Abstract
Postsynaptic α2A-adrenoceptor density is enhanced in the dorsolateral prefrontal cortex (DLPFC) of antipsychotic-treated schizophrenia subjects. This alteration might be due to transcriptional activation, and could be regulated by epigenetic mechanisms such as histone posttranslational modifications (PTMs). The aim of this study was to evaluate ADRA2A and ADRA2C gene expression (codifying for α2-adrenoceptor subtypes), and permissive and repressive histone PTMs at gene promoter regions in the DLPFC of subjects with schizophrenia and matched controls (n = 24 pairs). We studied the effect of antipsychotic (AP) treatment in AP-free (n = 12) and AP-treated (n = 12) subgroups of schizophrenia subjects and in rats acutely and chronically treated with typical and atypical antipsychotics. ADRA2A mRNA expression was selectively upregulated in AP-treated schizophrenia subjects (+93%) whereas ADRA2C mRNA expression was upregulated in all schizophrenia subjects (+53%) regardless of antipsychotic treatment. Acute and chronic clozapine treatment in rats did not alter brain cortex Adra2a mRNA expression but increased Adra2c mRNA expression. Both ADRA2A and ADRA2C promoter regions showed epigenetic modification by histone methylation and acetylation in human DLPFC. The upregulation of ADRA2A expression in AP-treated schizophrenia subjects might be related to observed bivalent chromatin at ADRA2A promoter region in schizophrenia (depicted by increased permissive H3K4me3 and repressive H3K27me3) and could be triggered by the enhanced H4K16ac at ADRA2A promoter. In conclusion, epigenetic predisposition differentially modulated ADRA2A and ADRA2C mRNA expression in DLPFC of schizophrenia subjects.
Similar content being viewed by others
Introduction
Schizophrenia is a chronic and disabling disease that affects around 1% of the world population [1]. Schizophrenia is recognized by positive (including delusions and hallucinations), negative (including lack of motivation and social withdrawal), and cognitive symptoms (including disturbances in working memory, selective attention, and learning). Noradrenergic system and its α2-adrenoceptors have been proposed to play a role in the pathophysiology and treatment of schizophrenia [2]. Among the three α2-adrenoceptor subtypes (α2A, α2B, and α2C), α2A- and α2C-adrenoceptors show the broadest distribution in central nervous system and they could be relevant in mental disorders as schizophrenia due to their specific role in memory and cognition [3]. Preclinical and clinical data have suggested that selective α2A-adrenoceptor agonists and α2C-adrenoceptor antagonists can ameliorate cognitive deficits [3,4,5,6,7]. The α2-adrenoceptor subtype-selective effects might be ascribed to their differential synaptic location in human dorsolateral prefrontal cortex (DLPFC) [8], a brain region that controls cognitive processes and emotions. In detail, presynaptically located α2-adrenoceptors might affect neuropsychiatric symptoms due to their effect on neurotransmitter feedback and regulation, whereas postsynaptic α2-adrenoceptors in DLPFC (mainly α2A-adrenoceptor subtype) may be critical in the regulation of cognitive functions as working memory [6]. In line with this, we recently reported postsynaptic α2A-adrenoceptor subtype upregulation in schizophrenia subjects [9]. This finding was specific for those schizophrenia subjects that were under antipsychotic treatment.
Schizophrenia’s etiology has been proposed to be multifactorial, because of the multiple small-effect but fewer large-effect susceptibility gene variants identified [10, 11]. α2A- and α2C-adrenoceptors are codified by ADRA2A and ADRA2C genes, which are located on chromosomes C10 and C4, respectively. Candidate gene studies have not found any association between polymorphisms at ADRA2A/C genes and schizophrenia [12,13,14,15]. Environmental factors may also contribute to the disorder’s etiology by their impact on epigenetic mechanisms [16, 17]. Epigenetics confers short- and long-term gene expression changes with no alteration of the DNA code and comprises mechanisms such as DNA methylation, histone post-translational modifications (PTMs), chromatin remodeling, and expression of noncoding RNAs. Several evidence suggests that histone PTMs contribute to the development of schizophrenia. Some of these findings are: altered expression of various enzymes, such as increased expression of histone methyltransferases (HMT) [18,19,20], histone deacetylase 1 (HDAC1) [21, 22], and reduced expression of HDAC2 [23, 24] in prefrontal cortex (PFC) of schizophrenia subjects. Studies of chromatin immunoprecipitation followed by sequencing (ChIP-Seq) in human brain have found an overrepresentation of open chromatin-associated modifications [histone H3 lysine 4 trimethylation (H3K4me3 and histone H3 lysine 27 acetylation (H3K27ac)] in schizophrenia-related genes, this finding being specific for neuronal cells [25]. Actually, studies in brain cortex of schizophrenia subjects have identified altered histone H3 acetylation and methylation at promoter regions of certain genes [26,27,28]. More recently, ChIP-seq evaluation of cell-type H3K4me3 in PFC of schizophrenia subjects has revealed individual alterations in neurons [29]. These findings, along with the observed HDAC inhibitory activity of mood stabilizer valproate when administered at therapeutic doses in schizophrenia [30, 31] suggest the importance of histone PTMs in schizophrenia.
The present study aimed to assess the mRNA expression of ADRA2A and ADRA2C in postmortem DLPFC of schizophrenia subjects. Due to the relevance of epigenetic changes in schizophrenia and given the possibility that histone PTMs at promoter regions could regulate ADRA2A and ADRA2C mRNA expression, we also evaluated PTMs of histone H3 (H3K4me3, H3K27me3, H3ac, H3K9ac, H3K27ac) and H4 (H4K5ac and H4K16ac) at promoter regions of both ADRA2A and ADRA2C genes. In addition, we evaluated the possible modulation of mRNA expression and epigenetic mechanisms by antipsychotic treatment by comparing schizophrenia subjects according to antipsychotic drug presence or absence in blood at the time of death.
Materials and methods
Postmortem human brain samples
Schizophrenia and control subjects included in this study were the same 48 subjects assessed in a previous work (see Brocos-Mosquera et al. [9] for detailed description). Briefly, human brain samples of DLPFC (Brodmann’s area 9, BA 9) were obtained at autopsies in the Basque Institute of Legal Medicine, Bilbao, Spain, and immediately stored at −70 °C until assay. As previously described [9], toxicological screening for the detection of antidepressants, antipsychotics, psychotropic drugs, and ethanol on blood was performed at the National Institute of Toxicology, Madrid, Spain.
