Abstract
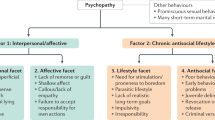
Disinhibited behaviours such as aggression, criminality and substance misuse are ubiquitous. In the USA, a violent crime occurs every 25 s, a non-violent crime every 4.1 s, an incidence of domestic violence every 3 s and substance misuse every 2.4 s. These behaviours are widespread, but more commonly exhibited by individuals with specific psychological problems, namely disorders characterized by disinhibition. Although individuals with disinhibitory disorders display similar behaviours, the underlying cognitive–affective factors are distinct and must be taken into account when developing scientifically informed interventions. In this Review, we provide a summary of key cognitive–affective factors associated with four disinhibitory disorders: substance use disorders, borderline personality disorder, antisocial personality disorder and psychopathy. We focus on these four disorders given their phenotypic overlap and because individuals with these disorders disproportionately find themselves ensnared in the legal system. We discuss the implications of integrating an understanding of cognitive–affective functioning for more successful interactions between individuals with these disorders and the police, courts and correctional facilities. To protect all members of society, we must consider how psychological science can have a greater role at various stages of legal intervention.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 digital issues and online access to articles
$59.00 per year
only $4.92 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Substance Abuse and Mental Health Services Administration. Key Substance Use and Mental Health Indicators in the United States: Results from the 2019 National Survey on Drug Use and Health (Center for Behavioral Health Statistics and Quality, Substance Abuse and Mental Health Services Administration, 2020).
Federal Bureau of Investigation. Crime in the U.S. 2019 https://ucr.fbi.gov/crime-in-the-u.s/2019/crime-in-the-u.s.-2019 (2019).
Leyro, T. M., Zvolensky, M. J. & Bernstein, A. Distress tolerance and psychopathological symptoms and disorders: a review of the empirical literature among adults. Psychol. Bull. 136, 576–600 (2010).
Tarter, R. E. et al. Neurobehavioral disinhibition in childhood predicts early age at onset of substance use disorder. Am. J. Psychiatry 160, 1078–1085 (2003).
Bergstrøm, H. & Farrington, D. P. “The beat of my heart”: the relationship between resting heart rate and psychopathy in a prospective longitudinal study. J. Crim. Psychol. 8, 333–344 (2018).
Gard, A. M. et al. The long reach of early adversity: parenting, stress, and neural pathways to antisocial behavior in adulthood. Biol. Psychiatry: Cognit. Neurosci. Neuroimaging 2, 582–590 (2017).
Brennan, G. M., Hyde, L. W. & Baskin-Sommers, A. R. Antisocial pathways associated with substance use disorders: characterizing etiological underpinnings and implications for treatment. Curr. Opin. Behav. Sci. 13, 124–129 (2017).
Brennan, G. M., Stuppy-Sullivan, A. M., Brazil, I. A. & Baskin-Sommers, A. R. Differentiating patterns of substance misuse by subtypes of antisocial traits in male offenders. J. Forens. Psychiatry Psychol. 28, 341–356 (2017).
Estrada, S., Tillem, S. M., Stuppy-Sullivan, A. & Baskin-Sommers, A. in Oxford Handbook of Positive Emotion and Psychopathology (ed. Gruber, J.) 312–332 (Oxford Univ. Press, 2019).
Baskin-Sommers, A., Curtin, J. J. & Newman, J. P. Altering the cognitive-affective dysfunctions of psychopathic and externalizing offender subtypes with cognitive remediation. Clin. Psychol. Sci. 3, 45–57 (2015).
Fazel, S., Yoon, I. A. & Hayes, A. J. Substance use disorders in prisoners: an updated systematic review and meta-regression analysis in recently incarcerated men and women. Addiction 112, 1725–1739 (2017).
De Brito, S. A. et al. Psychopathy. Nat. Rev. Dis. Primers 7, 49 (2021).
Widiger, T. A. & Gore, W. L. in Encyclopedia of Mental Health 2nd edn (ed. Friedman, H. S.) 270–277 (Academic, 2016).
Krueger, R. F. et al. Validity and utility of Hierarchical Taxonomy of Psychopathology (HiTOP): II. Externalizing superspectrum. World Psychiatry 20, 171–193 (2021).
Hodgins, S. Aggressive behavior among persons with schizophrenia and those who are developing schizophrenia: attempting to understand the limited evidence on causality. Schizophr. Bull. 43, 1021–1026 (2017).
Gorenstein, E. E. & Newman, J. P. Disinhibitory psychopathology: a new perspective and a model for research. Psychol. Rev. 87, 301–315 (1980).
Iacono, W. G., Malone, S. M. & McGue, M. Behavioral disinhibition and the development of early-onset addiction: common and specific influences. Annu. Rev. Clin. Psychol. 4, 325–348 (2008).
Carragher, N. et al. ADHD and the externalizing spectrum: direct comparison of categorical, continuous, and hybrid models of liability in a nationally representative sample. Soc. Psychiatry Psychiatr. Epidemiol. 49, 1307–1317 (2014).
Young, S. & Cocallis, K. M. Attention deficit hyperactivity disorder (ADHD) in the prison system. Curr. Psychiatry Rep. 21, 41 (2019).
Mohr-Jensen, C. & Steinhausen, H.-C. A meta-analysis and systematic review of the risks associated with childhood attention-deficit hyperactivity disorder on long-term outcome of arrests, convictions, and incarcerations. Clin. Psychol. Rev. 48, 32–42 (2016).
Frick, P. J. & Nigg, J. T. Current issues in the diagnosis of attention deficit hyperactivity disorder, oppositional defiant disorder, and conduct disorder. Annu. Rev. Clin. Psychol. 8, 77–107 (2012).
Barker, E. D. et al. The neurocognition of conduct disorder behaviors: specificity to physical aggression and theft after controlling for ADHD symptoms. Aggressive Behav. 37, 63–72 (2011).
Philipp-Wiegmann, F. et al. ADHD modulates the course of delinquency: a 15-year follow-up study of young incarcerated man. Eur. Arch. Psychiatry Clin. Neurosci. 268, 391–399 (2018).
