Abstract
Study design
Retrospective medical record review.
Objective
To determine the prevalence and describe the profile of person with SCI (PWSCI) admitted in the public healthcare sector in Gauteng, South Africa.
Setting
Specialized public healthcare rehabilitation units in Gauteng, South Africa.
Methods
Medical records of PWSCI admitted to public healthcare rehabilitation units between 01 January 2018 and 31 December 2019 were perused. Data were collected anonymously and then summarised using descriptive and inferential statistics. Significance was set at p < 0.05.
Results
386 of 998 participants (38.7%) were admitted following SCI and the mean age was 36.9 years. Most participants were male (69.9%), with females significantly more likely to sustain a NTSCI (p < 0.001), which was the least common cause of SCI (34.9%). Those sustaining a TSCI were found to be significantly younger than their NTSCI counterparts (p < 0.001). Assault was the leading cause of injury (35.2%), and a positive HIV status with the presence of comorbidities were found to be significant risk factors for developing a NTSCI (p < 0.001). Most injuries were between T7-T12 (39.9%) and were complete (56.9%). The rehabilitation length of stay 85.6 days, with a mortality rate of 6.48%.
Conclusions
Gauteng has among the highest global proportion of TSCI due to assault. Of interest, more females sustained a NTSCI than their male counterparts. There is a need to strengthen SCI prevention strategies, particularly targeting assault in young males and infectious causes in females and older populations. Further epidemiological and outcomes-based research is required for PWSCI.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) is devastating, with morbidity not only limited to physical aspects but emotional, social, and vocational life areas too [1, 2]. Injury may occur as a result of trauma – referred to as traumatic SCI (TSCI) – or from disease or degeneration of the spinal cord – termed non-traumatic SCI (NTSCI) [3]. There are varying incidence rates of SCI worldwide with an estimated global incidence of TSCI of between 10.5 and 23 cases per 100,000 population [4, 5]. By region, estimates of NTSCI incidence range between 0.6 and 6.8 per 100 000 population [6]. Falls are fast becoming the leading cause of TSCI in high-income regions worldwide with high incidences of tumours and degenerative conditions in those with NTSCI [5,6,7]. In low and middle-income regions, transportation-related injuries remain the leading cause of TSCI while high incidences of infection-related injury remains prominent in those with NTSCI [8]. Males, those between the age of 15 and 29 as well as those above 65 years are at highest risk of TSCI while a proportionate rise in age is associated with an increased risk of NTSCI [9].
Statistics South Africa uses the term ‘disability’ as an umbrella term to refer to conditions affecting vision, hearing, communication, mobility, cognition and self-care [10]. In South Africa, SCI surveillance data is scanty with SCI epidemiological data predominantly based in two provinces, the Western Cape [11,12,13,14] and KwaZulu-Natal [15, 16]. The country – Gauteng Province in particular – continues to report the highest proportion of assault-related TSCI worldwide with the NTSCI population suffering largely from HIV- and tuberculosis-related afflictions [5, 16]. A wide range of incidence has been published with estimates of between 20.0 and 123 injuries per million population [13, 16] with no actual prevalence rates published in Africa.
Rehabilitation of persons with SCI (PWSCI) is necessary to improve the individual’s ability to perform functional activities and empower them and their families with the knowledge and skills to prevent secondary health complications [17]. Admission to a specialised SCI unit for acute and/or rehabilitative care has been associated with a shortened length of stay, fewer health complications and lower mortality rates [18,19,20]. To support the global agenda of strengthening rehabilitation services worldwide, part of the “Rehabilitation 2030” initiative aims to collect information relevant to rehabilitation care [21]. Gauteng Province, housing the country’s executive capital city and being the most populous province [22], lacks recent and thorough data with current research outdated and limited [23,24,25]. Without adequate epidemiological data, planning for SCI care from an acute to chronic setting becomes challenging [26, 27]. This study thus aims to update and describe the profile of PWSCI receiving rehabilitation in the public healthcare sector in Gauteng, South Africa.
Methods
Study design
This quantitative study used a retrospective, medical record review study approach. Convenience sampling was used to select medical records appropriately fitting the inclusion criteria.
