Abstract
Adolescence is among the most vulnerable period for the emergence of serious mental illnesses. Addressing this vulnerability has generated interest in identifying markers of risk for symptoms and opportunities for early intervention. Physical fitness has been linked to psychopathology and may be a useful risk marker and target for early intervention. New wearable technology has made assessing fitness behavior more practical while avoiding recall and self-report bias. Still, questions remain regarding the clinical utility of physical fitness metrics for mental health, both transdiagnostically and along specific symptom dimensions. The current study includes 5007 adolescents (ages 10–13) who participated in the Adolescent Brain Cognitive Development (ABCD) study and additional sub-study that collected fitness data from wearable technology and clinical symptom measures. Physical fitness metrics included resting heart rate (RHR- an index of cardiovascular health), time spent sedentary (associated with increased inflammation and cardiovascular disease), and time spent in moderate physical activity (associated with increased neurogenesis, neuroplasticity, and healthy neurodevelopment). Self-report clinical symptoms included measures of psychosis-like experiences (PLE), internalizing symptoms, and externalizing symptoms. Increased RHR- lower cardiovascular fitness- related only to greater internalizing symptoms (t = 3.63). More sedentary behavior related to elevated PLE severity (t = 5.49). More moderate activity related to lower PLE (t = −2.69) and internalizing (t = −6.29) symptom severity. Wearable technology fitness metrics linked physical health to specific mental health dimensions, which emphasizes the utility of detailed digital health data as a marker for risk and the need for precision in targeting physical health behaviors to benefit symptoms of psychopathology.
Similar content being viewed by others
Introduction
Adolescence is a critical window in which symptoms of psychopathology tend to emerge [1,2,3,4]. This period is also a critical developmental window defined by marked changes in metabolic, hormonal, neural, and social health, which have a major impact on physical and mental health [1, 5]. These features make adolescence an ideal period for interventions that may promote physical and mental health. Addressing health behaviors may be an important treatment target as sedentary behavior is increasing and physical activity is decreasing among adolescents both due to an increasingly digital world and in the aftermath of the global pandemic [6]. Although reviews of physical activity in adolescence demonstrate a benefit to metabolic, neural, and mental health outcomes, these findings depend on recall and self-report data [1,2,3,4] that may be distorted by symptoms of psychopathology [7,8,9]. The recent expansion of wearable technology [10, 11] has improved the practicality of indexing actual health behaviors of individuals [1, 12,13,14,15]. Cardiovascular fitness measures, such as resting heart rate, previously required in-lab assessment but can now reliably be assessed with wearable technology [10, 11]. Additionally, few existing studies include more than one mental health symptom dimension. As a result, it is unclear whether fitness behaviors protect against emerging psychopathology generally or are associated with specific symptom dimensions of mental illness (i.e., psychosis-like experiences (PLEs), internalizing, externalizing domains).
Physical health behaviors have been associated with mental health outcomes [2, 16,17,18,19] in parallel studies of psychosis spectrum, internalizing, and externalizing psychopathologies [12,13,14,15, 20,21,22,23]. These parallel studies within a single clinical dimension have found similar associations between symptom severity and physical health. Specifically, lower cardiovascular fitness [2, 7, 24, 25] and more time spent in sedentary behavior [25,26,27,28,29,30] have been associated with increased symptoms of psychosis and internalizing psychopathologies (especially depression and anxiety) separately. Time spent engaged in moderate to intense physical activity has been related to lowered symptoms separately for psychosis [25], internalizing [18], and externalizing [31] psychopathologies both in observational [2, 16,17,18] and intervention [12,13,14,15, 20,21,22,23] studies. Similar observations across parallel clinical literatures may suggest a broad clinical benefit to improving physical activity regardless of symptom dimension [20, 22, 23]. This transdiagnostic benefit would be of great practical utility in early adolescence when symptoms of psychopathology begin to emerge but have not necessarily differentiated individuals into specific diagnostic categories. However, each health metric may have unique contributors to mental health symptoms [32, 33]. Indeed, Stubbs et al. (2017) showed that cardiovascular health, sedentary behaviors, and physical activity (number of steps) have unique contributions to psychosis symptoms through distinct metabolic pathways. This specificity may also provide insights into potential disease mechanisms that may have relevance to the risk for or treatment of disorders.
In studies of adolescence, physical fitness metrics are related to an array of outcomes, e.g., improvement in cognitive performance, increased structural connectivity, increased functional connectivity, decreased reported stress, decreased reported psychological stress [1, 34]. Prior Adolescent Brain Cognitive Development ® (ABCD) studies found that more optimal body mass index or body morphometry related to better health [5, 35, 36], cognitive outcomes [36,37,38], and brain development [5, 37, 38]. Although adolescent work has linked fitness metrics to larger categories of psychopathologies (PLEs, internalizing, externalizing), these symptom dimensions are often examined in parallel [2, 13] and do not account for the symptoms within the same individuals [3, 4]. Indeed, previous ABCD work has examined a smaller baseline subsample of the fitness data (particularly resting heart rate and the number of daily steps), finding that decreased fitness related to increased internalizing symptoms [9]. Questions remain regarding the transdiagnostic or symptom-specific benefit of health behaviors, which is ultimately necessary for targeted intervention and prevention efforts. If physical health relates to mental health transdiagnostically, then fitness could be used broadly as a potential risk marker or treatment target. In contrast, specificity in this relationship would emphasize a need for clinical precision when using physical health as a marker or treatment target for mental health outcomes.
