Abstract
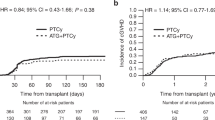
Serotherapeutic agents facilitate engraftment and prevent graft-versus-host disease (GVHD) following hematopoietic stem cell transplant. Anti-thymocyte globulin is generally added to conditioning chemotherapy for matched related donor transplant (MRD-HCT) for sickle cell disease (SCD). Alemtuzumab, however, is appealing due to its broad lymphocyte killing that may achieve very low rejection and GVHD rates. To assess the impact of alemtuzumab in MRD-HCT for SCD, we retrospectively reviewed transplant-related outcomes and markers of immunity in 38 consecutive patients at Texas Children’s Hospital having received myeloablative conditioning with alemtuzumab. Median follow-up was 4.8 years (range: 0.2–17). All patients engrafted. Donor chimerism was mixed in 47.1% of patients at ≥2-years. Donor chimerism <50% was uncommon (n = 2). One patient with low myeloid chimerism (19%) had sickle-related hemolysis at 10-years. Incidence of acute GVHD grade II–IV (5.3%) and extensive chronic GVHD (2.8%) was very low. Five-year event-free survival (EFS) and composite chronic GVHD-EFS were excellent at 94.7% (95% CI: 80.3, 98.6) and 89.2% (95% CI: 73.7, 95.8), respectively. Infections did not contribute to mortality although cytomegalovirus reactivation occurred commonly in the first 3 months after transplant. Our data suggest potential for alemtuzumab in myeloablative transplant for children with SCD although further evaluation in older patients and with unrelated donors is warranted.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Walters MC, Patience M, Leisenring W, Eckman JR, Scott JP, Mentzer WC, et al. Bone marrow transplantation for sickle cell disease. N Engl J Med. 1996;335:369–76. https://doi.org/10.1056/NEJM199608083350601. e-pub ahead of print 1996/08/08.
Vermylen C, Cornu G, Ferster A, Brichard B, Ninane J, Ferrant A, et al. Haematopoietic stem cell transplantation for sickle cell anaemia: the first 50 patients transplanted in Belgium. Bone marrow Transplant. 1998;22:1–6. https://doi.org/10.1038/sj.bmt.1701291. e-pub ahead of print 1998/07/25.
Dedeken L, Le PQ, Azzi N, Brachet C, Heijmans C, Huybrechts S, et al. Haematopoietic stem cell transplantation for severe sickle cell disease in childhood: a single centre experience of 50 patients. Br J Haematol. 2014;165:402–8. https://doi.org/10.1111/bjh.12737. e-pub ahead of print 2014/01/18.
Bernaudin F, Socie G, Kuentz M, Chevret S, Duval M, Bertrand Y, et al. Long-term results of related myeloablative stem-cell transplantation to cure sickle cell disease. Blood. 2007;110:2749–56. https://doi.org/10.1182/blood-2007-03-079665.
Gluckman E, Cappelli B, Bernaudin F, Labopin M, Volt F, Carreras J, et al. Sickle cell disease: an international survey of results of HLA-identical sibling hematopoietic stem cell transplantation. Blood. 2017;129:1548–56. https://doi.org/10.1182/blood-2016-10-745711.
Bernaudin F, Dalle JH, Bories D, de Latour RP, Robin M, Bertrand Y, et al. Long-term event-free survival, chimerism and fertility outcomes in 234 patients with sickle-cell anemia younger than 30 years after myeloablative conditioning and matched-sibling transplantation in France. Haematologica. 2020;105:91–101. https://doi.org/10.3324/haematol.2018.213207. e-pub ahead of print 2019/05/18.
Willemsen L, Jol-van der Zijde CM, Admiraal R, Putter H, Jansen-Hoogendijk AM, Ostaijen-Ten Dam MM, et al. Impact of serotherapy on immune reconstitution and survival outcomes after stem cell transplantations in children: thymoglobulin versus alemtuzumab. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2015;21:473–82. https://doi.org/10.1016/j.bbmt.2014.11.674.
Hale G, Waldmann H. CAMPATH-1 monoclonal antibodies in bone marrow transplantation. J Hematother. 1994;3:15–31. https://doi.org/10.1089/scd.1.1994.3.15. e-pub ahead of print 1994/01/01.
Hale G, Zhang MJ, Bunjes D, Prentice HG, Spence D, Horowitz MM, et al. Improving the outcome of bone marrow transplantation by using CD52 monoclonal antibodies to prevent graft-versus-host disease and graft rejection. Blood. 1998;92:4581–90. e-pub ahead of print 1998/12/09.
Contreras CF, Long-Boyle JR, Shimano KA, Melton A, Kharbanda S, Dara J, et al. Reduced Toxicity Conditioning for Nonmalignant Hematopoietic Cell Transplants. Biol Blood Marrow Transpl. 2020;26:1646–54. https://doi.org/10.1016/j.bbmt.2020.06.004. e-pub ahead of print 2020/06/11.