Study setting and population
This study was conducted at five specialised rehabilitation units for PWSCI in the public healthcare sector of Gauteng Province. All medical records for adult individuals (≥18 years) who had sustained a confirmed SCI, irrespective of cause of injury, were considered for this study. The medical records were deemed eligible if the individual had been admitted to any of the five specialised SCI units in the public healthcare sector in Gauteng between the 1st of January 2018 and the 31st of December 2019. Those with no neurological fallout following SCI (classified as “E” according to the American Spinal Injury Association Impairment Scale) and those with neurological fallout as a result of cranial and/or peripheral nerve system pathology were excluded from the study. No sample size was calculated for this study as all medical records that met the inclusion criteria were included in the study.
Data collection
A pilot study of ten medical records was conducted to ensure practicality, familiarity, efficiency and quality of the data collection form and overall study procedure [28]. No amendments needed to be made to the data collection form or to the study in its entirety. Data was collected using a specifically designed data collection form which included all aspects of the International Spinal Cord Injury Core Data Set (ISCICDS) [29, 30] as well as the following data: HIV status, presence and type of comorbidities, occupation, marital status, the highest level of education, the place from where the participant was admitted into rehabilitation, rehabilitation mortality as well as the type of mobility aid used at discharge from rehabilitation. Rehabilitation ward records were used to identify patients admitted into the rehabilitation ward/s across the study period with these records being pursued and those fitting the inclusion criteria enroled in the study.
Data analysis
Data were summarised using descriptive statistics with inferential statistics used to investigate relationships between independent and dependent variables. The SPSS v27 was used to analyse the data and continuous variables were analysed using mean with standard deviation as well as median and interquartile ranges. Categorical variables were analysed using frequencies and percentages. Only data that was available and collectable in the medical records were included in the analysis. Our data were not normally distributed, as confirmed by a less than 0.05 significance of the Shapiro-Wilk test of normality. Hence, non-parametric tests were used to analyse the data. The Mann–Whitney U test was used to determine whether significant differences existed between continuous variables of age, days to admission, length of, stay and cause of injury. The Chi-square measure of association and the Fischer’s exact test were used to determine the associations between independent and dependent categorical variables. The Spearman correlation coefficient was used to determine the relationship between age, days to admission and length of stay. Univariate and multivariate binary logistic regression was used to determine the predictors of cause of injury. Significance was set at p < 0.05 with a 95% confidence interval.
Ethical approval
Ethical clearance was granted by the University of the Witwatersrand’s Human Research Ethics Committee (certificate number M200582). Additionally, permission was granted by the management of each rehabilitation unit. The medical records and data collection sheet remain anonymous and this paper does not disclose any personal information.
Results
During the two-year study period, 998 patients were admitted for rehabilitation to Gauteng’s five specialised rehabilitation units. Of these, 386 had sustained a SCI and met all the inclusion criteria and were thus included in the study.
Sociodemographic profile
The mean (SD) age of study participants was 36.90 (12.12) years while the median age was 34 years (range 18–75). The most common age group was 31–45 (n = 148, 38.85%), closely followed by those 18–30 (n = 147, 38.58%) and then those 46–60 (n = 66, 17.32%) and 61 and over (n = 20, 5.25%). Participants with TSCI were significantly younger than those with NTSCI (p < 0.001). Males were more commonly injured than females (n = 270, 69.95%) across the two-year study period. Of note, females were more commonly affected by NTSCI than their male counterparts, with a male to female ratio of 5.44:1 and 0.75:1 for TSCI and NTSCI respectively. A positive and significant association was shown to exist between males and TSCI as well as between females and NTSCI (p < 0.001). Most of the participants in this study were Black (n = 357, 92.49%) and resided in the City of Tshwane (n = 91, 24.53%). A significant association was found to exist between formal employment and TSCI, with approximately half of the participants formally employed at the time of admission (n = 161, 48.20%) (p < 0.001). Unemployment and NTSCI were also found to be significantly associated (p < 0.001). A third of study participants had a matric certificate (n = 89, 35.60%). Most of the participants were never married (n = 226, 65.89%), with a significant association between TSCI and never being married, as well as between NTSCI and being married (p < 0.001). The sociodemographic profile of the included participants is presented in Table 1.
Injury profile
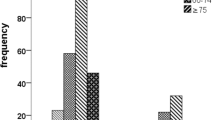
The overall prevalence of SCI in Gauteng public healthcare rehabilitation units was 38.67%. Traumatic SCI (n = 251, 65.03%) was more common than NTSCI (n = 135, 34.97%). The most common cause of injury overall was as a result of assault (n = 136, 35.23%) followed by transportation injuries (n = 87, 22.54%) and infectious causes (n = 66, 17.10%) – most commonly HIV- and tuberculosis-related. The injury frequency for TSCI and NTSCI is outlined below in Figs. 1 and 2 respectively. Of note, 5.18% of all participants (n = 20) were diagnosed with cancer and were included in the “other NTSCI” group.