Patrick, C. J., Fowles, D. C. & Krueger, R. F. Triarchic conceptualization of psychopathy: developmental origins of disinhibition, boldness, and meanness. Dev. Psychopathol. 21, 913–938 (2009).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders (DSM-5) (American Psychiatric Publishing, 2013).
Bach, B. & First, M. B. Application of the ICD-11 classification of personality disorders. BMC Psychiatry 18, 1–14 (2018).
Kotov, R. et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): a dimensional alternative to traditional nosologies. J. Abnorm. Psychol. 126, 454–477 (2017).
Krueger, R. F., Markon, K. E., Patrick, C. J., Benning, S. D. & Kramer, M. D. Linking antisocial behavior, substance use, and personality: an integrative quantitative model of the adult externalizing spectrum. J. Abnorm. Psychol. 116, 645–666 (2007).
Mullins-Sweatt, S. N., DeShong, H. L., Lengel, G. J., Helle, A. C. & Krueger, R. F. Disinhibition as a unifying construct in understanding how personality dispositions undergird psychopathology. J. Res. Pers. 80, 55–61 (2019).
Jones, A. & Sawyer, W. Arrest, Release, Repeat: How Police and Jails are Misused to Respond to Social Problems (National Institute of Corrections, 2019).
Bronson, J., Stroop, J., Zimmer, S. & Berzofsky, M. Drug Use, Dependence, and Abuse Among State Prisoners and Jail Inmates, 2007–2009 (US Department of Justice, 2020).
Krueger, R. F. et al. Etiologic connections among substance dependence, antisocial behavior and personality: modeling the externalizing spectrum. J. Abnorm. Psychol. 111, 411–424 (2002).
Robins, L. N. The intimate connection between antisocial personality and substance abuse. Soc. Psychiatry Psychiatr. Epidemiol. 33, 393–399 (1998).
Trull, T. J. et al. Borderline personality disorder and substance use disorders: an updated review. Borderline Personal. Disord. Emot. Dysregul. 5, 15 (2018).
Gunderson, J. G., Herpertz, S. C., Skodol, A. E., Torgersen, S. & Zanarini, M. C. Borderline personality disorder. Nat. Rev. Dis. Prim. 4, 18029 (2018).
Conn, C. et al. Borderline personality disorder among jail inmates: how common and how distinct? Correct. Compend. 35, 6–13 (2010).
Moore, K. E., Tull, M. T. & Gratz, K. L. Borderline personality disorder symptoms and criminal justice system involvement: the roles of emotion-driven difficulties controlling impulsive behaviors and physical aggression. Compr. Psychiatry 76, 26–35 (2017).
Howard, R., Hasin, D. & Stohl, M. Substance use disorders and criminal justice contact among those with co-occurring antisocial and borderline personality disorders: findings from a nationally representative sample. Personal. Ment. Health 15, 40–48 (2021).
Howard, R. C. Co-occuring antisocial and borderline personality disorders: a single syndrome? Ann. Psychiatry Ment. Health 5, 1120 (2017).
Volkert, J., Gablonski, T.-C. & Rabung, S. Prevalence of personality disorders in the general adult population in Western countries: systematic review and meta-analysis. Br. J. Psychiatry 213, 709–715 (2018).
Fazel, S. & Danesh, J. Serious mental disorder in 23 000 prisoners: a systematic review of 62 surveys. Lancet 359, 545–550 (2002).
Mueser, K. T. et al. Conduct disorder and antisocial personality disorder in persons with severe psychiatric and substance use disorders. Schizophr. Bull. 32, 626–636 (2006).
Krasnova, A., Eaton, W. W. & Samuels, J. F. Antisocial personality and risks of cause-specific mortality: results from the Epidemiologic Catchment Area study with 27 years of follow-up. Soc. Psychiatry Psychiatr. Epidemiol. 54, 617–625 (2019).
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders Vol. 3 (American Psychiatric Association, 1980).
Lykken, D. T. in Handbook of Psychopathy 3–13 (Guilford Press, 2006).
Crego, C. & Widiger, T. A. Psychopathy and the DSM. J. Personal. 83, 665–677 (2015).
Hare, R. D. Psychopathy: a clinical construct whose time has come. Crim. Justice Behav. 23, 25–54 (1996).
Werner, K. B., Few, L. R. & Bucholz, K. K. Epidemiology, comorbidity, and behavioral genetics of antisocial personality disorder and psychopathy. Psychiatr. Ann. 45, 195–199 (2015).
Sanz-García, A., Gesteira, C., Sanz, J. & García-Vera, M. P. Prevalence of psychopathy in the general adult population: a systematic review and meta-analysis. Front. Psychol. 12, 3278 (2021).
Driessen, J. M. et al. A comparison of latent profiles in antisocial male offenders. J. Crim. Justice 57, 47–55 (2018).
Kiehl, K. A. & Hoffman, M. B. The criminal psychopath: history, neuroscience, treatment, and economics. Jurimetrics 51, 355–397 (2011).
Baskin-Sommers, A. R. & Hearon, B. A. in The Handbook of Drugs and Society Ch. 11 (ed. Brownstein, H. H.) 218–235 (Wiley, 2015).
Belsky, D. W. et al. Etiological features of borderline personality related characteristics in a birth cohort of 12-year-old children. Dev. Psychopathol. 24, 251–265 (2012).
Patrick, C. J. in The Psychopath: Theory, Research, and Social Implications (eds Herve, H. & Yuille, J. C.) 207–252 (Erlbaum, 2007).
Cuthbert, B. N. The RDoC framework: facilitating transition from ICD/DSM to dimensional approaches that integrate neuroscience and psychopathology. World Psychiatry 13, 28–35 (2014).
Lewis, M., Haviland-Jones, J. M. & Barrett, L. F. Handbook of Emotions (Guilford Press, 2010).
Gazzaniga, M. S. Handbook of Cognitive Neuroscience (Springer, 2014).
Mason, W. A., Hitch, J. E. & Spoth, R. L. Longitudinal relations among negative affect, substance use, and peer deviance during the transition from middle to late adolescence. Substance Use Misuse 44, 1142–1159 (2009).
