Abstract
Background
Predominant affective temperament may affect adherence to prescribed pharmacotherapeutic interventions, warranting systematic review and meta-analysis.
Methods
The Scopus, Web of Science, PubMed, and OVID MedLine databases were inquired since inception up to 31st of March 2022 for records of any study design documenting quantitative evidence about affective temperaments as measured by the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego (TEMPS-A) questionnaire and treatment adherence measured by the means of major rating scales on the matter. People with low vs. high levels of treatment adherence, matched for otherwise clinically relevant variables, were deemed as cases and controls, respectively, using standardized mean differences (SMDs) in pertinent scores under random-effects meta-analysis.
Results
Nine studies encompassing 1138 subjects pointed towards significantly higher cyclothymic (SMD = −0.872; CI: [−1.51 to −0.24]; p = 0.007), irritable (SMD = −0.773; CI: [−1.17 to −0.37]; p < 0.001) and depressive (SMD = −0.758; CI: [−1.38 to −0.14]; p = 0.017) TEMPS-A scores both for psychiatric and nonpsychiatric samples with poorer adherence.
Limitations
Intrinsic limitations of the present report include the heterogeneity of the operational definitions documented across different primary studies, which nonetheless reported on the sole medication-treatment adherence, thus limiting the generalizability of the present findings based on a handful of comparisons.
Conclusions
Though further primary studies need to systematically account for different clinical and psychosocial moderators across different clinical populations and operational definitions, cyclothymic, depressive, and irritable temperament scores may nonetheless predict treatment adherence and, thus, overall treatment outcomes.
Similar content being viewed by others
Introduction
Affective temperaments (namely depressive, cyclothymic, hyperthymic, irritable, and anxious) represent relatively stable [1] —though stressor-sensitive [2]—biological “cores” of personality developing early during the lifespan, accounting for much of the individual activity level, rhythms, moods, and related cognitions according to their classical Akiskalian conceptualization rooting back to Greek psychological medicine and philosophy [3].
Though void of any pathological value per se, affective temperaments may nonetheless represent vulnerability factors towards the development of various configurations of mood [4] as well as other psychiatric disorders [5] and specific somatic conditions [6,7,8,9,10,11,12,13,14,15,16,17]. Affective temperaments may also affect the long-term course and treatment outcome of various conditions, although evidence modeling the relationship between affective temperaments and the prognosis of somatic diseases is tentative [13, 15, 18, 19].
The role of affective temperaments in prognosis and illness course in somatic illnesses in part may be related to their impact on complying with treatment recommendations. Adherence is the degree to which a patient follows therapeutic advice, including recommended lifestyle changes such as diet or exercise beyond the prescribed drugs [20]. According to the World Health Organization (WHO) statistics, the rate of adherence to long-term treatment of chronic diseases in developed countries does not exceed 50%, and in developing countries, the rate is even lower. Inadequate adherence to long-term therapies seriously jeopardizes the effectiveness of treatment and is, therefore, a critical issue in the health of the population for both qualities of life and health economics fields [20].
Affective temperaments can be readily assessed by broadly validated tools such as the Temperament Evaluation of Memphis, Pisa, Paris, and San Diego Autoquestionnaire (TEMPS-A) [21, 22], with recent evidence suggesting their influence on treatment adherence [23,24,25,26,27,28,29,30,31,32]. The identification of high-risk subgroups with critical treatment adherence should, theoretically, inform the treatment plan, ideally aiding the personalized medicine approach and enhancing the cost-effective interventions.
Despite the associated clinical and public health burden, most of the available studies documenting treatment adherence in relationship with affective temperaments is hampered by low statistical power, essentially due to the small representativeness of the samples, or they rely on inhomogeneous ratings for the same outcomes.
Both of the latter issues could nonetheless be effectively addressed using a meta-analytic approach, providing a meaningful overall effect estimation from pooling low statistical original studies applying different versions of the TEMPS using SMD (standardized mean difference). The aim of the present study was to investigate the effect of affective temperaments on medication adherence in psychiatric as well as in nonpsychiatric patients using a systematic review and meta-analysis approach.
Methods
The present systematic review and meta-analysis follow the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA), 2020 edition [33]. The review was not pre-registered.
Search strategy
We searched the Scopus, Web of Science, PubMed, and OVID MedLine databases from inception up to 31st of March 2022. The following search terms were used: “TEMPS-A” AND (“adherence” OR “compliance”) followed by manual search and cross-references validation.
Study selection
After pooling all the publications identified by the literature search across different databases, duplicate records were removed using a reference management software (EndNote v.20, Clarivate Analytics) [34] before fine manual review for duplicates. Two authors (GS and PD) performed the title and abstract screening, extracting the relevant full-texts using a-priori built extraction form (see below), and also assessed study eligibility and extracted data from the selected studies independently. Any eventual discrepancy between the reviewing authors was solved by consensus by inquiring a third author with considerable expertise in the field (XG).
