Abstract
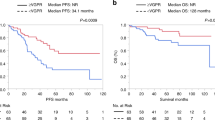
The application of high-dose melphalan and autologous stem cell transplant (SCT) to systemic AL amyloidosis (AL) has evolved over the past two decades and remains an important component of therapy for patients with AL. The era of novel agents created the opportunity to provide well -tolerated induction and post-SCT consolidation to AL patients eligible for SCT and the current availability of new monoclonal antibody therapies will likely provide additional opportunities to enhance the outcomes with SCT. In this review, we touch on the history of SCT for AL and examine the data on eligibility, mobilization, induction, risk-adapted melphalan dosing, engraftment, consolidation and maintenance, and long-term outcomes with SCT. We note that induction therapy may deprive some patients of the opportunity to proceed to SCT but is likely needed if the marrow plasmacytosis is > 10%, that risk-adapted melphalan dosing continues to be relevant, and that post-SCT consolidation improves the complete response rate as well as long-term overall survival. The importance of baseline cytogenetics is also highlighted, particularly for patients whose clonal plasma cells are ≤ 10% but harbor the t(11;14), because they may have improved survival with SCT.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Dispenzieri A, Kyle R, Merlini G, Miguel JS, Ludwig H, Hajek R, et al. International Myeloma Working Group guidelines for serum-free light chain analysis in multiple myeloma and related disorders. Leukemia. 2008;23:215–24.
Vrana JA, Gamez JD, Madden BJ, Theis JD, Bergen HR 3rd, Dogan A. Classification of amyloidosis by laser microdissection and mass spectrometry-based proteomic analysis in clinical biopsy specimens. Blood. 2009;114:4957–9.
Comenzo RL, Reece D, Palladini G, Seldin D, Sanchorawala V, Landau H, et al. Consensus guidelines for the conduct and reporting of clinical trials in systemic light-chain amyloidosis. Leukemia. 2012;26:2317–25.
Kyle RA, Linos A, Beard CM, Linke RP, Gertz MA, O’Fallon WM, et al. Incidence and natural history of primary systemic amyloidosis in Olmsted County, Minnesota, 1950 through 1989. Blood . 1992;79:1817–22.
Falk RH, Comenzo RL, Skinner M. The systemic amyloidoses. N Engl J Med. 1997;337:898–909.
Alexanian R, Haut A, Khan AU, Lane M, McKelvey EM, Migliore PJ, et al. Treatment for multiple myeloma. Combination chemotherapy with different melphalan dose regimens. JAMA. 1969;208:1680–5.
McElwain TJ, Powles RL. High-dose intravenous melphalan for plasma-cell leukaemia and myeloma. Lancet. 1983;2:822–4.
Barlogie B, Hall R, Zander A, Dicke K, Alexanian R. High-dose melphalan with autologous bone marrow transplantation for multiple myeloma. Blood. 1986;67:1298–301.
Merlini G. Treatment of primary amyloidosis. Semin Hematol. 1995;32:60–79.
Comenzo RL, Vosburgh E, Falk RH, Sanchorawala V, Reisinger J, Dubrey S, et al. Dose-intensive melphalan with blood stem-cell support for the treatment of AL (amyloid light-chain) amyloidosis: survival and responses in 25 patients. Blood. 1998;91:3662–70.
Kyle RA, Gertz MA, Greipp PR, Witzig TE, Lust JA, Lacy MQ, et al. A trial of three regimens for primary amyloidosis: colchicine alone, melphalan and prednisone, and melphalan, prednisone, and colchicine. N Engl J Med. 1997;336:1202–7.
Jaccard A, Moreau P, Leblond V, Leleu X, Benboubker L, Hermine O, et al. High-dose melphalan versus melphalan plus dexamethasone for AL amyloidosis. N Engl J Med. 2007;357:1083–93.
Sanchorawala V, Skinner M, Quillen K, Finn KT, Doros G, Seldin DC. Long-term outcome of patients with AL amyloidosis treated with high-dose melphalan and stem-cell transplantation. Blood. 2007;110:3561–3.
D’Souza A, Dispenzieri A, Wirk B, Zhang MJ, Huang J, Gertz MA, et al. Improved outcomes after autologous hematopoietic cell transplantation for light chain amyloidosis: a center for International Blood and Marrow Transplant Research Study. J Clin Oncol. 2015;33:3741–9.