DeLisi, M. & Vaughn, M. G. Foundation for a temperament-based theory of antisocial behavior and criminal justice system involvement. J. Crim. Justice 42, 10–25 (2014).
McHugh, R. K. & Goodman, F. R. Are substance use disorders emotional disorders? Why heterogeneity matters for treatment. Clin. Psychol. 26, e12286 (2019).
McHugh, R. K. & Kneeland, E. T. Affective vulnerability in substance use disorders. Curr. Opin. Psychol. 30, 54–58 (2019).
Taylor, J., Carlson, S. R., Iacono, W. G., Lykken, D. T. & McGue, M. Individual differences in electrodermal responsivity to predictable aversive stimuli and substance dependence. Psychophysiology 36, 193–198 (1999).
Verona, E., Patrick, C. J. & Lang, A. R. A direct assessment of the role of state and trait negative emotion in aggressive behavior. J. Abnorm. Psychol. 111, 249–258 (2002).
DeFreitas, K. D. & Hucker, S. J. in Encyclopedia of Forensic and Legal Medicine 2nd edn (eds Payne-James, J. & Byard, R. W.) 574–578 (Elsevier, 2015).
Bertsch, K., Florange, J. & Herpertz, S. C. Understanding brain mechanisms of reactive aggression. Curr. Psychiatry Rep. 22, 1–16 (2020).
Lazareck, S. et al. A longitudinal investigation of the role of self-medication in the development of comorbid mood and drug use disorders: findings from the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC). J. Clin. Psychiatry 73, 588–593 (2012).
Kemp, E., Sadeh, N. & Baskin-Sommers, A. A latent profile analysis of affective triggers for risky and impulsive behavior. Front. Psychol. 9, 2651 (2019).
Gratz, K. L., Rosenthal, M. Z., Tull, M. T., Lejuez, C. & Gunderson, J. G. An experimental investigation of emotion dysregulation in borderline personality disorder. J. Abnorm. Psychol. 115, 850–855 (2006).
Bornovalova, M. A. et al. A multimodal assessment of the relationship between emotion dysregulation and borderline personality disorder among inner-city substance users in residential treatment. J. Psychiatr. Res. 42, 717–726 (2008).
Sargeant, M. N., Daughters, S. B., Curtin, J. J., Schuster, R. & Lejuez, C. W. Unique roles of antisocial personality disorder and psychopathic traits in distress tolerance. J. Abnorm. Psychol. 120, 987–992 (2011).
Daughters, S. B., Sargeant, M. N., Bornovalova, M. A., Gratz, K. L. & Lejuez, C. W. The relationship between distress tolerance and antisocial personality disorder among male inner-city treatment seeking substance users. J. Personal. Disord. 22, 509–524 (2008).
Bornovalova, M. A., Lejuez, C. W., Daughters, S. B., Zachary Rosenthal, M. & Lynch, T. R. Impulsivity as a common process across borderline personality and substance use disorders. Clin. Psychol. Rev. 25, 790–812 (2005).
Bushman, B. J., Baumeister, R. F. & Phillips, C. M. Do people aggress to improve their mood? Catharsis beliefs, affect regulation opportunity, and aggressive responding. J. Personal. Soc. Psychol. 81, 17–32 (2001).
Weinberg, A., Klonsky, E. D. & Hajcak, G. Autonomic impairment in borderline personality disorder: a laboratory investigation. Brain Cogn. 71, 279–286 (2009).
Deckers, J. W. et al. The influence of stress on social cognition in patients with borderline personality disorder. Psychoneuroendocrinology 52, 119–129 (2015).
Drews, E., Fertuck, E. A., Koenig, J., Kaess, M. & Arntz, A. Hypothalamic–pituitary–adrenal axis functioning in borderline personality disorder: a meta-analysis. Neurosci. Biobehav. Rev. 96, 316–334 (2019).
Dixon-Gordon, K. L., Peters, J. R., Fertuck, E. A. & Yen, S. Emotional processes in borderline personality disorder: an update for clinical practice. J. Psychother. Integr. 27, 425–438 (2017).
Sylvers, P., Brennan, P. A., Lilienfeld, S. O. & Alden, S. A. Gender differences in autonomic indicators of antisocial personality disorder features. Personal. Disord. 1, 87–96 (2010).
Anton, M. E., Baskin-Sommers, A., Vitale, J. E., Curtin, J. J. & Newman, J. P. Differential effects of psychopathy and antisocial personality disorder symptoms on cognitive and fear processing in female offenders. Cogn. Affect. Behav. Neurosci. 12, 761–776 (2012).
Patrick, C. J. Physiological correlates of psychopathy, antisocial personality disorder, habitual aggression, and violence. Electrophysiol. Psychophysiol. Psychiatry Psychopharmacol. 21, 197–227 (2014).
Farrington, D. P. Interactions between resting heart rate and childhood risk factors in predicting convictions and antisocial personality scores. Crime. Delinq. 66, 1369–1391 (2020).
Koenig, J., Kemp, A. H., Feeling, N. R., Thayer, J. F. & Kaess, M. Resting state vagal tone in borderline personality disorder: a meta-analysis. Prog. Neuropsychopharmacol. Biol. Psychiatry 64, 18–26 (2016).
Krause-Utz, A., Winter, D., Niedtfeld, I. & Schmahl, C. The latest neuroimaging findings in borderline personality disorder. Curr. Psychiatry Rep. 16, 438 (2014).
Raine, A. A. Personality as a neurodevelopmental disorder. Annu. Rev. Clin. Psychol. 14, 259–289 (2018).
Sinha, R. How does stress increase risk of drug abuse and relapse? Psychopharmacology 158, 343–359 (2001).
Wrase, J. et al. Amygdala volume associated with alcohol abuse relapse and craving. Am. J. Psychiatry 165, 1179–1184 (2008).
Schulze, L., Schulze, A., Renneberg, B., Schmahl, C. & Niedtfeld, I. Neural correlates of affective disturbances: a comparative meta-analysis of negative affect processing in borderline personality disorder, major depressive disorder, and posttraumatic stress disorder. Biol. Psychiatry 4, 220–232 (2019).