Abdel-Azim H, Mahadeo KM, Zhao Q, Khazal S, Kohn DB, Crooks GM, et al. Unrelated donor hematopoietic stem cell transplantation for the treatment of non-malignant genetic diseases: an alemtuzumab based regimen is associated with cure of clinical disease; earlier clearance of alemtuzumab may be associated with graft rejection. Am J Hematol. 2015;90:1021–6. https://doi.org/10.1002/ajh.24141. e-pub ahead of print 2015/08/06.
Bhatia M, Jin Z, Baker C, Geyer MB, Radhakrishnan K, Morris E, et al. Reduced toxicity, myeloablative conditioning with BU, fludarabine, alemtuzumab and SCT from sibling donors in children with sickle cell disease. Bone Marrow Transplant. 2014;49:913–20. https://doi.org/10.1038/bmt.2014.84.
Mahadeo KM, Weinberg KI, Abdel-Azim H, Miklos DB, Killen R, Kohn D, et al. A reduced-toxicity regimen is associated with durable engraftment and clinical cure of nonmalignant genetic diseases among children undergoing blood and marrow transplantation with an HLA-matched related donor. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2015;21:440–4. https://doi.org/10.1016/j.bbmt.2014.11.005. e-pub ahead of print 2014/12/03.
Myers GD, Krance RA, Weiss H, Kuehnle I, Demmler G, Heslop HE, et al. Adenovirus infection rates in pediatric recipients of alternate donor allogeneic bone marrow transplants receiving either antithymocyte globulin (ATG) or alemtuzumab (Campath). Bone Marrow Transplant. 2005;36:1001–8. https://doi.org/10.1038/sj.bmt.1705164. e-pub ahead of print 2005/09/27.
Chakrabarti S, Mackinnon S, Chopra R, Kottaridis PD, Peggs K, O’Gorman P, et al. High incidence of cytomegalovirus infection after nonmyeloablative stem cell transplantation: potential role of Campath-1H in delaying immune reconstitution. Blood. 2002;99:4357–63. https://doi.org/10.1182/blood.v99.12.4357. e-pub ahead of print 2002/05/31.
Shah AJ, Kapoor N, Crooks GM, Weinberg KI, Azim HA, Killen R, et al. The effects of Campath 1H upon graft-versus-host disease, infection, relapse, and immune reconstitution in recipients of pediatric unrelated transplants. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2007;13:584–93. https://doi.org/10.1016/j.bbmt.2007.01.076. e-pub ahead of print 2007/04/24.
Fitzhugh CD, Cordes S, Taylor T, Coles W, Roskom K, Link M, et al. At least 20% donor myeloid chimerism is necessary to reverse the sickle phenotype after allogeneic HSCT. Blood. 2017;130:1946–8. https://doi.org/10.1182/blood-2017-03-772392. e-pub ahead of print 2017/09/10.
Abraham A, Hsieh M, Eapen M, Fitzhugh C, Carreras J, Keesler D, et al. Relationship between Mixed Donor-Recipient Chimerism and Disease Recurrence after Hematopoietic Cell Transplantation for Sickle Cell Disease. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2017;23:2178–83. https://doi.org/10.1016/j.bbmt.2017.08.038.
Magnani A, Pondarre C, Bouazza N, Magalon J, Miccio A, Six E, et al. Extensive multilineage analysis in patients with mixed chimerism after allogeneic transplantation for sickle cell disease: insight into hematopoiesis and engraftment thresholds for gene therapy. Haematologica. 2019. https://doi.org/10.3324/haematol.2019.227561. e-pub ahead of print 2019/09/21.
Tomblyn M, Chiller T, Einsele H, Gress R, Sepkowitz K, Storek J, et al. Guidelines for preventing infectious complications among hematopoietic cell transplant recipients: a global perspective. Preface. Bone Marrow Transplant. 2009;44:453–5. https://doi.org/10.1038/bmt.2009.254. e-pub ahead of print 2009/10/29.
Tzannou I, Papadopoulou A, Naik S, Leung K, Martinez CA, Ramos CA, et al. Off-the-Shelf Virus-Specific T Cells to Treat BK Virus, Human Herpesvirus 6, Cytomegalovirus, Epstein-Barr Virus, and Adenovirus Infections After Allogeneic Hematopoietic Stem-Cell Transplantation. J Clin Oncol: Off J Am Soc Clin Oncol. 2017;35:3547–57. https://doi.org/10.1200/JCO.2017.73.0655. e-pub ahead of print 2017/08/08.
Papadopoulou A, Gerdemann U, Katari UL, Tzannou I, Liu H, Martinez C, et al. Activity of broad-spectrum T cells as treatment for AdV, EBV, CMV, BKV, and HHV6 infections after HSCT. Sci Transl Med. 2014;6:242ra283 https://doi.org/10.1126/scitranslmed.3008825. e-pub ahead of print 2014/06/27.
Shearer WT, Rosenblatt HM, Gelman RS, Oyomopito R, Plaeger S, Stiehm ER, et al. Lymphocyte subsets in healthy children from birth through 18 years of age: the Pediatric AIDS Clinical Trials Group P1009 study. J Allergy Clin Immunol. 2003;112:973–80. https://doi.org/10.1016/j.jaci.2003.07.003.
