Abstract
The persistent difficulty in conceptualizing the relationship between addictive and other mental disorders stands out among the many challenges faced by the field of Psychiatry. The different philosophies and schools of thought about, and the sheer complexity of these highly prevalent clinical conditions make progress inherently difficult, not to mention the profusion of competing and sometimes contradictory terms that unnecessarily exacerbate the challenge. The lack of a standardized term adds confusion, fuels stigma, and contributes to a “wrong door syndrome” that captures the difficulty of not only diagnosing but also treating addictive and other mental disorders in an integrated manner. The World Association on Dual Disorders (WADD) proposes the adoption of the term “Dual Disorder” which, while still arbitrary, would help harmonize various clinical and research efforts by rallying around a single, more accurate, and less stigmatizing designation.
Similar content being viewed by others
Introduction
The advancement of a scientific mission relies on precise communication, and consistent messaging, including standard nomenclatures, plays a key role in that regard. Language has the power to shape people’s thoughts and beliefs: it can inspire, rally, and unite individuals toward common and positive goals, but it can also contribute to the emergence of wrong assumptions and stigmatizing stereotypes. The words we choose to describe the manifestation of an addictive disorder in association with other mental disorders offer good examples of the potentially detrimental aspects of language. Certain terms can have a significant impact on, among others, whether affected individuals will seek help or the quality of the treatment they receive. Here, we propose the term “Dual Disorder” (DD) as an apt descriptor of this clinical entity and provide the reasoning behind our recommendation of its adoption as standard nomenclature. We believe this will facilitate public and professional discourse in the field and help reduce the stigma and discrimination around psychiatric illnesses in general and addictive disorders [substance use disorders (SUD) and behavioral addictions] in particular.
A brief history of dual disorders
Multiple epidemiological studies have established that DDs are an expectation rather than an exception: a substantial fraction of patients suffering from a mental disorder at some point in their lives will also experience an addictive disorder, and vice versa [1, 2], which depending on various demographic factors and specific disorder dyads, can range from around 40–60% [3,4,5]. For the uninitiated, dual disorders are to be expected when it comes to treating people with various mental disorders, a prevalence that increases as the severity of mental disorders increases. More than 75% of severe psychiatric disorders occur with other mental disorders, such as SUD and other addictions [6].
If we take the perspective of those who seek addiction treatment, although the data are quite variable, close to 70% of them will present another mental disorder [7]. These data most likely reflect an underestimate, to the extent that only diagnostic categories and not symptomatic dimensions were used in the assessment. This kind of information is significantly underrecognized among mental health experts, whether they work within a mental health or addiction care network.
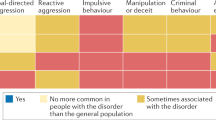
The accumulated evidence suggests that dual disorders reflect etiological overlaps, common contributing factors, and bidirectional relationships between paired conditions [8, 9]. For example, according to the National Epidemiological Survey on Alcohol and Related Conditions (NESARC) study, 96% of patients suffering from pathological gambling disorder have other mental disorders, depression being one of the most frequent [10]. Importantly, 87% of these patients display high impulsivity [11], probably a key marker prevalent among those suffering from depression. Thus, depression could be a specific phenotype that occurs with some measures of impulsivity [12, 13]. Similarly, there is robust evidence to suggest that maladaptive emotion regulation (ER) is central to the development and maintenance of a broad range of psychopathologies, including SUD [14]. The mediating role of dysfunctional ER in the bidirectional relationships between SUD and suicidality [15], offers another good example of the usefulness of transdiagnostic constructs.
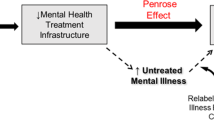
Importantly, dual disorders are frequently under-reported [16] and under-treated [17], partly due to the persistent challenges in understanding and classifying them [18, 19]. Their high prevalence, combined with huge diagnostic and treatment gaps, results in a significant burden for patients, their relatives, and society at large [20]. One of the most deleterious consequences of these systemic inadequacies is the so-called “wrong door syndrome”, characteristic of a persistently siloed healthcare landscape, that affects patients with dual disorders who are not sure where to find the right treatment [21]. Adoption of a DD-based nomenclature could increase clinicians’ awareness of the close and, at the same time, transdiagnostic relationships between the signs and symptoms of addictive and other mental disorders and help them address their etiologies and clinical manifestations in a more integrated and effective way [22].