Twenty-four subjects had an antemortem diagnosis of schizophrenia and were matched to 24 control subjects for sex, age, postmortem delay (time interval between death and autopsy, PMD), and storage time of the samples (ST, Table 1). Schizophrenia subjects were divided in 12 antipsychotic-free (AP-free) and 12 antipsychotic-treated (AP-treated) subjects according to the presence or absence of antipsychotics in blood at the time of death. Out of the 24 matched pairs of schizophrenia and control subjects, 5 pairs had to be excluded from the ADRA2A and ADRA2C mRNA expression study due to technical reasons [RNA integrity number (RIN) value below 5 and/or absence of cDNA amplification for more than one gene]. Full description of demographic and toxicological characteristics of all subjects in mRNA and epigenetics studies is shown in respective Supplementary Tables 1 and 2. Seventeen out of the 24 schizophrenia subjects had died by suicide, with a similar distribution in AP-free and -treated subgroups (see Supplementary Table 3 for summarized demographic characteristics). A cohort of suicide victims with antemortem diagnosis of major depression and matched controls was used for hypothesis validation (n = 13, see Supplementary Table 4 for demographic characteristics). Samples from schizophrenia or major depression subjects and matched controls were always processed in parallel. The study was developed in accordance with legal policy and ethical review boards for postmortem brain studies.
Animals and treatments
Animal housing and treatment were performed as already described [32]. Mice were randomly assigned to the different experimental groups. Briefly, male Sprague-Dawley rats were submitted to acute and chronic treatment with selected representative antipsychotic drugs with atypical and typical profile. Acutely treated rats were injected i.p. with saline (1 ml/kg, n = 5), risperidone (1 mg/kg, n = 5), clozapine (10 mg/kg, n = 4; both from Tocris, Bristol, UK) or haloperidol (1 mg/kg, n = 4; Sigma Aldrich, MO, USA) and sacrificed 3 h after the injection. Chronically treated rats were injected i.p., every 12 h, during 21 days, with saline (1 ml/kg, n = 6), risperidone (0.5 mg/kg, n = 6), clozapine (5 mg/kg, n = 6) or haloperidol (0.5 mg/kg, n = 6). Animals were sacrificed 48 h after the last injection of risperidone or clozapine and 72 h after that of haloperidol or saline. Brain cortex was dissected and stored at −70 °C until assays.
mRNA expression and cDNA synthesis
Total RNA was extracted using commercial RiboPureTM kit (Thermo Fisher Scientific, Waltham, MA, USA) according to the manufacturer’s instructions. RNA concentration and quality were measured in a NanoDrop 1000 Spectrophotometer (Thermo Fisher Scientific). RIN was also assessed for RNA quality in the Agilent 2100 Bioanalyzer (Agilent, Santa Clara, CA, USA) using Agilent RNA 6000 Nano kit and RNA Nano chips following the manufacturer’s instructions (see Supplementary Tables 1 and 4). Extracted human RNA underwent DNase digestion using the Deoxyribonuclease I, Amplification Grade (Thermo Fisher). 1 µg of total RNA was converted to single-stranded cDNA using High-Capacity cDNA Reverse Transcription kit (Thermo Fisher) following the manufacturer’s instructions.
Chromatin immunoprecipitation (ChIP) assay
Human postmortem brain (120 mg) was homogenized in 810 μl of douncing buffer (4 mM MgCl2, 1 mM CaCl2, and 10 mM Tris-HCl; pH = 7.5) and incubated with 1 U/ml of micrococcal nuclease (MNase; Sigma-Aldrich, St. Louis, MO, USA) for 10 min at 37 °C. The MNase activity was stopped by adding 10 mM EDTA. The sample was diluted by adding nine-fold volume excess of hypotonic lysis buffer [0.1 mM benzamidine, 0.1 mM phenylmethylsulfonylfluoride (PMSF), 1.5 mM 1,4-dithio-dl-threitol (DTT), and 0.2 mM EDTA; pH = 8.0] and then incubated on ice for 1 h. The sample was centrifuged at 1000 × g (5810 R centrifuge; Eppendorf, Hamburg, Germany) for 10 min at 4 °C to remove insoluble material. Soluble chromatin was diluted adding ten times concentrated incubation buffer (50 mM EDTA, 500 mM NaCl, and 200 mM Tris-HCl; pH = 7.5). 60 µl of diluted chromatin (input sample) were removed and saved at 4 °C until elution. Primary antibodies at different concentrations (see Supplementary Table 5) and 20 μl of fully suspended protein A magnetic beads (Millipore, Burlington, MA, USA) were added to aliquots of diluted chromatin and incubated overnight at 4 °C with rotation. Protein A magnetic beads were pelleted with the magnetic separator and the supernatant removed completely. Then, the protein A bead-antibody/chromatin complexes were washed by resuspending the pelleted beads in 0.5 ml each of the following cold buffers in this order: low salt (150 mM NaCl, 20 mM Tris-HCl, 2 mM EDTA, 0.1% SDS, 1% Triton X-100; pH = 8.1); high salt (500 mM NaCl, 20 mM Tris-HCl, 2 mM EDTA, 0.1% SDS,1% Triton X-100; pH = 8.1); LiCl immune complex wash buffer (250 mM LiCl, 10 mM Tris-HCl, 1 mM EDTA, 0.01% IGEPAL CA630, 0.01% deoxycholic acid; pH = 8.1) and TE buffer (1 mM EDTA, 10 mM Tris-HCl; pH = 8.1). Once resuspended in each washing buffer, beads were incubated for 20 min at 4 °C with rotation, followed by magnetic clearance and careful removal of supernatant fraction prior to the addition of next washing buffer. Elution of protein/DNA complexes to free DNA was carried out by incubation of immune complexes and input samples in ChIP elution buffer (1% SDS, 0.1 M NaHCO3) with proteinase K (100 ug/ml) at 62 °C for 2 h with shaking followed by an incubation at 95 °C for 10 min. Magnetic beads were separated from the complex antibody/chromatin and DNA in the supernatant of all samples (input included) was purified with QIAquick PCR purification kit (Qiagen, Hilden, Germany) following the manufacturer’s instructions. Final DNA volume was 1:4 diluted in molecular grade water.
Quantitative real-time PCR
Quantitative real time PCR (qPCR) was performed on cDNA synthesized from isolated mRNA and on genomic DNA obtained from ChIP assays. qPCR reactions were carried out using Power or Fast SYBR Green Master Mix (Thermo Fisher, Waltham, MA) on a StepOneTM system (Thermo Fisher) following the manufacturer’s instructions. The final volume for each reaction was 10 μl with either 20 ng of cDNA or 4 µl of genomic DNA (obtained from ChIP experiments) and corresponding gene specific primers (see Supplementary Table 6 for detailed specifications). Dissociation curve analyses were carried out at the end of each run for PCR product verification. mRNA expression of reference genes was assessed by pre-designed TaqMan® assays (Supplementary Table 7). All samples were run in triplicates. Each run included a negative water control. See Supplementary Figs. 1–3 for detailed characterization of qPCR assays.
Data analysis and statistical procedures
The mRNA expression of target genes ADRA2A and ADRA2C was corrected with that of reference genes GAPDH and RPS13, and with a reference sample (pool of control samples) using ΔΔCt method: ΔΔCt = (Ct (target gene)sample – Ct (reference gene)sample) – (Ct (target gene)reference sample – Ct (reference gene) reference sample). The relative amount of mRNA was calculated as 2−ΔΔCt. In the case of animal data, mRNA expression of Adra2a and Adra2c genes was corrected with that of Gapdh and Rps29. For ChIP data, fold changes relative to 6% of input DNA were determined using the comparative Ct method, where ΔCt = Ct (target gene)immunoprecipitated DNA sample – Ct (target gene)6% input DNA. The relative amount of immunoprecipitated DNA was calculated as 2−ΔCt. Relative amounts of both mRNA and DNA were subjected to Grubbs’ test to detect any possible outlier.
