Abstract
Objectives
To track and evaluate changes in the number and types of physical activity barriers experienced by adults with spinal cord injury (SCI) in response to a physical activity counselling intervention, using a newly-developed tracking and coding method.
Design
A secondary analysis of data from a randomized controlled trial of a physical activity behavioural intervention (#NCT03111030).
Setting
General community.
Participants
Adults with chronic SCI (n = 14).
Intervention
An introductory behavioural coaching session followed by eight, weekly follow-up sessions were delivered in-person or by phone/video call. The interventionist utilized behaviour-change techniques tailored to individual participants’ readiness for change, barriers, and preferences. Participants set goals for achieving the SCI exercise guidelines. Coaching sessions were audio-recorded and transcribed verbatim.
Main outcome measure(s)
Changes over time in the number of barriers reported within each level of a social-ecological model of influences on physical activity (intrapersonal, interpersonal, institutional, community, policy).
Results
A total of 152 physical activity barriers were identified across 122 coaching sessions. Within each level of influence, the number of identified barriers decreased significantly over the intervention period. Intrapersonal barriers (e.g., lack of motivation, low self-efficacy) were most frequently reported and showed the greatest reductions over time.
Conclusions
Using a new coding method to track changes in physical activity barriers, this pilot project showed a significant decrease in barriers over the course of a counselling intervention. Understanding physical activity barrier dynamics can improve the design of physical activity-enhancing interventions. Dynamic barrier-tracking methods could also be used to improve intervention implementation and evaluation.
Similar content being viewed by others
Introduction
Dozens of cross-sectional studies have documented physical activity barriers experienced by people with spinal cord injury (SCI) [1, 2] and other physical disabilities. In a meta-review of these studies, physical activity barriers and facilitators were thematically classified into a social-ecological model (SEM; see Fig. 1 for the SEM levels and barrier/facilitator themes) consisting of intrapersonal, interpersonal, institutional, community, and policy levels [3, 4]. The barriers were relatively consistent across studies, prompting a call to shift research from merely describing physical activity barriers, to developing barrier-alleviating interventions to support physical activity initiation and maintenance [3].
Reprinted with permission [pending] from the publisher (Human Kinetics) from the article, Physical activity and spinal cord injury: Lessons learned at the lowest end of the physical activity spectrum by Todd and Martin Ginis [15].
Schwarzer’s Health Action Process Approach (HAPA) model suggests that people initiating a physical activity regimen have a different mentality than people maintaining physical activity [5, 6]. Indeed, in a study of 238 adults with SCI, people intending to start a physical activity regimen (i.e., “intenders”) reported significantly less physical activity planning and lower self-efficacy to do specific physical activities, to schedule physical activity and to overcome physical activity barriers than people who were routinely active (i.e., “actors”) [7]. HAPA theorizing [5] suggests interventions that increase physical activity planning and self-efficacy will help physical activity intenders become actors. A randomized controlled trial (RCT) of 44 adults with SCI supported this hypothesis. Participants who made detailed plans for doing physical activity and overcoming specific physical activity barriers significantly increased their physical activity barrier self-efficacy and the number of minutes per week spent on physical activity, relative to participants in a control group [8]. These findings demonstrate the importance of planning as a behavioural intervention technique to overcome barriers and increase physical activity in adults with SCI.
When working with clients with SCI to develop barrier management plans, physical activity interventionists could formulate those plans by drawing from extensive evidence-based lists of physical activity barriers [2]. However, barriers to initiating physical activity (e.g., fear of injury) may differ from barriers to maintaining physical activity (e.g., boredom). We are unaware of any published study, in any disability group, that has examined whether physical activity barriers change over time and in response to a counselling intervention. Because different types of barriers require different types of intervention techniques or strategies [9], understanding the dynamics of physical activity barriers could help improve the design of physical activity-enhancing interventions. Intervention techniques could then be tailored to participants’ barriers and needs at different points of an intervention (e.g., when initiating a new physical activity regimen versus when trying to maintain a new regimen).