Most of the participants had complete lesions and were classified as AIS A as per the International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI) (n = 170, 56.86%). Traumatic SCI was found to be significantly associated with an AIS A injury (p < 0.001), while NTSCI and motor incomplete lesions (AIS C and AIS D) were significantly associated (p < 0.001). The most common site of injury was the lower thoracic region of T7-T12 (n = 105, 39.92%) (Table 2).
Most participants in this study were admitted into rehabilitation from tertiary-level healthcare institutions (n = 223, 62.82%). There was a mean (SD) time of 64.48 (59.78) days between the day of injury and day to rehabilitation admission (median 46 days, range 1–369), with the NTSCI group having a significantly longer waiting period than their TSCI counterparts (p < 0.001). Once admitted, the mean (SD) length of stay in rehabilitation was 85.59 (63.21) days (median 72 days, range 5–388 days). Most of the study participants were classified as HIV negative (n = 151, 69.91%) and most did not present with any health comorbidity (n = 243, 73.19%).
Significant associations were found to exist between the NTSCI group and being HIV positive (p < 0.001) as well as having a health comorbidity (p < 0.001). The most common comorbidity was tuberculosis (n = 44, 11.40%) followed by hypertension (n = 26, 6.74%) and diabetes (n = 5, 1.30%). Vertebral fractures were common (n = 256, 77.11%), with the high proportion in the NTSCI group likely a reflection of the disease process associated with spinal tuberculosis. Just under one half of the participants received spinal surgery (n = 154, 44.51%). There was a significant association between the TSCI group and both of these data sets (p < 0.001). Associated injuries (as defined by the ISCICDS and only recorded in persons with TSCI) were found to exist in just under half of the participants in the TSCI group (n = 85, 43.82%). The injury profile of the included participants is presented in Table 3.
Overall, most of the participants in this study were discharged from rehabilitation (n = 342, 88.60%) with an overwhelming proportion being discharged to a private residence (n = 330, 97.29%). Successful discharge from rehabilitation was significantly associated with the TSCI group with those sustaining a NTSCI more likely to not be discharged (p < 0.001). Of those that were not discharged from rehabilitation, 25 participants demised (6.48%), eight refused further rehabilitation care (2.07%), seven absconded (1.81%), and four became medically unstable and were deemed unfit to continue rehabilitation and were transferred back to acute care (1.04%). No participants made use of a ventilator or supplementary oxygen at discharge. Manually-operated wheelchairs (n = 185, 57.81%) were the most common type of assistive device used for mobility at discharge from rehabilitation. The injury profile information related to rehabilitation completion is provided in Table 4.
Binary logistic regression was used to explore sociodemographic predictors of SCI (Table 5). The probability of acquiring a TSCI was found to increase by 0.94 for every one-unit increase in age (p < 0.001) and by 0.14 in females as compared with their male counterparts (p < 0.001). Being unemployed was found to increase the odds of acquiring a TSCI by 0.37 (p < 0.001).
Traumatic SCI was found to be a significant predictor for sustaining a vertebral fracture as well as for requiring spinal surgery (p < 0.001) as illustrated in Table 6.
Binary logistic regression was also used to explore sociodemographic factors in relation to injury outcomes (Table 7). The probability of sustaining a vertebral fracture was found to increase significantly by 0.37 in females and 0.26 in the unemployed respectively (p < 0.001). A significant correlation exists between rehabilitation mortality and age with the risk of death increasing by 0.92 for every one-unit increase in age (p < 0.001).
Discussion
To our knowledge, this is the first study to report on the prevalence and profile of SCI in each of Gauteng’s public healthcare rehabilitation units. Across our two-year study period, 386 PWSCI were admitted to Gauteng’s five public rehabilitation unit’s – an average of 193 admissions per year. Hart [24] reported that there were 1 203 admissions to a single public healthcare rehabilitation unit in Gauteng over an 11-year period between 1988 and 1998 – an average of 109 admissions per year. In the country’s acute-care units, the number of admissions averaged between 13 and 349 admissions per year [13, 14]. The contrasting study settings, levels of care and time periods makes comparison difficult, highlighting the need for ongoing SCI surveillance in a public, private, acute and rehabilitative setting.