Data analysis was performed with GraphPad Prism 8© (GraphPad Software, Inc., San Diego, CA, USA), SPSS 26.0 (Chicago, IL, USA), and InVivoStat [33] programs, and results expressed as means ± SEM. Correlations between sex, age, PMD, ST, RIN, and experimental data were determined using multiple regression analysis. When significant, the relationship between numerical variables and experimental data was further studied by simple linear regression analysis. Statistical comparison of the means between control and schizophrenia subjects, and between males and females was performed by two-tailed Student’s t-test. If significant, statistical differences between means were studied by ANCOVA analysis with relevant variable as covariate. Statistical analysis of animal data was performed by one-way ANOVA test followed by Tukey’s multiple comparisons test. P values < 0.05 were considered statistically significant.
Results
Demographic and methodological variables contributing to ADRA2A and ADRA2C mRNA expression in human DLPFC
First, multiple regression analysis of data from control subjects was performed in order to study the contribution of nominal predictor variables (sex) and continuous predictor variables (age, PMD, ST, and RIN) to corrected ADRA2A and ADRA2C mRNA expression. A significant model emerged [F(1,17) = 9.568, p = 0.007]. The analysis revealed that corrected ADRA2A mRNA expression was significantly influenced by RIN of the samples (β = −0.6, p = 0.007), regardless of sex and age of the subjects and PMD and ST. Linear regression analysis showed a negative correlation between RIN and corrected ADRA2A mRNA expression (Supplementary Fig. 4). By contrast, corrected ADRA2C mRNA expression was not influenced by any of the variables. Therefore, when significant differences in ADRA2A mRNA expression between groups were observed, subsequent ANCOVA analyses with RIN as covariate were performed.
ADRA2A and ADRA2C mRNA expression in postmortem human DLPFC of schizophrenia subjects and matched controls
ADRA2A mRNA expression in schizophrenia subjects was not statistically different from that in matched controls (Δ = +25%, n = 19, p = 0.25, Fig. 1A). Division of schizophrenia group by presence or absence of blood antipsychotics revealed a significant increase in ADRA2A mRNA expression in AP-treated subjects (Δ = +93% vs matched controls, n = 9, p = 0.042, Fig. 1A). As previously mentioned, RIN of the samples negatively influenced ADRA2A mRNA expression. Although RIN of the samples was not significantly different between AP-treated schizophrenia subjects and matched controls (see Supplementary Table 1), ANCOVA analysis with RIN as covariate was performed. ANCOVA analysis estimated that ADRA2A mRNA expression in AP-treated schizophrenia subjects was 94% higher than in matched controls but the difference did not reach statistical significance (p = 0.065).
Corrected ADRA2A and ADRA2C mRNA expression in DLPFC of schizophrenia subjects (S, n = 19), antipsychotic-free (AP-free, n = 10) and antipsychotic-treated (AP-treated, n = 9) subjects, and their respective matched controls (C). Data are shown as mean ± SEM. Statistical significance is denoted by *p < 0.05, unpaired two-tailed Student’s t-test.
In schizophrenia subjects ADRA2C mRNA expression was significantly higher than in matched controls (Δ = +53%, n = 17, p = 0.016, Fig. 1B). Analysis of schizophrenia subjects according to the presence or absence of antipsychotic treatment, revealed that ADRA2C mRNA expression was non-significantly enhanced over that in controls in both AP-free (Δ = +53%, n = 9, p = 0.136, Fig. 1B) and AP-treated schizophrenia subjects (Δ = +54%, n = 8, p = 0.088, Fig. 1B).
ADRA2A and ADRA2C mRNA expression in schizophrenia subjects could also be influenced by the fact that most schizophrenia subjects in the study were suicide victims (13 out of 19). In order to evaluate this possibility, we analyzed ADRA2A and ADRA2C mRNA expression in suicide victims with an antemortem diagnosis of major depression. Compared to matched controls, neither ADRA2A nor ADRA2C mRNA expression was significantly altered (Supplementary Fig. 5).
Effect of antipsychotic treatment on Adra2a and Adra2c mRNA expression in rat brain cortex
Considering the specific ADRA2A mRNA increase observed in AP-treated schizophrenia subjects, we aimed to evaluate the effect of acute and chronic antipsychotic treatment in rat brain cortex Adra2a and Adra2c mRNA expression. As observed in Fig. 2, Adra2a mRNA expression was modulated by neither acute nor chronic treatment with atypical (risperidone and clozapine) or typical antipsychotics (haloperidol). However, compared to saline-treated rats Adra2c mRNA expression was significantly increased in acute (Δ = +154% vs saline, p < 0.0001, Fig. 2A) and non-significantly increased in chronically clozapine-treated rats (Δ = +45% vs saline, p = 0.177, Fig. 2B).
Corrected Adra2a and Adra2c mRNA expression in brain cortex of rats treated acutely (A) and chronically (B) with saline (SAL), risperidone (RIS), clozapine (CLZ), and haloperidol (HAL). Data are shown as mean ± SEM of 3−6 animals. Statistical analysis was performed by one-way ANOVA test followed by Tukey’s multiple comparison test. Statistical significance is denoted by ****p < 0.0001.
Demographic and methodological variables contributing to histone PTMs at ADRA2A and ADRA2C promoters in human DLPFC
The effect of demographic and methodological variables on histone PTMs at ADRA2A and ADRA2C promoters was individually analyzed. Significant models emerged for ADRA2A promoter-associated H3K27me3 [F(1,17) = 5.874, p = 0.027], H3ac [F(1,17) = 5.21, p = 0.036] and H4K5ac [F(1,17) = 5.194, p = 0.036]. H3K27me3 and H3ac at ADRA2A promoter were significantly influenced by sex of the subjects (β = 0.507, p = 0.027 and β = 0.484, p = 0.036, respectively), being higher in females than in males (Δ = +113% and Δ = +170%, respectively). H4K5ac at ADRA2A promoter gene was positively influenced by ST (β = 0.484, p = 0.036).
In the case of histone PTMs at ADRA2C promoter, significant models emerged for H3K27me3 [F(1,17) = 8.846, p = 0.009], H3K27ac [F(1,17) = 5.318, p = 0.034] and H4K16ac [F(1,17) = 5.561, p = 0.031]. H3K27me3 at ADRA2C promoter gene was influenced by sex of the subjects being higher in females than in males (β = 0.585, p = 0.009, Δ = +138%). At ADRA2C promoter H3K27ac was significantly influenced by PMD of samples (β=0.488, p = 0.034) whereas H4K16ac was influenced by ST (β = 0.496, p = 0.031). The effect of variables significantly contributing to experimental data is depicted in Supplementary Fig. 4.