No study design, age group, treatment modality, or publication language was applied. Contact with the authors was planned as necessary.
As our search terms included “TEMPS-A”, no qualitative studies were identified. We included studies that provided quantitative data both for the specific affective temperament types (measured with the TEMPS-A questionnaire) and for treatment adherence or compliance (measured with any adherence scale). For analysis of the effect size, associations of TEMPS-A scores and treatment adherence (e.g., mean difference, correlation) were also required.
Data extraction and analysis
From all included articles, we systematically extracted the following data: country of origin, characteristics of the patient populations (sample size, sex ratio, age, type of patient population), affective temperaments measurement scale, adherence measurement method and scale, and the reported mean affective temperament subscale ratings of the adherent and non-adherent patient groups with the corresponding indicator of standard deviation (SD), or the correlation coefficient of the different affective temperament subscale ratings and the adherence score. In those studies, where both mean and correlation was presented, we chose correlation to minimize inconsistency caused by the arbitrarily defined cut-points used to dichotomize adherence scales into adherent and non-adherent groups. In those studies, where more than two adherence subgroups were compared, or the means were reported separately by sex, we merged subgroups by calculating the weighted mean and pooled SD for the given related groups. For the meta-analysis, the extracted values were converted to standardized mean differences (SMDs) and standard deviations (SDs) for all included studies. Since we assumed significant methodological heterogeneity due to the lack of a uniform adherence measurement method, we used the random-effects method for meta-analytic pooling, based on SMDs in scores between adherent and non-adherent subjects. Meta-analytic findings are reported as pooled-SMDs with 95% confidence intervals (CIs).
Between-study heterogeneity was determined by calculating the prediction interval of the distribution of true effects. The I2, Q, and Tau2 statistics were likewise computed (where the Q-statistic provides a test of the null hypothesis that all studies in the analysis share a common effect size; I2 tells us what percentage of the variance in observed effects reflects variance in true effects rather than sampling error, and Tau2 is the variance of the true effects sizes) [35]. Possible causes of heterogeneity were explored by visual inspection of forest plots looking for outlier values and by subgroup analysis. Also, possible moderators were investigated by meta-regression analysis. Patient population, age, sex, and country of origin were analysed as possible moderators for all temperament subscales separately.
Quality and risk of bias within studies was assessed using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [36]. Publication bias were assessed using funnel plot techniques, Begg and Mazumdar’s method, and Egger’s regression test. Sensitivity analysis was performed to test the impact of the individual studies and also the impact of the effect size index selection.
All statistical analyses were implemented using the R package metaphor v.3.0 [37].
Results
The adopted search strategy returned a total of 219 hits, resulting in 169 records after duplicate removal, which were screened on the title and abstract for inclusion criteria, out of which 147 were excluded for not providing required information. Twenty-two records were ultimately selected for detailed review and potential inclusion. In one of the identified studies, necessary data were only partially reported, but successful contact with the authors allowed for the inclusion of that record [24].
Ten publications were found eligible for meta-analytic synthesis [23,24,25,–26, 28,29,30,31,32, 38], though one record was ultimately disregarded since its adherence definition (treatment drop-out) significantly differed from the rest of the other included studies (medication adherence). Finally, nine records encompassing 1138 subjects effectively participated in the meta-analytic synthesis of the evidence (Fig. 1 and Table 1).
Core characteristics of the nine analyzed reports [23,24,25,–26, 28,29,30,31,32] appear in Table 1. All studies found significant associations between adherence and TEMPS-A scores for one or more of cyclothymic, depressive, anxious, irritable, or hyperthymic temperament across four psychiatric and five nonpsychiatric samples. TEMPS-A subscale scores were higher among non-adherent versus adherent subjects as follows: irritable (k = 8 out of 9 = 89%), cyclothymic (k = 6 out of 9 = 67%), depressive (k = 6 out of 9 = 67%), anxious (k = 3 out of 9 = 33%), hyperthymic (k = 1 out of 9 = 11%).
Quality and risk of bias within studies
The risk of bias within studies was assessed by using the NIH Quality Assessment Tool for Observational Cohort and Cross-Sectional Studies [36] (Supplementary Table 1). According to our assessment, we identified potential risks of bias in seven studies [23,24,25,–26, 28, 29, 31] due to using non-validated scales, applying the non-standardized definition of cut-points used to dichotomize adherence scales into adherent and non-adherent groups, or potential imprecision in reported data.
Meta-analysis
Quantitative analysis was performed for each affective temperament type to test for differences in TEMPS-A subscale scores between adherent and non-adherent subjects. A negative effect represents that subjects with higher TEMPS-A scores favoring lower adherence. All results are reported in detail in Table 2, and those of particular interest are summarized below.
Based on nine studies meeting inclusion criteria (total n = 1138 subjects), patients with lower adherence had significantly higher cyclothymic (SMD = −0.869, CI: [−1.54 to −0.2], p = 0.011), irritable (SMD = −0.772 [CI: −1.14 to −0.4], p < 0.001) and depressive (SMD = −0.756, CI: [−1.39 to −0.12], p = 0.019) TEMPS-A scores compared to adherent subjects. Anxious (p = 0.072) and hyperthymic (p = 0.817) TEMPS scores were not different between the two groups.