The current paper examines the relationship between real-world physical fitness metrics (resting heart rate, time spent sedentary, time spent engaged in moderate to intense physical activity) recorded over several days for multiple weeks and clinical symptom dimensions in the ABCD Study. These analyses take advantage of a large, diverse national cohort [39] with real-world fitness and fitness behavior metrics from publicly available wearable technology [10, 11]. This sample does not rely on self-reported fitness behaviors or short-term health and behavior lab assessments [9, 11, 37, 38]. Instead, this rich dataset allows us to draw on a wider range of data in the largest characterization of physical health and mental health symptom dimensions [40]. We expect poor cardiovascular fitness (higher resting heart rate) will be associated with poor mental health based on prior self-report and descriptive actigraphy studies [1, 2, 25, 27]. Greater time spent sedentary, we expect to be associated with more PLEs and internalizing symptoms [25,26,27,28,29,30]. Finally, we hypothesize that more time spent in moderate-to-intense physical activity will be associated with better mental health across symptom dimensions [2, 13, 14, 18, 20, 24, 31].
Methods
Participants
The ABCD Study included 21 sites that were geographically distributed across the United States. Participants were recruited through public and private schools with a broad demographic diversity range aimed at youth between ages 9 and 10 at entry [41]. Each site employed a standardized probability sampling aimed to minimize systemic bias to ensure outreach to historically underrepresented groups and to maximally reflect the distribution of the demographic and socioeconomic characteristics of the U.S. population [41, 42]. The current subsample included 5007 individuals who participated in the regular clinical symptom assessment and the optional Fitbit portion of the study acquired during year 2 of data collection. This subsample ranged in age from 10.58 to 13.5 years (M = 11.95, StD = 0.65), was 48.41% female, and included a wide racial and household income of the subsample, Table 1. Body mass index was measures and calculated as a ratio of kilograms to meters squared (M = 20.17 kg/m2, StD = 4.32 kg/m2). Demographic information, i.e., sex assigned at birth, household income, age (in months), was collected at baseline from parents at the baseline visit. Household income was a self-reported category of three ranges (‘<$50,000’, ‘$50,000–$100,00’, ‘>$100,000’). Race and ethnicity are reported for the current subsample and were compared to the whole ABCD Study sample to assess national representativeness (See Table 1 and Supplementary Information). Race and ethnicity were not included because of a lack of theoretical basis for such a comparison in line with current recommendations to reduce the reinforcement of racial bias [43]. Post-hoc analyses were conducted to examine the potential influence of race and ethnicity, which did not impact the magnitude or the directions of the reported effects. Features of the sample were included in the model, including sex assigned at birth (male/female), age (in months), household income (category), and body mass index (kg/m2), due to their known association with cardiovascular health. All research protocols were approved by each respective institutional review board, including obtaining parents’ informed consent and child’s assent.
Prodromal Questionnaire-Brief Child Version (PQ-CB)
PQ-CB is a 21-item self-report questionnaire answered by the participant [44]. Each item is endorsed as present or not and then rated on a distress scale on a 6-point scale (0 indicates not present; 1 indicates no distress; 2–6 indicates present and some level of distress). The symptom severity score is a total of the distress (only items scored 2–6 in terms of distress) for all 21 items; items without a distress score of at least 2 were treated as 0 (not present), consistent with previous scoring and validations [44, 45].
Child Behavioral Checklist (CBCL)
Participants used an automated self-report version of the CBCL [46,47,48]. The CBCL is a 113-item questionnaire that measures aspects of the participants’ behavior across the past six months; each item was rated on a 3-point scale (not true, somewhat, or sometimes true, very or often true). Responses were used to generate ABCD-curated total scores for internalizing (including depression and anxiety subscales) and externalizing symptoms, which have been previously validated [9, 46,47,48]. Only those individuals who responded to every item were included in the analyses. Follow-up analyses included raw symptom scores which did not change the magnitude or direction of the effects from t-score assessments.
