Abstract
Cholestasis is a major cause of a series of bile flow malfunction-related liver diseases. Pregnane X receptor (PXR) is a key regulator in endo- and xeno-biotics metabolism, which has been considered as a promising therapeutic target for cholestasis. In this study we conducted human PXR (hPXR) agonistic screening using dual-luciferase reporter gene assays, which led to discovering a series of potent hPXR agonists from a small Euphorbiaceae diterpenoid library, containing 35 structurally diverse diterpenoids with eight different skeleton types. The most active compound 6, a lathyrane diterpenoid (5/11/3 ring system), dose-dependently activated hPXR with a high selectivity, and significantly upregulated the expression of hPXR downstream genes CYP3A4 and UGT1A1. In LCA-induced cholestasis mouse model, administration of compound 6 (50 mg· kg−1. d−1, ip) for 7 days significantly suppressed liver necrosis and decreased serum levels of AST, ALT, Tbili, ALP, and TBA, ameliorating LCA-induced cholestatic liver injury. We further revealed that compound 6 exerted its anti-cholestatic efficacy via activation of PXR pathway, accelerating the detoxification of toxic BAs and promoting liver regeneration. These results suggest that lathyrane diterpenoids may serve as a promising scaffold for future development of anti-cholestasis drugs.

Similar content being viewed by others
Introduction
Cholestasis is a clinical condition characterized by an impairment of bile acids (BAs) formation and flow [1]. The progression of cholestasis will accompany with intrahepatic retention of toxic BAs, leading to a series of cholestatic liver diseases, such as primary biliary cholangitis (PBC) and primary sclerosing cholangitis (PSC) [2]. Thus, the prevailing therapeutic strategy against cholestasis is mainly focused on eliminating the excess toxic BAs to maintain its homeostasis. Currently, ursodeoxycholic acid (UDCA) and obeticholic acid (OCA) are the only two FDA-approved drugs for anti-cholestasis therapy. UDCA, as the first-line drug for PBC, could stimulate the secretion of hepatocytes and cholangiocytes via stabilization of the “biliary HCO3− umbrella” [3]. OCA could inhibit BAs synthesis and uptake by activation of farnesoid X receptor (FXR) and is indicated for patients who are intolerant or non-responsive to UDCA [3]. However, the limited responses to these drugs still leave PBC patients a high risk of progression to end-stage liver disease and death [4,5,6]. Therefore, the development of novel therapeutic agents with different mechanisms for the treatment of cholestasis is urgently needed.
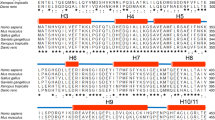
Pregnane X receptor (PXR, NR1I2) is a key member of nuclear receptor (NR) superfamily that comprises a DNA-binding domain (DBD), a ligand-binding domain (LBD), and a transactivation domain [7]. PXR is responsible for the metabolism of endobiotics (e.g., BAs, glucose, and lipids) and xenobiotics (e.g., drug and other therapeutic agents) [8,9,10] by regulating the expression of drug-metabolizing enzymes such as cytochrome P450 (CYPs), sulfotransferases (SULTs), and glucuronyltransferases (UGTs) [11], as well as numerous transporters [e.g., multidrug resistance protein 1 (MDR1) and multidrug resistance-associated proteins (MRPs)] [12]. Previous study has revealed the critical role of PXR in controlling the homeostasis of BAs [9]. After the activation of PXR, BAs undergo hydroxylation by phases I drug-metabolizing enzymes (e.g., CYP2B, CYP3A) and subsequent conjugation under the catalysis of phases II drug-metabolizing enzymes (e.g., UGTs, SULTs). These reactions will transform BAs to hydrophilic derivatives. PXR activation also upregulates the phase III transporters (e.g., MDR1), which finally efflux hydrophilic BAs metabolites into the bile or urine [13]. It has been reported that pregnenolone-16a-carbonitrile (PCN), a rodent PXR agonist, could protect against lithocholic acid (LCA)-induced cholestatic liver damage in wild-type mice, but fails in Pxr knockout mice [8, 14]. Rifampicin (RIF), a typical human PXR (hPXR) agonist, has recently shown to completely reverse severe persistent hepatocellular secretory failure induced by drugs or transient biliary obstruction in formerly healthy individuals [15]. These findings suggest that PXR is a promising therapeutic target for cholestasis, and the discovery of novel PXR agonists is of great value in anti-cholestasis drug development.