Schonland SO, Dreger P, de Witte T, Hegenbart U. Current status of hematopoietic cell transplantation in the treatment of systemic amyloid light-chain amyloidosis. Bone Marrow Transplant. 2012;47:895–905.
Landau HJ, Gertz MA, Comenzo RL. Autologous hematopoietic cell transplantation for systemic light chain (AL-) amyloidosis. Thomas’ Hematopoietic Cell Transplantation. Eds. Stephen J. Forman MD, Robert S. Negrin MD, Joseph H. Antin MD, Frederick R. Appelbaum MD. John Wiley & Sons, Ltd; Singapore, USA. 2016. p. 724–41.
Wong SW, Larivee D, Warner M, Sprague KA, Fogaren T, Comenzo RL. Stem cell transplantation in patients with systemic AL amyloidosis referred for transplant after suboptimal responses to bortezomib-based initial therapy. Bone Marrow Transplant. 2017;52:936–7.
Cibeira MT, Sanchorawala V, Seldin DC, Quillen K, Berk JL, Dember LM, et al. Outcome of AL amyloidosis after high-dose melphalan and autologous stem cell transplantation: long-term results in a series of 421 patients. Blood. 2011;118:4346–52.
Sanchorawala V, Sun F, Quillen K, Sloan JM, Berk JL, Seldin DC. Long-term outcome of patients with AL amyloidosis treated with high-dose melphalan and stem cell transplantation: 20-year experience. Blood. 2015;126:2345–7.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79:319–28.
Gertz MA, Lacy MQ, Dispenzieri A, Hayman SR, Kumar SK, Leung N, et al. Effect of hematologic response on outcome of patients undergoing transplantation for primary amyloidosis: importance of achieving a complete response. Haematologica. 2007;92:1415–8.
Palladini G, Dispenzieri A, Gertz MA, Kumar S, Wechalekar A, Hawkins PN, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30:4541–9.
Sanchorawala V, Wright DG, Seldin DC, Falk RH, Finn KT, Dember LM, et al. High-dose intravenous melphalan and autologous stem cell transplantation as initial therapy or following two cycles of oral chemotherapy for the treatment of AL amyloidosis: results of a prospective randomized trial. Bone Marrow Transplant. 2004;33:381–8.
Sanchorawala V, Brauneis D, Shelton AC, Lo S, Sun F, Sloan JM, et al. Induction therapy with bortezomib followed by bortezomib-high dose melphalan and stem cell transplantation for light chain amyloidosis: results of a prospective clinical trial. Biol Blood Marrow Transplant. 2015;21:1445–51.
Landau H, Smith M, Landry C, Chou JF, Devlin SM, Hassoun H, et al. Long-term event-free and overall survival after risk-adapted melphalan and SCT for systemic light chain amyloidosis. Leukemia. 2017;31:136–42.
Dhakal B, Strouse C, D’Souza A, Arce-Lara C, Esselman J, Eastwood D, et al. Plerixafor and abbreviated-course granulocyte colony-stimulating factor for mobilizing hematopoietic progenitor cells in light chain amyloidosis. Biol Blood Marrow Transplant. 2014;20:1926–31.
Bashir Q, Langford LA, Parmar S, Champlin RE, Qazilbash MH. Primary systemic amyloid light chain amyloidosis decompensating after filgrastim-induced mobilization and stem-cell collection. J Clin Oncol. 2011;29:e79–80.
Girnius S, Seldin DC, Meier-Ewert HK, Sloan JM, Quillen K, Ruberg FL, et al. Safety and efficacy of high-dose melphalan and auto-SCT in patients with AL amyloidosis and cardiac involvement. Bone Marrow Transplant. 2014;49:434–9.
Yeh JC, Shank BR, Milton DR, Qazilbash MH. Adverse prognostic factors for morbidity and mortality during peripheral blood stem cell mobilization in patients with light chain amyloidosis. Biol Blood Marrow Transplant. 2017;24:815–9.
Lisenko K, Wuchter P, Hansberg M, Mangatter A, Benner A, Ho AD, et al. Comparison of different stem cell mobilization regimens in AL amyloidosis patients. Biol Blood Marrow Transplant. 2017;23:1870–8.