Yang, Y. & Raine, A. Prefrontal structural and functional brain imaging findings in antisocial, violent, and psychopathic individuals: a meta-analysis. Psychiatry Res. 174, 81–88 (2009).
Pando-Naude, V. et al. Gray and white matter morphology in substance use disorders: a neuroimaging systematic review and meta-analysis. Transl. Psychiatry 11, 29 (2021).
Kavish, N. et al. On the associations between indicators of resting arousal levels, physiological reactivity, sensation seeking, and psychopathic traits. Personal. Individ. Differ. 141, 218–225 (2019).
Johnson, M. M., Mikolajewski, A., Shirtcliff, E. A., Eckel, L. A. & Taylor, J. The association between affective psychopathic traits, time incarcerated, and cortisol response to psychosocial stress. Hormones Behav. 72, 20–27 (2015).
Lorber, M. F. Psychophysiology of aggression, psychopathy, and conduct problems: a meta-analysis. Psychol. Bull. 130, 531–552 (2004).
Schmitt, W. A. & Newman, J. P. Are all psychopathic individuals low-anxious? J. Abnorm. Psychol. 108, 353–358 (1999).
O’Leary, M. M., Loney, B. R. & Eckel, L. A. Gender differences in the association between psychopathic personality traits and cortisol response to induced stress. Psychoneuroendocrinology 32, 183–191 (2007).
Glenn, A. L. in The Handbook of Neuropsychiatric Biomarkers, Endophenotypes and Genes 59–70 (Springer, 2009).
Hicks, B. M., Markon, K. E., Patrick, C. J., Krueger, R. F. & Newman, J. P. Identifying psychopathy subtypes on the basis of personality structure. Psychol. Assess. 16, 276–288 (2004).
Drislane, L., Vaidyanathan, U. & Patrick, C. Reduced cortical call to arms differentiates psychopathy from antisocial personality disorder. Psychol. Med. 43, 825 (2013).
Meffert, H., Gazzola, V., den Boer, J. A., Bartels, A. A. & Keysers, C. Reduced spontaneous but relatively normal deliberate vicarious representations in psychopathy. Brain 136, 2550–2562 (2013).
Scott, L. N. et al. Borderline personality disorder symptoms and aggression: a within-person process model. J. Abnorm. Psychol. 126, 429–440 (2017).
Mitchell, A. E., Dickens, G. L. & Picchioni, M. M. Facial emotion processing in borderline personality disorder: a systematic review and meta-analysis. Neuropsychol. Rev. 24, 166–184 (2014).
Bertsch, K., Hillmann, K. & Herpertz, S. C. Behavioral and neurobiological correlates of disturbed emotion processing in borderline personality disorder. Psychopathology 51, 76–82 (2018).
Kolla, N. J., Meyer, J. H., Bagby, R. M. & Brijmohan, A. Trait anger, physical aggression, and violent offending in antisocial and borderline personality disorders. J. Forensic Sci. 62, 137–141 (2017).
Hyde, L. W., Byrd, A. L., Votruba-Drzal, E., Hariri, A. R. & Manuck, S. B. Amygdala reactivity and negative emotionality: divergent correlates of antisocial personality and psychopathy traits in a community sample. J. Abnorm. Psychol. 123, 214–224 (2014).
Schneider, F. et al. Functional imaging of conditioned aversive emotional responses in antisocial personality disorder. Neuropsychobiology 42, 192–201 (2000).
Hicks, B. M. & Patrick, C. J. Psychopathy and negative emotionality: analyses of suppressor effects reveal distinct relations with emotional distress, fearfulness, and anger-hostility. J. Abnorm. Psychol. 115, 276–287 (2006).
Steuerwald, B. L. & Kosson, D. S. in The Clinical and Forensic Assessment of Psychopathy: A Practitioner’s Guide 111–135 (Taylor & Francis Group, 2000).
Baskin-Sommers, A., Stuppy-Sullivan, A. & Buckholtz, J. Psychopathic individuals experience, but don’t avoid regret during counterfactual decision-making. Proc. Natl Acad. Sci. USA 113, 14438–14443 (2016).
Hoppenbrouwers, S. S., Bulten, B. H. & Brazil, I. A. Parsing fear: a reassessment of the evidence for fear deficits in psychopathy. Psycholo. Bull. 142, 573–600 (2016).
Wilson, K., Juodis, M. & Porter, S. Fear and loathing in psychopaths: a meta-analytic investigation of the facial affect recognition deficit. Crim. Justice Behav. 38, 659–668 (2011).
Jackson, R. L., Neumann, C. S. & Vitacco, M. J. Impulsivity, anger, and psychopathy: the moderating effect of ethnicity. J. Personal. Disord. 21, 289–304 (2007).
Baskin-Sommers, A. & Newman, J. P. in Psychopathy and Law: A Practitioner’s Guide 79–97 (Wiley, 2012).
Baskin-Sommers, A. & Foti, D. J. Abnormal reward functioning across substance use disorders and major depressive disorder: considering reward as a transdiagnostic mechanism. Int. J. Psychophysiol. 98, 227–239 (2015).
Zeng, J. et al. Neurobiological correlates of cue-reactivity in alcohol-use disorders: a voxel-wise meta-analysis of fMRI studies. Neurosci. Biobehav. Rev. 128, 294–310 (2021).
Kühn, S. & Gallinat, J. Common biology of craving across legal and illegal drugs — a quantitative meta-analysis of cue–reactivity brain response. Eur. J. Neurosci. 33, 1318–1326 (2011).
Volkow, N. D., Fowler, J., Wang, G., Baler, R. & Telang, F. Imaging dopamine’s role in drug abuse and addiction. Neuropharmacology 56, 3–8 (2009).
Volkow, N. D., Koob, G. & Baler, R. Biomarkers in substance use disorders. ACS Chem. Neurosci. 6, 522–525 (2015).
Volkow, N. D. & Li, T.-K. Drug addiction: the neurobiology of behaviour gone awry. Nat. Rev. Neurosci. 5, 963–970 (2004).