Natural products (NPs) have proved to be a valuable source of anti-cholestasis agents. The two approved PBC drugs, UDCA and OCA, are all derived from NPs. Recently, several NPs, such as tanshinone IIA, schisandrol B, solomonsterols A and B, have been identified as potent hPXR agonists [16,17,18]. All these underscored that seeking anti-cholestasis leads from natural sources might be a shortcut. In our continuing efforts toward discovering biologically active diterpenoids from Euphorbiaceae plants [19,20,21], we conducted hPXR agonistic screening from a small Euphorbiaceae diterpenoid library, containing 35 structurally diverse diterpenoids with eight different skeleton types. Interestingly, all of the lathyrane diterpenoids (1–7), featuring a macrocyclic ring system (5/11/3), exhibited potent activity. Among them, compound 6 with comparable efficacy to RIF was further evaluated for hepatoprotective effect against LCA-induced cholestatic liver injury in mice. Herein, we reported the discovery, in vivo anti-cholestasis efficacy, and the underlying mechanism of compound 6.
Materials and methods
Chemical and reagents
All compounds used in this study were obtained from an in-house Euphorbiaceae diterpenoid library (purity ≥95%). Chemical structures of Euphorbiaceae diterpenoids 1–35 were shown in Fig. S1. NMR spectra of compound 6 were shown in Figs. S3, S4. Dulbecco’s Modified Eagle’s Medium (DMEM) and fetal bovine serum (FBS) were purchased from Corning (New York, USA). Penicillin (100 U/mL) and streptomycin (100 μg/mL) were purchased from Gibco (Rockford, USA). Williams’ E medium (WEM), 1% ITS, 1% GlutaMAX were obtained from Thermo Fisher Scientific (Rockford, USA). Dexamethasone and RIF (purity ≥98%) were obtained from Sigma-Aldrich (Darmstadt, Germany) and dimethyl sulfoxide (DMSO) was purchased from MP Biomedicals (Irvine, USA). LCA was obtained from Aladdin Company (Shanghai, China). The pSG5-hPXR expression plasmid was generously offered by Dr. Steven Kliewer (University of Texas Southwestern Medical Center, Dallas, USA). The pGL3-CYP3A4-XREM luciferase reporter plasmid was generously offered by Dr. Jeff Staudinger (University of Kansas, Lawrence, USA). The pGL4.74-[hRluc/TK] control vector plasmid was obtained from Promega (Madison, USA). Rabbit polyclonal anti-CYP2B10 (A1463), anti-CYP3A11 (A2544) and anti-UGT1A1 (A6186) were purchased from ABclonal (Wuhan, China). Rabbit polyclonal anti-CDK4 (D120396) was purchased from Sangon (Shanghai, China). Rabbit monoclonal anti-PCNA (13110) and) anti-β-ACTIN (4970) were purchased from Cell Signaling Technology (Danvers, USA).
Cell culture
HEK293T cells were purchased from ATCC and cultured in DMEM medium supplemented with 10% FBS and 1% penicillin/streptomycin. Human hepatoma cell line HepaRG (Thermo Fisher Scientific, Rockford, USA) was cultured in WEM supplemented with 10% FBS, 1% ITS, 1% GlutaMAX, 1% penicillin/streptomycin and 0.1 μM dexamethasone for 2 weeks. Then, HepaRG cells were shifted to the same medium containing 2% DMSO (differentiation medium) for next 2 weeks. The cells were used for experiments after differentiation. Cells were all incubated at 37 °C with 5% CO2.
Dual-luciferase reporter assays
Dual-luciferase reporter gene assays were performed according to our previous description [17, 22, 23]. HEK293T cells were seeded in 96‐well plates at a density of 1.2 × 104 cells/well and then co-transfected with 100 ng pGL3‐CYP3A4‐XREM‐Luc, 50 ng pSG5‐hPXR, and 3 ng pGL4.74 [hRluc/TK] using Opti-MEM (Gibco, Danvers, USA) and Megatran 1.0 (OriGene, Rockville, USA) according to the manufacturer’s instructions. After 6 h transfection, the mixtures were replaced with new culture medium containing 10 μM hPXR positive agonist RIF or the tested compounds and incubated for 24 h. Luciferase activity was measured using a Dual-Luciferase Reporter Assay System Kit (Promega, Madison, USA) by an ultra-sensitive tube luminometer (Berthold, Germany). Renilla activity was measured as normalization to firefly luciferase activity for each well.
Quantitative reverse-transcription polymerase chain reaction
Total RNA isolation, cDNA synthesis and qRT-PCR analysis were performed as described previously [17]. Briefly, total RNA from HepaRG cells or mice liver tissues was purified using Trizol reagent (Invitrogen, Waltham, USA), and randomly reverse-transcribed to cDNA with PrimeScript RT reagent kit (Accurate biology, Changsha, China). qRT-PCR analysis for specific genes was performed using SYBR Premix Ex Taq II kit (Accurate biology, Changsha, China) in Applied Biosystems 7500 Real-Time PCR System. Relative mRNA expression was calculated by the Comparative CT method using Gapdh of mice or ACTB of HepaRG as reference. The gene-specific primer sequences are listed in Table S1.