Heterogeneity was high for all temperaments subscales (I2 = 88–95%, p < 0.001), with wide prediction intervals for the true effect size estimation, including zero, suggesting that true effects vary from around −2.9 SMD in some populations to 1.2 SMD in others.
Forest plots with pooled SMDs, 95% CIs, and 95% prediction intervals (PIs) for the relevant temperament subscales (where statistically significant associations of affective temperament scores with adherence were found) are presented in Fig. 2.
Forest plots based on random-effects meta-analyses of TEMPS-A scores for cyclothymic, irritable, and depressive temperaments with 95% confidence intervals (CIs) in nine comparisons of adherent versus non-adherent subjects (total n = 1138), with pooled standardized mean differences (SMDs). The estimated 95% prediction interval (PI) likewise presented, in which the true effect size was predicted to fall in 95% of all comparable populations.
Sensitivity analysis
Impact of one outlying study
The inspection of the forest plots (Fig. 2) revealed one outlying study [29], which reported a much bigger effect size than the rest of the others. Meta-analysis was repeated with the exclusion of the latter study. The main findings of the meta-analysis without the one outlier study are summarized in Table 3.
Exclusion of the outlying study from the meta-analysis resulted in a still large sample (k = 8, n = 918), insignificant heterogeneity (I2 = 32–37%, p > .05), and a somewhat reduced but still significant negative meta-analytic association for cyclothymic, irritable and depressive temperaments. Estimated PIs do not include zero anymore, suggesting that in 95% of all comparable populations, a negative true effect exists.
Forest plots without the one outlier study with pooled SMDs, 95% CIs, and 95% prediction intervals for the relevant temperament subscales are presented in Fig. 3.
Forest plots without the one excluded study, based on random-effects meta-analyses of TEMPSA scores for cyclothymic, irritable, and depressive temperaments with 95% CIs in eight comparisons of adherent versus non-adherent subjects (total n = 918), with pooled SMDs. The estimated 95% PIs also displayed, in which the true effect size was predicted to fall in 95% of all comparable populations.
Impact of individual studies
In order to investigate the impact of each individual study on the summary estimate, sensitivity analysis was performed by iteratively excluding one study from the analyses and recalculating the overall SMDs. We performed analyses both with and without the excluded outlying study in order to make sure that its removal didn’t cause any bias (Supplementary Tables 2, 3). The overall SMDs did not vary substantially after excluding any individual study, indicating that the results were not driven by one of the analyzed individual studies, either with or without the excluded outlying study.
Impact of the selected effect size index
As presented in Table 1, the reported effect size indices were heterogeneous among the included studies, some measured effect size as SMD, while others as correlation. We decided to select SMD as our effect size index in the current analysis, and although correlation and SMD can be mathematically converted to each other, this conversion might have an impact on the results in some cases [39]. In order to investigate the impact of this selection on the summary estimates, sensitivity analysis was performed by recalculating all the reported results with correlation instead of SMD as the effect size index. We performed analyses both with and without the excluded outlying study in order to make sure that converting between effect size indices didn’t cause any bias (Supplementary Tables 4, 5). The overall results did not vary substantially with correlation as the effect size index, indicating that the results were not biased by the effect size selection.
Publication bias
Publication bias analysis was performed on 8 studies after the removal of one outlier [23,24,25,–26, 28, 30,31,32]. Based on inspection of funnel plots, and also on Egger’s regression and Begg and Mazumdar’s rank correlation tests (p = 0.976; 0.933; 0.497, and p = 1.000; 0.548; 0.398 for cyclothymic/irritable/depressive TEMPS-A subscales, respectively), there was no evidence of publication bias (Supplementary Fig. 1).
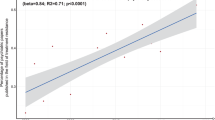
Moderator variables
In case of cyclothymic, irritable, and depressive temperaments, meta-regression results didn’t show any moderating effect of age, sex, patient population, or country of origin. In case of anxious temperament subgroup analysis revealed that among psychiatric patients anxious temperament scores were significantly higher with medication non-adherence vs adherence (SMD = -0.593; CI: [−0.82 to −0.36]; p < 0.001), but not in nonpsychiatric population (SMD = −0.042; CI: [−0.38 to 0.3]; p = 0.807). In case of hyperthymic temperament, female sex moderated the effect on medication adherence (Slope = −0.0449, CI: [−0.08 to −0.01], p = 0.009, and Intercept = 2.269; CI: [0.55 to 3.98]; p = 0.009), R2 = 49.03%). All the meta-regression results are reported in Supplementary Table 6.