Glucksberg H, Storb R, Fefer A, Buckner CD, Neiman PE, Clift RA, et al. Clinical manifestations of graft-versus-host disease in human recipients of marrow from HL-A-matched sibling donors. Transplantation. 1974;18:295–304. https://doi.org/10.1097/00007890-197410000-00001. e-pub ahead of print 1974/10/01.
Shulman HM, Sullivan KM, Weiden PL, McDonald GB, Striker GE, Sale GE, et al. Chronic graft-versus-host syndrome in man. A long-term clinicopathologic study of 20 Seattle patients. Am J Med. 1980;69:204–17. e-pub ahead of print 1980/08/01.
Holtan SG, DeFor TE, Lazaryan A, Bejanyan N, Arora M, Brunstein CG, et al. Composite end point of graft-versus-host disease-free, relapse-free survival after allogeneic hematopoietic cell transplantation. Blood. 2015;125:1333–8. https://doi.org/10.1182/blood-2014-10-609032. e-pub ahead of print 2015/01/17.
Solh M, Zhang X, Connor K, Brown S, Solomon SR, Morris LE, et al. Factors Predicting Graft-versus-Host Disease-Free, Relapse-Free Survival after Allogeneic Hematopoietic Cell Transplantation: multivariable Analysis from a Single Center. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2016;22:1403–9. https://doi.org/10.1016/j.bbmt.2016.04.006. e-pub ahead of print 2016/04/21.
Henter JI, Horne A, Arico M, Egeler RM, Filipovich AH, Imashuku S, et al. HLH-2004: diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48:124–31. https://doi.org/10.1002/pbc.21039. e-pub ahead of print 2006/08/29.
Alzahrani M, Damlaj M, Jeffries N, Alahmari B, Singh A, Rondelli D, et al. Non-myeloablative human leukocyte antigen-matched related donor transplantation in sickle cell disease: outcomes from three independent centres. Br J Haematol. 2021;192:761–8. https://doi.org/10.1111/bjh.17311. e-pub ahead of print 2021/02/04.
Marsh RA, Fukuda T, Emoto C, Neumeier L, Khandelwal P, Chandra S, et al. Pretransplant Absolute Lymphocyte Counts Impact the Pharmacokinetics of Alemtuzumab. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2017;23:635–41. https://doi.org/10.1016/j.bbmt.2017.01.071. e-pub ahead of print 2017/01/17.
Marsh RA, Lane A, Mehta PA, Neumeier L, Jodele S, Davies SM, et al. Alemtuzumab levels impact acute GVHD, mixed chimerism, and lymphocyte recovery following alemtuzumab, fludarabine, and melphalan RIC HCT. Blood. 2016;127:503–12. https://doi.org/10.1182/blood-2015-07-659672. e-pub ahead of print 2015/12/09.
Brazauskas R, Scigliuolo GM, Wang HL, Cappelli B, Ruggeri A, Fitzhugh CD, et al. Risk score to predict event-free survival after hematopoietic cell transplant for sickle cell disease. Blood. 2020;136:623–6. https://doi.org/10.1182/blood.2020005687.
Ngwube A, Shah N, Godder K, Jacobsohn D, Hulbert ML, Shenoy S. Abatacept is effective as GVHD prophylaxis in unrelated donor stem cell transplantation for children with severe sickle cell disease. Blood Adv. 2020;4:3894–9. https://doi.org/10.1182/bloodadvances.2020002236. e-pub ahead of print 2020/08/20.
Saraf SL, Oh AL, Patel PR, Sweiss K, Koshy M, Campbell-Lee S, et al. Haploidentical Peripheral Blood Stem Cell Transplantation Demonstrates Stable Engraftment in Adults with Sickle Cell Disease. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2018;24:1759–65. https://doi.org/10.1016/j.bbmt.2018.03.031. e-pub ahead of print 2018/04/16.
Author information
Authors and Affiliations
Contributions
TDJ concept creation, data collection and analysis, manuscript writing. KY, GS, SB, BS, BO, JC, ED, CM manuscript editing. BF, HEH, RAK, KL concept creation, manuscript editing.
Corresponding author
Ethics declarations
Competing interests
Dr HEH is a co-founder with equity in Allovir and Marker Therapeutics, has served on advisory boards for Gilead, Kiadis, Novartis, Tessa Therapeutics and received research support from Tessa Therapeutics and Kuur Therapeutics.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
John, T.D., Friend, B., Yassine, K. et al. Matched related hematopoietic cell transplant for sickle cell disease with alemtuzumab: the Texas Children’s Hospital experience. Bone Marrow Transplant 56, 2797–2803 (2021). https://doi.org/10.1038/s41409-021-01415-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-021-01415-6
This article is cited by
-
Non-relapse cytopenias following allogeneic stem cell transplantation, a case based review
Bone Marrow Transplantation (2022)
-
Antineoplastics
Reactions Weekly (2022)