Histone PTMs at ADRA2A and ADRA2C promoters in postmortem human DLPFC of schizophrenia subjects
To evaluate the possible epigenetic modulation of altered ADRA2A and ADRA2C mRNA expression in schizophrenia subjects, histone modification signature comprised of histone methylations—permissive H3K4me3 and repressive H3K27me3—and histone acetylations—H3ac, H3K9ac, H3K27ac, H4K5ac, and H4K16ac—was evaluated at both ADRA2A and ADRA2C promoter regions.
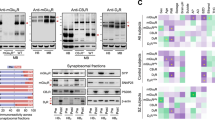
For ADRA2A promoter region, in schizophrenia subjects, both permissive H3K4me3 (Δ=+105%, p = 0.021, Fig. 3A) and repressive H3K27me3 (Δ = +86%, p = 0.01, Fig. 3B) were increased compared to matched controls. Division of schizophrenia subjects by presence or absence of blood antipsychotics, revealed that H3K27me3 at ADRA2A promoter was significantly increased in AP-treated schizophrenia subjects (Δ = +159% vs matched controls, p = 0.006, Fig. 3B). Although non-significantly, H3K4me3 at ADRA2A promoter was also increased in AP-treated schizophrenia subjects (Δ = +135% vs matched controls, p = 0.072, Fig. 3A). Separate analysis of AP-free and AP-treated schizophrenia subjects also revealed the selective increase of H4K16ac in AP-treated schizophrenia subjects (D = +82% increase, p = 0.029, Fig. 3G). The rest of the studied histone PTMs were not significantly different between the compared groups.
Histone 3 methylation [H3K4me3 (A) and H3K27me3 (B)] and acetylation [H3ac (C), H3K9ac (D), H3K27ac (E)] and histone 4 acetylation [H4K5ac (F) and H4K16ac (G)] at ADRA2A promoter region. Data are shown as mean ± SEM. Statistical significance is denoted by *p < 0.05, **p < 0.01, paired two-tailed Student’s t-test. C control subjects, S schizophrenia subjects, AP-free antipsychotic-free, AP-treated antipsychotic-treated.
The study of histone PTMs at ADRA2C promoter region in schizophrenia subjects showed a significant increase of H3K27me3 (Δ = +52%, p = 0.046, Fig. 4B), H3K9ac (Δ = +63%, p = 0.007, Fig. 4D) and H4K5ac (Δ = +55%, p = 0.027, Fig. 4F). Separate analysis of AP-free and AP-treated subjects showed that compared to matched controls, H3K9ac was increased in AP-free subjects (Δ = +67%, p = 0.043, Fig. 4D), whereas H4K5ac was increased in AP-treated subjects (Δ = +103%, p = 0.048, Fig. 4F). The rest of the studied histone PTMs were not significantly different between the compared groups.
Histone 3 methylation [H3K4me3 (A) and H3K27me3 (B)] and acetylation [H3ac (C), H3K9ac (D), H3K27ac (E)] and histone 4 acetylation [H4K5ac (F) and H4K16ac (G)] at ADRA2C promoter region. Data are shown as mean ± SEM. Statistical significance is denoted by *p < 0.05, **p < 0.01, paired two-tailed Student’s t-test. C control subjects, S schizophrenia subjects, AP-free antipsychotic-free, AP-treated antipsychotic-treated.
In addition, none of the studied histone PTMs was found to be different between schizophrenia and control subjects at promoter region of reference gene GAPDH (Supplementary Fig. 6).
Discussion
In this study, we observed a differential ADRA2A and ADRA2C mRNA expression in DLPFC of schizophrenia subjects. ADRA2A mRNA expression was selectively upregulated in AP-treated subjects, whereas ADRA2C mRNA expression was enhanced in schizophrenia subjects regardless of the presence or absence of antipsychotics in blood at the time of death.
The selective upregulation of ADRA2A mRNA expression in those schizophrenia subjects that showed detectable antipsychotic blood levels is in line with previous reports indicating a higher α2A-adrenoceptor protein expression in synaptosomal and postsynaptic membranes of the same AP-treated schizophrenia subjects [9]. In human PFC, α2A-adrenoceptor represents the main α2-adrenoceptor subtype [34,35,36]. Electron microscopy studies have shown α2A-adrenoceptors to be prevalent in neurons, showing presynaptic and postsynaptic location [37]. Subcellular fractionation of human DLPFC followed by immunolabeling showed the predominant postsynaptic location of α2A-adrenoceptors (95%) while only the remaining 5% is in the presynapse [8]. In this sense, due to mRNA predominant somatic location, and although certain ADRA2A mRNA expression in glial cells cannot be ruled out [37,38,39], we believe that most of the mRNA expression detected in our study may belong to postsynaptic neuronal mRNA. Moreover, present observations suggest that ADRA2A mRNA upregulation in AP-treated schizophrenia subjects might be the driving force in the upregulated postsynaptic α2A-adrenoceptor protein expression observed in the same subjects [9]. Postsynaptic neuronal expression of α2-adrenoceptors has been demonstrated on GABAergic interneurons [40] and on glutamatergic pyramidal neurons [41] of rat and rhesus monkey frontal cortex. Yet, the relevance of the enhanced mRNA and protein expression of α2A-adrenoceptors in AP-treated schizophrenia subjects is unknown. In DLPFC, postsynaptically located α2A-adrenoceptors play a relevant role in cognitive processes. From its postsynaptic location, α2A-adrenoceptors control noradrenergic tone on layer III pyramidal cells and upon stimulation by selective agonists, α2A-adrenoceptors enhance DLPFC-dependent working memory [42, 43]. Whether enhanced α2A-adrenoceptors in DLPFC of AP-treated schizophrenia subjects contributed to improve cognitive outcomes in these subjects is unknown.