Perotti C, Del Fante C, Viarengo G, Perlini S, Vezzoli M, Rodi G, et al. Peripheral blood progenitor cell mobilization and collection in 42 patients with primary systemic amyloidosis. Transfusion. 2005;45:1729–34.
Fricker SP. Physiology and pharmacology of plerixafor. Transfus Med Hemother. 2013;40:237–45.
Comenzo RL, Sanchorawala V, Fisher C, Akpek G, Farhat M, Cerda S, et al. Intermediate-dose intravenous melphalan and blood stem cells mobilized with sequential GM + G-CSF or G-CSF alone to treat AL (amyloid light chain) amyloidosis. Br J Haematol. 1999;104:553–9.
Gertz MA, Lacy MQ, Dispenzieri A, Ansell SM, Elliott MA, Gastineau DA, et al. Risk-adjusted manipulation of melphalan dose before stem cell transplantation in patients with amyloidosis is associated with a lower response rate. Bone Marrow Transplant. 2004;34:1025–31.
Landau H, Hassoun H, Rosenzweig MA, Maurer M, Liu J, Flombaum C, et al. Bortezomib and dexamethasone consolidation following risk-adapted melphalan and stem cell transplantation for patients with newly diagnosed light-chain amyloidosis. Leukemia. 2013;27:823–8.
McCarthy PL, Holstein SA, Petrucci MT, Richardson PG, Hulin C, Tosi P, et al. Lenalidomide maintenance after autologous stem-cell transplantation in newly diagnosed multiple myeloma: a meta-analysis. J Clin Oncol. 2017;35:3279–89.
Scheid C, Sonneveld P, Schmidt-Wolf IG, van der Holt B, el Jarari L, Bertsch U, et al. Bortezomib before and after autologous stem cell transplantation overcomes the negative prognostic impact of renal impairment in newly diagnosed multiple myeloma: a subgroup analysis from the HOVON-65/GMMG-HD4 trial. Haematologica. 2014;99:148–54.
Dispenzieri A, Lacy MQ, Zeldenrust SR, Hayman SR, Kumar SK, Geyer SM, et al. The activity of lenalidomide with or without dexamethasone in patients with primary systemic amyloidosis. Blood. 2007;109:465–70.
Sanchorawala VFK, Fennessey S, Shelton A, Dember LM, Zeldis JB, Skinner M, et al. Durable haematologic complete responses can be achieved with lenalidomide in AL amyloidosis. Amyloid. 2010;17:84a.
Specter R, Sanchorawala V, Seldin DC, Shelton A, Fennessey S, Finn KT, et al. Kidney dysfunction during lenalidomide treatment for AL amyloidosis. Nephrol Dial Transplant. 2010;26:881–6.
Tapan U, Seldin DC, Finn KT, Fennessey S, Shelton A, Zeldis JB, et al. Increases in B-type natriuretic peptide (BNP) during treatment with lenalidomide in AL amyloidosis. Blood. 2010;116:5071–2.
Cowan AJ, Seldin DC, Skinner M, Quillen K, Doros G, Tan J, et al. Amyloid deposits in the bone marrow of patients with immunoglobulin light chain amyloidosis do not impact stem cell mobilization or engraftment. Biol Blood Marrow Transplant. 2012;18:1935–8.
Saba N, Sutton D, Ross H, Siu S, Crump R, Keating A, et al. High treatment-related mortality in cardiac amyloid patients undergoing autologous stem cell transplant. Bone Marrow Transplant. 1999;24:853–5.
Falk RH. Diagnosis and management of the cardiac amyloidoses. Circulation. 2005;112:2047–60.
Comenzo RL, Gertz MA. Autologous stem cell transplantation for primary systemic amyloidosis. Blood. 2002;99:4276–82.
Dispenzieri A, Gertz MA, Kyle RA, Lacy MQ, Burritt MF, Therneau TM, et al. Serum cardiac troponins and N-terminal pro-brain natriuretic peptide: a staging system for primary systemic amyloidosis. J Clin Oncol. 2004;22:3751–7.