Luijten, M., Schellekens, A. F., Kühn, S., Machielse, M. W. & Sescousse, G. Disruption of reward processing in addiction: an image-based meta-analysis of functional magnetic resonance imaging studies. JAMA Psychiatry 74, 387–398 (2017).
Vollm, B. et al. Neuronal correlates and serotonergic modulation of behavioural inhibition and reward in healthy and antisocial individuals. J. Psychiatr. Res. 44, 123–131 (2010).
Mazas, C. A., Finn, P. R. & Steinmetz, J. E. Decision-making biases, antisocial personality, and early-onset alcoholism. Alcoholism 24, 1034–1040 (2000).
Peters, J. & Buchel, C. The neural mechanisms of inter-temporal decision-making: understanding variability. Trends Cognit. Sci. 15, 227–239 (2011).
Bickel, W. K., Johnson, M. W., Koffarnus, M. N., MacKillop, J. & Murphy, J. G. The behavioral economics of substance use disorders: reinforcement pathologies and their repair. Annu. Rev. Clin. Psychol. 10, 641–677 (2014).
Bjork, J. M., Hommer, D. W., Grant, S. J. & Danube, C. Impulsivity in abstinent alcohol-dependent patients: relation to control subjects and type 1-/type 2-like traits. Alcohol 34, 133–150 (2004).
Claus, E. D., Kiehl, K. A. & Hutchison, K. E. Neural and behavioral mechanisms of impulsive choice in alcohol use disorder. Alcohol. Clin. Exp. Res. 35, 1209–1219 (2011).
Mitchell, J. M., Fields, H. L., D’esposito, M. & Boettiger, C. A. Impulsive responding in alcoholics. Alcohol. Clin. Exp. Res. 29, 2158–2169 (2005).
Petry, N. M. Delay discounting of money and alcohol in actively using alcoholics, currently abstinent alcoholics, and controls. Psychopharmacology 154, 243–250 (2001).
Coffey, S. F., Gudleski, G. D., Saladin, M. E. & Brady, K. T. Impulsivity and rapid discounting of delayed hypothetical rewards in cocaine-dependent individuals. Exp. Clin. Psychopharmacol. 11, 18–25 (2003).
Heil, S. H., Johnson, M. W., Higgins, S. T. & Bickel, W. K. Delay discounting in currently using and currently abstinent cocaine-dependent outpatients and non-drug-using matched controls. Addict. Behav. 31, 1290–1294 (2006).
Hoffman, W. F. et al. Neuropsychological function and delay discounting in methamphetamine-dependent individuals. Psychopharmacology 188, 162–170 (2006).
Hoffman, W. F. et al. Cortical activation during delay discounting in abstinent methamphetamine dependent individuals. Psychopharmacology 201, 183–193 (2008).
Monterosso, J. R., Aron, A. R., Cordova, X., Xu, J. & London, E. D. Deficits in response inhibition associated with chronic methamphetamine abuse. Drug Alcohol. Depend. 79, 273–277 (2005).
Kirby, K. N., Petry, N. M. & Bickel, W. K. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J. Exp. Psychol. Gen. 128, 78–87 (1999).
Kirby, K. N. & Petry, N. M. Heroin and cocaine abusers have higher discount rates for delayed rewards than alcoholics or non-drug-using controls. Addiction 99, 461–471 (2004).
MacKillop, J. et al. Delayed reward discounting and addictive behavior: a meta-analysis. Psychopharmacology 216, 305–321 (2011).
Paret, C., Jennen-Steinmetz, C. & Schmahl, C. Disadvantageous decision-making in borderline personality disorder: partial support from a meta-analytic review. Neurosci. Biobehav. Rev. 72, 301–309 (2017).
Amlung, M. et al. Delay discounting as a transdiagnostic process in psychiatric disorders: a meta-analysis. JAMA Psychiatry 76, 1176–1186 (2019).
Petry, N. M. Discounting of delayed rewards in substance abusers: relationship to antisocial personality disorder. Psychopharmacology 162, 425–432 (2002).
Andrade, L. F., Riven, L. & Petry, N. M. Associations between antisocial personality disorder and sex on discounting rates. Psychol. Rec. 64, 639–646 (2014).
Bobova, L., Finn, P. R., Rickert, M. E. & Lucas, J. Disinhibitory psychopathology and delay discounting in alcohol dependence: personality and cognitive correlates. Exp. Clin. Psychopharmacol. 17, 51–61 (2009).
Sargeant, M. N., Bornovalova, M. A., Trotman, A. J. M., Fishman, S. & Lejuez, C. W. Facets of impulsivity in the relationship between antisocial personality and abstinence. Addict. Behav. 37, 293–298 (2012).
Hosking, J. G. et al. Disrupted prefrontal regulation of striatal subjective value signals in psychopathy. Neuron 95, 221–231.e4 (2017).
Morgan, J. E., Gray, N. S. & Snowden, R. J. The relationship between psychopathy and impulsivity: a multi-impulsivity measurement approach. Pers. Individ. Differ. 51, 429–434 (2011).
Sebastian, A., Jacob, G., Lieb, K. & Tüscher, O. Impulsivity in borderline personality disorder: a matter of disturbed impulse control or a facet of emotional dysregulation? Curr. Psychiatry Rep. 15, 339 (2013).
Miyake, A. & Friedman, N. P. The nature and organization of individual differences in executive functions: four general conclusions. Curr. Dir. Psychol. Sci. 21, 8–14 (2012).
Smith, J. L., Mattick, R. P., Jamadar, S. D. & Iredale, J. M. Deficits in behavioural inhibition in substance abuse and addiction: a meta-analysis. Drug Alcohol. Depend. 145, 1–33 (2014).
Noël, X. et al. Supervisory attentional system in nonamnesic alcoholic men. Arch. Gen. Psychiatry 58, 1152–1158 (2001).
Ornstein, T. et al. Profiles of cognitive dysfunction in chronic amphetamine and heroin abusers. Neuropsychopharmacology 23, 113–126 (2000).