By contrast, ADRA2C mRNA expression was upregulated in postmortem brain of schizophrenia subjects regardless of the presence of antipsychotics in blood. Evaluation of α2C-adrenoceptor protein expression in the same subjects revealed that α2C-adrenoceptor density in synaptosomal subcellular fractions was unaltered regardless of antipsychotic drug presence [9]. However, mRNA and protein expression do not necessarily need to be regulated in parallel [44] and the increase in ADRA2C mRNA expression in schizophrenia deserves further investigation. These results may suggest that ADRA2C upregulation would be a feature of schizophrenia pathology as opposed to α2A-adrenoceptor mRNA and protein expression selective upregulation in AP-treated schizophrenia subjects but other factors should also be considered. In most of the AP-treated schizophrenia subjects of this study, blood toxicology detected the presence of atypical antipsychotic drugs (Supplementary Table 1). In this sense, atypical antipsychotic drugs such as clozapine and risperidone show α2-adrenoceptor antagonistic properties with a preference for α2C- over α2A-adrenoceptor [5, 45, 46]. In order to study if α2-adrenoceptor antagonism by antipsychotic drugs could induce ADRA2A and ADRA2C mRNA expression, we conducted experiments in acutely and chronically AP-treated male rat brain cortex. Our results showed that Adra2c mRNA expression was upregulated in rats treated with either acute or chronic clozapine whereas Adra2a mRNA expression was unaltered. Although inclusion of female rats might have improved data validity, obtained results may be interpreted by pharmacological mechanisms. The selective upregulation of Adra2c mRNA expression triggered by acute and chronic clozapine but not by risperidone might relate to α2-adrenoceptor occupancy. In rodents, systemic administration of 5 mg/kg of clozapine occupies 65% of α2A- and 95% of α2C-adrenoceptors in brain [47], whereas 0.5 mg/kg risperidone only occupies 12% of α2A- and 19% of α2C-adrenoceptors [48]. Thus, increased ADRA2C mRNA expression in schizophrenia might be related to α2C-adrenoceptor antagonism by some atypical antipsychotic drugs. However, ADRA2C mRNA expression was non-significantly enhanced over control values in both AP-free and AP-treated schizophrenia subjects. It is worth mentioning that toxicological analysis in blood samples of AP-free schizophrenia subjects indicates that antipsychotics had not been present in an antemortem period of days but it does not discard previous antipsychotic usage by these subjects. Thus, modulation of ADRA2C mRNA expression by past antipsychotic drug usage in AP-free subjects might also be considered. On the other hand, the results in both acute and chronically-treated rats failed to explain the upregulation of ADRA2A mRNA expression in AP-treated schizophrenia subjects. Whether this lack of consistency is due to differences among species or due to a specific antipsychotic-induced modulation of ADRA2A mRNA expression in brains of schizophrenia subjects is unknown. An alternative approach would have been to study ADRA2A and ADRA2C mRNA expression in human brain of subjects treated with antipsychotic drugs but without schizophrenia diagnose. However, the limited availability of that kind of samples would have hindered the study. Thus, the hypothesis that antipsychotic drug effects on schizophrenia brains might differ from their effect on non-pathological brains points to the need of relevant animal models of schizophrenia. Actually, antipsychotic drugs have already shown differential effects on schizophrenia animal models compared to control animals [49].
As previously mentioned, another important aspect is that 13 of 19 schizophrenia subjects in the mRNA study died by suicide, with a similar distribution in AP-free and AP-treated subgroups. α2-adrenoceptors have been reported to be increased in postmortem brain of suicide victims [50] with vast literature reporting upregulated α2-adrenoceptors in brains of suicide victims with an antemortem diagnosis of major depression (see [51,52,53,54] and references within). However, information on α2A and α2C-adrenoceptor subtype delineation is still lacking. Thus, we aimed to evaluate if enhanced ADRA2C mRNA expression in these schizophrenia subjects could be related to suicide completion by using a cohort of 13 depressed suicide victims. The results showed that neither ADRA2A nor ADRA2C mRNA were altered in depressed suicide victims as opposed to results in the schizophrenia cohort. Therefore, modulation of ADRA2C mRNA expression due to suicidal completion does not seem plausible.
Epigenetics may be particularly relevant for understanding schizophrenia [17]. Besides literature on DNA methylation studies in schizophrenia and the growing number of studies on miRNA [55], several findings indicate that histone PTMs may play a role in the etiology and pathophysiology of schizophrenia [26,27,28,29]. Thus, the association of several histone H3 and histone H4 PTMs at ADRA2A and ADRA2C promoter regions was studied. The results show specific histone PTMs at ADRA2A and ADRA2C promoters in schizophrenia with selective mechanisms in AP-free and AP-treated subjects. To our knowledge, this is the first time that histone PTMs at ADRA2A and ADRA2C are reported.
Regarding ADRA2A epigenetic regulation, both ADRA2A promoter-associated H3K4me3 and H3K27me3 were increased in schizophrenia subjects. The relevance of histone methylation processes was already put forward in the GWAS study from the Psychiatric Genomics Consortium [56], whereby histone methylation showed the strongest association with psychiatric disorders. Moreover, H3K27 methyltransferase EZH1 expression has been reported to be increased in PFC of schizophrenia subjects [18]. With our methodology, we cannot assure that regulation of ADRA2A promoter by H3K4me3 and H3K27me3 occur at the same cell. Actually, as earlier discussed, ADRA2A mRNA expression in brain cortex can be ascribed to GABAergic interneurons, glutamatergic pyramidal neurons and astrocytes [38, 40, 41]. However, levels of H3K4me3 and H3K27me3 at ADRA2A promoter showed a positive correlation in human brain (Supplementary Fig. 7) suggesting that these two marks could be concomitantly upregulated in schizophrenia. This parallel increase in H3K4me3 and H3K27me3 marks might be conflicting in the view of their respective permissive and repressive transcriptional influence. Nevertheless, increased H3K4me3 and H3K27me3 at ADRA2A promoter region can be explained in the light of bivalent chromatin. Bivalent chromatin refers to those gene promoter regions that show both H3K4me3 and H3K27me3 and thus have characteristics of both active and repressive chromatin [57]. This dual marking keeps genes silent but poised for prompt activation if triggered by certain stimuli. Bivalent chromatin is important in early development [57] but has also been reported in physiological and pathological processes such as aging [58], cancer [59], and autism [60]. Bivalently marked domains are often associated to high-CpG-content promoters [61]. In this sense, estimated CpG island content at ADRA2A and ADRA2C promoters is 317 and 341 while it is 123 for GAPDH (accessed in UCSC genome browser [62]). Moreover, an annotated list of bivalent chromatin regions in human embrionary stem cells identified ADRA2A and ADRA2C promoters as bivalent domains based on overlapping H3K4me3 and H3K27me3 peaks [63]. Thus, enriched bivalency at ADRA2A promoter depicted by both H3K4me3 and H3K27me3 enhancement in DLPFC of schizophrenia subjects would render ADRA2A gene poised for transcriptional action. Upon the right stimulus, this state might be easily activated and lead to increased ADRA2A mRNA expression in the cell. This enhanced bivalency would mean that schizophrenia subjects show an epigenetic predisposition for ADRA2A mRNA regulation, which might be a specific feature of schizophrenia. Alternatively, as previously discussed, H3K4me3 and H3K27me3 marks at ADRA2A promoter might also be due to past effect of antipsychotic treatment. Actually, at ADRA2A promoter of AP-treated schizophrenia subjects, H3K4me3 and H3K27me3 were both increased over control values, the difference being statistically significant for H3K27me3.
Another important observation was that in AP-treated schizophrenia subjects, permissive H4K16ac at ADRA2A promoter was significantly higher than in matched controls whereas it remained unaltered in AP-free schizophrenia subjects. Increased H4K16ac at ADRA2A promoter might be one of the mechanisms tipping the scales in favor of a higher ADRA2A mRNA expression in AP-treated schizophrenia subjects. Indeed, among histone H4 PTMs, H4K16ac shows greater individual effect on gene expression than counterparts H4K5, K8, and K12, at least for a subset of genes [64].
