Abstract
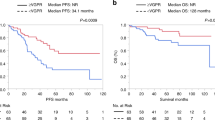
Relapse after ASCT is an important factor affecting the long-term prognosis of patients with AL amyloidosis. However, the risk factors of relapse are unknown and there are limited studies on treatment outcomes of these patients. We retrospectively reviewed 170 patients with AL amyloidosis who underwent ASCT between 2010 and 2021. Seventy-six patients confirmed as relapse and the median time from ASCT to relapse was 39 months. On multivariate analysis of variables before and after ASCT, lambda restricted, dFLC >30 mg/L pre ASCT, reduced dose melphalan and dFLC >10 mg/L at 6 months after ASCT were independent risk factors for relapse, and achieving CR after induction therapy and renal response after ASCT were protective factors. Most relapsed patients were treated with bortezomib-based regimens (50%) followed by daratumumab-based regimens (22.2%) and other chemotherapy regimens (13.9%). The overall hematological response in evaluable patients was 68.2% with 56.8% achieving CR/VGPR. The median PFS and OS from post-transplant relapse were 25 months and 81 months, respectively. Patients receiving bortezomib or daratumumab showed a better survival compared to other chemotherapy regimens. In conclusion, this study identified independent risk factors of post-transplant relapse and demonstrated the superiority of bortezomib or daratumumab treatment for these patients.
Clinical trial registration
NCT04210791.

This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
Data availability
The data are available from the corresponding author on reasonable request.
References
Sidiqi MH, Aljama MA, Buadi FK, Warsame RM, Lacy MQ, Dispenzieri A, et al. Stem cell transplantation for light chain amyloidosis: decreased early mortality over time. J Clin Oncol. 2018;36:1323–9.
Hwa YL, Warsame R, Gertz MA, Buadi FK, Lacy MQ, Kumar SK, et al. Delineation of the timing of second-line therapy post-autologous stem cell transplant in patients with AL amyloidosis. Blood. 2017;130:1578–84.
Ravichandran S, Law S, Mahmood S, Wisniowski B, Foard D, Fontana M, et al. Early relapse is an adverse prognostic marker in systemic immunoglobulin light chain (AL) Amyloidosis. Leukemia. 2022;36:1180–4.
Warsame R, Bang SM, Kumar SK, Gertz MA, Lacy MQ, Buadi F, et al. Outcomes and treatments of patients with immunoglobulin light chain amyloidosis who progress or relapse post autologous stem cell transplant. Eur J Haematol. 2014;92:485–90.
Al Saleh AS, Ebraheem MS, Sidiqi MH, Dispenzieri A, Muchtar E, Buadi FK, et al. Treatment and outcomes of patients with light chain amyloidosis who received a second line of therapy post autologous stem cell transplantation. Blood cancer J. 2022;12:59.
Browning S, Quillen K, Sloan JM, Doros G, Sarosiek S, Sanchorawala V. Hematologic relapse in AL amyloidosis after high-dose melphalan and stem cell transplantation. Blood. 2017;130:1383–6.
Gertz MA, Comenzo R, Falk RH, Fermand JP, Hazenberg BP, Hawkins PN, et al. Definition of organ involvement and treatment response in immunoglobulin light chain amyloidosis (AL): a consensus opinion from the 10th International Symposium on Amyloid and Amyloidosis, Tours, France, 18-22 April 2004. Am J Hematol. 2005;79:319–28.
Kumar S, Dispenzieri A, Lacy MQ, Hayman SR, Buadi FK, Colby C, et al. Revised prognostic staging system for light chain amyloidosis incorporating cardiac biomarkers and serum-free light chain measurements. J Clin Oncol. 2012;30:989–95.
Comenzo RL, Reece D, Palladini G, Seldin D, Sanchorawala V, Landau H, et al. Consensus guidelines for the conduct and reporting of clinical trials in systemic light-chain amyloidosis. Leukemia. 2012;26:2317–25.
Dittrich T, Bochtler T, Kimmich C, Becker N, Jauch A, Goldschmidt H, et al. AL amyloidosis patients with low amyloidogenic free light chain levels at first diagnosis have an excellent prognosis. Blood. 2017;130:632–42.
Gustine JN, Staron A, Szalat RE, Mendelson LM, Joshi T, Ruberg FL, et al. Predictors of hematologic response and survival with stem cell transplantation in AL amyloidosis: A 25-year longitudinal study. Am J Hematol. 2022;97:1189–99.
Ozga M, Zhao Q, Benson D Jr, Elder P, Williams N, Bumma N, et al. AL amyloidosis: The effect of fluorescent in situ hybridization abnormalities on organ involvement and survival. Cancer Med. 2021;10:965–73.
Bochtler T, Hegenbart U, Kunz C, Benner A, Seckinger A, Dietrich S, et al. Gain of chromosome 1q21 is an independent adverse prognostic factor in light chain amyloidosis patients treated with melphalan/dexamethasone. Amyloid : Int J Exp Clin Investig. 2014;21:9–17.
Sidiqi MH, Aljama MA, Muchtar E, Buadi FK, Warsame R, Lacy MQ, et al. Light chain type predicts organ involvement and survival in AL amyloidosis patients receiving stem cell transplantation. Blood Adv. 2018;2:769–76.
Tandon N, Muchtar E, Sidana S, Dispenzieri A, Lacy MQ, Dingli D, et al. Revisiting conditioning dose in newly diagnosed light chain amyloidosis undergoing frontline autologous stem cell transplant: impact on response and survival. Bone marrow Transplant. 2017;52:1126–32.