Fitness assessments
Fitbit Charge HR2 devices used proprietary algorithms to measure health metrics at a one-second sampling rate for heart rate using photoplethysmography, which has been validated against gold-standard measures of heart rate [9, 49,50,51]. Heart rate metrics were used to calculate resting heart rate, minutes spent in sedentary activity, and minutes spent in moderate to intense activity (a total of minutes spent fairly active and very active). The ABCD Study calculated fitness metrics by week and provided filtering standards for data that met the minimum quality. Curated weekly fitness summaries were acquired for individuals with at least 600 min of continuous data per day for at least four weekdays and at least 1 weekend day for three weeks (M = 874.3, StD = 66.6 per day) consistent with the supplied ABCD Study working group recommendations (fit_ss_meet_abcd_rule) [11]. For all fitness metrics, a grand mean was created across the days of the week, which were then additionally averaged across all the weeks for which data was available. Follow-up analyses included a correction for the average number of daily hours with data (Supplementary Table 2) and a proportion of recorded time spent in sedentary or moderate activity [52] (Supplementary Table 3), which did not change the magnitude or direction of reported findings. Finally, the moderate to intense activity level included a sum of the time spent active and very active based on previous research [52].
Analytical strategy
For each FitBit Metric, separate multilevel models examined the relationship between a single fitness metric (resting heart rate, time spent sedentary, time spent in moderate to intense activity) with all three of the symptom dimensions (psychosis-like experience symptoms severity (PLE), internalizing, externalizing symptoms), accounting for the random effects of familial relatedness, and the fixed effects of sex, age, household income, and body mass index using lme4 [53] in Rv.4.2.1. Composite symptoms relating to fitness were explored for specificity within the symptom domain (e.g., anxiety and depression subdomains for the internalizing composite symptoms). These additional analyses were done only in the cases of significant effects to reduce the overall number of models tested. Follow-up analyses created a natural log transformation of the symptom scores to address the high number of zero symptom scores, which did not alter the interpretation, magnitude, or direction of the reported effects. For replicability and transparency, all analytic code has been provided [51]. Although all effect sizes will be provided, only those effects that pass correction for multiple comparisons for three fitness metrics (Bonferroni correction p = 0.017) will be interpreted. All model parameters were largely independent (intercorrelation of fixed effects r’s <0.10; Variable Inflation Factor <3.48).
Results
Participants
Participants’ demographic descriptions and model parameters are available in Table 1. Representativeness of the sample was assessed by comparing the current analytic sample to the whole ABCD sample for comparisons to the United States and excluded subsample (see Supplementary Table 1) [42, 54]. There were no significant differences in the distribution of sex assigned at birth compared to the whole ABCD study sample, χ2(1) = 0.50141, p = 0.4789. The current sample’s household income did differ from the larger ABCD study sample, χ2(2) = 110.52, p < 2.2e−16. The current study sample includes fewer individuals with a household income of less than $50,000 (OR = 0.74). Finally, the current sample differed in racial makeup from the larger ABCD Study sample, χ2(3) = 215.34, p < 2.2e−16, such that the current sample had a higher proportion of white (OR = 1.36) and multiracial (OR = 1.24) participants and a lower proportion of black participants (OR = 0.63).
Fitness metrics
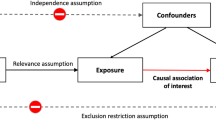
Fitness metrics were predicted by current symptoms (PLEs, internalizing, externalizing) in a multilevel model that accounted for the random effects of individuals and relatedness and the fixed effects of age, sex, household income, and body mass index, Fig. 1A. Full statistics for all model parameters are provided in Table 2.
Psychosis-like experience severity
There was a main effect of current PLE severity on resting heart rate, t(4542) = 2.13, p = 0.033, which did not survive correction for multiple comparisons, Fig. 2A. There was a significant main effect of current PLE severity on time spent sedentary, t(4514) = 5.49, p < 0.001, such that greater current PLE severity related to more time spent sedentary, Fig. 2B. There was a significant main effect of current PLE severity on time spent in moderate to intense physical activity, t(4522) = −2.70, p = 0.007, such that less current PLE severity related to more time spent physically active, Fig. 2C.
A Resting heart rate by PLE severity, B time spent in sendentary activity by PLE severity, C time spent in moderate activity by PLE severity, D resting heart rate by total internalizing severity, E time spent in sendentary activity by total internalizing severity, F time spent in moderate activity by total internalizing severity, G resting heart rate by total externalizing severity, H time spent in sendentary activity by total externalizing severity, I time spent in moderate activity by total externalizing severity. PQ-CB Prodromal Questionnaire-Brief Child Version, CBCL Child Behavioral Checklist.
Internalizing total symptoms
There was a significant main effect of current total internalizing symptoms on resting heart rate, t(4536) = 3.63, p = 0.0002, such that greater current internalizing symptoms were related to elevated resting heart rate (Fig. 2D). There was no significant main effect of current total internalizing symptoms on time spent sedentary, t(4520) = −0.18, p = 0.86; Fig. 2E. There was a significant main effect of current total internalizing symptoms on time spent in moderate physical activity, t(4513) = −6.286, p < 0.001, such that less current total internalizing symptoms were related to more time in moderate physical activity, Fig. 2F.