Regarding ADRA2C epigenetic regulation, present results show that in DLPFC of schizophrenia subjects enhanced repressive H3K27me3, and permissive H3K9ac and H4K5ac coexist at ADRA2C promoter region. This pattern of acetylation at histone H3 and H4 together with the repressive methylation at histone H3 suggests that epigenetic modulation of transcriptional activity of ADRA2C is also tightly regulated. The histone code depicted by the joint increase in the permissive PTMs H3K9ac and H4K5ac might determine the transcriptional activation of ADRA2C gene [65], although precise histone PTM functions still remain unknown [66]. Analysis of schizophrenia subjects based on antipsychotic drug presence revealed the significant upregulation of H3K9ac and H4K5ac in AP-free and AP-treated schizophrenia subjects, respectively. These results may suggest a selective influence of antipsychotic treatment on H4K5ac at ADRA2C promoter. However, we acknowledge that the lack of significance in certain subgroups could be due to the human variability of the samples and the reduction of the sample size when dividing the schizophrenia group regarding the presence of antipsychotics in blood.
Modulation of epigenetic mechanisms by antipsychotic treatment is starting to be evaluated. The majority of published articles have evaluated antipsychotic influence on DNA methylation at neurotransmitter-associated candidate genes or genome-wide level [67]. However, data about the effect of antipsychotic drug treatment on histone PTM is scarce. Most relevant findings concern the atypical antipsychotic-induced upregulation of HDAC2, which has been related to histone hypoacetylation at GRM2 promoter [27, 68]. Further evidence on clozapine role in epigenetics is provided by the enhanced expression of HMT mixed-lineage leukemia 1 (Mll1) by chronic clozapine [28]. Together with present results, these studies highlight the need for further investigation on antipsychotic drug influence on epigenetic mechanisms.
Studies in postmortem human brain are also complicated by the effect of confounding demographic and methodological factors [69, 70]. According to our results, histone PTMs at ADRA2A and ADRA2C promoters are influenced by sex, ST, and PMD of the samples. Actually, the effect of sex on epigenetics has been previously described [71] with evidence for HDAC and HMT sex-specific expression [18, 28, 72]. In this sense, our study found that all histone PTMs affected by sex of the subjects showed increased values for females. In any case, the effect of these factors was override by careful matching of schizophrenia and control subjects according to sex, age, PMD, and ST.
In summary, the current study shows ADRA2A and ADRA2C differential regulation in schizophrenia. The unique upregulation of ADRA2A mRNA expression in AP-treated schizophrenia subjects but not in AP-treated rats is likely an outcome of epigenetic predisposition depicted by enhanced bivalent chromatin at ADRA2A promoter. On the other hand, increased ADRA2C mRNA expression in schizophrenia might be due to the pathophysiology of the disease or to the effect of antipsychotic treatment. Also for ADRA2C, histone acetylation and methylation is specifically upregulated at promoter regions. In the light of current and past results [9], the suggested antipsychotic effect potentiation by α2A-adrenoceptor agonists or α2C-adrenoceptor antagonists deserves further study [5]. A final warning due to the specificity of histone PTMs at different genes is that the impact of coadjuvant antipsychotic and HDAC inhibitors [31] at relevant gene clusters should also be carefully studied.
References
McCutcheon RA, Reis Marques T, Howes OD. Schizophrenia—An overview. JAMA Psychiatry. 2020;77:201–10.
Maletic V, Eramo A, Gwin K, Offord SJ & Duffy RA. The role of norepinephrine and its α-adrenergic receptors in the pathophysiology and treatment of major depressive disorder and schizophrenia: A systematic review. Front Psychiatry. 2017. https://doi.org/10.3389/fpsyt.2017.00042.
Uys MM, Shahid M, Harvey BH. Therapeutic potential of selectively targeting the α2C-adrenoceptor in cognition, depression, and schizophrenia—new developments and future perspective. Front Psychiatry. 2017. https://doi.org/10.3389/fpsyt.2017.00144.
Betti AH, Antonio CB, Herzfeldt V, Pitta MGDR, Pitta IDR, do Rego JL, et al. PT-31, a putative α2-adrenoceptor agonist, is effective in schizophrenia cognitive symptoms in mice. Behav Pharm. 2019;30:574–87.
Brosda J, Jantschak F, Pertz HH. α2-Adrenoceptors are targets for antipsychotic drugs. Psychopharmacology. 2014;231:801–12.
Arnsten AFT. Catecholamine influences on dorsolateral prefrontal cortical networks. Biol Psychiatry. 2011;69:e89–99.
Arnsten AFT, Wang M. Targeting prefrontal cortical systems for drug development: Potential therapies for cognitive disorders. Annu Rev Pharmacol Toxicol. 2016;56:339–60.
Erdozain AM, Brocos-Mosquera I, Gabilondo AM, Meana JJ, Callado LF. Differential α2A - and α2C-adrenoceptor protein expression in presynaptic and postsynaptic density fractions of postmortem human prefrontal cortex. J Psychopharmacol. 2019;33:244–9.
Brocos-Mosquera I, Gabilondo AM, Díez-Alarcia R, Muguruza C, Erdozain AM, Meana JJ, Callado LF. α2A- and α2C-adrenoceptor expression and functionality in postmortem prefrontal cortex of schizophrenia subjects. Eur Neuropsychopharmacol. 2021;52:3–11.
Prata DP, Costa-Neves B, Cosme G, Vassos E. Unravelling the genetic basis of schizophrenia and bipolar disorder with GWAS: A systematic review. J Psychiatr Res. 2019;114:178–207.
Schizophrenia Working Group of the Psychiatric Genomics Consortium. Biological insights from 108 schizophrenia-associated genetic loci. Nature. 2014;511:421–7.
Bolonna AA, Arranz MJ, Munro J, Osborne S, Petouni M, Martinez M, et al. No influence of adrenergic receptor polymorphisms on schizophrenia and antipsychotic response. Neurosci Lett. 2000;280:65–68.
Tsai SJ, Wang YC, Yu Younger WY, Lin CH, Yang KH, Hong CJ. Association analysis of polymorphism in the promoter region of the alpha2a-adrenoceptor gene with schizophrenia and clozapine response. Schizophr Res. 2001;49:53–58.
Clark DA, Mata I, Kerwin RW, Munro J, Arranz MJ. No association between ADRA2A polymorphisms and schizophrenia. Am J Med Genet Part B Neuropsychiatr Genet. 2007;144:341–3.
Lochman J, Plesník J, Janout V, Povová J, Míšek I, Dvořáková D, et al. Interactive effect of MTHFR and ADRA2A gene polymorphisms on pathogenesis of schizophrenia. Neuroendocrinol Lett. 2013;34:792–7.
Peedicayil J, Grayson DR. An epigenetic basis for an omnigenic model of psychiatric disorders. J Theor Biol. 2018;443:52–55.
Richetto J, Meyer U. Epigenetic modifications in schizophrenia and related disorders: Molecular scars of environmental exposures and source of phenotypic variability. Biol Psychiatry. 2020;89:215–26.
Johnstone AL, O’Reilly JJ, Patel AJ, Guo Z, Andrade NS, Magistri M, et al. EZH1 is an antipsychotic-sensitive epigenetic modulator of social and motivational behavior that is dysregulated in schizophrenia. Neurobiol Dis. 2018;119:149–58.