Western blot analysis
Western blot analysis was performed according to our previous description [17]. Protein from liver tissues was extracted by RIPA lysis buffer (Biocolor BioScience and Technology, Shanghai, China) and protein concentration was determined using a BCA assay kit (Thermo Scientific, Rockford, USA). Protein extracts were subjected to SDS-PAGE and electrophoretically transferred to PVDF membranes (Millipore, Bedford, USA). The membranes were blocked with Tris-buffered saline containing 5% non-fat dry milk and then incubated with primary antibodies at 4 °C overnight, including CYP2B10, CYP3A11, UGT1A1, cyclin-dependent kinase 4 (CDK4), and proliferating cell nuclear antigen (PCNA). Then, the membranes were incubated with secondary horseradish peroxidase-conjugated anti-rabbit antibody (7074, Cell Signaling Technology, Danvers, USA) at room temperature for an hour. Protein bands were visualized by an enhanced chemiluminescence detection kit (Millipore, Bedford, USA). The intensity of specific bands was analyzed by Quantity One software (Bio-Rad Laboratories, Hercules, USA).
Animal treatment
C57BL/6 mice (6–8 weeks, 22–25 g) were obtained from Guangdong Medical Laboratory Animal Center, and housed in a specific pathogen free room with a constant room temperature, a 12/12 h light/dark cycle and free access to food and water. Mice were randomly divided into six groups including the vehicle, PCN, compound 6, LCA, LCA + PCN, and LCA + compound 6 group. The PCN, compound 6 (50 mg/kg) and LCA (125 mg/kg) were dissolved in corn oil, respectively. Mice of the PCN, LCA + PCN group or compound 6, LCA + compound 6 group were injected intraperitoneally with PCN (50 mg· kg−1· d−1) or compound 6 (50 mg· kg−1· d−1) for 7 days, respectively; while the vehicle and LCA group were injected intraperitoneally with equal corn oil. In addition, mice of the LCA, LCA + PCN, and LCA + compound 6 group were injected intraperitoneally with LCA (125 mg/kg) at the 4th day for twice daily by 4 successive days. Twelve hours after the last LCA injection, mice were sacrificed by CO2 asphyxia. Serum and liver samples were harvested and snap-frozen in liquid nitrogen, then stored at −80 °C. All animal experiments were approved by the Ethics Committee on the Care and Use of Laboratory Animals of Sun Yat-sen University (Guangzhou, China).
Histological and biochemical evaluation
Liver tissues were fixed in neutral buffered formalin, embedded in paraffin, sectioned and stained with hematoxylin & eosin (H&E). H&E-stained liver sections were examined by a DMI 3000B microscopy (Olympus, Tokyo Japan). Serum alanine aminotransferase (ALT), aspartate aminotransferase (AST), alkaline phosphatase (ALP), total bile acids (TBAs), and total bilirubin (Tbili) were analyzed using commercial kits according to the manufacturer’s instructions.
Statistical analysis
All the presented data and results were confirmed by at least three independent experiments. The data were presented as means ± SD and analyzed with GraphPad Prism 8.0 software (GraphPad Software, San Diego USA). Statistical differences between two groups were determined using Student’s t-test. For multiple group comparison, one-way ANOVA followed by Dunnett’s multiple comparison post hoc test was performed. A value of P < 0.05 was accepted as statistically significant.
Results
hPXR agonistic activity screening of Euphorbiaceae diterpenoids
Plants of the Euphorbiaceae family are well-known for producing highly functionalized diterpenes, namely Euphorbiaceae diterpenoids. In our continuing efforts toward discovering biologically active diterpenoids from Euphorbiaceae plants, an in-house Euphorbiaceae diterpenoid library, containing 35 structurally diverse diterpenoids with 8 different skeleton types (Fig. 1a, Table S2 and Supplementary Fig. S1), were screened for the hPXR agonistic activity in the current study. Cell viability assay revealed that all of the compounds had no obvious cytotoxicity on HEK293T cells at the concentration of 10 μM (Fig. 1b). Then, the dual-luciferase reporter gene assay was performed on HEK293T cells via transient transfection with reporter plasmids [17]. The results showed that 19 diterpenoids (1–8, 11–13, 15, 19, 20, 23–25, 30, and 34) could significantly increase the luciferase activity of reporter gene at 10 μM, as compared to the vehicle (Fig. 1c). It was worth noticing that all of the lathyrane diterpenoids (5/11/3 ring system, 1−7) exhibited potent hPXR agonistic activity. Among them, the most active compound 6, (7-hydroxy-lathyrol-3,5,7-triacetate) [24], could significantly activate hPXR at 2.7-fold as compared to the vehicle group, being comparable to RIF (activation fold = 2.9). Moreover, we have detected whether compound 6 can activate other NRs. Compound 6 could not activate hFXR or hLXRα at 10 μM and only exhibited low activation on hCAR, while the corresponding positive controls were active (Supplementary Fig. S2). These evidences suggested that lathyrane diterpenoids may serve as hPXR agonists and compound 6 showed the most promising efficacy.
