Abstract
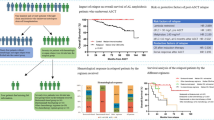
The goal of therapy in AL amyloidosis is to inhibit further production of the amyloidogenic light chains, thereby allowing organ recovery and improving survival. We aimed to assess the impact of depth of hematologic response prior to ASCT on survival. We conducted a retrospective study of 128 newly diagnosed AL amyloidosis patients who received induction prior to ASCT between January 2007 and August 2017 at Mayo Clinic. The overall response rate to induction was 86% (CR 18%, VGPR 31% and PR 38%). With a median follow up of 52 months, the median PFS and OS was 48.5 months and not reached, respectively. Response depth to induction therapy was associated with improved PFS and OS. The median PFS was not reached for patients achieving ≥VGPR prior to ASCT and 34.1 months for patients achieving PR or less (P = 0.0009). The median OS was longer in patients with deeper responses (not reached for ≥VGPR vs. 128 months for PR or less (P = 0.02)). On multivariable analysis, independent predictors of OS were melphalan conditioning dose (RR = 0.42; P = 0.036) and depth of response prior to transplant (RR 0.37; P = 0.0295). Hematologic response prior to transplant predicts improved post transplant outcomes in AL amyloidosis.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Merlini G, Bellotti V. Molecular mechanisms of amyloidosis. N Engl J Med. 2003;349:583–96. https://doi.org/10.1056/NEJMra023144.
Blancas-Mejia LM, Misra P, Dick CJ, Cooper SA, Redhage KR, Bergman MR, et al. Immunoglobulin light chain amyloid aggregation. Chem Commun (Camb, Engl). 2018;54:10664–74. https://doi.org/10.1039/c8cc04396e.
Afrough A, Saliba RM, Hamdi A, Honhar M, Varma A, Cornelison AM, et al. Impact of induction therapy on the outcome of immunoglobulin light chain amyloidosis after autologous hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2018;24:2197–203. https://doi.org/10.1016/j.bbmt.2018.07.010.
Palladini G, Dispenzieri A, Gertz MA, Kumar S, Wechalekar A, Hawkins PN, et al. New criteria for response to treatment in immunoglobulin light chain amyloidosis based on free light chain measurement and cardiac biomarkers: impact on survival outcomes. J Clin Oncol. 2012;30:4541–9. https://doi.org/10.1200/jco.2011.37.7614.
Muchtar E, Dispenzieri A, Leung N, Lacy MQ, Buadi FK, Dingli D, et al. Depth of organ response in AL amyloidosis is associated with improved survival: grading the organ response criteria. Leukemia. 2018;32:2240–9. https://doi.org/10.1038/s41375-018-0060-x.
Muchtar E, Gertz MA, Kumar SK, Lacy MQ, Dingli D, Buadi FK, et al. Improved outcomes for newly diagnosed AL amyloidosis between 2000 and 2014: cracking the glass ceiling of early death. Blood. 2017;129:2111–9. https://doi.org/10.1182/blood-2016-11-751628.
Vaxman I, Dispenzieri A, Muchtar E, Gertz M. New developments in diagnosis, risk assessment and management in systemic amyloidosis. Blood Rev. 2019:100636. https://doi.org/10.1016/j.blre.2019.100636.
Vij R, Kumar S, Zhang MJ, Zhong X, Huang J, Dispenzieri A, et al. Impact of pretransplant therapy and depth of disease response before autologous transplantation for multiple myeloma. Biol Blood Marrow Transplant. 2015;21:335–41. https://doi.org/10.1016/j.bbmt.2014.10.023. [published Online First: 2014/12/03]
Kim JS, Kim K, Cheong JW, Min YH, Suh C, Kim H, et al. Complete remission status before autologous stem cell transplantation is an important prognostic factor in patients with multiple myeloma undergoing upfront single autologous transplantation. Biol Blood Marrow Transplant. 2009;15:463–70. https://doi.org/10.1016/j.bbmt.2008.12.512.