Verdejo-García, A., Bechara, A., Recknor, E. C. & Perez-Garcia, M. Executive dysfunction in substance dependent individuals during drug use and abstinence: an examination of the behavioral, cognitive and emotional correlates of addiction. J. Int. Neuropsychol. Soc. 12, 405–415 (2006).
Wittmann, M., Leland, D. S., Churan, J. & Paulus, M. P. Impaired time perception and motor timing in stimulant-dependent subjects. Drug Alcohol. Depend. 90, 183–192 (2007).
Ersche, K. D. et al. Cognitive dysfunction and anxious-impulsive personality traits are endophenotypes for drug dependence. Am. J. Psychiatry 169, 926–936 (2012).
Ersche, K. D., Clark, L., London, M., Robbins, T. W. & Sahakian, B. J. Profile of executive and memory function associated with amphetamine and opiate dependence. Neuropsychopharmacology 31, 1036–1047 (2006).
Shallice, T. Specific impairments of planning. Philos. Trans. R. Soc. London B Biol. Sci. 298, 199–209 (1982).
Zhang, M. et al. Shared gray matter alterations in subtypes of addiction: a voxel-wise meta-analysis. Psychopharmacology 238, 2365–2379 (2021).
Goldstein, R. Z. & Volkow, N. D. Dysfunction of the prefrontal cortex in addiction: neuroimaging findings and clinical implications. Nat. Rev. Neurosci. 12, 652–669 (2011).
Zilverstand, A., Huang, A. S., Alia-Klein, N. & Goldstein, R. Z. Neuroimaging impaired response inhibition and salience attribution in human drug addiction: a systematic review. Neuron 98, 886–903 (2018).
Ogilvie, J. M., Stewart, A. L., Chan, R. C. K. & Shum, D. H. K. Neuropsychological measures of executive function and antisocial behavior: a meta-analysis. Criminology 49, 1063–1107 (2011).
Dolan, M. & Anderson, I. M. Executive and memory function and its relationship to trait impulsivity and aggression in personality disordered offenders. J. Forensic Psychiatry 13, 503–526 (2002).
Morgan, A. B. & Lilienfeld, S. O. A meta-analytic review of the relation between antisocial behavior and neuropsychological measures of executive function. Clin. Psychol. Rev. 20, 113–136 (2000).
Dolan, M. & Park, I. The neuropsychology of antisocial personality disorder. Psychol. Med. 32, 417–427 (2002).
Stuppy-Sullivan, A. M. & Baskin-Sommers, A. Evaluating dysfunction in cognition and reward among offenders with antisocial personality disorder. Personal. Disord. 10, 416–426 (2019).
Verona, E., Sprague, J. & Sadeh, N. Inhibitory control and negative emotional processing in psychopathy and antisocial personality disorder. J. Abnorm. Psychol. 121, 498–510 (2012).
Hagenhoff, M. et al. Executive functions in borderline personality disorder. Psychiatry Res. 210, 224–231 (2013).
Sprock, J., Rader, T. J., Kendall, J. P. & Yoder, C. Y. Neuropsychological functioning in patients with borderline personality disorder. J. Clin. Psychol. 56, 1587–1600 (2000).
Domes, G. et al. The influence of emotions on inhibitory functioning in borderline personality disorder. Psychol. Med. 36, 1163–1172 (2006).
Linhartová, P. et al. Impulsivity in patients with borderline personality disorder: a comprehensive profile compared with healthy people and patients with ADHD. Psychol.Med. 50, 1829–1838 (2020).
Maes, J. H. & Brazil, I. A. No clear evidence for a positive association between the interpersonal-affective aspects of psychopathy and executive functioning. Psychiatry Res. 210, 1265–1274 (2013).
Baskin-Sommers, A. R. et al. Mapping the association of global executive functioning onto diverse measures of psychopathic traits. Personal. Disord. 6, 336–346 (2015).
Zeier, J. D., Baskin-Sommers, A. R., Hiatt Racer, K. D. & Newman, J. P. Cognitive control deficits associated with antisocial personality disorder and psychopathy. Personal. Disord. 3, 283–293 (2012).
Raymond, J. Interactions of attention, emotion and motivation. Prog. Brain Res. 176, 293–308 (2009).
Petersen, S. E. & Posner, M. I. The attention system of the human brain: 20 years after. Annu. Rev. Neurosci. 35, 73–89 (2012).
Myers, N. E., Stokes, M. G. & Nobre, A. C. Prioritizing information during working memory: beyond sustained internal attention. Trends Cognit. Sci. 21, 449–461 (2017).
Le Pelley, M. E., Mitchell, C. J., Beesley, T., George, D. N. & Wills, A. J. Attention and associative learning in humans: an integrative review. Psychol. Bull. 142, 1111–1140 (2016).
Tillem, S. M., Weinstein, H. & Baskin-Sommers, A. Psychopathy is associated with an exaggerated attention bottleneck: EEG and behavioral evidence from a dual-task paradigm. Cogn. Affect. Behav. Neurosci. 21, 881–893 (2021).
Dux, P. E., Ivanoff, J., Asplund, C. L. & Marois, R. Isolation of a central bottleneck of information processing with time-resolved FMRI. Neuron 52, 1109–1120 (2006).
Newman, J. P. & Baskin-Sommers, A. in Cognitive Neuroscience of Attention 421–440 (Guilford Press, 2011).
Baskin-Sommers, A., Curtin, J. J. & Newman, J. P. Emotion-modulated startle in psychopathy: clarifying familiar effects. J. Abnorm. Psychol. 122, 458–468 (2013).
Baskin-Sommers, A., Curtin, J. J. & Newman, J. P. Specifying the attentional selection that moderates the fearlessness of psychopathic offenders. Psychol. Sci. 22, 226–234 (2011).
Baskin-Sommers, A., Curtin, J. J., Li, W. & Newman, J. P. Psychopathy-related differences in selective attention are captured by an early event-related potential. Personal. Disord. 3, 370–378 (2012).
Larson, C. L. et al. The interplay of attention and emotion: top-down attention modulates amygdala activation in psychopathy. Cognitive, Affective, Behav. Neurosci. 13, 757–770 (2013).