Discussion
Based on nine studies meeting inclusion criteria involving 1138 subjects in total, strong, adverse associations of affective temperament scores with adherence were found for cyclothymic, irritable, and depressive temperaments both in psychiatric and nonpsychiatric patient samples either with or without the outlier study suggesting an involvement of these temperamental types in determining decreased adherence.
Therapeutic adherence, especially in various somatic and psychiatric disorders of a more chronic nature requiring longer-term or continuous maintenance therapy is pivotal to controlling the symptoms and preventing recurrences in the majority of disorders, influencing illness course and outcome, thus the success and safety of using the efficacious treatment and the long-term well-being of patients. Adherence to treatment is also strongly related to preventable healthcare costs related to relapses and recurrences, repeated hospital admissions, a chronic disease course, and resulting decreased productivity [23], amounting to an estimated 100 billion USD in the US alone [40].
Finding and selecting an efficacious pharmacological treatment is thus only one component of the therapeutic success, while the other, equally important and equally challenging, is the active participation of the patient in the form of adhering to medical recommendations. In case of all medical specialties combined, it is estimated that 30–50% of patients do not take their medications as prescribed [40]. Thus increasing the efficacy of adherence to interventions is an imminent public health challenge prompting the WHO to claim that improving adherence would have a significantly greater impact on the general health of the population than improvement in specific pharmacological and other medical treatments [20, 40].
The biopsychosocial model of illness acknowledges biological, psychological, and social aspects as equally important in understanding and explaining treatment adherence [41]. Therapy adherence is a highly complex process involving multiple contributing factors of both dynamic and static nature, including a complex pattern of factors related to the patient, the treatment, the doctor-patient relationship, and the environment, many of which are underlined by psychological characteristics of the patient. Moreover, as opposed to more concrete barriers to adherence, psychological barriers are more challenging and complex, thus also more difficult to identify and address [42]. Important components of these psychological barriers include or are determined by personality and temperamental factors of the patients, which have been less studied, even though these are strongly associated with adherence-related behaviors by determining emotions, cognitions, attitudes as well as reactions. It has increasingly been suggested that personality may have a significant impact on the long-term course and outcomes of several illnesses, and also medication adherence may, in fact, be an important factor mediating this effect [43]. Especially considering that the paradigm shift from compliance to adherence in describing the willingness of the patient to cooperate with the prescribed treatment was prompted by abandoning the conceptualization of the patient as the passive and obedient part in their treatment in favor of a more active role where the patient assumes a behavior matching the clinician's recommendation on all components of treatment including pharmacotherapy, lifestyle, as well as following up with appointments and further tests, we increasingly understand that good treatment management requires understanding of such patient characteristics as personal experience, disease-related beliefs, perception of health status, psychological state, as well as personality and temperamental factors of the patients [23].
Several models of medication adherence have been developed which aim to take the psychological characteristics of patients into consideration. These include for example the Health Belief Model by Rosenstock [44] highlighting the role of beliefs about susceptibility and seriousness of a health problem leading to a perception of threat which will be combined with perceived benefits and barriers of a course of action, a personal sense of self-efficacy, and environmental cues to action, together determining engagement in a behavior aimed at addressing the health threat; The Theory of Planned Behavior [45] which focuses on the role of intentions, shaped by attitudes, norms and perceived self-efficacy, in predicting adherence-related behaviors; the Necessity-Concerns Framework which suggests that beliefs about necessity of treatment are weighed against worries about adverse effects as the key determinants of decisions on adherence, or the Information-Motivation-Strategy model [46] which addresses cognitive, social and environmental factors postulating that the patient must have sufficient information on what they should do, have to possess the motivation to do it, and must have the strategy and means to actually execute it. The above models include several important aspects where temperamental and personality factors, and specifically affective temperaments, which determine emotional reactivity, related cognitions, and behaviors, may have a key contribution to actually determine adherence-related behaviors.
In light of the above, our results supporting that more marked irritable, cyclothymic and depressive affective temperaments are associated with decreased adherence may hold several important clinical and public health implications. The analysis and understanding of these factors and their impact on non-adherent behavior may provide important cues for both identifying the psychological support of patients to be able to better cooperate with therapy, as well as for psychological or psychiatric interventions if necessary to increase adherence. By identifying temperamental contributors for non-adherence, screening methods and risk indicators, as well as focused psychotherapeutic, education and supportive methods could also be developed. Thus, understanding the role of the core of personality, i.e., temperament and how they influence medication-related attitudes, beliefs, cognitions, emotions, and behaviors would provide a novel and crucial possibility to develop patient-tailored and personalized education, support, and intervention methods to target the obstacles of adhering to medical recommendations and increase the active participation of patients in their successful treatment.
Out of the five affective temperament types described by Akiskal, we saw the significant impact of three, namely, cyclothymic, irritable, and depressive, on an increased risk of non-adherence to therapy. Considering the characteristics of these affective temperamental types may provide some clues both on how they influence adherence and what types of interventions they allow for. In general, cyclothymic and irritable temperaments induce less favorable reactions toward disturbing events [30]. Corresponding to earlier definitions by Kraepelin, cyclothymic temperament is a constitutive predisposition toward intolerance of subjective pain as well as a tendency for enhanced emotional response upon intense stressful and painful experience [22, 29] and is also associated with hopelessness [47]. Thus, these temperaments would make it more difficult to tolerate the burden of taking long-term medications, accepting the unchangeable fact of illness and sustained or even lifelong adherence to the required medication regime, and make also the acceptance of having to tolerate side effects more difficult.