The lack of consensus on standard terminology has resulted in the proliferation of competing labels, contributing to increasing societal stigma and self-stigma for affected individuals. For starters, the World Health Organization (WHO) usually refers to “dual diagnosis” when a SUD presents together with another psychiatric disorder in the same person, but it also encompasses any two psychiatric or even any two SUD [23], thus the term is nonspecific by definition. This may help explain why this organization has begun to use the term dual disorder, at least in one of its more recent reports [22]. Meanwhile, the European Monitoring Centre for Drugs and Drug Addiction (EMCDDA) has used the terms “comorbidity” [24] and “dual diagnosis” [25] interchangeably to describe the temporal coexistence of two or more psychiatric disorders, as defined by the International Classification of Diseases (ICD), when one of them is problematic substance use [26]. The American Association of Addiction Medicine (ASAM)’s criteria for patient placement also uses dual diagnosis, although interchangeably with yet another term: “co-occurring disorder” (COD) [27], which seems to also be the preferred term for the Substance Abuse and Mental Health Services Administration (SAMSHA) in the US [28]. Meanwhile, in the Spanish, French, Portuguese, and Italian languages, the most widespread and accepted term is “dual pathology” [29]. But there is more: we can find other particularly troubling (i.e., stigmatizing) terms in some older articles [30] or nonscientific literature [31] that refer to a population of patients with addictive disorders and other mental illnesses as “mentally ill chemical abusers” (MICA)(or its reverse: “chemically addicted mentally ill”). For reasons that will be explained in the next section, the WADD prefers the term “Dual Disorder” (DD), which has been introduced progressively, at least since the early 90 s [32], and already enjoys substantial support in that both, the UN Commission on Narcotic Drugs (UNCND) [22] and the World Psychiatric Association (WPA) has among its different scientific sections one on “dual disorders”, while an influential US treatment guideline has also been recommending its use for the past two decades [33].
While the existing lack of consensus about the proper nomenclature hinders both research and clinical efforts, it is just the tip of the iceberg: Underneath this cacophony of terms lie many different and often conflicting schools of thought about the nature of this complex and neglected condition. The reality is that DD have been ignored or even denied for years and that in many settings, the disorder is poorly understood or overlooked altogether.
Using science to chart a path forward
Our field has long been saddled with a lack of clarity on whether DD represent distinct entities or alternative clinical manifestations of a single core, underlying pathophysiological process. The reality is that many patients present with a heterogeneous collection of addictive and other mental disorders, and these symptoms and their severity can change over time [34].
There is broad scientific consensus that all mental disorders, including addiction, are disorders of the brain. This consensus, while not monolithic (some authors opt for a more nuanced approach, although still neurobiological in nature when it comes to SUD [35]), is rather robust and based on multiple lines of evidence [36, 37]. Yet, despite such broad agreement, references to addictive and other psychiatric disorders as separate entities are still common, as if the former were fundamentally different from the latter. If addictions are mental disorders, it behooves us to refer to “addictive and other mental disorders”, a turn of phrase in which the order is important because it denotes that an addiction (whether drug-related or behavioral) is also a mental disorder and, therefore, a brain disorder.
Moreover, it would be difficult to argue that addictive, and other mental disorders are two completely different types of mental disorders, for this would require the highly unlikely assumption that the high degree of co-prevalence between them is the result of random factors or measurement artifacts. In fact, the NESARC study has demonstrated, for example, that purely substance-induced mood disorders (SIMD) accounted for a very small percentage of mood disorders among all those with SUD [38]. Similar patterns of comorbidity and risk factors in individuals with SIMD and those with mood depressive disorder suggest that the two conditions likely share underlying etiological factors [39]. The emerging consensus is that addictive and other mental disorders are strongly linked, albeit via complex and not necessarily direct relationships. Indeed, a range of factors is likely to contribute to the particularly strong linkage between a lifetime diagnosis of addictive and other mental disorders, with specific early-life events and factors identified as contributing more strongly to the emergence of dual compared to single disorders [40, 41]. Progress in the neurosciences is providing new perspectives from which to identify the underlying mechanisms involved in the onset and development of addictive disorders. In the case of SUD, they have spurred better pathophysiological theories [42, 43] with the power to improve our understanding of their multi-level interactions with other psychiatric disorders. Similar lines of thinking are also being applied to other addictive disorders, such as gambling or compulsive sexual behavior [44, 45].
From molecules to environment
Neuroscience has shown that addictive and other mental disorders often display sets of interconnected and/or overlapping brain processes, rather than being disorders primarily defined by a single behavior (such as uncontrollable excessive drug use) [46]. These connections operate at multiple phenomenological levels, but the clearest examples may be the neurotransmitter systems that show deficits in various psychiatric conditions and that are also the direct targets of addictive drugs. To state the obvious, all psychoactive substances with addiction liability have a counterpart or connection with one or more endogenous systems, such as the dopaminergic, opioidergic, endocannabinoid, or cholinergic-nicotinic systems [47, 48]. Therefore, an inherited or acquired impairment in any of these neurotransmitter systems and circuits could help explain common underlying risks of suffering both addictive behaviors and other psychiatric symptoms, including pathological personality traits or disorders [29, 49]. Recent advances in our understanding of such interindividual differences reinforce the need to incorporate the drug-of-choice model [50]. This model considers that people may be more susceptible to a certain drug or class of drugs (or to compulsive video game use, for example), based on individual differences, and different mental disorders or symptoms, including endophenotypes, such as personality traits. It is well known that the administration of psychoactive substances do not have the same effects among different individuals [51, 52]. One of the clearest examples is that stimulants calm down people with Attention-Deficit/Hyperactivity Disorder (ADHD), but not others, by correcting imbalances in dopamine and norepinephrine levels [53]. This differential effect on different people/brains can be transferred to all psychoactive substances such as nicotine, alcohol, cannabis, cocaine, and opioids, as evinced by a growing scientific literature.