a The skeletons of compounds in Euphorbiaceae diterpenoid library. b The cytotoxicity of compounds 1–35 (10 μM) on HEK293T cells. c Effect of compounds 1–35 on hPXR activation. Dual-luciferase reporter assays were performed in HEK293T cells transiently transfected with expression plasmid (pSG5-hPXR), reporter plasmid (pGL3-CYP3A4-XREM-Luc), and the control plasmid (pGL4.74-TK). Cells were treated with the positive agonist RIF (10 μM) or compounds 1–35 (10 μM) for 24 h. Data are presented as means ± SD (n = 3). *P < 0.05; **P < 0.01; ***P < 0.001, versus the vehicle.
Compound 6 activates hPXR and upregulates the expression of PXR downstream genes
Given the potent hPXR agonistic activity of compound 6, the dose-dependent assay was performed. As shown in Fig. 2b, compound 6 could dose-dependently increase the luciferase activity of reporter genes by 1.7-, 2.4-, 2.7-, and 5.2-fold at 1, 5, 10, 50 μM, respectively (compared to the vehicle). To determine the effect of compound 6 on hPXR-target genes responsible for BAs metabolism, HepaRG cells with a high expression of drug-metabolizing enzymes and transporters [11], were treated with compound 6 at 10 μM for 24 h. The qRT-PCR analysis showed that compound 6 significantly increased the mRNA expressions of CYP3A4 and UGT1A1 by 24.3- and 1.4-fold activity, respectively (Fig. 2d). These results indicated that compound 6 could dose-dependently activate hPXR and upregulate hPXR-target genes involved in BAs metabolism.
a The cytotoxicity of compound 6 (1, 5, 10, 50 μM) on HEK293T cells. b Dual-luciferase reporter assays were performed in HEK293T cells. Cells were treated with the positive agonist RIF (10 μM) or compound 6 (1, 5, 10, 50 μM) for 24 h. c The cytotoxicity of compound 6 (10 μM) on HepaRG cells. d qRT-PCR analysis of CYP3A4 and UGT1A1 mRNA levels after treatment with compound 6 (10 μM) for 24 h in HepaRG cells. Data are presented as means ± SD (n = 3). **P < 0.01; ***P < 0.001, versus the vehicle.
Compound 6 prevents against LCA-induced cholestatic liver injury in mice
The prominent hPXR agonistic activity of compound 6 in vitro prompted us to further evaluate its anti-cholestasis and hepatoprotective effects in vivo. Thus, LCA-induced cholestasis mice model was applied, and PCN, a well-known rodent PXR agonist, was used as the positive control drug. After treatment with LCA for 4 days, morphological and histopathological changes, including gall bladder enlargement, diffuse vacuolization, and neutrophils infusion, indicated the severe liver damage in the LCA group (Fig. 3). These changes were significantly ameliorated by the pretreatment with compound 6. Accordingly, the increased levels of serum ALT, AST, and Tbili induced by LCA were all significantly decreased in compound 6-pretreated mice, as compared to the LCA-induced group, with the reduction level by 47.3%, 58.0% and 68.1%, respectively (Fig. 4a, b, e). Meanwhile, pretreatment with compound 6 also dramatically decreased serum ALP and TBA, as compared to the LCA-induced group by 49.0% and 83.2% respectively (Fig. 4c, d). These results suggested that compound 6 could remarkablely protect against LCA-induced cholestatic liver injury in mice.
Serum ALT (a), AST (b), ALP (c), TBA (d), and Tbili (e) levels elevated by LCA, were significantly reduced by pretreatment with compound 6 or PCN. Data are presented as means ± SD (n = 4–7 for all groups). **P < 0.01; ***P < 0.001, versus the vehicle group respectively; #P < 0.05; ##P < 0.01; ###P < 0.001, versus the LCA-treated group respectively.