Nevertheless, before further interpreting the results, we must also mention the initially detected high heterogeneity and the possible underlying causes. Although in the current meta-analysis, heterogeneity turned out to be mostly driven by one outlying study, and its exclusion made the sample rather homogenous, the initial high heterogeneity was not unexpected due to the different patient populations, the various methods used to measure adherence, and the fact, that adherence in clinical practice is a combined and dimensional construct with several influencing factors.
The issue of various measurement methods is not specific to this particular study, according to a recent systematic review of the existing adherence measurement scales, there are at least 121 patient-reported outcome measures on medication adherence in clinical use with various levels of consistency of their different psychometric properties [48]. In our current analysis, all nine included studies used different methods for recording adherence. Six different scales were used (MMAS, MARS, BAASIS, VAS, CRS, Likert scale), also different versions of one scale and different cut-off points were used to dichotomize adherence data. But despite all of this variability of adherence measurement methods, our results suggest that, in fact, they all addressed the same phenomenon because, with the removal of only one outlier study, heterogeneity between the rest of the studies became insignificant.
Regarding different patient populations, high heterogeneity was also presumed. Although emerging evidence supports the influence of temperament on treatment adherence both in psychiatric and nonpsychiatric populations, there are several other influencing factors, some of which may be deeply related to the different kinds of diseases and illness phases. For instance, in psychiatric practice, adherence to antipsychotics is highly related to a substantial lack of insight [49], whereas poor adherence in depression may be more related to cognitive aspects rather than a lack of will to step out of acute depression [50]. Also, in case of psychotropic medications of any kind, fear of stigmatization can play a role in non-adherence [50], while this factor is not relevant in case of chronic somatic diseases [51]. In case of diabetes treatment, the prevalence of non-adherence to insulin is higher compared to prescribed oral antidiabetics due to the fear of injections and the embarrassment related to injecting in public [52], which is also a unique factor related to this certain disease and more specifically to this certain prescribed medication. These are just a few examples of how different factors may underlie non-adherence in different patient groups. Unfortunately, current evidence doesn’t allow for such subtler distinction due to the lack of data for quantitative meta-analysis, however, the performed subgroup analysis suggests that the effect of cyclothymic, irritable, and depressive temperaments on adherence are not significantly different between psychiatric and nonpsychiatric populations. A possible explanation for this could be either that affective temperaments have a direct effect on adherence which is independent of the patient population, which can be explained by the general characteristics of these temperament types discussed earlier, or that affective temperaments have a different kind of indirect moderating effect on the different kind of underlying factors finally all resulting in non-adherence. For instance, among psychiatric patients, cyclothymic temperament has been found to be associated with negative attitudes toward psychotropic medications and their negative side effects, which may result in decreased adherence [32], while among patients with diabetes, cyclothymic temperament type has been associated with inadequate eating habits, which may also indirectly affect adherence to medical recommendations and disease outcome [24]. Both assumptions (direct and indirect effects of affective temperaments) are presumably valid, but we still have quite little knowledge about the causal relations behind.
In fact, there should be several additional moderators and mediators which may moderate (or may be in turn moderated by) the biological effect modifiers (affective temperaments, in this instance) and, therefore, might also explain the dispersion of real effects and as such, the initially detected heterogeneity and the observed effect size of the outlier study. A number of patient-related risk and protective factors for adherence have been identified so far—we already mentioned some of them earlier—that can possibly be also influenced by affective temperaments to some extent. These include, but are not limited to lower socioeconomic status, ethnicity, the impact of local cultural norms, social pressure or stigmatization, adolescence and old age, loneliness in old age, psychiatric disorders associated with the disease, personality disorders, comorbid somatic diseases, drug use, cognitive impairment, pregnancy, disease severity, poor insight and negative drug-related beliefs [50]. Also, while affective temperaments should hold relatively stable during the lifespan, they have also been found to be sensitive to certain factors, such as age, sex, or severity of illness [53].
In the present study, moderator analysis hasn’t identified any moderators in case of cyclothymic, irritable, and depressive temperaments, while anxious predominant temperament was found to be a possible risk factor for treatment non-adherence in psychiatric populations and hyperthymic predominant temperament as a possible protective factor against non-adherence among male subjects. It is important to note that the number of eligible studies may not have provided enough statistical power to examine moderating factors by meta-regression, furthermore, in some of the original studies, adherence and affective temperaments were not the measures of interest, but they themselves were the confounding or moderator variables, therefore no data was available on additional factors possibly moderating the affective temperament-adherence relationship.