Chase KA, Rosen C, Rubin LH, Feiner B, Bodapati AS, Gin H, et al. Evidence of a sex-dependent restrictive epigenome in schizophrenia. J Psychiatr Res. 2015;65:87–94.
Chase KA, Gavin DP, Guidotti A, Sharma RP. Histone methylation at H3K9: Evidence for a restrictive epigenome in schizophrenia. Schizophr Res. 2013;149:15–20.
Bahari-Javan S, Varbanov H, Halder R, Benito E, Kaurani L, Burkhardt S, et al. HDAC1 links early life stress to schizophrenia-like phenotypes. Proc Natl Acad Sci USA. 2017;114:E4686–E4694.
Sharma RP, Grayson DR, Gavin DP. Histone deactylase 1 expression is increased in the prefrontal cortex of schizophrenia subjects: Analysis of the National Brain Databank microarray collection. Schizophr Res. 2008;98:111–7.
Schroeder FA, Gilbert TM, Feng N, Taillon BD, Volkow ND, Innis RB, et al. Expression of HDAC2 but Not HDAC1 transcript is reduced in dorsolateral prefrontal cortex of patients with schizophrenia. ACS Chem Neurosci. 2017;8:662–8.
Gilbert TM, Zürcher NR, Wu CJ, Bhanot A, Hightower BG, Kim M, et al. PET neuroimaging reveals histone deacetylase dysregulation in schizophrenia. J Clin Invest. 2019;129:364–72.
Girdhar K, Hoffman GE, Jiang Y, Brown L, Kundakovic M, Hauberg ME, et al. Cell-specific histone modification maps in the human frontal lobe link schizophrenia risk to the neuronal epigenome. Nat Neurosci. 2018;21:1126–36.
Tang B, Dean B, Thomas EA. Disease- and age-related changes in histone acetylation at gene promoters in psychiatric disorders. Transl Psychiatry. 2011;1:e64.
Kurita M, Holloway T, García-Bea A, Kozlenkov A, Friedman AK, Moreno JL, et al. HDAC2 regulates atypical antipsychotic responses through the modulation of mGlu2 promoter activity. Nat Neurosci. 2012;15:1245–54.
Huang H-S, Matevossian A, Whittle C, Kim SY, Schumacher A, Baker SP, et al. Prefrontal dysfunction in schizophrenia involves mixed-lineage leukemia 1-regulated histone methylation at GABAergic gene promoters. J Neurosci. 2007;27:11254–62.
Gusev FE, Reshetov DA, Mitchell AC, Andreeva TV, Dincer A, Grigorenko AP, et al. Chromatin profiling of cortical neurons identifies individual epigenetic signatures in schizophrenia. Transl Psychiatry. 2019;9:256.
Sharma RP, Rosen C, Kartan S, Guidotti A, Costa E, Grayson DR, et al. Valproic acid and chromatin remodeling in schizophrenia and bipolar disorder: Preliminary results from a clinical population. Schizophr Res. 2006;88:227–31.
Wang Y, Xia J, Helfer B, Li C, Leucht S. Valproate for schizophrenia. Cochrane Database Syst Rev. 2016;11:CD004028.
García-Bea A, Miranda-Azpiazu P, Muguruza C, Marmolejo-Martinez-Artesero S, Díez-Alarcia R, Gabilondo AM, et al. Serotonin 5-HT2A receptor expression and functionality in postmortem frontal cortex of subjects with schizophrenia: Selective biased agonism via Gαi1-proteins. Eur Neuropsychopharmacol. 2019;29:1453–63.
Clark RA, Shoaib M, Hewitt KN, Stanford SC, Bate ST. A comparison of InVivoStat with other statistical software packages for analysis of data generated from animal experiments. J Psychopharmacol. 2012;26:1136–42.
Ordway GA, Jaconetta SM, Halaris AE. Characterization of subtypes of alpha-2 adrenoceptors in the human brain. J Pharmacol Exp Ther. 1993;264:967–76.
Grijalba B, Callado LF, Javier Meana J, García-Sevilla JA, Pazos A. α2-Adrenoceptor subtypes in the human brain: A pharmacological delineation of [3H]RX-821002 binding to membranes and tissue sections. Eur J Pharmacol. 1996;310:83–93.
Sastre M, García‐Sevilla JA. α2‐Adrenoceptor subtypes identified by [3H]RX821002 binding in the human brain: The agonist Guanoxabenz does not discriminate different forms of the predominant α2A subtype. J Neurochem. 1994;63:1077–85.
Aoki C, Venkatesan C, Go CG, Forman R, Kurose H. Cellular and subcellular sites for noradrenergic action in the monkey dorsolateral prefrontal cortex as revealed by the immunocytochemical localization of noradrenergic receptors and axons. Cereb Cortex. 1998;8:269–77.
Hertz L, Lovatt D, Goldman SA, Nedergaard M. Adrenoceptors in brain: Cellular gene expression and effects on astrocytic metabolism and [Ca2+]i. Neurochem Int. 2010;57:411–20.
Glass MJ, Huang J, Aicher SA, Milner TA, Pickel VM. Subcellular localization of α-2A-adrenergic receptors in the rat medial nucleus tractus solitarius: Regional targeting and relationship with catecholamine neurons. J Comp Neurol. 2001;433:193–207.
Modirrousta M, Mainville L, Jones BE. Gabaergic neurons with α2-adrenergic receptors in basal forebrain and preoptic area express c-Fos during sleep. Neuroscience. 2004;129:803–10.
Wang M, Ramos BP, Paspalas CD, Shu Y, Simen A, Duque A, et al. α2A-Adrenoceptors strengthen working memory networks by inhibiting cAMP-HCN channel signaling in prefrontal cortex. Cell. 2007;129:397–410.
Arnsten AF, Goldman-Rakic PS. Alpha 2-adrenergic mechanisms in prefrontal cortex associated with cognitive decline in aged nonhuman primates. Science. 1985;230:1273–6.
Arnsten AFT, Wang MJ, Paspalas CD. Neuromodulation of thought: Flexibilities and vulnerabilities in prefrontal cortical network synapses. Neuron. 2012;76:223–39.
Liu Y, Beyer A, Aebersold R. On the dependency of cellular protein levels on mRNA abundance. Cell. 2016;165:535–50.
Schotte A, Janssen PF, Gommeren W, Luyten WH, Van Gompel P, Lesage AS, et al. Risperidone compared with new and reference antipsychotic drugs: In vitro and in vivo receptor binding. Psychopharmacology. 1996;124:57–73.
Kalkman HO, Loetscher E. α2C-adrenoceptor blockade by clozapine and other antipsychotic drugs. Eur J Pharmacol. 2003;462:33–40.
Marcus MM, Jardemark KE, Wadenberg M-L, Langlois X, Hertel P, Svensson TH. Combined α2 and D2/3 receptor blockade enhances cortical glutamatergic transmission and reverses cognitive impairment in the rat. Int J Neuropsychopharmacol. 2005;8:315–27.