Compound 6 regulates PXR-mediated metabolize enzymes involved in BAs homeostasis in mice
To further verify whether the anti-cholestasis and hepatoprotective effects of compound 6 in vivo were due to the PXR activation, the expression of PXR target genes closely involved in BAs detoxification were detected. As shown in Fig. 5, treatment with PCN alone could significantly upregulate the mRNA expressions of Cyp2b10, Cyp3a11 and Ugt1a1, as compared to the vehicle. Similarly, compound 6 significantly upregulated Cyp3a11 and Ugt1a1, suggesting that compound 6 could activate PXR in mice. Upon LCA administration, pretreatment with PCN remarkably upregulated Cyp2b10, Cyp3a11, and Ugt1a1, as compared to LCA-induced group, while compound 6 pretreatment only significantly upregulated Cyp3a11, as compared to the vehicle. Consistent with the mRNA expression, Western blot analysis also showed that pretreatment with compound 6 markedly upregulated the protein expression of CYP3A11, as compared to the vehicle. Taken together, these data showed that compound 6 could activate PXR and upregulate PXR target genes involved in BAs homeostasis. However, its PXR activation effect in mice was weaker than that of PCN, which explained the better anti-cholestasis and hepatoprotective effects of PCN.
Hepatic gene expression of Cyp2b10 (a), Cyp3a11 (b), and Ugt1a1 (c) were determined using qRT-PCR analysis. Levels of CYP2B10, CYP3A11, and UGT1A1 (d) protein in mouse livers were determined by Western blot analysis. Data are presented as the means ± SD (n = 3 or 4). *P < 0.05; **P < 0.01; ***P < 0.001, versus the vehicle group respectively; ##P < 0.01; ###P < 0.001, versus the LCA-treated group respectively.
Compound 6 upregulates liver regeneration-related proteins
Our previous study has revealed that the activation of PXR could upregulate the expression of liver regeneration-related proteins such as CDK4 and PCNA, which resulted in the proliferation of hepatocyte and liver regeneration [25, 26]. Thus, the protein expression of CDK4 and PCNA were detected to explore the effect of compound 6 on liver regeneration (Fig. 6). Compared to the LCA-treated group, compound 6 could significantly increase the protein expression of CDK4 while increase PCNA to a slight extent. Also, compound 6 could induce CDK4 and PCNA expression. Similarly, pretreatment with PCN significantly upregulated the protein expression of CDK4 and a slight increase of PCNA expression was found. These findings suggested that compound 6 and PCN could upregulate liver regeneration-related protein to prevent against cholestatic liver injury.
Discussion
Cholestasis is a clinical condition where bile flow is defective, leading to a series of cholestatic liver diseases. Currently, the lack of clinic anti-cholestasis drugs (only UDCA and OCA) and their limited responses to patients pose an urgent need for the development of novel therapeutic agents to delay or relieve cholestasis-associated symptoms. PXR plays a crucial role in BAs detoxification by regulating the expression of the drug-metabolizing enzymes (e.g., CYP3A, CYP2B, and UGT1A1) and transporters (e.g., MDR1), and is considered as a promising therapeutic target for cholestasis.
Historically, NPs have played an irreplaceable role in drug discovery. Recent reports indicated that more than half of the FDA-approved clinical drugs between 1981 and 2014 were derived from NPs [27]. In past decades, diterpenoids occurring in plants of the Euphorbiaceae family, namely Euphorbiaceae diterpenoids, have attracted considerable interest from both natural product chemists and pharmacologists [28, 29]. Their potential druggability has been proved by our previous studies [19, 21, 30] and also by several marketed or clinical testing drugs, as exemplified by picato (ingenane-type) [31], resiniferatoxin (daphnane-type) [32], and prostratin (tigliane-type) [33]. In this context and in our continuing efforts toward discovering biologically active diterpenoids from Euphorbiaceae plants, an in-house Euphorbiaceae diterpenoid library with eight different skeleton types were screened for the hPXR agonistic activity in the current study. The results showed that half of diterpenoids could significantly activate hPXR at 10 μM. Noticeably, all of the lathyrane diterpenoids exhibited potent hPXR agonistic activity, and compound 6 showed the most potent efficacy comparable to RIF. Further investigation revealed that compound 6 can activate hPXR in a concentration-dependent manner and remarkably increased the expression of CYP3A4 and UGT1A1. Moreover, compound 6 could not activate hFXR and hLXRα while only exhibited low activation on hCAR, indicating that compound 6 has a high selectivity for hPXR.
