Abstract
Study design
Descriptive study.
Objectives
To describe patient handling at injury site, number of healthcare centre transfers to reach tertiary trauma centre, modes of transportation, and time from injury to reaching tertiary trauma centres among individuals with acute traumatic spinal cord injury (tSCI).
Setting
Acute SCI rehabilitation centre, Nepal.
Methods
All individuals with new tSCI admitted for rehabilitation over period of 1 year were eligible for enrolment. Following written, informed consent, enroled individuals participated in structured one-on-one interview. Data collected included demographics, injury details, pre-hospital handling techniques, and transportation specifics to tertiary trauma centre.
Results
In total, 211 individuals were enroled in the study. Eight (4%) individuals were assisted by first responders or traffic police, with majority (n = 203, 96%) assisted by untrained individuals. One was transferred from injury site using spinal motion restriction measures. Half were transported exclusively by ambulance while others used combinations of transportation. Six (3.4%) individuals were cared for by trained medical person during transport. Half required two or more hospital transfers prior to reaching a tertiary trauma centre. In total, 98 individuals required >24 h to reach the tertiary trauma centre.
Conclusions
Individuals sustaining a tSCI in Nepal often experience improper handling, multiple hospital transfers, and prolonged time to reach tertiary trauma centres following acute tSCI. Further expanding emergency medical response systems throughout the country, training and equipping first responders in spinal motion restriction techniques, and establishing clear referral pathways for individuals with suspected tSCI are warranted. Development in these specific areas may reduce morbidity and mortality following acute tSCI.
Similar content being viewed by others
Introduction
Rapid and effective pre-hospital care, including basic life support and advanced cardiac life support, is essential to preserve life and reduce complications among individuals with acute traumatic spinal cord injury (tSCI) [1,2,3,4,5]. Furthermore, safe handling with proper pre-hospital spinal motion restriction when required following acute tSCI may reduce further neurological deterioration [1,2,3,4,5]. In low- and middle-income countries (LMICs) like Nepal, pre-hospital management can be challenging due to limited resources including equipment, trained first responders, and the absence of established pathways and systems of care for individuals with suspected tSCI [4]. The World Health Organization’s Guidelines for Essential Trauma Care provides a list of essential, achievable goals for trauma care in LMICs [1]. Specific to tSCI, essential guidelines include recognising the risk/presence of tSCI at every level of health care facility, from rural village health posts to tertiary hospitals. Furthermore, patients with suspected tSCI should arrive at tertiary care centres within 2 hours of injury utilising appropriate spinal motion restriction and transport techniques to minimise morbidity and mortality [1].
Data specific to pre-hospital care for individuals with spine injuries in Nepal are limited. One retrospective, acute hospital-based study found that patients with spine injuries reached the tertiary trauma centre on average 42 hours post-injury [6]. A more recent retrospective study reported that among 125 individuals who presented to a major trauma centre in the capital city, none were transported using spinal motion restriction techniques. Additionally, 30% of these individuals were presented more than 2 days post-injury [7]. To our knowledge, no study has examined pre-hospital care and patient handling at the site of injury, along with transportation in detail following tSCI in the setting of Nepal.
This study aims to improve our understanding of current pre-hospital care among individuals with acute tSCI in Nepal. Specific objectives are to describe patient handling at the site of injury, number of healthcare centre transfers between the injury site and tertiary trauma centre, modes of transportation, and time from injury to reaching tertiary trauma centres among individuals with tSCI.
Methods
A descriptive study was designed to include all individuals with tSCI admitted to SIRC over the period of 1 year. Primary data were collected from eligible individuals from 15th July 2019 to 14th July 2020. SIRC is the largest SCI rehabilitation hospital in Nepal, which sees an average of 300 individuals per year with new SCI cases from all 77 districts of the country.