Externalizing total symptoms
There was no significant main effect of current total externalizing symptoms on resting heart rate, t(4484) = 1.76, p = 0.08, Fig. 2G. There was no significant main effect of current total externalizing symptoms on time spent sedentary, t(4435) = 0.81, p = 0.99, Fig. 2H. There was no significant main effect of current total externalizing symptoms on time spent in moderate activity, t(4448) = 2.159, p = 0.03, Fig. 2I.
Follow-up analyses of anxiety and depression dimensions
Follow-up analyses were conducted for only those fitness metrics that were significantly related to internalizing symptoms (resting heart rate and moderate to intense physical exercise; Bonferroni correction adjusted for two models). Metrics were predicted by current symptoms in a multilevel model that accounted for the random effects of individuals and relatedness and the fixed effects of age, sex, household income, and body mass index. Full statistics for all model parameters are provided in Table 3; effects by symptom dimension are depicted in Fig. 1B.
There was a significant main effect of current total depression symptoms on resting heart rate, t(4445) = 3.073, p = 0.002, such that greater current depression symptoms were related to elevated resting heart rate. There was a significant main effect of current total depression symptoms on the total time spent engaged in moderate to intense physical activity, t(4403) = −4.043, p < 0.001, such that less current depression symptoms were related to more time spent engaged in moderate to intense physical activity. There was no significant main effect of anxiety disorder symptoms on resting heart rate, t(4391) = 1.45, p = 0.15. There was a significant main effect of current total anxiety symptoms on the total time spent engaged in moderate to intense physical activity, t(4337) = −2.392, p = 0.017, such that less current anxiety symptoms were related to more time spent engaged in moderate to intense physical activity.
Discussion
Wearable technology metrics of fitness and fitness behaviors showed unique patterns of relationships to mental health dimensions. This study strengthens the evidence for a clear link between physical and mental health [2, 31, 34, 55]. Despite expectations that physical health would relate to lower overall psychopathology, physical health behaviors showed specificity among mental symptom dimensions. Better cardiovascular health (lower resting heart rate) was related to lower internalizing symptoms, which were driven by depression symptoms and not anxiety. In contrast, increased time spent sedentary had unique relevance to PLE severity but not internalizing or externalizing symptoms. Finally, greater time spent engaged in moderate to intense physical activity was related to lower levels of both PLE severity and internalizing symptoms, but not externalizing symptoms. Features of physical health are related to dimensions of mental health, but clinical precision may be required when using physical health as a marker of risk or target for mental health intervention to match the right target to the right symptoms.
Cardiovascular health (resting heart rate) was related to current internalizing symptoms in adolescence. This finding extends a large, decades-long literature linking depression [2, 16, 49] in three ways: moving findings earlier in development, examining longer real-world assessments of resting heart rate, and accounting for additional symptom dimensions within an individual. Cardiovascular health was related to fewer internalizing symptoms (d = −0.19), which was driven by fewer depression symptoms (d = −0.17) rather than anxiety (d = 0.07). Though this effect size is small, it is similar to previously reported effects (d = −0.166) [4]. Despite previous literature suggesting a general relationship between cardiovascular health and mental health across the psychosis spectrum [7, 24, 25, 27, 56, 57] and internalizing [2,3,4, 18, 21, 22, 58], the current study found that internalizing alone was related when accounting for other symptom dimensions within the model. However, it is noteworthy that PLE severity and internalizing symptom effects were in a similar direction and magnitude to the noted findings, albeit not significant. These findings emphasize the need for future work to examine the relationship between multiple symptom dimensions to explore this specificity.
Increased time spent sedentary was related to greater PLEs severity. This finding is consistent with many studies demonstrating that symptoms across the psychosis spectrum are related to greater time spent sedentary [25, 26, 28, 29, 52]. These findings highlight the potential for time spent sedentary to be explored as a relevant early risk factor for psychosis that shows specificity among other symptom dimensions. Additionally, the specificity of this behavior may merit additional investigations into biological mechanisms related to increased sedentary behaviors (e.g., increased inflammation) [26] as potential mechanisms of emerging PLE severity.
More time spent engaged in moderate physical activity related to reduced PLE severity and internalizing symptoms, but not externalizing symptoms. This finding is consistent with a growing literature suggesting a beneficial impact of physical exercise on attenuated and clinical psychosis symptoms [16, 24]. It was expected that physical activity would generally benefit all mental health dimensions. In contrast, moderate to intense physical activity may only relate to PLE severity and internalizing disorders and may not be associated with externalizing disorders, which highlights the importance of considering symptom dimensions for targeted interventions as well as risk behaviors.