Young males continue to be significantly most at risk of sustaining a TSCI, with world-high levels of assault – largely due to gunshot and stab wounds – most prominent (p < 0.001). These findings are consistent with literature previously published in Gauteng [23, 24] the Western Cape [11] and Kwazulu-Natal [16]. Crime levels, particularly those related to assault, have been shown to be highest in Gauteng [31]. Disabling injuries contribute significantly to the national burden of disease putting a strain on an already burdened healthcare system [32]. Interventions to address the prevention of crime, particularly in the male population, must be strengthened.
Notable findings were discovered in the NTSCI population. We found that significantly more females sustained a NTSCI (p < 0.001) with this population being significantly older too (p < 0.001). This reflects previous literature from Kwazulu-Natal which, to the authors knowledge, is the only literature worldwide where more females are affected by NTSCI than males [15, 16]. This may be a direct reflection and association between the high proportion of infectious-related NTSCI and a country with one of the highest prevalence’s of HIV and tuberculosis in Sub-Saharan Africa, particularly in women [33]. These conditions are associated with serious long-term health implications and, superimposed on a NTSCI, may talk to the significant rate of unemployment in this study group (p < 0.001) [31, 33, 34]. It is imperative that the country urgently addresses the prevention and management of HIV at various healthcare levels in line with the “90-90-90” programme as outlined by the Joint United Nations Programme on HIV/AIDS [35]. We also noted that those with a NTSCI waited significantly longer for rehabilitation admission (p < 0.001). This may be a reflection of the usually gradual and progressive nature of onset of most NTSCI conditions. Further, one must note that medical work-ups and investigations may be delayed in a heavily over-burdened and under-funded public healthcare sector. A significant proportion of participants in the NTSCI group did not complete their rehabilitation stay (p < 0.001). This may be because of the older age and direct correlation to a higher mortality rate as well as the higher proportion of HIV and other health comorbidities of this group potentially affecting their medical stability. We suggest that more research is conducted in the NTSCI populations, particularly with regards to disability and functional outcomes.
Mixed results with regards to injury classification and severity were found as compared with previously published South African literature. Complete injury and paraplegia was found to be most prevalent in our study, similar to outdated Gauteng literature by Hart and Williams [23] and Hart [24]. This differs to published research from Kwazulu-Natal [16] and the Western Cape [11,12,13,14] where incomplete injuries and quadriplegia were most common. Study setting and injury aetiology is likely to have influenced these findings. Gauteng’s literature focussed on the rehabilitative stage and reflected high levels of SCI as a result of assault while Kwazulu-Natal and the Western Cape reflected findings from the acute stage with high levels of transportation-related injuries. Those with injuries as a result of transportation may also be compensated by the country’s Road Accident Fund and have received their rehabilitation in the private healthcare sector. Patients with complete injuries experience more functional fallout, are at higher risk of secondary complications and have a higher risk of mortality post discharge [36,37,38]. There is a need to strengthen access to rehabilitation care with focussed and appropriate planning of rehabilitation services minimising poor health outcomes in those with SCI.
Our study investigated associations between sociodemographic and injury profiles. Age, gender and being unemployed were all found to be significant predictors of acquiring a TSCI. The risk of sustaining a vertebral fracture was found to increase significantly by 0.37 in females and 0.26 in the unemployed respectively. Traumatic SCI was found to be a significant predictor of sustaining a vertebral fracture as well as underdoing spinal surgery. However, a low proportion of those with spinal fractures underwent spinal surgery and were rather managed conservatively. Again, financial and human resource limitations within the public healthcare sector is the likely driver behind this finding. This highlights the need to advocate for resources from theatre time to equipment and specialists. Ultimately, however, preventing TSCI would have a direct economic benefit to the health system [3, 15].
Our study showed a mortality rate of 6.48%. In an acute care unit in the Western Cape, the mortality rate was two-thirds lower at 2.2% [12]. The risk of death in this study increased by 0.92 for every one-unit increase in age. In-hospital mortality rates are reported to be three times higher in low-middle income countries, with mortality being an indicator of quality of hospital care [39]. Madasa et al. [38] reported that almost one-quarter of those sustaining a TSCI died four years after injury. This highlights the need to review acute-care standard operating procedures and address long term follow-up care to maximise health outcomes and limit mortality in this high-risk population.