Hassan H, Verma K, Ferri G, Brauneis D, Quillen K, Sloan JM, et al. Modified high-dose versus high-dose melphalan conditioning in older patients undergoing autologous stem cell transplantation for immunoglobulin light chain amyloidosis. Transplant Cell Ther. 2022;28:761.e1–e7.
Vaxman I, Sidiqi MH, Al Saleh AS, Kumar S, Muchtar E, Dispenzieri A, et al. Depth of response prior to autologous stem cell transplantation predicts survival in light chain amyloidosis. Bone marrow Transplant. 2021;56:928–35.
D’Souza A, Dispenzieri A, Wirk B, Zhang MJ, Huang J, Gertz MA, et al. Improved outcomes after autologous hematopoietic cell transplantation for light chain amyloidosis: a center for international blood and marrow transplant research study. J Clin Oncol. 2015;33:3741–9.
Cowan AJ, Klippel ZK, Stevenson PA, Hyun TS, Tuazon S, Becker PS, et al. Pre-transplantation novel agent induction predicts progression-free survival for patients with immunoglobulin light-chain amyloidosis undergoing high-dose melphalan and autologous stem cell transplantation. Amyloid. 2016;23:254–9.
Huang X, Ren G, Chen W, Guo J, Zhao L, Zeng C, et al. The role of induction therapy before autologous stem cell transplantation in low disease burden AL amyloidosis patients. Amyloid. 2021;28:75–83.
Manwani R, Cohen O, Sharpley F, Mahmood S, Sachchithanantham S, Foard D, et al. A prospective observational study of 915 patients with systemic AL amyloidosis treated with upfront bortezomib. Blood. 2019;134:2271–80.
Shen KN, Miao HL, Zhang CL, Feng J, Zhang L, Cao XX, et al. Posttreatment dFLC less than 10 mg/L predicts superior organ response and longer time to next treatment in newly diagnosed light-chain amyloidosis patients treated with bortezomib. Leuk lymphoma. 2021;62:874–82.
Sarosiek S, Zheng L, Sloan JM, Quillen K, Brauneis D, Sanchorawala V. Comparing measures of hematologic response after high-dose melphalan and stem cell transplantation in AL amyloidosis. Blood cancer J. 2020;10:88.
Reece DE, Hegenbart U, Sanchorawala V, Merlini G, Palladini G, Blade J, et al. Long-term follow-up from a phase 1/2 study of single-agent bortezomib in relapsed systemic AL amyloidosis. Blood. 2014;124:2498–506.
Shimazaki C, Fuchida S, Suzuki K, Ishida T, Imai H, Sawamura M, et al. Phase 1 study of bortezomib in combination with melphalan and dexamethasone in Japanese patients with relapsed AL amyloidosis. Int J Hematol. 2016;103:79–85.
Venner CP, Lane T, Foard D, Rannigan L, Gibbs SD, Pinney JH, et al. Cyclophosphamide, bortezomib, and dexamethasone therapy in AL amyloidosis is associated with high clonal response rates and prolonged progression-free survival. Blood. 2012;119:4387–90.
Schwotzer R, Manz MG, Pederiva S, Waibel C, Caspar C, Lerch E, et al. Daratumumab for relapsed or refractory AL amyloidosis with high plasma cell burden. Hematol Oncol. 2019;37:595–600.
Shragai T, Gatt M, Lavie N, Vaxman I, Tadmor T, Rouvio O, et al. Daratumumab for relapsed AL amyloidosis-When cumulative real-world data precedes clinical trials: A multisite study and systematic literature review. Eur J Haematol. 2021;106:184–95.
Lecumberri R, Krsnik I, Askari E, Sirvent M, González-Pérez MS, Escalante F, et al. Treatment with daratumumab in patients with relapsed/refractory AL amyloidosis: a multicentric retrospective study and review of the literature. Amyloid. 2020;27:163–7.
Cohen OC, Brodermann MH, Blakeney IJ, Mahmood S, Sachchithanantham S, Ravichandran S, et al. Rapid response to single agent daratumumab is associated with improved progression-free survival in relapsed/refractory AL amyloidosis. Amyloid. 2020;27:200–5.
Sanchorawala V, Sarosiek S, Schulman A, Mistark M, Migre ME, Cruz R, et al. Safety, tolerability, and response rates of daratumumab in relapsed AL amyloidosis: results of a phase 2 study. Blood. 2020;135:1541–7.
Acknowledgements
The authors thank all members of the National Clinical Research Center of Kidney Diseases, Jinling Hospital for caring for AL amyloidosis patients and helping to extract data. This research was supported by the National Natural Science Foundation of China (82270767).
Author information
Authors and Affiliations
Contributions
YYZ and XHH designed the study, collected and analyzed the data, and wrote manuscript. JZG, WCC and LZ managed patients and revised the manuscript critically. All authors reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethics approval statement and patient consent statement
The study was approved by ethics committees of Jinling Hospital and was conducted according to the Declaration of Helsinki. All patients in this study have signed an informed consent form for the use of clinical data for research purposes.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Zhang, Y., Guo, J., Chen, W. et al. Risk factors, treatments and outcomes of patients with light chain amyloidosis who relapse after autologous stem cell transplantation. Bone Marrow Transplant 59, 350–358 (2024). https://doi.org/10.1038/s41409-023-02185-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41409-023-02185-z
This article is cited by
-
Relapsed systemic light chain amyloidosis – in search of a higher bar
Bone Marrow Transplantation (2024)