Despite several strengths of this study, but it is also important to note relevant limitations and future directions. First, these individuals are young and relatively healthy, which may limit the range of physical and mental health impacts observed in the current sample [59]. This preclinical range is also a strength, as the current findings are more generalizable to preventative interventions in adolescent populations. This relatively healthy sample may also underestimate the relationship between physical and mental health. Although the reported effects were small (d = 0.08–0.19), they are similar to other risk markers of psychopathology, including paternal diagnoses (d = 0.21) [60], risk genes (d = 0.096–0.17) [61], and irritable temperament (d = 0.16) [60]. Next, prior intervention studies demonstrated that physical activity is an effective intervention for reducing externalizing symptoms [3, 14, 23, 31]. Reductions in externalizing symptoms may be related to the change in dosage of physical activity level, which would not appear from the current observational approach [23, 31]. Further, some previous studies observed that increased physical activity related to increased externalizing psychopathologies [4, 55]. Additionally, it is notable that the current metrics reflect aggregate measures but follow-up analyses suggested that the amount of time did not bias the primary findings (See Supplementary Table 3). Furthermore, the fitbit data available reflects a single time point, a mere snapshot in a very dynamic period. As a result, causality cannot be determined in the current sample. More research is needed to elucidate whether changes in health behavior precede changes in symptoms, making health data a useful risk marker that could potentially be modified by targeted interventions. This lack of longitudinal data also limits the insight into the influence of the dynamic metabolic and sexually dimorphic development that occurs in this time period, see Supplementary figures. Finally, future studies should consider examining the relationship to specific symptoms, e.g., motor slowing [62,63,64], coordination [29], dysphoria [3, 23], that may provide new insight into the types of patients that may benefit most from exercise interventions.
There are several strengths of this study. First, the study accounts for co-occurring dimensions of clinical symptoms within the same individuals. This model approach allows us to directly compare the relationship of health metrics to relevant symptom dimensions while accounting for levels of psychopathology along other dimensions. Second, the study reflects a large cohort that provides confidence in the estimation of the effects, but the generalizability of the findings still depends on the representativeness of the sample demographics [54]. Notably, the current sample was significantly wealthier and did not have a representative racial makeup compared to the larger United States demographics [41, 42]. These differences in income and race should be considered in future research and as a potential bias in the current sample. It is noteworthy, however, that income was included in the current models and follow-up analyses accounting for race and ethnicity did not alter the magnitude or direction of reported effects [42]. Finally, the study was in emerging adolescence, a time when psychopathology typically emerges. As a result, these relationships have strong implications for the relevance of exercise as an early and preventative intervention. Taken together, these findings may suggest that physical activity shows a dimension-specific reduction in symptoms. The current investigation demonstrates this relationship between physical and mental health in a pre-adolescence sample, immediately preceding the emergence of mental illness diagnoses and unmasking vulnerability. It is also notable that this early adolescent population has experienced fewer of the impacts that mental health issues have on physical health, e.g., impact of medication and neurotoxic effects of mental health episodes [59]. Similarly, individuals experiencing mental health issues also may have their fitness activities impacted by changes in mental health. As a result, this study strengthens the evidence for a clear link between physical and mental health [2, 31, 34, 55]. That this relation becomes apparent during this pre-adolescence period has possibly sizable implications for earlier intervention and prevention efforts [17, 65]. Finally, these results are somewhat surprising as a growing body of evidence has targeted health behaviors to improve mental health diagnoses in parallel. However, the specificity of particular digital health metrics to particular symptoms highlights an opportunity to tailor these interventions to address the specific symptoms and needs of an individual.
Data availability
All data are available for download through the National Data Archive supported by the National Institutes of Mental Health for anyone with an approved data use agreement. Authors have also provided a full analytic code that would allow anyone to replicate the analyses presented.
References
Belcher BR, Zink J, Azad A, Campbell CE, Chakravartti SP, Herting MM. The roles of physical activity, exercise, and fitness in promoting resilience during adolescence: effects on mental well-being and brain development. Biol Psychiatry Cogn Neurosci Neuroimaging. 2021;6:225–37.
Biddle SJH, Asare M. Physical activity and mental health in children and adolescents: a review of reviews. Br J Sports Med. 2011;45:886–95.
Wu X, Bastian K, Ohinmaa A, Veugelers P. Influence of physical activity, sedentary behavior, and diet quality in childhood on the incidence of internalizing and externalizing disorders during adolescence: a population-based cohort study. Ann Epidemiol. 2018;28:86–94.
He J-P, Paksarian D, Merikangas KR. Physical activity and mental disorder among adolescents in the United States. J Adolesc Health. 2018;63:628–35.
Brooks SJ, Parks SM, Stamoulis C. Widespread positive direct and indirect effects of regular physical activity on the developing functional connectome in early adolescence. Cereb Cortex. 2021;31:4840–52.
Xiang M-Q, Tan X-M, Sun J, Yang H-Y, Zhao X-P, Liu L, et al. Relationship of physical activity with anxiety and depression symptoms in Chinese college students during the COVID-19 outbreak. Front Psychol. 2020;11:582436.
Damme KSF, Sloan RP, Bartels MN, Ozsan A, Ospina LH, Kimhy D, et al. Psychosis risk individuals show poor fitness and discrepancies with objective and subjective measures. Sci Rep. 2021;11:9851.