At the next level of analysis, research in genetics and precision psychiatry has uncovered significant evidence that some DD dyads (e.g., cannabis/attention deficit [54], tobacco use disorder/schizophrenia [55], alcoholism/depression [56], gambling/ADHD [57,58,59], drug use/schizophrenia [60]; smoking/suicide attempts [61], cocaine/ADHD [62], seem to show at least some common genetic bases. Such sharing of genetic underpinnings presents a towering challenge to the rigid compartmentalizing diagnostic boundaries that separate addictive from other psychiatric disorders, one with far-reaching implications for translational research and therapeutic outcomes [63].
In addition, and similar to addictive disorders, the prevalence and severity of a DD is also linked to the early onset of the disorder [29, 64], befitting the model of developmental disorders that often begin during late childhood and adolescence and may present with different phenotypes, whether addiction-related or other personality traits, such as disorganized attachment [65], impulsiveness [66], etc. Our growing understanding of the many ways in which environmental factors, such as trauma and early-life stress [67, 68] or sleep deficits [69, 70], can perturb brain development and function and increase the risk of addictive and/or other mental disorders, offers additional compelling arguments towards an improved explanation of the complex pathophysiology of DDs [71].
The combined analysis at the genetic, neurophysiological, and developmental levels, is bringing the bidirectional nature of these relationships into sharper focus. It is clear that the chronic use of any psychoactive (including addictive) substances can jeopardize various aspects of brain activity, like blood flow, neurotransmitter activity, structure, and functional connectivity, in ways that could either trigger or exacerbate the symptoms of a mental illness [9]. Additionally, it is hardly surprising to discover that unmet mental healthcare needs are closely linked to the consumption of psychoactive substances that can lead to a SUD [51, 72]. This is consistent with the self-medication hypothesis, as revisited from a neurobiological perspective [73]. And at the behavioral level, overlaid atop mechanistic arguments, is the fact that rigid or inflexible emotional responses and atypical patterns of thinking and behaving are central to many, if not all, of the emotion-related disorders, including depression, anxiety, stress, eating, substance, and some personality disorders [74].
When combined, these data points offer new insights into the many ways in which brain function can be perturbed and help explain the high prevalence of DD. Advances in this area could usher in new approaches to enable healthcare professionals to offer more adequate personalized assessments and evidence-based treatments for people with DD. Importantly, it is worth emphasizing that the benefits of adopting a standard term would extend not only to addictive disorders involving psychoactive substances but to any behavioral addiction, such as gambling disorder [75], internet gaming disorder [76], or social network site addiction [77, 78], as they move through the various stages of the clinical recognition process [79]. Behavioral addictive processes, not involving psychoactive substances, are also likely to share multiple neurobiological and genetic links with some substance use and, by extension, other psychiatric disorders. For example, brain imaging studies are consistent with the notion that both pathological gambling (DSM-5 TR) and gaming disorder (ICD-11), which are the only behavioral addictions included in internationally recognized classifications, display deficits in neuronal pathways implicated in behavioral control, which, similar to the case of SUD, display enhanced impulsivity as an underlying vulnerability [80]. On the other hand, the similarities (and differences) between SUD and other (non-substance) addictive behaviors that are under consideration for future designation as behavioral addictions, are also beginning to shed some light on the potential overlaps. One key example is a reduced ability to delay gratification, long observed in SUD, that appears to be associated with some forms of obesity [81] as well as with social media addiction [82]. Finally, the genetic, individual, and environmental factors that increase vulnerability for developing some SUD are also similar to those promoting behavioral addictions not involving substances [83, 84] and, of course, other mental disorders.
The nomenclature dilemma
One of the obstacles in the pursuit of a more rational, neuroscience-based classification of DD (as well as other complex mental disorders more broadly) stems from the fact that DSM-based instruments are not well suited to address complex phenomena, for they use diagnostic categories (rather than symptom dimensions) that may not always reach the diagnostic criteria threshold. It is evident that, despite the advantages of having a categorical diagnostic system based on the observation of psychopathological phenomena, just as Kraepelin did in the early days of psychiatry, ca. 1915 [85], the lack of sensitivity and reliability makes it difficult to capture the broad spectrum of mental symptom manifestations and the relationships between them [86]. This helps explain why the DSM and ICD have systematically and consistently overlooked DD across successive revisions.