Lahuerta JJ, Mateos MV, Martinez-Lopez J, Rosinol L, Sureda A, de la Rubia J, et al. Influence of pre- and post-transplantation responses on outcome of patients with multiple myeloma: sequential improvement of response and achievement of complete response are associated with longer survival. J Clin Oncol. 2008;26:5775–82. https://doi.org/10.1200/jco.2008.17.9721.
Miller KC, Gertz MA, Buadi FK, Hayman SR, Lacy MQ, Dispenzieri AA, et al. The impact of re-induction prior to salvage autologous stem cell transplantation in multiple myeloma. Bone Marrow Transplant 2019;54:2039–50. https://doi.org/10.1038/s41409-019-0590-5. [published Online First: 2019/06/14].
Jackson GH, Davies FE, Pawlyn C, Cairns DA, Striha A, Collett C, et al. Response-adapted intensification with cyclophosphamide, bortezomib, and dexamethasone versus no intensification in patients with newly diagnosed multiple myeloma (Myeloma XI): a multicentre, open-label, randomised, phase 3 trial. Lancet Haematol. 2019;6:e616–29. https://doi.org/10.1016/s2352-3026(19)30167-x.
Sanchorawala V, Wright DG, Seldin DC, Falk RH, Finn KT, Dember LM, et al. High-dose intravenous melphalan and autologous stem cell transplantation as initial therapy or following two cycles of oral chemotherapy for the treatment of AL amyloidosis: results of a prospective randomized trial. Bone Marrow Transplant. 2004;33:381–8. https://doi.org/10.1038/sj.bmt.1704346.
Sanchorawala V, Brauneis D, Shelton AC, Lo S, Sun F, Sloan JM, et al. Induction Therapy with Bortezomib Followed by Bortezomib-High Dose Melphalan and Stem Cell Transplantation for Light Chain Amyloidosis: Results of a Prospective Clinical Trial. Biol Blood Marrow Transplant: J Am Soc Blood Marrow Transplant. 2015;21:1445–51. https://doi.org/10.1016/j.bbmt.2015.04.001.
Huang X, Wang Q, Chen W, Zeng C, Chen Z, Gong D, et al. Induction therapy with bortezomib and dexamethasone followed by autologous stem cell transplantation versus autologous stem cell transplantation alone in the treatment of renal AL amyloidosis: a randomized controlled trial. BMC Med. 2014;12:2. https://doi.org/10.1186/1741-7015-12-2.
Hwa YL, Kumar SK, Gertz MA, Lacy MQ, Buadi FK, Kourelis TV, et al. Induction therapy pre-autologous stem cell transplantation in immunoglobulin light chain amyloidosis: a retrospective evaluation. Am J Hematol. 2016;91:984–8. https://doi.org/10.1002/ajh.24453.
Gupta VK, Brauneis D, Shelton AC, Quillen K, Sarosiek S, Sloan JM, et al. Induction therapy with bortezomib and dexamethasone and conditioning with high-dose melphalan and bortezomib followed by autologous stem cell transplantation for immunoglobulin light chain amyloidosis: long-term follow-up analysis. Biol Blood Marrow Transplant. 2019;25:e169–e73. https://doi.org/10.1016/j.bbmt.2019.01.007.
Minnema MC, Nasserinejad K, Hazenberg B, Hegenbart U, Vlummens P, Ypma PF, et al. Bortezomib-based induction followed by stem cell transplantation in light chain amyloidosis: results of the multicenter HOVON 104 trial. Haematologica. 2019;104:2274–82. https://doi.org/10.3324/haematol.2018.213900.
Rajkumar SV, Dimopoulos MA, Palumbo A, Blade J, Merlini G, Mateos MV, et al. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538–48. https://doi.org/10.1016/s1470-2045(14)70442-5.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79:319–28. https://doi.org/10.1002/ajh.20381.