Andorko ND, Rakhshan-Rouhakhtar P, Hinkle C, Mittal VA, McAllister M, DeVylder J, et al. Assessing validity of retrospective recall of physical activity in individuals with psychosis-like experiences. Psychiatry Res. 2019;273:211–7.
Nelson BW, Flannery JE, Flournoy J, Duell N, Prinstein MJ, Telzer E. Concurrent and prospective associations between fitbit wearable-derived RDoC arousal and regulatory constructs and adolescent internalizing symptoms. J Child Psychol Psychiatry. 2022;63:282–95.
Godino, Wing JG, Zambotti D, de M, Baker FC, Bagot K, et al. Performance of a commercial multi-sensor wearable (Fitbit Charge HR) in measuring physical activity and sleep in healthy children. PLoS ONE. 2020;15:e0237719.
Bagot KS, Matthews SA, Mason M, Squeglia LM, Fowler J, Gray K, et al. Current, future and potential use of mobile and wearable technologies and social media data in the ABCD study to increase understanding of contributors to child health. Dev Cogn Neurosci. 2018;32:121–9.
Mittal V, Dean D, Gupta T, Bryan A. Aerobic exercise intervention for clinical high-risk youth improves cognitive and hippocampal abnormalities. Schizophr Bull. 2017;43:S168.
Oertel-Knöchel V, Mehler P, Thiel C, Steinbrecher K, Malchow B, Tesky V, et al. Effects of aerobic exercise on cognitive performance and individual psychopathology in depressive and schizophrenia patients. Eur Arch Psychiatry Clin Neurosci. 2014;264:589–604.
Verret C, Guay M-C, Berthiaume C, Gardiner P, Béliveau L. A physical activity program improves behavior and cognitive functions in children With ADHD: an exploratory study. J Atten Disord. 2012;16:71–80.
Ospina LH, Wall M, Jarskog LF, Ballon JS, McEvoy J, Bartels MN, et al. Improving cognition via exercise (ICE): study protocol for a multi-site, parallel-group, single-blind, randomized clinical trial examining the efficacy of aerobic exercise to improve neurocognition, daily functioning, and biomarkers of cognitive change in individuals with schizophrenia. J Psychiatr Brain Sci. 2019;4:e190020 https://doi.org/10.20900/jpbs.20190020
Mittal VA, Vargas T, Juston Osborne K, Dean D, Gupta T, Ristanovic I, et al. Exercise treatments for psychosis: a review. Curr Treat Options Psych. 2017;4:152–66.
Thompson E, Millman ZB, Okuzawa N, Mittal V, DeVylder J, Skadberg T, et al. Evidence-based early interventions for individuals at clinical high risk for psychosis: a review of treatment components. J Nerv Ment Dis. 2015;203:342–51.
Morres ID, Hatzigeorgiadis A, Stathi A, Comoutos N, Arpin-Cribbie C, Krommidas C, et al. Aerobic exercise for adult patients with major depressive disorder in mental health services: a systematic review and meta-analysis. Depression Anxiety. 2019;36:39–53.
Walther S, Vladimirova I, Alexaki D, Schäppi L, Damme KSF, Mittal VA, et al. Low physical activity is associated with two hypokinetic motor abnormalities in psychosis. J Psychiatr Res. 2022;146:258–63.
Damme KS, Gupta T, Ristanovic I, Kimhy D, Bryan AD, Mittal VA. Exercise intervention in individuals at clinical high risk for psychosis: benefits to fitness, symptoms, hippocampal volumes, and functional connectivity. Schizophr Bull. 2022;48:1394–405.
Dean DJ, Bryan AD, Newberry R, Gupta T, Carol E, Mittal VA. A supervised exercise intervention for youth at risk for psychosis: an open-label pilot study. J Clin Psychiatry. 2017;78:e1167–e1173.
Jerstad SJ, Boutelle KN, Ness KK, Stice E. Prospective reciprocal relations between physical activity and depression in female adolescents. J Consult Clin Psychol. 2010;78:268–72.
Gawrilow C, Stadler G, Langguth N, Naumann A, Boeck A. Physical activity, affect, and cognition in children with symptoms of ADHD. J Atten Disord. 2016;20:151–62.
Carney R, Cotter J, Bradshaw T, Firth J, Yung AR. Cardiometabolic risk factors in young people at ultra-high risk for psychosis: a systematic review and meta-analysis. Schizophr Res. 2016;170:290–300.
Vancampfort D, De Hert M, Myin-Germeys I, van Winkel R, Firth J, Van Damme T, et al. Lower cardiorespiratory fitness is associated with more time spent sedentary in first episode psychosis: a pilot study. Psychiatry Res. 2017;253:13–17.
Stubbs B, Gardner-Sood P, Smith S, Ismail K, Greenwood K, Farmer R, et al. Sedentary behaviour is associated with elevated C-reactive protein levels in people with psychosis. Schizophr Res. 2015;168:461–4.