Compound 6 (7-hydroxy-lathyrol-3,5,7-triacetate), possessing a lathyrane skeleton, is derived from a traditional Chinese medicine, Euphorbia lathyris. Lathyranes are the major components of E. lathyris and have been reported to possess a wide range of biological activities. Our current in vitro studies showed that compound 6 possessed prominent hPXR agonistic activity. To further evaluate its hepatoprotective effects against cholestatic liver injury in vivo, LCA-induced mice model was performed. As expected, treatment with LCA for 4 days resulted in the severe liver damages, while pretreatment with compound 6 could significantly ameliorate these changes. In serum biochemical markers, ALT, AST, and Tbili were characterized as crucial indicators of hepatocyte damage, while ALP and TBA were identified as important indicators of cholestasis [34]. The increases in serum ALT, AST, ALP, TBA and Tbili induced by LCA were all significantly attenuated in compound 6-pretreated mice. To verify whether the anti-cholestasis and hepatoprotective effects of compound 6 in vivo are due to its activation of PXR, PXR-mediated downstream genes involved in BAs detoxification were detected. qRT-PCR in combination with Western blot results showed that pretreatment with compound 6 could significantly upregulate the expression of CYP3A11. Taken together, compound 6 possessed potent PXR agonistic effect in vivo, which resulted in accelerating toxic BAs detoxification to prevent against intrahepatic cholestasis and liver injury. However, its agonistic effect in mice was weaker than that of PCN, which explained the dissatisfactory anti-cholestasis and hepatoprotective efficacy of compound 6 in vivo. Moreover, human and mouse PXR have 95% homology in the DBD, but only have 75% homology in the LBD [35]. PXR has significant inter-species differences in ligand-dependent activation, and whether compound 6 could protect against LCA-induced cholestatic liver injury in PXR-humanized (hPXR) mice should be further studied.
Although the regulation of bile acid homeostasis is considered as the prevailing therapeutic strategy for cholestatic liver diseases, promotion in liver regeneration could be an alternative approach. Liver regeneration is usually activated after partial hepatectomy or acute liver damage. Its mechanism involves activation of cell cycle-related pathways [36,37,38]. It has been reported that PXR activation by PCN can significantly promote liver regeneration after partial hepatectomy and liver regeneration process is delayed after partial hepatectomy in Pxr−/− mice, indicating that PXR and PXR activation play a crucial role in liver regeneration. The mechanisms include the modulation of the STAT3-mediated signaling pathway and genes involved in lipid metabolism such as PPARα, PPARγ, and FAE [39]. Most recently, we revealed that the activation of PXR could interact with yes-associated protein (YAP) and upregulate the expression of proliferation-related proteins such as CCNA1, CCND1, PCNA and CDK4, which led to the proliferation of hepatocyte and liver regeneration [25]. In this study, compound 6 could upregulate CDK4 as compared to the LCA-treated group. More importantly, compound 6 could induce CDK4 and PCNA expression. These results suggested that compound 6 could promote liver regeneration to prevent against LCA-induced cholestatic liver injury.
In summary, the hPXR-based anti-cholestatic screening from a small Euphorbiaceae diterpenoid library in the current study led to the discovery of a series of potent hPXR agonists. Interestingly, all of the lathyrane diterpenoids, featuring a 11-membered macro-ring, exhibited potent hPXR agonistic activity. The most active compound 6 could activate hPXR in a dose-dependent manner with a high selectivity and significantly upregulate the expressions of hPXR downstream genes CYP3A4 and UGT1A1. Further studies revealed that compound 6 could significantly ameliorate the LCA-induced cholestatic liver injury in mice and the activation of PXR pathway by compound 6 could accelerate the detoxification of toxic BAs and promote the liver regeneration. Our current study suggests that lathyrane diterpenoids may serve as a “privileged skeleton” in anti-cholestasis drug development and compound 6 is a promising lead pending further in-depth druggability evaluation.
References
Trauner M, Meier PJ, Boyer JL. Molecular pathogenesis of cholestasis. N Engl J Med. 1998;339:1217–27.
Ghonem NS, Assis DN, Boyer JL. On fibrates and cholestasis: a review. Hepatology. 2015;62:635–43.
Beuers U, Trauner M, Poupon R. New paradigms in the treatment of hepatic cholestasis: from UDCA to FXR, PXR and beyond. J Hepatol. 2015;62:S25–37.
Nevens F, Andreone P, Mazzella G, Strasser SI, Bowlus C, Invernizzi P, et al. A placebo-controlled trial of obeticholic acid in primary biliary cholangitis. N Engl J Med. 2016;375:631–43.
Goldstein J, Levy C. Novel and emerging therapies for cholestatic liver diseases. Liver Int. 2018;38:1520–35.
Harms MH, Lammers WJ, Thorburn D, Corpechot C, Invernizzi P, Janssen H, et al. Major hepatic complications in ursodeoxycholic acid-treated patients with primary biliary cholangitis: risk factors and time trends in incidence and outcome. Am J Gastroenterol. 2018;113:254–64.