This lack of categorization clarity has provided fertile grounds for the proliferation of competing terms that aim to capture the same phenomenon. It is worth pointing out that every one of these terms, including DD, is arbitrary and colored by the “realist” tradition that considers constructs such as schizophrenia or SUD as true reflections of mental phenomena. This, in spite of the fact that we can only observe the signs, symptoms, and course of the illnesses we postulate result from these disorders [87]. Thus, it would be highly desirable to explore next-generation “instrumentalist” approaches that consider existing constructs as mere tools to be evaluated on their empirical adequacy [87]. It is evident that in this third decade of the 21st century, an era of breathtaking neuroscientific advances and the dawn of personalized medicine and precision psychiatry, patients and their relatives have a right to expect more than diagnoses based on the phenomenological description of their experiences [50]. Unfortunately, we are not yet in a position to deploy a new classification of mental disorders. While we wait for the many ongoing laudable efforts in this direction [88,89,90,91] to bear fruit, the WADD proposes adopting DD as the preferred standard terminology, a recommendation that is based not only on the listed drawbacks suffered by the competing terms but also on its own merits.
The term “comorbidity”, coined by Fenstein in 1970 to indicate the coexistence of two different and separate diseases [92], has been used in psychiatry when two different diagnostic categories coexist, for example, tobacco use disorder and schizophrenia, with the obvious implication that these two symptomatic expressions remained unrelated. The term “dual diagnosis” operates under a similar rationale since it refers to two categorically different diagnoses. This debate goes back many years when it was proposed that the definition of comorbidity merely specifies an association in time, not necessarily a causal relationship, between conditions [93]. Similarly, the terms “concurrent disorders,” and “co-occurring disorders” imply a purely temporal relationship, which could reflect either a common underlying cause or completely unrelated etiologies [94].
On the other hand, the term DD offers a broad, symptomatic, and dimensional view of the condition that includes different mental disorders or symptoms, including personality traits (endophenotypes), that determine vulnerability or resilience to addictive and other mental disorders [95]. The result is a more consistent heuristic framework for conducting translational research on mental disorders. The dual disorder is also the term that most naturally conveys the need for both broad assessments to identify multiple conditions as well as appropriately integrated interventions that could modify the trajectory of DD by abandoning the simplistic notion that these are brain disorders featuring different psychopathological expressions. The term dual disorders, unlike dual diagnosis or comorbidity, includes not only a unified vision of two diagnostic categories (DSM-5) but also transdiagnostic, syndromic, and symptomatic dimensions, which may be simultaneous or sequential during the life span, and that could be readily incorporated into Research Domain Criteria (RDoC) type projects, allowing us to advance more steadily towards precision psychiatry [96].
Somewhat paradoxically, a DD-based framework would also be consistent with DSM and ICD polythetic criteria whereby specific mental disorders are defined by multiple symptoms, not all of which need to be present or currently active (e.g., in a “preaddiction” stage [86] or when a SUD is in early or sustained remission) to consider a mental disorder present in a specific individual [97]. Thus, the term DD is compatible with DSM/ICD operational definitions whereby DD represent not only the temporary coexistence of different disorders but also the sequential events that manifest themselves at different points along the life span and the course of a person’s mental illness.
Finally, as suggested throughout this perspective, an equally important benefit of the term is that it could help alleviate the stigma and discrimination that adds to the suffering of patients with a dual disorder: The main competing terms (i.e., dual diagnosis, and comorbid or co-occurring conditions), imply two different diagnostic entities (hence, separate conditions) that are individually rooted in DSM categorizations and merely happen to occur in one person. We believe the proposed harmonization opens up the possibility of going beyond the diagnostic categories of the DSM, one of whose problems is not considering dual disorders, and thus include dimensions of mental symptoms and dysfunctional personality traits that could enable a more accurate diagnosis and clinical management. The concept “Dual Disorder” (one complex condition) shifts the focus to the individual patient, promoting a more personalized approach because it evokes the complex nature of seemingly unrelated manifestations contributing to one condition and making it possible to treat the person and not just an addictive or other mental disorders.
Conclusion
It is evident that consensus-building efforts are needed to facilitate the adoption of a common term to define the clinical reality of dual disorders. Here, we call for the adoption of “Dual Disorder” as the standard term in research work and clinical practice. We believe that this would constitute an important step forward not only to improve the education of health professionals but also to achieve better integration of mental health and addiction services when treating a single person suffering from different manifestations of mental disorders. Also, this new perspective must reach patients, their families, and society in general, suffering from disorders that have been stigmatized, misunderstood, discriminated against, and mishandled for too long, and making it possible for them to find “the right door” leading to effective recovery.
References
Lev-Ran S, Imtiaz S, Rehm J, Le Foll B. Exploring the association between lifetime prevalence of mental illness and transition from substance use to substance use disorders: results from the National Epidemiologic Survey of Alcohol and Related Conditions (NESARC). Am J Addict. 2013;22:93–8.