Bueno-Antequera J, Oviedo-Caro MÁ, Munguía-Izquierdo D. Sedentary behaviour, physical activity, cardiorespiratory fitness and cardiometabolic risk in psychosis: the PsychiActive project. Schizophr Res. 2018;195:142–8.
Stubbs B, Williams J, Gaughran F, Craig T. How sedentary are people with psychosis? A systematic review and meta-analysis. Schizophr Res. 2016;171:103–9.
Mittal VA, Bernard JA, Strauss GP, Walther S. New insights into sedentary behavior highlight the need to revisit the way we see motor symptoms in psychosis. Schizophr Bull. 2021;47:877–9.
Choi KW, Stein MB, Nishimi KM, Ge T, Coleman JRI, Chen C-Y, et al. An exposure-wide and mendelian randomization approach to identifying modifiable factors for the prevention of depression. Am J Psychiatry. 2020;177:944–54.
Hoza B, Martin CP, Pirog A, Shoulberg EK. Using physical activity to manage ADHD symptoms:the state of the evidence. Curr Psychiatry Rep. 2016;18:113.
Stubbs B, Chen L-J, Chung M-S, Ku P-W. Physical activity ameliorates the association between sedentary behavior and cardiometabolic risk among inpatients with schizophrenia: a comparison versus controls using accelerometry. Compr Psychiatry. 2017;74:144–50.
Kluge A, Kirschner M, Hager OM, Bischof M, Habermeyer B, Seifritz E, et al. Combining actigraphy, ecological momentary assessment and neuroimaging to study apathy in patients with schizophrenia. Schizophr Res. 2018;195:176–82.
White RL, Babic MJ, Parker PD, Lubans DR, Astell-Burt T, Lonsdale C. Domain-specific physical activity and mental health: a meta-analysis. Am J Prev Med. 2017;52:653–66.
Ronan L, Alexander-Bloch A, Fletcher PC. Childhood obesity, cortical structure, and executive function in healthy children. Cereb Cortex. 2020;30:2519–28.
Rapuano KM, Rosenberg MD, Maza MT, Dennis NJ, Dorji M, Greene AS, et al. Behavioral and brain signatures of substance use vulnerability in childhood. Dev Cogn Neurosci. 2020;46:100878.
Green R. Health behaviors and the adolescent brain: predicting cognition from physical activity and diet in children enrolled in the ABCD® Study. UVM Honors College Senior Theses. 2022. https://scholarworks.uvm.edu/hcoltheses/467.
Hall PA, Best JR, Beaton EA, Sakib MN, Danckert J. Morphology of the prefrontal cortex predicts body composition in early adolescence: cognitive mediators and environmental moderators in the ABCD Study. Soc Cogn Affect Neurosci. 2023;18:nsab104.
Casey BJ, Cannonier T, Conley MI, Cohen AO, Barch DM, Heitzeg MM, et al. The adolescent brain cognitive development (ABCD) study: imaging acquisition across 21 sites. Dev Cogn Neurosci. 2018;32:43–54.
Funkhouser CJ, Chacko AA, Correa KA, Kaiser AJE, Shankman SA. Unique longitudinal relationships between symptoms of psychopathology in youth: A cross-lagged panel network analysis in the ABCD study. J Child Psychol Psychiatry. 2020. https://doi.org/10.1111/jcpp.13256.
Garavan H, Bartsch H, Conway K, Decastro A, Goldstein RZ, Heeringa S, et al. Recruiting the ABCD sample: design considerations and procedures. Dev Cogn Neurosci. 2018;32:16–22.
Heeringa SG, Berglund PA. A guide for population-based analysis of the adolescent brain cognitive development (ABCD) study baseline data. 2020. https://doi.org/10.1101/2020.02.10.942011.
Cardenas-Iniguez C, Gonzalez MR “We controlled for race and ethnicity…” Recommendations for the responsible use and communication of race and ethnicity in neuroimaging research. 2023. https://doi.org/10.31234/osf.io/xs8t3.
Karcher NR, Barch DM. The ABCD study: understanding the development of risk for mental and physical health outcomes. Neuropsychopharmacology. 2021;46:131–42.
Loewy RL, Pearson R, Vinogradov S, Bearden CE, Cannon TD. Psychosis risk screening with the Prodromal Questionnaire-brief version (PQ-B). Schizophr Res. 2011;129:42–46.
Thompson WK, Barch DM, Bjork JM, Gonzalez R, Nagel BJ, Nixon SJ, et al. The structure of cognition in 9 and 10 year-old children and associations with problem behaviors: findings from the ABCD study’s baseline neurocognitive battery. Dev Cogn Neurosci. 2019;36:100606.
Steinberger D, Barch D. The effect of perceived discrimination on mental health and cognitive functioning. Modern Psychol Stud. 2021;27. https://scholar.utc.edu/mps/vol27/iss1/3.