Watkins RE, Wisely GB, Moore LB, Collins JL, Lambert MH, Williams SP, et al. The human nuclear xenobiotic receptor PXR: structural determinants of directed promiscuity. Science. 2001;292:2329–33.
Staudinger JL, Goodwin B, Jones SA, Hawkins-Brown D, MacKenzie KI, LaTour A, et al. The nuclear receptor PXR is a lithocholic acid sensor that protects against liver toxicity. Proc Natl Acad Sci USA. 2001;98:3369–74.
Chen Y, Tang Y, Guo C, Wang J, Boral D, Nie D. Nuclear receptors in the multidrug resistance through the regulation of drug-metabolizing enzymes and drug transporters. Biochem Pharmacol. 2012;83:1112–26.
Swanson HI, Wada T, Xie W, Renga B, Zampella A, Distrutti E, et al. Role of nuclear receptors in lipid dysfunction and obesity-related diseases. Drug Metab Dispos. 2013;41:1–11.
Rosenfeld JM, Vargas R Jr, Xie W, Evans RM. Genetic profiling defines the xenobiotic gene network controlled by the nuclear receptor pregnane X receptor. Mol Endocrinol. 2003;17:1268–82.
Synold TW, Dussault I, Forman BM. The orphan nuclear receptor SXR coordinately regulates drug metabolism and efflux. Nat Med. 2001;7:584–90.
Jonker JW, Liddle C, Downes M. FXR and PXR: Potential therapeutic targets in cholestasis. J Steroid Biochem. 2012;130:147–58.
Xie W, Radominska-Pandya A, Shi Y, Simon CM, Nelson MC, Ong ES, et al. An essential role for nuclear receptors SXR/PXR in detoxification of cholestatic bile acids. Proc Natl Acad Sci USA. 2001;98:3375–80.
van Dijk R, Kremer AE, Smit W, van den Elzen B, van Gulik T, Gouma D, et al. Characterization and treatment of persistent hepatocellular secretory failure. Liver Int. 2015;35:1478–88.
Zhang X, Ma Z, Liang Q, Tang X, Hu D, Liu C, et al. Tanshinone IIA exerts protective effects in a LCA-induced cholestatic liver model associated with participation of pregnane X receptor. J Ethnopharmacol. 2015;164:357–67.
Zeng H, Jiang Y, Chen P, Fan X, Li D, Liu A, et al. Schisandrol B protects against cholestatic liver injury through pregnane X receptors. Br J Pharmacol. 2017;174:672–88.
Festa C, De Marino S, D'Auria MV, Bifulco G, Renga B, Fiorucci S, et al. Solomonsterols A and B from Theonella swinhoei. the first example of C-24 and C-23 sulfated sterols from a marine source endowed with a PXR agonistic activity. J Med Chem. 2010;54:401–5.
Zhu J, Wang R, Lou L, Li W, Tang G, Bu X, et al. Jatrophane diterpenoids as modulators of P-glycoprotein-dependent multidrug resistance (MDR): advances of structure-activity relationships and discovery of promising MDR reversal agents. J Med Chem. 2016;59:6353–69.
Li W, Wang RM, Pan YH, Zhao YY, Yuan FY, Huang D, et al. Crotonpenoids A and B, two highly modified clerodane diterpenoids with a tricyclo [7.2.1.02,7] dodecane core from Croton yanhuii: isolation, structural elucidation, and biomimetic semisynthesis. Org Lett. 2020;22:4435–9.
Sang J, Li W, Diao HJ, Fan RZ, Huang JL, Gan L, et al. Jolkinolide B targets thioredoxin and glutathione systems to induce ROS-mediated paraptosis and apoptosis in bladder cancer cells. Cancer Lett. 2021;509:13–25.
Fan S, Liu C, Jiang Y, Gao Y, Chen Y, Fu K, et al. Lignans from Schisandra sphenanthera protect against lithocholic acid-induced cholestasis by pregnane X receptor activation in mice. J Ethnopharmacol. 2019;245:112103–12.
Zhao YY, Yao XP, Jiao TY, Tian JN, Gao Y, Fan SC, et al. Schisandrol B promotes liver enlargement via activation of PXR and YAP pathways in mice. Phytomedicine. 2021;84:153520–6.
Narayanan P, Röhrl M, Zechmeister K, Engel DW, Hoppe W. Structure of 7-hydroxy-lathyrol a further diterpene from Euphorbia lathyris. Tetrahedron Lett. 1971;12:1325–8.
Jiang Y, Feng D, Ma X, Fan S, Gao Y, Fu K, et al. Pregnane X receptor regulates liver size and liver cell fate by yes-associated protein activation in mice. Hepatology. 2019;69:343–58.