Dispenzieri A, Gertz MA, Kyle RA, Lacy MQ, Burritt MF, Therneau TM, et al. Prognostication of survival using cardiac troponins and N-terminal pro-brain natriuretic peptide in patients with primary systemic amyloidosis undergoing peripheral blood stem cell transplantation. Blood. 2004;104:1881–7.
Gertz MA, Lacy MQ, Dispenzieri A, Kumar SK, Dingli D, Leung N, et al. Refinement in patient selection to reduce treatment-related mortality from autologous stem cell transplantation in amyloidosis. Bone Marrow Transplant. 2013;48:557–61.
Gertz MA, Leung N, Lacy MQ, Dispenzieri A, Zeldenrust SR, Hayman SR, et al. Clinical outcome of immunoglobulin light chain amyloidosis affecting the kidney. Nephrol Dial Transplant. 2009;24:3132–7.
Palladini G, Hegenbart U, Milani P, Kimmich C, Foli A, Ho AD, et al. A staging system for renal outcome and early markers of renal response to chemotherapy in AL amyloidosis. Blood. 2014;124:2325–32.
Wong SW, Toskic D, Warner M, Varga C, Moreno-Koehler A, Fein D, et al. Primary amyloidosis with renal involvement: outcomes in 77 consecutive patients at a single center. Clin Lymphoma Myeloma Leuk. 2017;17:759–66.
Leung N, Slezak JM, Bergstralh EJ, Dispenzieri A, Lacy MQ, Wolf RC, et al. Acute renal insufficiency after high-dose melphalan in patients with primary systemic amyloidosis during stem cell transplantation. Am J Kidney Dis. 2005;45:102–11.
Leung N, Kumar SK, Glavey SV, Dispenzieri A, Lacy MQ, Buadi FK, et al. The impact of dialysis on the survival of patients with immunoglobulin light chain (AL) amyloidosis undergoing autologous stem cell transplantation. Nephrol Dial Transplant. 2016;31:1284–9.
Munshi NC, Anderson KC, Bergsagel PL, Shaughnessy J, Palumbo A, Durie B, et al. Consensus recommendations for risk stratification in multiple myeloma: report of the International Myeloma Workshop Consensus Panel 2. Blood. 2011;117:4696–700.
Neben K, Lokhorst HM, Jauch A, Bertsch U, Hielscher T, van der Holt B, et al. Administration of bortezomib before and after autologous stem cell transplantation improves outcome in multiple myeloma patients with deletion 17p. Blood. 2012;119:940–8.
Neben K, Jauch A, Hielscher T, Hillengass J, Lehners N, Seckinger A, et al. Progression in smoldering myeloma is independently determined by the chromosomal abnormalities del(17p), t(4;14), gain 1q, hyperdiploidy, and tumor load. J Clin Oncol. 2013;31:4325–32.
Bochtler T, Hegenbart U, Cremer FW, Heiss C, Benner A, Hose D, et al. Evaluation of the cytogenetic aberration pattern in amyloid light chain amyloidosis as compared with monoclonal gammopathy of undetermined significance reveals common pathways of karyotypic instability. Blood. 2008;111:4700–5.
Bryce AH, Ketterling RP, Gertz MA, Lacy M, Knudson RA, Zeldenrust S, et al. Translocation t(11;14) and survival of patients with light chain (AL) amyloidosis. Haematologica. 2009;94:380–6.
Hayman SR, Bailey RJ, Jalal SM, Ahmann GJ, Dispenzieri A, Gertz MA, et al. Translocations involving the immunoglobulin heavy-chain locus are possible early genetic events in patients with primary systemic amyloidosis. Blood. 2001;98:2266–8.
Bochtler T, Hegenbart U, Kunz C, Granzow M, Benner A, Seckinger A, et al. Translocation t(11;14) is associated with adverse outcome in patients with newly diagnosed AL amyloidosis when treated with bortezomib-based regimens. J Clin Oncol. 2015;33:1371–8.
Bochtler T, Hegenbart U, Kunz C, Benner A, Kimmich C, Seckinger A, et al. Prognostic impact of cytogenetic aberrations in AL amyloidosis patients after high-dose melphalan: a long-term follow-up study. Blood. 2016;128:594–602.
