poor). Patients with very poor risk had worse 5yOS (hazard ratio 2.17, 95% confidence interval (CI) 1.02–4.61; p = 0.04) and a much higher 5yCIR (hazard ratio 2.52, 95% CI 1.05–6.04; p = 0.04) than those of patients in the standard group in the multivariate analysis, indicating that very poor risk cytogenetic characteristics independently predicted worse outcome after HSCT in pediatric patients with MDS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Tefferi A, Vardiman JW. Myelodysplastic syndromes. N Engl J Med. 2009;361:1872–85.
Hasle H, Wadsworth LD, Massing BG, McBride M, Schultz KR. A population-based study of childhood myelodysplastic syndrome in British Columbia, Canada. Br J Haematol. 1999;106:1027–32.
Deeg HJ, Storer B, Slattery JT, Anasetti C, Doney KC, Hansen JA, et al. Conditioning with targeted busulfan and cyclophosphamide for hemopoietic stem cell transplantation from related and unrelated donors in patients with myelodysplastic syndrome. Blood. 2002;100:1201–7.
Armand P, Kim HT, DeAngelo DJ, Ho VT, Cutler CS, Stone RM, et al. Impact of cytogenetics on outcome of de novo and therapy-related AML and MDS after allogeneic transplantation. Biol Blood Marrow Transplant. 2007;13:655–64.
Greenberg PL, Cox C, LeBeau MM, Fenaux P, Morel P, Sanz G, et al. International scoring system for evaluating prognosis in myelodysplastic syndromes. Blood. 1997;89:2079–88.
Greenberg PL, Tuechler H, Schanz J, Sanz G, Garcia-Manero G, Solé F, et al. Revised international prognostic scoring system for myelodysplastic syndromes. Blood. 2012;120:2454–65.
Deeg HJ, Scott BL, Fang M, Shulman HM, Gyurkocza B, Myerson D, et al. Five-group cytogenetic risk classification, monosomal karyotype, and outcome after hematopoietic cell transplantation for MDS or acute leukemia evolving from MDS. Blood. 2012;120:1398–408.
Koenecke C, Göhring G, de Wreede LC, van Biezen A, Scheid C, Volin L, et al. Impact of the revised International Prognostic Scoring System, cytogenetics and monosomal karyotype on outcome after allogeneic stem cell transplantation for myelodysplastic syndromes and secondary acute myeloid leukemia evolving from myelodysplastic syndromes: a retrospective multicenter study of the European Society of Blood and Marrow Transplantation. Haematologica. 2015;100:400–8.
Della Porta MG, Alessandrino EP, Bacigalupo A, van Lint MT, Malcovati L, Pascutto C, et al. Predictive factors for the outcome of allogeneic transplantation in patients with MDS stratified according to the revised IPSS-R. Blood. 2014;123:2333–42.
Hasle H, Niemeyer CM, Chessells JM, Baumann I, Bennett JM, Kerndrup G, et al. A pediatric approach to the WHO classification of myelodysplastic and myeloproliferative diseases. Leukemia. 2003;17:277–82.
Atsuta Y, Suzuki R, Yoshimi A, Gondo H, Tanaka J, Hiraoka A, et al. Unification of hematopoietic stem cell transplantation registries in Japan and establishment of the TRUMP system. Int J Hematol. 2007;86:269–74.
Bennet JM, Catovsky D, Daniel MT, Flandrin G, Galton DA, Gralnick HR, et al. Proposals for the classification of the myelodysplastic syndromes. Br J Haematol. 1982;51:189–99.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A, et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood. 2009;114:937–51.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M, et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant. 2009;15:367–9.
Kanda Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013;48:452–8.
Andolina JR, Kletzel M, Tse WT, Jacobsohn DA, Duerst RE, Schneiderman J, et al. Allogeneic hematopoetic stem cell transplantation in pediatric myelodysplastic syndromes: improved outcomes for de novo disease. Pediatr Transplant. 2011;15:334–43.
Gohring G, Michalova K, Beverloo HB, Betts D, Harbott J, Haas OA, et al. Complex Karyotype newly defined: the strongest prognostic factor in advanced childhood myelodysplastic syndrome. Blood. 2010;116:3766–9.