Martinez-Raga J, Knecht C, de Alvaro R, Szerman N, Ruiz P. Addressing dual diagnosis patients suffering from attention deficit hyperactivity disorders and comorbid substance use disorders: a review of treatment considerations. Addict Dis Treat. 2013;12:213–30.
Hasin DS, Grant BF. The National Epidemiologic Survey on Alcohol and Related Conditions (NESARC) Waves 1 and 2: review and summary of findings. Soc Psychiatry Psychiatr Epidemiol. 2015;50:1609–40.
Kessler RC, Chiu WT, Demler O, Merikangas KR, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617–27.
Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54:313–21.
Alsuhaibani R, Smith DC, Lowrie R, Aljhani S, Paudyal V. Scope, quality and inclusivity of international clinical guidelines on mental health and substance abuse in relation to dual diagnosis, social and community outcomes: a systematic review. BMC Psychiatry. 2021;21:209.
Arias F, Szerman N, Vega P, Mesias B, Basurte I, Morant C, et al. Madrid study on the prevalence and characteristics of outpatients with dual pathology in community mental health and substance misuse services. Adicciones. 2013;25:118–27.
Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates, and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: results from the national epidemiologic survey on alcohol and related conditions. J Clin Psychiatry. 2005;66:677–85.
Volkow ND. Drug abuse and mental illness: progress in understanding comorbidity. Am J Psychiatry. 2001;158:1181–3.
Cowlishaw S, Hakes JK. Pathological and problem gambling in substance use treatment: results from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). Am J Addict. 2015;24:467–74.
Grant JE, Levine L, Kim D, Potenza MN. Impulse control disorders in adult psychiatric inpatients. Am J Psychiatry. 2005;162:2184–8.
Corruble E, Benyamina A, Bayle F, Falissard B, Hardy P. Understanding impulsivity in severe depression? A psychometrical contribution. Prog Neuro Psychopharmacol Biol Psychiatry. 2003;27:829–33.
Swann AC, Steinberg JL, Lijffijt M, Moeller FG. Impulsivity: differential relationship to depression and mania in bipolar disorder. J Affect Disord. 2008;106:241–8.
Sloan E, Hall K, Moulding R, Bryce S, Mildred H, Staiger PK. Emotion regulation as a transdiagnostic treatment construct across anxiety, depression, substance, eating and borderline personality disorders: a systematic review. Clin Psychol Rev. 2017;57:141–63.
Riquino MR, Priddy SE, Howard MO, Garland EL. Emotion dysregulation as a transdiagnostic mechanism of opioid misuse and suicidality among chronic pain patients. Borderline Personal Disord Emot Dysregul. 2018;5:11.
Bahorik AL, Newhill CE, Queen CC, Eack SM. Under-reporting of drug use among individuals with schizophrenia: prevalence and predictors. Psychol Med. 2014;44:61–69.
Ross S, Peselow E. Co-occurring psychotic and addictive disorders: neurobiology and diagnosis. Clin Neuropharmacol. 2012;35:235–43.
Samet S, Nunes EV, Hasin D. Diagnosing comorbidity: concepts, criteria, and methods. Acta Neuropsychiatr. 2004;16:9–18.
Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction 2006;101:76–88.
Peris L, Szerman N. Partial agonists and dual disorders: focus on dual schizophrenia. Front Psychiatry. 2021;12:769623.
Szerman N, Martínez-Raga J, Baler R, Roncero C, Vega P, Basurte-Villamor I, et al. Joint statement on dual disorders: Addiction and other mental disorders. Salud Ment. 2017;40:245–7.
Volkow ND, Torrens M, Poznyak V, Saenz E, Busse A, Kashino W, et al. Managing dual disorders: a statement by the Informal Scientific Network, UN Commission on Narcotic Drugs. World Psychiatry. 2020;19:396–7.
Pillard P, Revke D, Fleischmann A, Krupchanka D, Carragher N, Roache S, et al. Lexicon of Alcohol and Drug Terms. Geneva: World Health Organization; 1994.
EMCDDA. Comorbidity of substance use and mental health disorders in Europe (Perspectives on drugs). Lisbon: The European Monitoring Centre for Drugs and Drug Addiction; 2016.
Torrens M, Mestre-Pinto JI, Montanari L, Vicente J, Domingo-Salvany A. Dual diagnosis: an European perspective. Adicciones 2017;29:3–5.
WHO: The ICD-10 Classification of Mental and Behavioural Disorders. Clinical descriptions and diagnostic guidelines World Health Organization; 2019.
Stallvik M, Nordahl HM. Convergent validity of the ASAM criteria in co-occurring disorders. J Dual Diagn. 2014;10:68–78.
SAMHSA. Co-Occurring Disorders and Other Health Conditions. Rockville: Substance Abuse and Mental Health Services Administration; 2021.