As we discussed above, adherence is a complex construct with several possible moderating and mediating factors, so research in the next step should focus on identifying these external factors indirectly affecting temperament expressions or factors moderating their effect on treatment adherence, also delineating the different causal processes behind the non-adherence—temperament relationship in case of different diseases. Especially because affective temperaments are strongly genetically- and biologically based, exhibit a stable course throughout the lifespan, and are relatively unmodifiable directly using psychological and psychotherapeutic technics, so even though they are somewhat sensitive to external stimuli and stressors, changing them cannot be a realistic goal even in case of a patient-tailored and personalized therapy. However, we also see that although temperaments may affect adherence directly to some extent through behavior consistent with those traits (e.g., patients with cyclothymic temperament might be more intolerant of subjective pain), temperament most often not directly, but indirectly affects adherence by shaping behavior through different perceptions and processing of environmental stimuli [54, 55], which mediating factors, in turn, can already be modified through psychological and psychotherapeutic techniques.
Thus, rather than affective temperaments being the focus of psychotherapy themselves, we should first identify these mediating and moderating factors followed by targeting those with educational, supportive, and psychotherapeutic techniques in order to improve treatment adherence and overall treatment outcomes as a consequence. We should also understand how the genetic background and socioeconomic contributors to the development of temperaments may be related to later medication adherence.
Limitations
Intrinsic limitations of the present study essentially rely on the paucity of evidence eligible for inclusion as well as the various thresholds set by the authors to operationally defined adherence outcomes.
Conclusions
To the best of our knowledge, this is the first meta-analysis to show that affective temperament scores measured by the TEMPS-A scale can contribute to identifying the risk of medication non-adherence. Though further primary studies need to systematically account for different clinical and psychosocial moderators across different clinical populations and operational definitions, cyclothymic, depressive, and irritable temperament scores may nonetheless predict treatment adherence and, thus, overall treatment outcomes. In clinical practice, the TEMPS-A scale might be useful for screening patients before treatment in order to identify non-adherent high-risk groups and support them to increase their adherence. The real goal for forthcoming ecological studies is to explain the variance of effect modifier, i.e. affective temperament beyond other confounding factors across different settings. While affective temperaments should hold relatively stable during the lifespan, they may nonetheless be sensitive to intense environmental stressors, thus understanding the residual variance of modifiable factors is crucial from a public health perspective.
References
Kawamura Y, Akiyama T, Shimada T, Minato T, Umekage T, Noda Y, et al. Six-year stability of affective temperaments as measured by TEMPS-A. Psychopathology. 2010;43:240–7.
Gonda X, Eszlári N, Sutori S Aspan N, Rihmer Z, Juhasz G, et al. Nature and nurture: effects of affective temperaments on depressive symptoms are markedly modified by stress exposure. Front Psychiatry. 2020;11:599.
Akiskal HS, Akiskal KK. In search of Aristotle: temperament, human nature, melancholia, creativity and eminence. J Affect Disord. 2007;100:1–6.
Miola A, Baldessarini RJ, Pinna M, Tondo L. Relationships of affective temperament ratings to diagnosis and morbidity measures in major affective disorders. Eur Psychiatry. 2021;64:e74.
Rihmer Z, Akiskal KK, Rihmer A, Akiskal HS. Current research on affective temperaments. Curr Opin Psychiatry. 2010;23:12–8.
Vecsey-Nagy M, Szilveszter B, Kolossvary M, Boussoussou M, Vattay B, Gonda X, et al. The association between accelerated vascular aging and cyclothymic affective temperament in women. J Psychosom Res. 2021;145:110423.
Korosi B, Vecsey-Nagy M, Kolossvary M, Nemcsik-Bencze Z, Szilveszter B, Laszlo A, et al. Association between cyclothymic affective temperament and age of onset of hypertension. Int J Hypertens. 2019;2019:9248247.
Korsi B, Gyngysi H, Batta D, Laszlo A, Kovacs I, Tisler A, et al. Evaluation of affective temperaments and arterial stiffness in different hypertension phenotypes. Hypertens Res. 2021;44:47–54.
Vecsey-Nagy M, Szilveszter B, Kolossváry M, Gonda X, Rihmer Z, Merkely B, et al. The association between early vascular aging and cyclothymic affective temperament. Eur Heart J Cardiovasc Imaging. 2021;22:jeaa356.239.
Kőrösi B, Batta D, Gonda X, Rihmer Z, Nemcsik-Bencze Z, Laszlo A, et al. Association between irritable affective temperament and nighttime peripheral and central systolic blood pressure in hypertension. Artery Res. 2019;25:41–7.
Korosi B, László A, Tabák Á, Batta D, Lenart L, Fekete A, et al. The impact of currently recommended antihypertensive therapy on depression and other psychometric parameters: a prospective pilot study. Neuropsychopharmacol Hung. 2017;27:S849–50.
Eory A, Rozsa S, Torzsa P, Kalabay L, Gonda X, Rihmer Z. Affective temperaments contribute to cardiac complications in hypertension independently of depression. Psychother Psychosom. 2014;83:187–9.