Kikuchi A, Hasegawa D, Ohtsuka Y, Hamamoto K, Kojima S, Okamura J, et al. Outcome of children with refractory anaemia with excess of blast (RAEB) and RAEB in transformation (RAEB-T) in the Japanese MDS99 study. Br J Haematol. 2012;158:657–61.
Moriwaki K, Manabe A, Taketani T, Kikuchi A, Nakahata T, Hayashi Y. Cytogenetics and clinical features of pediatric myelodysplastic syndrome in Japan. Int J Hematol. 2014;100:478–84.
Luna-Fineman S, Shannon KM, Atwater SK, Davis J, Masterson M, Orgega J, et al. Myelodysplastic and myeloproliferative disorders of childhood: a study of 167 patients. Blood. 1999;93:459–66.
Oran B, Kongtim P, Popat U, de Lima M, Jabbour E, Lu X, et al. Cytogenetics, donor type, and use of hypomethylating agents in myelodysplastic syndrome with allogeneic stem cell transplantation. Biol Blood Marrow Transplant. 2014;20:1618–25.
Strahm B, Nolke P, Zecca M, Korthof ET, Bierings M, Furlan I, et al. Hematopoietic stem cell transplantation for advanced myelodysplastic syndrome in children: results of the EWOG-MDS 98 study. Leukemia. 2011;25:455–62.
Madureira ABM, Eapen M, Locatelli F, Teira P, Zhang MJ, Davies SM, et al. Analysis of risk factors influencing outcome in children with myelodysplastic syndrome after unrelated cord blood transplantation. Leukemia. 2011;25:449–54.
Wlodarski MW, Hirabayashi S, Pastor V, Starý J, Hasle H, Masetti R, et al. Prevalence, clinical characteristics, and prognosis of GATA2-related myelodysplastic syndromes in children and adolescents. Blood. 2016;127:1387–97.
Locatelli F, Strahm B. How I treat myelodysplastic syndromes of childhood. Blood. 2018;131:1406–14.
Basquiera AL, Pizzi S, Correas AG, Longo PG, Goldman WC, Prates MV, et al. Allogeneic hematopoietic stem cell transplantation in pediatric myelodysplastic syndromes: a multicenter experience from Argentina. Pediatr Blood Cancer. 2015;62:153–7.
Smith AR, Christiansen EC, Wagner JE, Cao Q, MacMillan ML, Stefanski HE, et al. Early hematopoietic stem cell transplant is associated with favorable outcomes in children with MDS. Pediatr Blood Cancer. 2013;60:705–10.
de Lima M, Giralt S, Thall PF, de Padua Silva L, Jones RB, Komanduri K, et al. Maintenance therapy with low-dose azacitidine after allogeneic hematopoietic stem cell transplantation for recurrent acute myelogenous leukemia or myelodysplastic syndrome: a dose and schedule finding study. Cancer. 2010;116:5420–31.
Bejar R, Stevenson K, Abdel-Wahab O, Galili N, Nilsson B, Garcia-Manero G, et al. Clinical effect of point mutations in myelodysplastic syndromes. N Engl J Med. 2011;364:2496–506.
Papaemmanuil E, Cazzola M, Boultwood J, Malcovati L, Vyas P, Bowen D, et al. Somatic SF3B1 mutation in myelodysplasia with ring sideroblasts. N Engl J Med. 2011;365:1384–95.
Bejar R, Stevenson K, Caughey B, Lindsley RC, Mar BG, Stojanov P, et al. Somatic mutations predict poor outcome in patients with myelodysplastic syndrome after hematopoietic stem-cell transplantation. J Clin Oncol. 2014;32:2691–8.
Acknowledgements
We thank all medical and co-medical staff who participated in the treatment of pediatric patients with MDS in Japan.
Author information
Authors and Affiliations
Contributions
SY, MK, KW, SI, DH, YA, and NY designed the study, SY performed the statistical analysis, SY, and NY wrote the paper, and MN, AH, MS, TK, FI, HY, YT, YK, YH, and AM were the principal investigators at the centers recruiting the highest number of patients for the study. All authors reviewed and approved the final version of the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Yamamoto, S., Kato, M., Watanabe, K. et al. Prognostic value of the revised International Prognostic Scoring System five-group cytogenetic abnormality classification for the outcome prediction of hematopoietic stem cell transplantation in pediatric myelodysplastic syndrome. Bone Marrow Transplant 56, 3016–3023 (2021). https://doi.org/10.1038/s41409-021-01446-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01446-z