Szerman N, Martinez-Raga J, Peris L, Roncero C, Basurte I, Vega P, et al. Rethinking dual disorders/pathology. Addict Disord Their Treat. 2013;12:1–4.
Carey KB. Treatment of the mentally ill chemical abuser: description of the Hutchings Day Treatment Program. Psychiatr Q. 1989;60:303–16.
Portage. Freedom from addiction. Montreal: Portage Addiction Treatment Centers; 2014.
Decker KP, Ries RK. Differential diagnosis and psychopharmacology of dual disorders. Psychiatr Clin North Am. 1993;16:703–18.
Kim T, Mueser D, Noordsy L, Drake R, Fox L. Integrated Treatment for Dual Disorders. In: ed. Barlow. DHA guide to effective practice. New York: The Guilford Press; 2003.
Luo SX, Levin FR. Towards precision addiction treatment: new findings in co-morbid substance use and attention-deficit hyperactivity disorders. Curr Psychiatry Rep. 2017;19:14.
Snoek A, Matthews S. Introduction: testing and refining Marc Lewis’s Critique of the brain disease model of addiction. Neuroethics 2017;10:1–6.
Cuthbert BN. Research Domain Criteria: toward future psychiatric nosologies. Dialogues Clin Neurosci. 2015;17:89–97.
Volkow ND, Boyle M. Neuroscience of addiction: relevance to prevention and treatment. Am J Psychiatry. 2018;175:729–40.
Grant BF, Stinson FS, Dawson DA, Chou SP, Ruan WJ, Pickering RP. Co-occurrence of 12-month alcohol and drug use disorders and personality disorders in the United States: results from the National Epidemiologic Survey on Alcohol and Related Conditions. Arch Gen Psychiatry. 2004;61:361–8.
Blanco C, Alegria AA, Liu SM, Secades-Villa R, Sugaya L, Davies C, et al. Differences among major depressive disorder with and without co-occurring substance use disorders and substance-induced depressive disorder: results from the National Epidemiologic Survey on Alcohol and Related Conditions. J Clin Psychiatry. 2012;73:865–73.
Salom CL, Betts KS, Williams GM, Najman JM, Alati R. Predictors of comorbid polysubstance use and mental health disorders in young adults-a latent class analysis. Addiction 2016;111:156–64.
Salom CL, Williams GM, Najman JM, Alati R. Familial factors associated with development of alcohol and mental health comorbidity. Addiction 2015;110:248–57.
Badiani A, Belin D, Epstein D, Calu D, Shaham Y. Opiate versus psychostimulant addiction: the differences do matter. Nat Rev Neurosci. 2011;12:685–700.
Ceceli AO, Bradberry CW, Goldstein RZ. The neurobiology of drug addiction: cross-species insights into the dysfunction and recovery of the prefrontal cortex. Neuropsychopharmacology 2022;47:276–91.
Antons S, Brand M, Potenza MN. Neurobiology of cue-reactivity, craving, and inhibitory control in non-substance addictive behaviors. J Neurol Sci. 2020;415:116952.
Brand M, Wegmann E, Stark R, Muller A, Wolfling K, Robbins TW, et al. The Interaction of Person-Affect-Cognition-Execution (I-PACE) model for addictive behaviors: Update, generalization to addictive behaviors beyond internet-use disorders, and specification of the process character of addictive behaviors. Neurosci Biobehav Rev. 2019;104:1–10.
Volkow ND. Personalizing the treatment of substance use disorders. Am J Psychiatry. 2020;177:113–6.
Tomkins DM, Sellers EM. Addiction and the brain: the role of neurotransmitters in the cause and treatment of drug dependence. Can Med Assoc J. 2001;164:817–21.
Volkow ND, Michaelides M, Baler R. The neuroscience of drug reward and addiction. Physiol Rev. 2019;99:2115–40.
Szerman N, Peris L. Personality Disorders and Addiction Disorders. In: el-Guebaly N, Carrà, G, Galanter, M Milano. Textbook of Addiction Treatment: International Perspectives. Springer-Verlag: 2015. pp. 2063–83.
Szerman N, Peris L. Precision psychiatry and dual disorders. J Dual Diagn. 2018;14:237–46.
Ward HB, Beermann A, Nawaz U, Halko MA, Janes AC, Moran LV, et al. Evidence for schizophrenia-specific pathophysiology of nicotine dependence. Front Psychiatry 2022;13:804055.
Wardle MC, Marcus BA, de Wit H. A preliminary investigation of individual differences in subjective responses to D-amphetamine, alcohol, and delta-9-tetrahydrocannabinol using a within-subjects randomized trial. PLoS ONE. 2015;10:e0140501.
Faraone SV. The pharmacology of amphetamine and methylphenidate: Relevance to the neurobiology of attention-deficit/hyperactivity disorder and other psychiatric comorbidities. Neurosci Biobehav Rev. 2018;87:255–70.