Li X, Sun J, Fan X, Guan L, Li D, Zhou Y, et al. Schisandrol B promotes liver regeneration after partial hepatectomy in mice. Eur J Pharmacol. 2019;818:96–102.
Newman DJ, Cragg GM. Natural products as sources of new drugs from 1981 to 2014. J Nat Prod. 2016;79:629–61.
Shi Q-W, Su X-H, Kiyota H. Chemical and pharmacological research of the plants in genus Euphorbia. Chem Rev. 2008;108:4295–327.
Vasas A, Hohmann J. Euphorbia diterpenes: isolation, structure, biological activity, and synthesis. Chem Rev. 2014;114:8579–612.
Song Q-Q, Rao Y, Tang GH, Sun ZH, Zhang JS, Huang ZS, et al. Tigliane diterpenoids as a new type of antiadipogenic agents inhibit GRα-dexras1 axis in adipocytes. J Med Chem. 2019;62:2060–75.
Gupta AK, Paquet M. Ingenol mebutate: a promising treatment for actinic keratoses and nonmelanoma skin cancers. J Cutan Med Surg. 2013;17:173–9.
Kissin I, Szallasi A. Therapeutic targeting of TRPV1 by resiniferatoxin, from preclinical studiesto clinical trials. Curr Top Med Chem. 2011;11:2159–70.
Miana GA, Riaz M, Shahzad-ul-Hussan S, Paracha RZ, Paracha UZ. Prostratin: an overview. Mini-Rev Med Chem. 2015;15:1122–30.
Kong Y, Gao X, Wang C, Ning C, Liu K, Liu Z, et al. Protective effects of yangonin from an edible botanical kava against lithocholic acid-induced cholestasis and hepatotoxicity. Eur J Pharmacol. 2018;824:64–71.
Buchman CD, Chai SC, Chen T. A current structural perspective on PXR and CAR in drug metabolism. Expert Opin Drug Metab Toxicol. 2018;14:635–47.
Jeong D-H, Jang JJ, Lee SJ, Lee JH, Lim IK, Lee MJ, et al. Expression patterns of cell cycle-related proteins in a rat cirrhotic model induced by CCl4 or thioacetamide. J Gastroenterol. 2001;36:24–32.
Fan X, Chen P, Tan H, Zeng H, Jiang Y, Wang Y, et al. Dynamic and coordinated regulation of KEAP1-NRF2-ARE and p53/p21 signaling pathways is associated with acetaminophen injury responsive liver regeneration. Drug Metab Dispos. 2014;42:1532–9.
Fan X, Jiang Y, Wang Y, Tan H, Zeng H, Wang Y, et al. Wuzhi Tablet (Schisandra Sphenanthera extract) protects against acetaminophen-induced hepatotoxicity by inhibition of CYP-mediated bioactivation and regulation of NRF2-ARE and p53/p21 pathways. Drug Metab Dispos. 2014;42:1982–90.
Dai G, He L, Bu P, Wan YJ. Pregnane X receptor is essential for normal progression of liver regeneration. Hepatology. 2008;47:1277–87.
Acknowledgements
This work was supported by National Natural Science Foundation of China (nos. 82025034, 81973392, 81973195, and 82104020), the Shenzhen Science and Technology Program (no. KQTD20190929174023858), the National Key Research and Development Program (Grant: 2017YFE0109900), the Fundamental Research Funds for the Central Universities (no. 20ykjc04), the Guangdong Provincial Key Laboratory of Construction Foundation (no. 2017B030314030), the China Postdoctoral Science Foundation (no. 2020M683138), the Local Innovative and Research Teams Project of Guangdong Pearl River Talents Program (no. 2017BT01Y093), the 111 project (no. B16047), the Key Laboratory Foundation of Guangdong Province (no. 2017B030314030), the Local Innovative and Research Teams Project of Guangdong Pearl River Talents Program (2017BT01Y093).
Author information
Authors and Affiliations
Contributions
DH, YYZ, RMW, SY, and HCB participated in research design. DH, YYZ, RMW, FYY, and XY performed experiments. DH, YYZ, RMW, WL, XLY, GHT, SY, and HCB wrote or revised the paper.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Supplementary information
Rights and permissions
About this article
Cite this article
Huang, D., Zhao, Yy., Wang, Rm. et al. Natural product-based screening led to the discovery of a novel PXR agonist with anti-cholestasis activity. Acta Pharmacol Sin 43, 2139–2146 (2022). https://doi.org/10.1038/s41401-021-00793-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41401-021-00793-3
Keywords
This article is cited by
-
Bile acid-mediated signaling in cholestatic liver diseases
Cell & Bioscience (2023)