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Colby C, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum free light chain measurements. J Clin Oncol. 2012;30:989–95. https://doi.org/10.1200/jco.2011.38.5724.
Comenzo RL, Reece D, Palladini G, Seldin D, Sanchorawala V, Landau H, et al. Consensus guidelines for the conduct and reporting of clinical trials in systemic light-chain amyloidosis. Leukemia. 2012;26:2317–25. https://doi.org/10.1038/leu.2012.100.
Reece DE, Hegenbart U, Sanchorawala V, Merlini G, Palladini G, Blade J, et al. Efficacy and safety of once-weekly and twice-weekly bortezomib in patients with relapsed systemic AL amyloidosis: results of a phase 1/2 study. Blood. 2011;118:865–73. https://doi.org/10.1182/blood-2011-02-334227.
Sidiqi MH, Aljama MA, Buadi FK, Warsame RM, Lacy MQ, Dispenzieri A, et al. Stem cell transplantation for light chain amyloidosis: decreased early mortality over time. J Clin Oncol. 2018;36:1323–9. https://doi.org/10.1200/jco.2017.76.9554.
Wong SW, Hegenbart U, Palladini G, Shah GL, Landau HJ, Warner M, et al. Outcome of patients with newly diagnosed systemic light-chain amyloidosis associated with deletion of 17p. Clin Lymphoma, Myeloma Leuk. 2018;18:e493–9. https://doi.org/10.1016/j.clml.2018.07.292.
Muchtar E, Gertz MA, Kourelis TV, Sidana S, Ronald SG, Lacy MQ, et al. Bone marrow plasma cells 20% or greater discriminate presentation, response, and survival in AL amyloidosis. Leukemia. 2019. https://doi.org/10.1038/s41375-019-0655-x.
Landau H, Hassoun H, Rosenzweig MA, Maurer M, Liu J, Flombaum C, et al. Bortezomib and dexamethasone consolidation following risk-adapted melphalan and stem cell transplantation for patients with newly diagnosed light-chain amyloidosis. Leukemia. 2013;27:823–8. https://doi.org/10.1038/leu.2012.274.
Funding
NCI SPORE MM SPORE 5P50 CA186781-04.
Author information
Authors and Affiliations
Contributions
IV designed the study, analyzed the data, wrote the first draft and approved the final version of the manuscript. HS designed the study and critically reviewed the manuscript and approved the final version of the manuscript. ASA analyzed the data and critically reviewed the manuscript and approved the final version of the manuscript. SK, EM, AD, FB, DD, ML, SH, NL, WG, TK, RE, and WH critically revised the manuscript and approved the final version of the manuscript. MAG designed the study, analyzed the data, wrote the first draft and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
Dr. Gertz reports personal fees from Ionis/Akcea, personal fees from Alnylam, personal fees from Prothena, personal fees from Celgene, personal fees from Janssen, grants and personal fees from Spectrum, personal fees from Annexon, personal fees from Appellis, personal fees from Amgen, personal fees from Medscape, personal fees from Physicians Education Resource, personal fees for Data Safety Monitoring board from Abbvie, personal fees from Research to Practice, speaker fees from Teva, Speaker fees from Johnson and Johnson; Speaker fees from Medscape, Speaker fees DAVA oncology; Advisory Board for Pharmacyclics Advisory Board for Proclara outside the submitted work; Development of educational materials for i3Health, Educational Program development i3Health, Royalties from Springer Publishing, Grant Funding Amyloidosis Foundation; International Waldenstrom Foundation. The authors declare that they have no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Vaxman, I., Sidiqi, M.H., Al Saleh, A.S. et al. Depth of response prior to autologous stem cell transplantation predicts survival in light chain amyloidosis. Bone Marrow Transplant 56, 928–935 (2021). https://doi.org/10.1038/s41409-020-01136-2
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-020-01136-2
This article is cited by
-
Risk factors, treatments and outcomes of patients with light chain amyloidosis who relapse after autologous stem cell transplantation
Bone Marrow Transplantation (2024)