Soler Artigas M, Sanchez-Mora C, Rovira P, Richarte V, Garcia-Martinez I, Pagerols M, et al. Attention-deficit/hyperactivity disorder and lifetime cannabis use: genetic overlap and causality. Mol Psychiatry. 2020;25:2493–503.
Scott JG, Matuschka L, Niemela S, Miettunen J, Emmerson B, Mustonen A. Evidence of a causal relationship between smoking tobacco and schizophrenia spectrum disorders. Front Psychiatry. 2018;9:607.
McHugh RK, Weiss RD. Alcohol use disorder and depressive disorders. Alcohol Res. 2019;40:e1–8.
Luderer M, Ramos Quiroga JA, Faraone SV, Zhang James Y, Reif A. Alcohol use disorders and ADHD. Neurosci Biobehav Rev. 2021;128:648–60.
Vilar-Ribo L, Sanchez-Mora C, Rovira P, Richarte V, Corrales M, Fadeuilhe C, et al. Genetic overlap and causality between substance use disorder and attention-deficit and hyperactivity disorder. Am J Med Genet Part B Neuropsychiatr Genet. 2021;186:140–50.
Waluk OR, Youssef GJ, Dowling NA. The relationship between problem gambling and attention deficit hyperactivity disorder. J Gambl Stud. 2016;32:591–604.
Mallard TT, Harden KP, Fromme K. Genetic risk for schizophrenia is associated with substance use in emerging adulthood: an event-level polygenic prediction model. Psychol Med. 2019;49:2027–35.
Mullins N, Kang J, Campos AI, Coleman JRI, Edwards AC, Galfalvy H, et al. Dissecting the shared genetic architecture of suicide attempt, psychiatric disorders, and known risk factors. Biol Psychiatry 2022;91:313–27.
Manni C, Cipollone G, Pallucchini A, Maremmani AGI, Perugi G, Maremmani I. Remarkable reduction of cocaine use in dual disorder (adult attention deficit hyperactive disorder/cocaine use disorder) patients treated with medications for ADHD. Int J Environ Res Public Health. 2019;16:3911.
Polimanti R, Agrawal A, Gelernter J. Schizophrenia and substance use comorbidity: a genome-wide perspective. Genome Med. 2017;9:25.
Hildebrand Karlen M, Nilsson T, Wallinius M, Billstedt E, Hofvander B. A bad start: the combined effects of early onset substance use and ADHD and CD on criminality patterns, substance abuse and psychiatric comorbidity among young violent offenders. J Pers Oriented Res. 2020;6:39–54.
Ramirez-Castillo D, Garcia-Roda C, Guell F, Fernandez-Montalvo J, Bernacer J, Moron I. Frustration tolerance and personality traits in patients with substance use disorders. Front Psychiatry. 2019;10:421.
Torales J, Castaldelli-Maia JM, da Silva AG, Campos MW, Gonzalez-Urbieta I, Barrios I. Even more complex…. when mental disorder meets addiction in youth: dual pathology. Curr Drug Res Rev. 2019;11:40–43.
Tschetter KE, Callahan LB, Flynn SA, Rahman S, Beresford TP, Ronan PJ. Early life stress and susceptibility to addiction in adolescence. Int Rev Neurobiol. 2022;161:277–302.
Roberto M, Spierling SR, Kirson D, Zorrilla EP. Corticotropin-releasing factor (CRF) and addictive behaviors. Int Rev Neurobiol. 2017;136:5–51.
Yang FN, Liu TT, Wang Z. Functional connectome mediates the association between sleep disturbance and mental health in preadolescence: a longitudinal mediation study. Hum Brain Mapp. 2022;43:2041–50.
Greenwald MK, Moses TEH, Roehrs TA. At the intersection of sleep deficiency and opioid use: mechanisms and therapeutic opportunities. Transl Res. 2021;234:58–73.
Brady KT, Sinha R. Co-occurring mental and substance use disorders: the neurobiological effects of chronic stress. Am J Psychiatry. 2005;162:1483–93.
Harris KM, Edlund MJ. Self-medication of mental health problems: new evidence from a national survey. Health Serv Res. 2005;40:117–34.
Khantzian EJ. The self-medication hypothesis of substance use disorders: a reconsideration and recent applications. Harv Rev Psychiatry. 1997;4:231–44.
Coifman KG, Summers CB. Understanding emotion inflexibility in risk for affective disease: integrating current research and finding a path forward. Front Psychol. 2019;10:392.
Rash CJ, Petry NM. Gambling disorder in the DSM-5: opportunities to improve diagnosis and treatment especially in substance use and homeless populations. Curr Addict Rep. 2016;3:249–53.
Przybylski AK, Weinstein N, Murayama K. Internet gaming disorder: investigating the clinical relevance of a new phenomenon. Am J Psychiatry. 2017;174:230–6.