Conclusion
Young males are most at risk of SCI and are consequentially admitted for rehabilitation in the public healthcare setting in Gauteng. Assault continues to be the leading cause of SCI in Gauteng, with numbers unrivalled the world over. These injuries tend to be severe, most commonly causing complete paraplegia to the lower thoracic spine. The NTSCI population differed, however, with the older female populations of Gauteng significantly more affected with their injuries most often incomplete in nature. The risk of NTSCI in those with HIV and comorbidities was high, a point of interest for preventative care and an indicator to optimise the ongoing care in these populations. Being unemployed was found to be a risk factor for sustaining a TSCI, a worrying finding given South Africa’s high unemployment rate. Not being married was also found to have a significant association for TSCI. There is an urgent need to realise community and societal reintegration post discharge from rehabilitation while addressing stigma and empowering those with SCI.
Implications
Practice
Prevention strategies must be strengthened for both TSCI and NTSCI. While the world implements preventative strategies aimed at transport- and fall-related injuries, South Africa would do well to address the high levels of violence and crime in the fight against TSCI. In the continued absence of an acute public healthcare SCI unit in Gauteng, acute healthcare provision for PWSCI will continue to remain disjointed. It is imperative, then, that continued education and professional development of both the general population and medical personnel working with PWSCI (particularly at tertiary- and regional-level healthcare facilities) is undertaken respectively. Further, patients will continue to wait long periods for their chance in rehabilitation for a stay that generally lasts just short of three months. While the majority of those that are admitted will be deemed fit for discharge by the multidisciplinary team and return to their private residences’, not all will reach this state. While the proportion of those not completing rehabilitation remains less than 10%, as healthcare professionals we should endeavour to realise a successful rehabilitation rate of 100%.
Research
Surveillance research on SCI is recommended. It is recommended that this same study be conducted at Gauteng’s private healthcare rehabilitation units over the same study period. This will provide grounds for direct comparisons to be made between the two cohorts and give Gauteng a complete picture of SCI rehabilitation. Similar research to that presented here should be conducted in other provinces to provide a more complete picture of SCI in South Africa and help guide policy change by ensuring the best possible care and opportunity for these individual’s post-injury. More research regarding the profile and outcomes of NTSCI is required both locally and abroad.
Data availability
The datasets analysed for this study are available from the authors on reasonable request.
References
Craig A, Tran Y, Middleton J. Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord. 2009;47:108–14. https://doi.org/10.1038/sc.2008.115.
Malekzadeh H, Golpayegani M, Ghodsi Z, Sadeghi-Naini M, Asgardoon M, Baigi V, et al. Direct cost of illness for spinal cord injury: a systematic review. Glob Spine J. 2022;12:1267–81. https://doi.org/10.1177/21925682211031190.
World Health Organization. International perspectives on spinal cord injury. WHO; 2013. https://apps.who.int/iris/bitstream/handle/10665/94192/WHO_NMH_VIP_13.03_eng.pdf;jsessionid=C5909EC39AA45BBB7B95FE638F5FB4C0?sequence=1. Accessed 15 Jan 2023.
Kumar R, Lim J, Mekary RA, Rattani A, Dewan MC, Sharif SY, et al. Traumatic spinal cord injury: global epidemiology and worldwide volume. World Neurosurg. 2018;113:e345–363. https://doi.org/10.1016/j.wneu.2018.02.033.
Lee BB, Cripps RA, Fitzharris M, Wing PC. The global map for traumatic spinal cord injury epidemiology: update 2011, global incidence rate. Spinal Cord. 2014;52:110–6. https://doi.org/10.1038/sc.2012.158.
New PW, Cripps RA, Bone Lee B. Global maps of non-traumatic spinal cord injury epidemiology: towards a living data repository. Spinal Cord. 2014;52:97–109. https://doi.org/10.1038/sc.2012.165.
Kang Y, Ding H, Zhou H, Wei ZJ, Liu L, Pan DY, et al. Epidemiology of worldwide spinal cord injury: a literature review. J Neurorestoratol. 2018;6:1–9. https://doi.org/10.2147/JN.S143236.
Musubire AK, Meya DB, Bohjanen PR, Katabira ET, Barasukana P, Boulware DR, et al. A systematic review of non-traumatic spinal cord injuries in sub-Saharan Africa and a proposed diagnostic algorithm for resource-limited settings. Front Neurol. 2017;8:618–27. https://doi.org/10.3389/fneur.2017.00618.