Marcus MM, Wiker C, Frånberg O, Konradsson-Geuken A, Langlois X, Jardemark K, et al. Adjunctive α2-adrenoceptor blockade enhances the antipsychotic-like effect of risperidone and facilitates cortical dopaminergic and glutamatergic, NMDA receptor-mediated transmission. Int J Neuropsychopharmacol. 2010;13:891–903.
Meyer U, Knuesel I, Nyffeler M, Feldon J. Chronic clozapine treatment improves prenatal infection-induced working memory deficits without influencing adult hippocampal neurogenesis. Psychopharmacology. 2010;208:531–43.
Pandey GN, Dwivedi Y. Noradrenergic function in suicide. Arch Suicide Res. 2007;11:235–46.
Callado LF, Meana JJ, Grijalba B, Pazos A, Sastre M, García-Sevilla JA. Selective increase of α2A-adrenoceptor agonist binding sites in brains of depressed suicide victims. J Neurochem. 1998;70:1114–23.
Meana JJ, Barturen F, García-Sevilla JA. α2-Adrenoceptors in the brain of suicide victims: Increased receptor density associated with major depression. Biol Psychiatry. 1992;31:471–90.
Rivero G, Gabilondo AM, García-Sevilla JA, La Harpe R, Callado LF, Meana JJ. Increased α2- and β1-adrenoceptor densities in postmortem brain of subjects with depression: Differential effect of antidepressant treatment. J Affect Disord. 2014;167:343–50.
Ordway GA, Schenk J, Stockmeier CA, May W, Klimek V. Elevated agonist binding to α2-adrenoceptors in the locus coeruleus in major depression. Biol Psychiatry. 2003;53:315–23.
Smigielski L, Jagannath V, Rössler W, Walitza S, Grünblatt E. Epigenetic mechanisms in schizophrenia and other psychotic disorders: A systematic review of empirical human findings. Mol Psychiatry. 2020;25:1718–48.
Network and Pathway Analysis Subgroup of Psychiatric Genomics Consortium. Psychiatric genome-wide association study analyses implicate neuronal, immune, and histone pathways. Nat Neurosci. 2015;18:199–209.
Bernstein BE, Mikkelsen TS, Xie X, Kamal M, Huebert DJ, Cuff J, et al. A bivalent chromatin structure marks key developmental genes in embryonic stem cells. Cell. 2006;125:315–26.
Rakyan VK, Down TA, Maslau S, Andrew T, Yang T-P, Beyan H, et al. Human aging-associated DNA hypermethylation occurs preferentially at bivalent chromatin domains. Genome Res. 2010;20:434–9.
Ohm JE, McGarvey KM, Yu X, Cheng L, Schuebel KE, Cope L, et al. A stem cell-like chromatin pattern may predispose tumor suppressor genes to DNA hypermethylation and heritable silencing. Nat Genet. 2007;39:237–42.
Corley MJ, Vargas-Maya N, Pang APS, Lum-Jones A, Li D, Khadka V, et al. Epigenetic delay in the neurodevelopmental trajectory of DNA methylation states in autism spectrum disorders. Front Genet. 2019;10:907.
Zhou VW, Goren A, Bernstein BE. Charting histone modifications and the functional organization of mammalian genomes. Nat Rev Genet. 2011;12:7–18.
UCSC. UCSC Genome Browser https://genome.ucsc.edu/. 2021.
Court F, Arnaud P. An annotated list of bivalent chromatin regions in human ES cells: A new tool for cancer epigenetic research. Oncotarget. 2017;8:4110–24.
Dion MF, Altschuler SJ, Wu LF, Rando OJ. Genomic characterization reveals a simple histone H4 acetylation code. Proc Natl Acad Sci USA. 2005;102:5501–6.
Villaseñor R, Baubec T. Regulatory mechanisms governing chromatin organization and function. Curr Opin Cell Biol. 2021;70:10–17.
Morgan MAJ, Shilatifard A. Reevaluating the roles of histone-modifying enzymes and their associated chromatin modifications in transcriptional regulation. Nat Genet. 2020;52:1271–81.
Ovenden ES, McGregor NW, Emsley RA, Warnich L. DNA methylation and antipsychotic treatment mechanisms in schizophrenia: Progress and future directions. Prog Neuro-Psychopharmacol Biol Psychiatry. 2018;81:38–49.
Ibi D, de la Fuente Revenga M, Kezunovic N, Muguruza C, Saunders JM, Gaitonde SA. et al. Antipsychotic-induced Hdac2 transcription via NF-κB leads to synaptic and cognitive side effects. Nat Neurosci. 2017;20:1247–59.
Nagy C, Maheu M, Lopez JP, Vaillancourt K, Cruceanu C, Gross JA, et al. Effects of postmortem interval on biomolecule integrity in the brain. J Neuropathol Exp Neurol. 2015;74:459–69.
Preece P, Cairns NJ. Quantifying mRNA in postmortem human brain: Influence of gender, age at death, postmortem interval, brain pH, agonal state, and inter-lobe mRNA variance. Mol Brain Res. 2003;118:60–71.
Singh G, Singh V, Schneider JS. Post-translational histone modifications and their interaction with sex influence normal brain development and elaboration of neuropsychiatric disorders. Biochim Biophys Acta Mol Basis Dis. 2019;1865:1968–81.
Gilbert TM, Zürcher NR, Catanese MC, Tseng CJ, Di Biase MA, Lyall AE, et al. Neuroepigenetic signatures of age and sex in the living human brain. Nat Commun. 2019;10:2945.
Acknowledgements
This work was supported by Spanish MINECO (grant SAF2013-48586-R) and Basque Government (grant IT1211/19). The authors would like to thank the staff members of the Basque Institute of Legal Medicine for their cooperation in the study.
Author information
Authors and Affiliations
Contributions
BM, JJM, and LFC collaborated in obtaining the sample collection from postmortem human brains and the information about demographic, clinical, and toxicological data of these subjects IB-M, PM-A, CM, VC-M, and GR performed the experiments. IB-M, CM, and GR performed data analysis. IB-M and GR produced the figures and tables. JJM, LFC, and GR conceptualized the project. IB-M, CM, JJM, LFC, and GR managed literature searches. GR wrote the manuscript, and all authors contributed to and edited the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Brocos-Mosquera, I., Miranda-Azpiazu, P., Muguruza, C. et al. Differential brain ADRA2A and ADRA2C gene expression and epigenetic regulation in schizophrenia. Effect of antipsychotic drug treatment. Transl Psychiatry 11, 643 (2021). https://doi.org/10.1038/s41398-021-01762-4
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41398-021-01762-4
This article is cited by
-
Effect of antipsychotic drugs on group II metabotropic glutamate receptor expression and epigenetic control in postmortem brains of schizophrenia subjects
Translational Psychiatry (2024)
-
Preliminary study on toxicological mechanism of golden cuttlefish (Sepia esculenta) larvae exposed to cd
BMC Genomics (2023)
-
A preclinical secondary pharmacology resource illuminates target-adverse drug reaction associations of marketed drugs
Nature Communications (2023)
-
Identification of potentially functional modules and diagnostic genes related to amyotrophic lateral sclerosis based on the WGCNA and LASSO algorithms
Scientific Reports (2022)