Eőry A, Gonda X, Torzsa P, Kalabay L, Rihmer Z. Affective temperaments: from neurobiological roots to clinical application. Orv Hetil. 2011;152:1879–86.
László A, Babos L, Kis-Igari Z, Pálfy A, Torzsa P, Eőry A, et al. Identification of hypertensive patients with dominant affective temperaments might improve the psychopathological and cardiovascular risk stratification: a pilot, case–control study. Ann Gen Psychiatry. 2015;14:1–8.
Eory A, Gonda X, Lang Z, Torzsa P, Kalman J, Kalabay L, et al. Personality and cardiovascular risk: Association between hypertension and affective temperaments-a cross-sectional observational study in primary care settings. Eur J Gen Pract. 2014;20:247–52.
Hargittay C, Gonda X, Markus B, Sipkovits Z, Voros K, Kalabay L, et al. The relationship between anxiety and diabetes. Orv Hetil. 2021;162:1226–32.
Lesiewska N, Kamińska A, Junik R, Michalewicz M, Myszkowski B, Borkowska A, et al. Affective temperament and glycemic control–the psychological aspect of obesity and diabetes mellitus. Diabetes Metab Syndr Obes. 2021;14:4981.
Rihmer Z, Akiskal KK, Rihmer A, Akiskal HS. Current research on affective temperaments. Curr Opin Psychiatry. 2010;23:12–18.
Vecsey-Nagy M, Szilveszter B, Kolossvary M, Boussoussou M, Vattay B, Gonda X, et al. The association between accelerated vascular aging and cyclothymic affective temperament in women. J Psychosom Res. 2021;145:6.
World Health Organization (WHO). Adherence to long-term therapies: evidence for action. Geneva: World Health Organization, 2003.
Dembińska-Krajewska D, Rybakowski J. [The Temperament Evaluation of Memphis, Pisa and San Diego Autoquestionnaire (TEMPS-A)–an important tool to study affective temperaments]. Psychiatr Pol. 2014;48:261–76.
Akiskal HS, Akiskal KK, Haykal RF, Manning JS, Connor PD. TEMPS-A: progress towards validation of a self-rated clinical version of the Temperament Evaluation of the Memphis, Pisa, Paris, and San Diego Autoquestionnaire. J Affect Disord. 2005;85:3–16.
Pasquale CD, Veroux M, Fornaro M, Sinagra N, Basile G, Gozzo C, et al. Psychological perspective of medication adherence in transplantation. World J Transplant. 2016;6:736.
Yamamoto T, Sakurai K, Watanabe M, Sakuma I, Kanahara N, Shiina A, et al. Cyclothymic temperament is associated with poor medication adherence and disordered eating in type 2 diabetes patients: a case–control study. Diabetes Ther. 2021;12:2611–24.
Shamsi A, Yavarmanesh H, Harati H, Eiliaei S, Sadeghian M. The relationship between medication adherence and affective temperaments in patients with congestive heart failure. Psychiatria. 2021;17:115–20.
Shamsi A, Khodaifar F, Arzaghi SM, Sarvghadi F, Ghazi A. Is there any relationship between medication compliance and affective temperaments in patients with type 2 diabetes?. J diabetes Metab Disord. 2014;13:96.
Moola S, Munn Z, Tufanaru C, Aromataris E, Sears K, Sfetcu R, et al. Systematic reviews of etiology and risk. In: Aromataris E, Munn Z, editors. JBI manual for evidence synthesis. Adelaide, Australia: JBI, 2020.
Kamei K, Terao T, Katayama Y, Hoaki N. Affective temperaments and psychotropic adherence. J Affect Disord. 2013;150:1142–7.
Fornaro M, De Berardis D, Iasevoli F, Pistorio ML, D’Angelo E, Mungo S, et al. Treatment adherence towards prescribed medications in bipolar-II acute depressed patients: relationship with cyclothymic temperament and “therapeutic sensation seeking” in response towards subjective intolerance to pain. J Affect Disord. 2013;151:596–604.
Buturak SV, Emel EB, Koçak OM. The effect of temperament on the treatment adherence of bipolar disorder type I. Nord J Psychiatry. 2016;70:176–82.
Belvederi Murri M, Mamberto S, Briatore L, Mazzucchelli C, Amore M, Cordera R. The interplay between diabetes, depression and affective temperaments: a structural equation model. J Affect Disord. 2017;219:64–71.
Bahrini L, Damak R, Cheour M. The role of the affective temperament in the treatment adherence in psychiatry. Pan Afr Med J. 2015;25:2.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. J Clin Epidemiol. 2021;134:178–89.
Team TE EndNote. Clarivate: Philadelphia. 2013.
Borenstein M. Common mistakes in meta-analysis: and how to avoid them. Biostat, Incorporated. New Jersey USA; 2019.