Sadeh, N. & Verona, E. Visual complexity attenuates emotional processing in psychopathy: implications for fear-potentiated startle deficits. Cogn. Affect. Behav. Neurosci. 12, 346–360 (2012).
Newman, J. P. & Kosson, D. S. Passive avoidance learning in psychopathic and nonpsychopathic offenders. J. Abnorm. Psychol. 95, 252–256 (1986).
Newman, J. P. & Schmitt, W. A. Passive avoidance in psychopathic offenders: a replication and extension. J. Abnorm. Psychol. 107, 527–532 (1998).
Drayton, L., Santos, L. & Baskin-Sommers, A. Psychopaths fail to automatically take the perspective of others. Proc. Natl Acad. Sci. USA 115, 3302–3307 (2018).
Anderson, B. A. What is abnormal about addiction-related attentional biases? Drug Alcohol. Depend. 167, 8–14 (2016).
Verdejo-Garcia, A., Garcia-Fernandez, G. & Dom, G. Cognition and addiction. Dialogues Clin. Neurosci. 21, 281–290 (2019).
Boutros, N. N., Gooding, D., Sundaresan, K., Burroughs, S. & Johanson, C. E. Cocaine-dependence and cocaine-induced paranoia and mid-latency auditory evoked responses and sensory gating. Psychiatry Res. 145, 147–154 (2006).
Lijffijt, M. et al. A pilot study revealing impaired P50 gating in antisocial personality disorder. J. Neuropsychiatry Clin. Neurosci. 21, 328–331 (2009).
Casey, B., Taylor-Thompson, K., Rubien-Thomas, E., Robbins, M. & Baskin-Sommers, A. Healthy development as a human right: insights from developmental neuroscience for youth justice. Annu. Rev. Law Soc. Sci. 16, 203–222 (2020).
Mizner, S. Police ‘command and control’ culture is often lethal — especially for people with disabilities. ACLU https://www.aclu.org/blog/criminal-law-reform/reforming-police/police-command-and-control-culture-often-lethal-especially (2018).
Cheatham, A. & Maizland, L. How police compare in different democracies. CFR, https://www.cfr.org/backgrounder/how-police-compare-different-democracies (2021).
Yu, R., Geddes, J. R. & Fazel, S. Personality disorders, violence, and antisocial behavior: a systematic review and meta-regression analysis. J. Personal. Disord. 26, 775–792 (2012).
Grann, M. & Fazel, S. Substance misuse and violent crime: Swedish population study. BMJ 328, 1233–1234 (2004).
National Alliance on Mental Illness. Crisis Intervention Team (CIT) programs. NAMI https://www.nami.org/Advocacy/Crisis-Intervention/Crisis-Intervention-Team-(CIT)-Programs (2021).
Compton, M. T. et al. The police-based crisis intervention team (CIT) model: I. Effects on officers’ knowledge, attitudes, and skills. Psychiatr. Serv. 65, 517–522 (2014).
Compton, M. T. et al. The police-based crisis intervention team (CIT) model: II. Effects on level of force and resolution, referral, and arrest. Psychiatr. Serv. 65, 523–529 (2014).
Watson, A. C. & Wood, J. D. Everyday police work during mental health encounters: a study of call resolutions in Chicago and their implications for diversion. Behav. Sci. Law 35, 442–455 (2017).
Rogers, M. S., McNiel, D. E. & Binder, R. L. Effectiveness of police crisis intervention training programs. J. Am. Acad. Psychiatry Law 47, 414–421 (2019).
American Law Institute. Model Penal Code: Official Draft and Explanatory Notes: Complete Text of Model Penal Code as Adopted at the 1962 Annual Meeting of the American Law Institute at Washington, D.C., May 24, 1962 (The Institute, 1985).
Legal Dictionary. Model Penal Code. The Free Dictionary https://legal-dictionary.thefreedictionary.com/Model+Penal+Code (2021).
Yaffe, G. in Addiction and Self-Control (ed. Levy, N.) 190–213 (Oxford Univ. Press 2013).
Coppola, F. Motus animi in mente insana. J. Crim. Law Criminol. 109, 1–70 (2019).
Miley, L. N. et al. An examination of the effects of mental disorders as mitigating factors on capital sentencing outcomes. Behav. Sci. Law 38, 381–405 (2020).
Skeem, J. L., Polaschek, D., Patrick, C. J. & Lilienfeld, S. O. Psychopathic personality: bridging the gap between scientific evidence and public policy. Psychol. Sci. Public Interest. 12, 95–162 (2011).
Donohue, A., Arya, V., Fitch, L. & Hammen, D. Legal insanity: assessment of the inability to refrain. Psychiatry 5, 58–66 (2008).
Yaffe, G. in Handbook of Clinical Neurology Vol. 118 (eds Bernat, J. L. & Richard Beresford, H.) 345–356 (Elsevier, 2013).
National Institute of Justice. Overview of drug courts. NIJ https://nij.ojp.gov/topics/articles/overview-drug-courts (2020).
Olver, M. E. et al. Reliability and validity of the Psychopathy Checklist — Revised in the assessment of risk for institutional violence: a cautionary note on DeMatteo et al. Psychol. Public Policy Law 26, 490–510 (2020).
Dellazizzo, L., Luigi, M., Giguère, C. É., Goulet, M. H. & Dumais, A. Is mental illness associated with placement into solitary confinement in correctional settings? A systematic review and meta-analysis. Int. J. Ment. Health Nurs. 29, 576–589 (2020).
Aiyer, S. M., Heinze, J. E., Miller, A. L., Stoddard, S. A. & Zimmerman, M. A. Exposure to violence predicting cortisol response during adolescence and early adulthood: understanding moderating factors. J. Youth Adolesc. 43, 1066–1079 (2014).
Bronson, J. & Berzofsky, M. Indicators of Mental Health Problems Reported by Prisoners and Jail Inmates, 2011–12. Report No. NCJ250612 (US Department of Justice, 2017).
Brooner, R. K., Kidorf, M., King, V. L. & Stoller, K. Preliminary evidence of good treatment response in antisocial drug abusers. Drug Alcohol. Depend. 49, 249–260 (1998).