All individuals with tSCI admitted to SIRC during the study period were eligible for enrolment. The following were excluded: individuals with non-traumatic SCI and non-SCI presenting diagnoses (i.e., stroke, traumatic brain injury); individuals with tSCI who were unconscious or disoriented immediately following the injury; individuals who sustained tSCI outside Nepal; and individuals who had sustained SCI more than one year prior to admission.
After providing written informed consent, enroled individuals participated in a structured interview with a trained interviewer. The interview was supplemented by the written medical record and provided the following information: demographic data (name, age, sex, address, occupation), injury data (date of injury, cause of injury, classification of injury according to International Standards for the Classification of Spinal Cord Injury), and pre-hospital handling data (people involved in transfer, techniques/equipment used for transfer, mode of transportation and time taken to reach intervening trauma centre). The interviewer recorded responses and information from the medical record on a standardised de-identified data entry form (see questionnaire for details).
Data were entered into an SPSS database, version 25.0 (IBM, New York, USA) and analysed using descriptive statistics. Continuous variables are presented as mean (standard deviation) and categorical variables are presented as frequency (percentage).
Results
Individual with SCI stratification and demographics
Two hundred and eighty-three individuals with SCI were admitted to SIRC over a period of 1 year (15 July 2019 to 14 July 2020). Seventeen were immediately excluded due to non-traumatic causes. Forty-six individuals were excluded for being unconscious or disoriented immediately following the injury. Four were excluded as their injuries occurred outside Nepal. Five were excluded as prior cases (occurring more than 1 year before the current rehabilitation admission). The remaining 211 individuals completed the study.
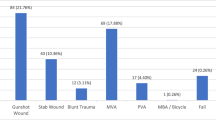
Most patients were male (n = 160, 75.8%), with a male-to-female ratio of 3.1:1.0. Mean age was 40.1 (±15.0), ranging from 11–79. See Table 1 for more details. Seventy-one (33.6%) individual injuries resulted in tetraplegia, 45 (59.2%) of which were incomplete (AIS B-D). One hundred and forty (66.4%) individual injuries resulted in paraplegia, of which 83 (59.2%) were complete (AIS A). The number of males and females sustaining complete tSCI were 83 and 27 respectively. See Table 1 for more details.
Initial handling at the injury site
Eight (4%) individuals in this study were initially assisted by trained individuals (first responders or traffic police), while 203 (96%) were initially assisted by untrained individuals. Five individuals with tSCI self-extricated themselves from the injury site. They either crawled or walked or rode a bike to reach home or hospital (see Fig. 1). As part of the initial response, 21 (10%) individuals (or those assisting the individual) called an ambulance or emergency help line (see Table 2). In terms of transfer techniques utilised, only one individual (0.5%) was transferred utilising a spine board for spinal motion restriction. No individuals with tetraplegia had cervical spinal motion restriction measures applied at the injury site. The majority of individuals were physically carried by two or more people (see Table 2).
Transportation and time from injury site to tertiary trauma centre
Following the initial response, individuals were transferred to nearby healthcare centres through a variety of methods. Approximately half of individuals were transported exclusively via ambulance. An additional third of individuals were transported using a combination of ambulance and different modes of transportation to reach the trauma centre (see Table 2).
All individuals who rode in an ambulance at any point in time (179 individuals) were asked about personnel and equipment on board. According to their recollection, six (3.4%) were staffed by a trained medical person; 81 (45.3%) were equipped with oxygen cylinders; 15 (8.4%) had a spine board, and 11 (6.1%) had a cervical collar onboard. All individuals were asked why other means of transport were preferred over ambulance and the most frequent reasons were lack of available ambulance service (56.9%) and prolonged time required for the ambulance to arrive (36.5%).
The number of healthcare centres (i.e., rural health posts, hospitals, district hospitals) where individuals were assessed prior to reaching the tertiary trauma centre ranged from 0–5 (average 1.6 ± 1.1). Only 31 (14.7%) individuals were transported to the trauma centre directly (see Table 3). Twenty-four (11%) individuals reached the tertiary trauma centre within 2 hours of injury. Of these, none received spine stabilisation. Ninety-eight (46%) individuals required more than 24 hours to reach the tertiary centre. The detailed time required from the moment of injury to reach the tertiary trauma centre is presented in Table 3.