Van Den Berg MEL, Castellote JM, Mahillo-Fernandez I, de Pedro-Cuesta J. Incidence of spinal cord injury worldwide: a systematic review. Neuroepidemiology. 2010;34:184–93. https://doi.org/10.1159/000279335.
Statistics South Africa. Census 2011: profile of persons with disabilities in South Africa. 2011. https://www.statssa.gov.za/publications/Report-03-01-59/Report-03-01-592011.pdf. Accessed 15 September 2022.
Joseph C, Delcarme A, Vlok I, Wahman K, Phillips J, Wikmar NL. Incidence and aetiology of spinal cord injury in Cape Town, South Africa: a prospective, population-based study. Spinal Cord. 2015;53:692–6. https://doi.org/10.1038/sc.2015.51.
Sothmann J, Stander J, Kruger N, Dunn R. Epidemiology of acute spinal cord injuries in the Groote Schuur Hospital acute spinal cord injury (GSH ASCI) unit, Cape Town, South Africa, over the past 11 years. S Afr Med J. 2015;105:835–9. https://doi.org/10.7196/SAMJnew.8072.
Phillips J, Braaf J, Joseph C. Another piece to the epidemiological puzzle of traumatic spinal cord injury in Cape Town, South Africa: a population-based study. S Afr Med J. 2018;108:1051–4. https://doi.org/10.7196/SAMJ.2018.v108i12.13134.
Miseer S, Mann T, Davis J. Burden and Profile of Spinal pathology at a Major Tertiary Hospital in the Western Cape, South Africa. SA Orthop J. 2019;18. https://doi.org/10.17159/2309-8309/2019/v18n1a4.
Godlwana LL, Gounden P, Ngubo P, Nsibande T, Nyawo K, Puckree T. Incidence and profile of spinal tuberculosis in patients at the only public hospital admitting such patients in Kwazulu-Natal. Spinal Cord. 2008;46:372–4. https://doi.org/10.1038/sj.sc.3102150.
Pefile N, Mothabeng JD, Naidoo S. Profile of patients with spinal cord injuries in Kwazulu-Natal, South Africa: implications for vocational rehabilitation. J Spinal Cord Med. 2019;42:709–18. https://doi.org/10.1080/10790268.2018.1428264.
Van Wyk V. Activity limitations and participation restrictions four years after traumatic spinal cord injury in Cape Town, South Africa. Master’s Thesis, University of the Western Cape; 2018. http://etd.uwc.ac.za/xmlui/bitstream/handle/11394/6873/3305-4225-2-SM.pdf?sequence=1&isAllowed=y. Accessed 26 January 2021.
Parent S, Barchi S, LeBreton M, Casha S, Fehlings MG. The impact of specialized centers of care for spinal cord injury on length of stay, complications and mortality: a systematic review of the literature. J Neurotrauma. 2011;28:1363–70. https://doi.org/10.1089/neu.2009.1151.
Maharaj MM, Stanford RE, Lee BB, Mobbs RJ, Marial O, Schiller M, et al. The effects of early or direct admission to a specialized spinal injury unit on outcomes after traumatic spinal cord injury. Spinal Cord. 2017;55:518–24. https://doi.org/10.1038/sc.2016.117.
Conradsson D, Rhoda A, Mlenzana N, Wikmar LN, Wahman K, Hultling C, et al. Strengthening health systems for persons with traumatic spinal cord injury in South Africa and Sweden: a protocol for a longitudinal study of processes and outcomes. Front Neuro. 2018;9:453–9. https://doi.org/10.3389/fneur.2018.00453.
World Health Organization. Rehabilitation 2030: a call for action. 2017. https://www.who.int/disabilities/care/Rehab2030MeetingReport2.pdf?ua=1. Accessed 11 April 2020.
Statistics South Africa. Mid-year population estimates 2019 (Statistical Release P0302) 2020. http://www.statssa.gov.za/publications/P0302/P03022019.pdf. Accessed 18 March 2020.
Hart C, Williams E. Epidemiology of spinal cord injuries: a reflection of changes in South African Society. Paraplegia. 1994;32:709–14. https://doi.org/10.1038/sc.1994.115.
Hart C. Spinal cord injury statistics at the Natalspruit Hospital spinal unit over an 11-year period. S Afr J Physiother. 2000;56:13–15.