Messina, N. P., Wish, E. D. & Nemes, S. Therapeutic community treatment for substance abusers with antisocial personality disorder. J. Subst. Abuse Treat. 17, 121–128 (1999).
Budney, A. J., Sigmon, S. C. & Higgins, S. T. in Addiction Recovery Tools: A Practical Handbook Ch. 9 (ed. Coombts, R. H.) 147–170 (SAGE, 2001).
McHugh, R. K., Hearon, B. A. & Otto, M. W. Cognitive behavioral therapy for substance use disorders. Psychiatr. Clin. North Am. 33, 511–525 (2010).
Linehan, M. M. Cognitive-Behavioral Treatment of Borderline Personality Disorder (Guilford Publications, 2018).
National Alliance on Mental Illness. Mental health treatment while incarcerated. NAMI https://www.nami.org/Advocacy/Policy-Priorities/Improving-Health/Mental-Health-Treatment-While-Incarcerated (2021).
Haney, C. Reforming Punishment: Psychological Limits to the Pains of Imprisonment. (American Psychological Association, 2006).
de Boer, J. & Gerrits, J. Learning from Holland: the TBS system. Psychiatry 6, 459–461 (2007).
Satel, S. & Lilienfeld, S. O. Addiction and the brain-disease fallacy. Front. Psychiatry 4, 141 (2014).
Chang, S.-A. A., Tillem, S., Benson-Williams, C. & Baskin-Sommers, A. Cognitive empathy in subtypes of antisocial individuals. Front. Psychiatry 12, 1070 (2021).
Magnusson, K. Interpreting Cohen’s d effect size: an interactive visualization. RPsychologist https://rpsychologist.com/cohend/ (2021).
Brazil, I. A., van Dongen, J. D. M., Maes, J. H. R., Mars, R. B. & Baskin-Sommers, A. Classification and treatment of antisocial individuals: from behavior to biocognition. Neurosci. Biobehav. Rev. 91, 259–277 (2016).
Mossman, D. From group data to useful probabilities: the relevance of actuarial risk assessment in individual instances. J. Am. Acad. Psychiatry Law 43, 93–102 (2014).
Scurich, N. & John, R. S. A Bayesian approach to the group versus individual prediction controversy in actuarial risk assessment. Law Hum. Behav. 36, 237–246 (2012).
Newman, J. P., Curtin, J. J., Bertsch, J. D. & Baskin-Sommers, A. Attention moderates the fearlessness of psychopathic offenders. Biol. Psychiatry 67, 66–70 (2010).
Douaihy, A. B., Kelly, T. M. & Sullivan, C. Medications for substance use disorders. Soc. Work. Public Health 28, 264–278 (2013).
Volkow, N. D. & Skolnick, P. New medications for substance use disorders: challenges and opportunities. Neuropsychopharmacology 37, 290–292 (2012).
National Institute on Drug Abuse. Principles of drug addiction treatment: a research-based guide. National Institutes of Health https://www.drugabuse.gov/publications/principles-drug-addiction-treatment-research-based-guide-third-edition (2018).
Smedslund, G. et al. Motivational interviewing for substance abuse. Cochrane Database Syst. Rev. 7, 1–126 (2011).
Zanarini, M. C., Frankenburg, F. R., Reich, D. B., Harned, A. L. & Fitzmaurice, G. M. Rates of psychotropic medication use reported by borderline patients and axis II comparison subjects over 16 years of prospective follow-up. J. Clin. Psychopharmacol. 35, 63–67 (2015).
Kendall, T., Burbeck, R. & Bateman, A. Pharmacotherapy for borderline personality disorder: NICE guideline. Br. J. Psychiatry 196, 158–159 (2010).
Bateman, A. & Fonagy, P. Mentalization based treatment for borderline personality disorder. World Psychiatry 9, 11 (2010).
Black, D. W. The treatment of antisocial personality disorder. Curr. Treat. Options Psychiatry 4, 295–302 (2017).
Salekin, R. T. Psychopathy and therapeutic pessimism clinical lore or clinical reality? Clin. Forensic Psychol. Law 22, 257–290 (2019).
Acknowledgements
A.B.-S. thanks the Russell Sage Foundation for providing space to think through the topics covered in this Review.
Author information
Authors and Affiliations
Contributions
A.B-S. researched data for the Review. A.B-S. and C.S contributed substantially to discussion of the content. All authors contributed to writing the Review, and reviewed and/or edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Peer review
Peer review information
Nature Reviews Psychology thanks Katja Bertsch, Keanan Joyner and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Glossary
- Hierarchical Taxonomy of Psychopathology (HiTOP)
-
A newer classification system focused on grouping signs, symptoms, and maladaptive traits and behaviours into broad spectra of psychopathology rather than discrete categorical diagnoses.
- Amygdala
-
A region of the brain important for emotion processing and detecting salient information.
- Ventromedial prefrontal cortex
-
A brain region in the prefrontal cortex that is involved in processing risk, emotional responding and the cognitive processing of morality.
- Fronto-limbic circuitry
-
Neural circuitry that connects the frontal lobe with subcortical regions, such as the amygdala, and regulates mood, cognition and behaviour.
- Hippocampus
-
A brain structure embedded in the temporal lobe that has a major role in learning and memory.
- Mesocorticolimbic circuitry
-
Neural circuitry that extends from regions deep within the brain to the prefrontal cortex to transport dopamine (a neurotransmitter) and supports reward learning.
- Orbitofrontal cortex
-
A brain region in the prefrontal cortex that has a role in representing the affective values of reinforcers in decision-making, executive function and learning.
- Startle response
-
The magnitude of muscle twitch measured by placing sensors on the orbicularis oculi muscle under the eye.
- Electroencephalography
-
A non-invasive electrical monitoring method to record electrical activity on the scalp through a cap and sensors placed on the head and face.
Rights and permissions
About this article
Cite this article
Baskin-Sommers, A., Ruiz, S., Sarcos, B. et al. Cognitive–affective factors underlying disinhibitory disorders and legal implications. Nat Rev Psychol 1, 145–160 (2022). https://doi.org/10.1038/s44159-022-00020-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s44159-022-00020-8