Andreassen CS, Torsheim T, Brunborg GS, Pallesen S. Development of a facebook addiction scale. Psychol Rep. 2012;110:501–17.
Brailovskaia J, Margraf J, Teismann T. Repetitive negative thinking mediates the relationship between addictive Facebook use and suicide-related outcomes: a longitudinal study. Curr Psychol. 2021;1–9.
Potenza MN. Non-substance addictive behaviors in the context of DSM-5. Addict Behav. 2014;39:1–2.
Potenza MN. Review. The neurobiology of pathological gambling and drug addiction: an overview and new findings. Philos Trans R Soc Lond Ser B Biol Sci. 2008;363:3181–9.
Volkow ND, Baler RD. Now vs Later brain circuits: implications for obesity and addiction. Trends Neurosci. 2015;38:345–52.
Turel O, He Q, Brevers D, Bechara A. Delay discounting mediates the association between posterior insular cortex volume and social media addiction symptoms. Cogn Affect Behav Neurosci. 2018;18:694–704.
Nower L, Blaszczynski A, Anthony WL. Clarifying gambling subtypes: the revised pathways model of problem gambling. Addiction 2021;117:2000–8.
Verdejo-Garcia A, Clark L, Verdejo-Roman J, Albein-Urios N, Martinez-Gonzalez JM, Gutierrez B, et al. Neural substrates of cognitive flexibility in cocaine and gambling addictions. Br J Psychiatry. 2015;207:158–64.
Hoff P. The Kraepelinian tradition. Dialogues Clin Neurosci. 2015;17:31–41.
McLellan AT, Koob GF, Volkow ND. Preaddiction—a missing concept for treating substance use disorders. JAMA Psychiatry. 2022;79:749–51.
Kendler KS. Potential lessons for DSM from contemporary philosophy of science. JAMA Psychiatry. 2022;79:99–100.
Arseneault L. Taxonomy of psychopathology: a work in progress and a call for interdisciplinary research. World Psychiatry. 2021;20:73–74.
Dalgleish T, Black M, Johnston D, Bevan A. Transdiagnostic approaches to mental health problems: Current status and future directions. J Consulting Clin Psychol. 2020;88:179–95.
Hirjak D, Schwarz E, Meyer-Lindenberg A. Twelve years of research domain criteria in psychiatric research and practice: claim and reality. Der Nervenarzt. 2021;92:857–67.
Kotov R, Krueger RF, Watson D, Cicero DC, Conway CC, DeYoung CG, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a quantitative nosology based on consensus of evidence. Annu Rev Clin Psychol. 2021;17:83–108.
Feinstein AR. The pre-therapeutic classification of co-morbidity in chronic disease. J Chronic Dis. 1970;23:455–68.
Kaplan B, Crawford S, Cantell M, Kooistra L, Dewey D. Comorbidity, co-occurrence, continuum: What’s in a name? Child Care Health Dev. 2006;32:723–31.
Morisano D, Babor TF, Robaina KA. Co-occurrence of substance use disorders with other psychiatric disorders: Implications for treatment services. Nord Stud Alcohol Drugs. 2014;31:1.
Belcher AM, Volkow ND, Moeller FG, Ferre S. Personality traits and vulnerability or resilience to substance use disorders. Trends Cogn Sci. 2014;18:211–7.
NIMH. Research Domain Criteria (RDoC). Bethesda, MD 20892-9663, National Institute of Mental Health; Office of Science Policy, Planning, and Communications. National Institutes of Health; 2022.
Krueger RF, Bezdjian S. Enhancing research and treatment of mental disorders with dimensional concepts: toward DSM-V and ICD-11. World Psychiatry. 2009;8:3–6.
Author information
Authors and Affiliations
Consortia
Contributions
NS and RB drafted the original manuscript. MT, RF, YPSB, CS, IM, LS, JDA, and JC made substantial contributions to the original conception of the work, then revised, edited, and supplemented the first draft with their own comments and suggestions. The authors constitute the World Association on Dual Disorders’ Executive Committee, which has unanimously endorsed the recommendation made in this article.
Corresponding author
Ethics declarations
Competing interests
NS: has received honoraria/expenses from Lundbeck, Janssen, Takeda and Otsuka and fee for Consulting/ Advisory Board from Neuroxpharm. MT: has received honoraria or consultation fees for:Gilead, MSD, Camurus, Servier, Angellini, Lundbeck, Otzuka, and fee for participation in a company sponsored speaker’s bureau of Camurus, Servier, Angellini, Lundbeck, Otzuka. The remaining authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szerman, N., Torrens, M., Maldonado, R. et al. Addictive and other mental disorders: a call for a standardized definition of dual disorders. Transl Psychiatry 12, 446 (2022). https://doi.org/10.1038/s41398-022-02212-5
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-02212-5