Health, N.I.o. Quality assessment tool for observational cohort and cross-sectional studies [Internet]. Bethesda (MD): American. 2014 [cited 2017 Aug 27]. Available from https://www.nhlbi.nih.gov/health-topics/study-quality-assessment-tools.
Viechtbauer W. Conducting meta-analyses in R with the metafor Package. J Stat Softw. 2010;36:1–48.
Fornaro M, Novello S, Fusco A, Anastasia A, De Prisco M, Mondin AM, et al. Clinical features associated with early drop-out among outpatients with unipolar and bipolar depression. J Psychiatr Res. 2021;136:522–8.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, et al. Cochrane handbook for systematic reviews of interventions. New Jersey: John Wiley & Sons, 2019
Marcum ZA, Sevick MA, Handler SM. Medication nonadherence: a diagnosable and treatable medical condition. JAMA. 2013;309:2105–6.
Lindau ST, Laumann EO, Levinson W, Waite LJ. Synthesis of scientific disciplines in pursuit of health: The interactive biopsychosocial model. Perspect Biol Med. 2003;46:S74.
Martin LR, Feig C, Maksoudian CR, Wysong K, Faasse K. A perspective on nonadherence to drug therapy: psychological barriers and strategies to overcome nonadherence. Patient Prefer Adherence. 2018;12:1527.
van Dooren FE, Nefs G, Schram MT, Verhey FR, Denollet J, Pouwer F. Depression and risk of mortality in people with diabetes mellitus: a systematic review and meta-analysis. PLoS ONE. 2013;8:e57058.
Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–35.
Ajzen I. The theory of planned behavior. Organ Behav Hum Decis Process. 1991;50:179–211.
DiMatteo MR, Haskard-Zolnierek KB, Martin LR. Improving patient adherence: a three-factor model to guide practice. Health Psychol Rev. 2012;6:74–91.
Innamorati M, Rihmer Z, Akiskal H, Gonda X, Erbuto D, Murri MB, et al. Cyclothymic temperament rather than polarity is associated with hopelessness and suicidality in hospitalized patients with mood disorders. J Affect Disord. 2015;170:161–5.
Kwan YH, Weng SD, Loh DHF, Phang JK, Oo LJY, Blalock DV, et al. Measurement properties of existing patient-reported outcome measures on medication adherence: systematic review. J Med Internet Res. 2020;22:e19179.
García S, Martínez-Cengotitabengoa M, López-Zurbano S, Zorrilla I, López P, Vieta E, et al. Adherence to antipsychotic medication in bipolar disorder and schizophrenic patients: a systematic review. J Clin Psychopharmacol. 2016;36:355–71.
Solmi M, Miola A, Croatto G, Pigato G, Favaro A, Fornaro M, et al. How can we improve antidepressant adherence in the management of depression? A targeted review and 10 clinical recommendations. Braz J Psychiatry. 2021;43:189–202.
Cheen MHH, Tan YZ, Oh LF, Wee HL, Thumboo J. Prevalence of and factors associated with primary medication non-adherence in chronic disease: a systematic review and meta-analysis. Int J Clin Pr. 2019;73:e13350.
Krass I, Schieback P, Dhippayom T. Adherence to diabetes medication: a systematic review. Diabet Med. 2015;32:725–37.
Solmi M, Zaninotto L, Toffanin T, Veronese N, Lin K, Stubbs B, et al. A comparative meta-analysis of TEMPS scores across mood disorder patients, their first-degree relatives, healthy controls, and other psychiatric disorders. J Affect Disord. 2016;196:32–46.
Vo PT, Bogg T. Testing theory of planned behavior and neo-socioanalytic theory models of trait activity, industriousness, exercise social cognitions, exercise intentions, and physical activity in a representative US sample. Front Psychol. 2015;6:1114.
Hampson SE. Personality processes: mechanisms by which personality traits “get outside the skin”. Annu Rev Psychol. 2012;63:315–39.
Funding
Open access funding provided by Semmelweis University.
Author information
Authors and Affiliations
Contributions
GS: conceptualization, methodology, search, title and abstract screening, data extraction, data analysis, visualization, writing original draft and further versions. MF: conceptualization, methodology, interpretation, and critical revision of the manuscript for important intellectual content. PD: search, title and abstract screening, data extraction, review and commenting original draft and further versions. SV: conceptualization, review and commenting original draft and further verions. XG: conceptualization, methodology, writing and review original draft and further versions, interpretation, study supervision. All authors have approved the final article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Szabo, G., Fornaro, M., Dome, P. et al. A bitter pill to swallow? Impact of affective temperaments on treatment adherence: a systematic review and meta-analysis. Transl Psychiatry 12, 360 (2022). https://doi.org/10.1038/s41398-022-02129-z
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-022-02129-z
This article is cited by
-
Adherence to dietary recommendations mediates the effect of affective temperaments on infertility treatment outcomes
Scientific Reports (2024)
-
Affective temperaments show stronger association with infertility treatment success compared to somatic factors, highlighting the role of personality focused interventions
Scientific Reports (2023)