Discussion
This study describes in detail the pre-hospital care and pathways experienced by individuals with tSCI in Nepal. The overwhelming majority (95%) of individuals in our study were assisted by untrained responders, with 21 (10%) calling an emergency help number or ambulance. Proper handling at the site of injury for individuals with suspected SCI requires a timely response by trained individuals. The need for more trained first responders and standarisation of emergency preparation was further supported by Banstola et al.’s recent nationwide survey of Nepal’s first response system [8]. Similar to our study, they found that among ambulances used throughout the country, only 2.9% were staffed by trained paramedics or EMTs. Not only are trained first responders needed, but proper equipment is also needed during suspected tSCI to apply proper spinal motion restriction. Among individuals in our study, only one (0.5%) received spinal motion restriction at the site of injury using a spine board. No individuals initially had a cervical collar applied, though 11 (5.2%) subsequently received cervical collars at intermediate health centres. Similarly, Dhakal et al. in 2018 found that among 91 individuals presenting to a major trauma centre in the capital city, none arrived with spinal motion restriction measures in place [7]. Acharya et al. looked at ambulance equipment among 109 ambulances utilised by a tertiary trauma centre and found that many ambulances had a cot only, while none were equipped with a cervical collar or other means of spinal motion restriction [9].
Participants in this study used multiple combinations of transportation modes to reach the trauma centre, with only half using ambulance transportation exclusively. Lack of availability and delay in response were cited as the primary reasons for using non-ambulance transportation. According to Shrestha et al., among 160 individuals presenting to a trauma centre in Nepal, only 31% came via ambulance, while others used private vehicles and public transportation [10]. Not knowing the number to call an ambulance and delayed arrival of the ambulance were their most common reasons. These collective findings highlight the need to expand emergency medical services. This expansion will require not just increased numbers of adequately staffed and equipped ambulances, but improved road access and clear referral pathways.
Regarding time from injury to reaching the tertiary trauma centre, our study found significant delays. Only 24 (11%) individuals in our study reached the tertiary trauma centre within the WHO’s recommended 2-hour window [1]. Furthermore, nearly half required more than 24 hours to reach the trauma centre. Related to this, most individuals visited two or more health centres before reaching the tertiary centre. Dhakal et al. also studied transport times for individuals with spine trauma in Nepal and found that 30% reached the trauma centre more than 48 hours after their initial injury [7]. In their 10-year study of nearly 900 individuals with acute tSCI, Bajracharya et al. found a mean transport time of 41.6 hours to reach the trauma centre [6]. These delays with multiple transfers increase the risk of further clinical and neurological deterioration along with known complications including pressure injuries.
Our findings highlight the need to further develop Nepal’s emergency response services. Nepal Ambulance Service, a private non-profit organization was established in 2011 and has expanded ambulance access throughout the country. Additionally, they offer a toll-free number (#102) to access their services which is available in most, but not all of the country [11]. The government of Nepal recognises the need to improve pre-hospital care. The Nepal Health Sector Strategy Implementation Plan 2016–2021 specifically outlines the need to “develop guidelines for national ambulance service with a unified telephone number, including networking and standardisation of emergency response services,” as well as ensure the availability of appropriate transportation [12].
Strengths of this study include the large sample size relative to studies specific to tSCI. Additionally, the one-on-one structured interview design provided in-depth detail related to the pre-hospital care experienced by study participants. As SIRC is the largest SCI rehabilitation centre in the country, accepting patients from every district of Nepal, we believe our findings represent a broad range of geographical and handling/transportation conditions. However, we recognise that this rehabilitation-based sample selection may limit generalisability, representing only those individuals who have progressed to acute SCI rehabilitation. For example, people with less severe SCI who recover fully during acute care may be underrepresented. Additionally, those with both very mild and very severe injuries may never reach the trauma or rehabilitation centres and therefore be underrepresented. Furthermore, our sample may underrepresent those who died on-site or during the acute phase, given sub-optimal care and delays in treatment. Additional studies focusing on cost-effective and feasible interventions for first response, spinal motion restriction, and referral pathways for individuals with suspected tSCI are warranted.