Warsame R, Kumar SK, Gertz MA, Lacy MQ, Buadi FK, Hayman SR, et al. Abnormal FISH in patients with immunoglobulin light chain amyloidosis is a risk factor for cardiac involvement and for death. Blood Cancer J. 2015;5:e310.
Jaccard A, Comenzo RL, Hari P, Hawkins PN, Roussel M, Morel P, et al. Efficacy of bortezomib, cyclophosphamide and dexamethasone in treatment-naive patients with high-risk cardiac AL amyloidosis (Mayo Clinic stage III). Haematologica. 2014;99:1479–85.
Wechalekar AD, Schonland SO, Kastritis E, Gillmore JD, Dimopoulos MA, Lane T, et al. A European collaborative study of treatment outcomes in 346 patients with cardiac stage III AL amyloidosis. Blood. 2013;121:3420–7.
Weiss BM, Wong SW, Comenzo RL. Beyond the plasma cell: emerging therapies for immunoglobulin light chain amyloidosis. Blood 2016;127:2275–80. https://doi.org/10.1182/blood-2015-11-681650
Sanchorawala V, Palladini G, Kukreti V, Zonder JA, Cohen AD, Seldin DC, et al. A phase 1/2 study of the oral proteasome inhibitor ixazomib in relapsed or refractory AL amyloidosis. Blood. 2017;130:597–605.
Kaufman GP, Schrier SL, Lafayette RA, Arai S, Witteles RM, Liedtke M. Daratumumab yields rapid and deep hematologic responses in patients with heavily pretreated AL amyloidosis. Blood. 2017;130:900–2.
Gertz et al. Stem Cell Transplantation Compared With Melphalan Plus Dexamethasone in the Treatment of Immunoglobulin Light Chain Amyloidosis. Cancer. 2016.
M.A. Gertz, E. Blood, D.H. Vesole, et al. A multicenter phase 2 trial of stem cell transplantation for immunoglobulin light-chain amyloidosis (E4A97): an Eastern Cooperative Oncology Group Study Bone Marrow Transplant, 34 (2004), pp. 149–54.
Skinner et al. High-Dose Melphalan and Autologous Stem-Cell Transplantation in Patients with AL Amyloidosis: An 8-Year Study. Ann Int Med 2004;140:85–93.
Dispenzieri et al. Patients with immunoglobulin light chain amyloidosis undergoing autologous stem cell transplantation have superior outcomes compared with patients with multiple myeloma: a retrospective review from a tertiary referral center. Bone Marrow Transplantation volume 48, 1302–07 (2013).
Comenzo RL. How I treate amyloidosis. Blood. 2009.
Perfetti et al. Long term results of a risk-adapted approach to melphalan conditioning in ASCT for primary AL amyloidosis Haematologica, 2006.
Acknowledgements
We thank the Division of Hematology-Oncology and Departments of Medicine and Pathology and Laboratory Medicine at Tufts for their continued support, and also acknowledge the support by the Amyloidosis and Myeloma Research Fund at Tufts, the Cam Neely and John Davis Myeloma Research Fund, the John C Davis Program for Myeloma and Amyloid at Tufts, the Sidewater Family Fund, the Lavonne Horowitz Trust, the Werner and Elaine Dannheiser Fund for Research on the Biology of Aging of the Lymphoma Foundation, David and Barbara Levine (in memoriam), and the Demarest Lloyd Jr Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Varga, C., Comenzo, R.L. High-dose melphalan and stem cell transplantation in systemic AL amyloidosis in the era of novel anti-plasma cell therapy: a comprehensive review. Bone Marrow Transplant 54, 508–518 (2019). https://doi.org/10.1038/s41409-018-0284-4
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-018-0284-4
This article is cited by
-
Peripheral Nervous, Hepatic, and Gastrointestinal Endpoints for AL Amyloidosis Clinical Trials: Report from the Amyloidosis Forum Multi-organ System Working Group
Advances in Therapy (2023)
-
Amyloidosis with Cardiac Involvement: Identification, Characterization, and Management
Current Hematologic Malignancy Reports (2021)
-
Diagnosis and treatment of cardiac amyloidosis: position statement of the German Cardiac Society (DGK)
Clinical Research in Cardiology (2021)
-
The Amyloidosis Forum: a public private partnership to advance drug development in AL amyloidosis
Orphanet Journal of Rare Diseases (2020)