Farahdel B, Thapaliya B, Suresh P, Ray B, Calhoun VD, Liu J. Confirmatory factor analysis on mental health status using ABCD cohort. In: 2021 IEEE International Conference on Bioinformatics and Biomedicine (BIBM); Houston, TX, USA, 2021. p. 3540–7. https://doi.org/10.1109/BIBM52615.2021.9669378.
Wang R, Blackburn G, Desai M, Phelan D, Gillinov L, Houghtaling P, et al. Accuracy of wrist-worn heart rate monitors. JAMA Cardiol. 2017;2:104–6.
Nelson BW, Low CA, Jacobson N, Areán P, Torous J, Allen NB. Guidelines for wrist-worn consumer wearable assessment of heart rate in biobehavioral research. npj Digit Med. 2020;3:1–9.
Nelson BW, Allen NB. Accuracy of Consumer Wearable Heart Rate Measurement During an Ecologically Valid 24-Hour Period: Intraindividual Validation Study. JMIR mHealth uHealth. 2019;7:e10828.
Mittal VA, Gupta T, Orr JM, Pelletier-Baldelli A, Dean DJ, Lunsford-Avery JR, et al. Physical activity level and medial temporal health in youth at ultra high-risk for psychosis. J Abnorm Psychol. 2013;122:1101–10.
Bates D, Mächler M, Bolker B, Walker S. Fitting linear mixed-effects models using lme4. J Stat Softw. 2015;64:1–48.
Alliende LM, Vargas T, Mittal VA. Representation challenges in large clinical datasets. Schizophr Bull. 2023;49:1414–7.
Moore MJ, Werch CE. Sport and physical activity participation and substance use among adolescents. J Adolesc Health. 2005;36:486–93.
Scheewe TW, Takken T, Kahn RS, Cahn W, Backx FJG. Effects of exercise therapy on cardiorespiratory fitness in patients with schizophrenia. Med Sci Sports Exerc. 2012;44:1834–42.
Scheewe TW, van Haren NEM, Sarkisyan G, Schnack HG, Brouwer RM, de Glint M, et al. Exercise therapy, cardiorespiratory fitness and their effect on brain volumes: a randomised controlled trial in patients with schizophrenia and healthy controls. Eur Neuropsychopharmacol. 2013;23:675–85.
Isaksson J, Selinus EN, Åslund C, Nilsson KW. Physical activity in early adolescence predicts depressive symptoms 3 years later: a community-based study. J Affect Disord. 2020;277:825–30.
Mittal VA, Wakschlag LS. Research domain criteria (RDoC) grows up: strengthening neurodevelopmental investigation within the RDoC framework. J Affect Disord. 2017;216:30–35.
Pagliaccio D, Alqueza KL, Marsh R, Auerbach RP. Brain volume abnormalities in youth at high risk for depression: adolescent brain and cognitive development study. J Am Acad Child Adolesc Psychiatry. 2020;59:1178–88.
Flint J, Kendler KS. The genetics of major depression. Neuron. 2014;81:484–503.
Damme KSF, Osborne KJ, Gold JM, Mittal VA. Detecting motor slowing in clinical high risk for psychosis in a computerized finger tapping model. Eur Arch Psychiatry Clin Neurosci. 2020;270:393–7.
Damme KSF, Park JS, Walther S, Vargas T, Shankman SA, Mittal VA. Depression and psychosis risk shared vulnerability for motor signs across development, symptom dimensions, and familial risk. Schizophr Bull. 2022;48:752–62.
Damme KSF, Park JS, Vargas T, Walther S, Shankman SA, Mittal VA. Motor abnormalities, depression risk, and clinical course in adolescence. Biol Psychiatry Glob Open Sci. 2022;2:61–9.
Addington J, Carstensen G, Piskulic D, Raedler T, Addington D. Identification and treatment of youth with attenuated psychosis syndromes: a Canadian perspective. In: Li H, Shapiro DI, Seidman LJ, editors. Handbook of attenuated psychosis syndrome across cultures: international perspectives on early identification and intervention. Cham: Springer International Publishing, 2019. p. 187–97.
Acknowledgements
This work was supported by the National Institutes of Mental Health (Grant R01MH103231, R01MH112545, R01MH094650, R21/R33MH103231; T32MH126368).
Author information
Authors and Affiliations
Contributions
Katherine S.F. Damme – conceptualization, data curation, formal analyses, analytic software, methodology, visualization, writing-original draft, writing-review & editing; Teresa G. Vargas – project administration (data use agreement), writing-review & editing; Sebastian Walther - writing-review & editing; Stewart Shankman - writing-review & editing; Vijay A Mittal – conceptualization, funding acquisition, writing-review & editing
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Damme, K.S.F., Vargas, T.G., Walther, S. et al. Physical and mental health in adolescence: novel insights from a transdiagnostic examination of FitBit data in the ABCD study. Transl Psychiatry 14, 75 (2024). https://doi.org/10.1038/s41398-024-02794-2
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-024-02794-2