Data availability
The datasets generated and analysed during the current study are available from the corresponding author on reasonable request.
References
Mock C, Lormand JD, Goosen J, Joshipura M, Peden M. Guidelines for essential trauma care. Geneva: World Health Organization; 2004.
Chhabra H (editor). ISCoS textbook on comprehensive management of spinal cord injuries. 1st ed. New Delhi: Wolters Kluwer; 2015.
Kornhall D, Jørgensen J, Brommeland T, Hyldmo P, Asbjørnsen H, Dolven T, et al. The Norwegian guidelines for the prehospital management of adult trauma patients with potential spinal injury. Scand J Trauma Resusc Emerg Med. 2017;25:1–11.
Maschmann C, Jeppesen E, Rubin M, Barfod C. New clinical guidelines on the spinal stabilisation of adult trauma patients—consensus and evidence based. Scand J Trauma Resusc Emerg Med. 2019;27:1–10. https://doi.org/10.1186/s13049-019-0655-x.
Ahn H, Singh J, Nathens A, MacDonald R, Travers A, Tallon J, et al. Pre-hospital care management of a potential spinal cord injured patient: a systematic review of the literature and evidence-based guidelines. J Neurotrauma. 2011;28:1341–61.
Bajracharya S, Singh M, Singh G, Shrestha B. Clinico-epidemiological study of spinal injuries in a predominantly rural population of eastern Nepal: a 10 years’ analysis. Indian J Orthop. 2007;41:286.
Dhakal G, Paudel S, Dhungana S, Gurung G, Kawaguchi Y. Epidemiological characteristics of dorsal and lumbar spine trauma presenting to a Trauma Hospital in Kathmandu, Nepal: formulation of a national spine policy. Spine Surg Relat Res. 2018;2:249–52.
Banstola A, Smart G, Raut R, Ghimire K, Pant P, Joshi P, et al. State of post-injury first response systems in Nepal—a nationwide survey. Front Public Health. 2021;9:1–7.
Acharya R, Badhu A, Shah T, Shrestha S. Availability of life support equipment and its utilization by ambulance drivers. J Nepal Health Res Counc. 2017;15:182–6.
Shrestha SK, Koirala K, Amatya B. Patient’s mode of transportation presented in the emergency department of a tertiary care centre, Kavre, Nepal. Kathmandu Univ Med J. 2018;16:39–42.
Bhandari D, Yadav N. Developing an integrated emergency medical services in a low-income country like Nepal: a concept paper. Int J Emerg Med. 2020;13:1–5.
Government of Nepal Ministry of Health. Nepal Health Sector Strategy Implementation Plan 2016–2021. 2017.
Acknowledgements
The physiotherapists of Physiotherapy Department of SIRC have assisted in collecting the demographic data of individuals with SCI.
Author information
Authors and Affiliations
Contributions
SS was responsible for constructing the questionnaire, collecting feedback from expertise, submission for ethical approval, carrying out interview, data entry, statistical analysis, interpreting results and manuscript writing. KS was responsible for constructing the questionnaire, collecting feedback from expertise, data entry, statistical analysis and handling technical issues. CCG contributed to study design, data analysis, and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
All applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research. SIRC’s research committee and the Nepal Health Research Council approved the study (Reg.no 235/019).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Shrestha, S., Shrestha, K. & Groves, C.C. Patient handling and transportation from site of injury to tertiary trauma centres in Nepal following acute traumatic spinal cord injury: a descriptive study. Spinal Cord Ser Cases 8, 79 (2022). https://doi.org/10.1038/s41394-022-00545-3
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00545-3