Mashola MK, Mothabeng DJ. Associations between health behaviour, secondary health conditions and quality of life in people with spinal cord injury. Afr J Disabil. 2019;8:1–9. https://doi.org/10.4102/ajod.v8i0.463.
Morris LD, Grimmer KA, Twizeyemariya A, Coetzee M, Leibbrandt DC, Louw QA. Health system challenges affecting rehabilitation services in South Africa. Disabil Rehabil. 2021;43:877–83. https://doi.org/10.1080/09638288.2019.1641851.
Tiwari R, Ned L, Chikte U. HRH planning for rehabilitation services: a focus to reduce inter-provincial inequalities. S Afr Health Rev. 2020;2020:53–63. https://hdl.handle.net/10520/ejc-healthr-v2020-n1-a9.
Thabane L, Ma J, Chu R, Cheng J, Ismaila A, Rios LP, et al. A tutorial on pilot studies: the what, why and how. BMC Med. Res. Methodol. 2010;10. https://doi.org/10.1186/1471-2288-10-1.
DeVivo MJ, Biering-Sorensen F, Charlifue S, Noonan V, Stripling T, Wing P. International spinal cord injury core data set. Spinal Cord. 2006;44:535–40. https://doi.org/10.1038/sj.sc.3101958.
Biering-Sorensen F, DeVivo MJ, Charlifue S, Chen Y, New PW, Noonan V, et al. International spinal cord injury core data set (version 2.0) – including standardization of reporting. Spinal Cord. 2017;55:759–64. https://doi.org/10.1038/sc.2017.59.
South African Police Service. Crime statistics: integrity. 2022. https://www.saps.gov.za/services/crimestats.php. Accessed 13 September 2022.
Institute for Health Metrics and Evaluation. South Africa health data. 2022. https://www.healthdata.org/south-africa. Accessed 13 September 2022.
Ramjee G, Daniels B. Women and HIV in Sub-Saharan Africa. AIDS Res Ther. 2013;10:30–38. https://doi.org/10.1186/1742-6405-10-30.
Myezwa H, Hanass-Hancock J, Ajidahun AT, Carpenter B. Disability and health outcomes – from a cohort of people on long-term anti-retroviral therapy. Sahara J. 2018;15:50–59. https://doi.org/10.1080/17290376.2018.1459813.
Joint United Nations Programme on HIV/AIDS. 90-90-90: an ambitious treatment target to help end the AIDS epidemic. 2014. https://www.unaids.org/sites/default/files/media_asset/90-90-90_en.pdf. Accessed 23 April 2021.
Joseph C, Wikmar L. Prevalence of secondary medical complications and risk factors for pressure ulcers after traumatic spinal cord injury during acute care in South Africa. Spinal Cord. 2016;54:535–9. https://doi.org/10.1038/sc.2015.189.
Pilusa S, Myezwa H, Potterton J. Secondary health conditions in people with spinal cord injury in South Africa: prevalence and associated factors. S Afr Med J. 2021;111:1211–7. https://doi.org/10.7196/SAMJ.2021.v111i12.15761.
Madasa V, Boggenpoel B, Phillips J, Joseph C. Mortality and secondary complications four years after traumatic spinal cord injury in Cape Town, South Africa. Spinal Cord Ser Cases. 2020;6:84–90. https://doi.org/10.1038/s41394-020-00334-w.
Chamberlain JD, Meier S, Mader L, von Groot PM, Brinkhof MWG. Mortality and longevity after spinal cord injury: systematic review and meta-analysis. Neuroepidemiology. 2015;44:182–98. https://doi.org/10.1159/000382079.
Acknowledgements
The authors would like to thank all the participating rehabilitation units for granting us access to their databases.
Funding
This study was supported by the National Research Fund (Thuthuka Grant 118017). The funding body played no role in the study data procedures, nor in the writing of this paper. Open access funding provided by University of the Witwatersrand.
Author information
Authors and Affiliations
Contributions
M.A.A., S.P., and M.K.M. conceptualised the study. M.A.A. collected and analysed the data. M.A.A., S.P., and M.K.M. wrote and edited the paper.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Alves, M.A., Pilusa, S. & Mashola, M.K. The prevalence and profile of spinal cord injury in public healthcare rehabilitation units in Gauteng, South Africa. Spinal Cord Ser Cases 9, 15 (2023). https://doi.org/10.1038/s41394-023-00571-9
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-023-00571-9