We are unaware of any published studies that describe methods to track and analyze physical activity barriers in intervention studies over time in any population. In the absence of such methods, we developed a new systematic coding method for dynamic tracking and evaluation of changes in physical activity barriers. This paper describes the application and results of those methods in a pilot study consisting of secondary analysis of data collected from a physical activity behavioural coaching intervention for adults with SCI [10].
Methods
Design and participants
This study was approved by the Clinical Research Ethics Board of the University of British Columbia. A secondary analysis was conducted of data collected from participants in the treatment condition (n = 14; Mage = 46 ± 14 years; 36% female) of a 9-week RCT of a physical activity behavioural coaching intervention involving adults with chronic SCI (Mtime-post-injury = 15±14 years; 36% tetraplegia; 57% motor-complete injuries). As part of the study inclusion criteria, all participants were currently performing less than 150 min per week of physical activity at baseline. On average, participants in the treatment condition self-reported 68 min (SD = 56 min) per week of moderate-vigorous intensity physical activity at baseline. The complete study inclusion and exclusion criteria are published elsewhere [10].
Intervention
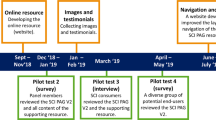
A complete description of the development and delivery of this patient and provider co-developed physical activity intervention has been previously published [10, 11]. Briefly, the intervention was framed within Schwarzer’s HAPA model [5]. Treatment-condition participants received an introductory, 1-h behavioural coaching session in week 1, followed by eight, weekly 10–15-min follow-up sessions in weeks 2–9. Author JM delivered all coaching in-person at the research facility or by phone/Skype. The intervention utilized behaviour change techniques (BCT; e.g., problem solving, graded tasks, action planning) [12] tailored to each participant’s HAPA [5] stage, barriers and preferences. Participants and the interventionist co-developed goals for achieving the SCI exercise guidelines [13] and self-selected their exercise location (e.g., home, community).
Data Collection, Coding Method, and Analysis
All coaching sessions were audio-recorded and transcribed verbatim. A coding method, documented in a coding manual, was developed to code/categorize physical activity barriers within the framework of a SEM ([3]; see Fig. 1). A barrier was defined as any intrapersonal, interpersonal, institutional, community, or policy-level factor that hinders a person from participating in physical activity. Each barrier was coded as being situated at the intrapersonal, interpersonal, community, institutional, or policy level based on a previous SEM analysis of factors related to physical activity participation in adults with disability [3]. More specifically, codes and codes’ descriptions for potential physical activity barriers were created using identified factors from this previous SEM analysis [3]. In that review of reviews [3], factors related to physical activity were extracted from each included paper and then inductively organized and coded according to common categories. The categories were then deductively coded as being situated within the intrapersonal, interpersonal, institutional/organizational, community or policy level of McLeroy et al.’s SEM [4]. The coding method was tested on three coaching-session transcripts whereby barriers mentioned in each transcript were identified, extracted into a list, and deductively coded by two authors working independently. Coding agreement between the two independent coders was 83%–100%. Given the high level of agreement, the coding method was then applied to barriers that were identified and extracted from the remaining transcripts. Finally, codes that were not identified in the any of the transcripts were removed from the coding manual.
The two authors worked independently to code the remaining coaching-session transcripts. Coding discrepancies were discussed until agreement was achieved or resolved by the senior authors. Coder agreement and mean prevalence and bias-adjusted kappa (PABAK) were calculated across transcripts.
Total number of barriers mentioned overall, and within each level of the SEM, were calculated for each participant at each session. Paired samples t-tests were conducted to test for change in the total number of barriers, and number of barriers within each SEM level, mentioned at session 1 versus 9. Statistical comparisons were conducted at these two time-points only, in order to avoid inflation of alpha and risk of a Type 1 error. However, to visualize dynamic changes in the number and types of barriers reported over all time points, these variables were plotted across all nine sessions of the intervention.
Results
Transcripts were available for 123 of 126 coaching sessions (2.4% missing data). Average session duration was 23 min for the introductory session (range: 13–31 min) and 12 min for the follow-up sessions (range: 7–17 min).
Coding Process Statistics
The final coding manual included 21 barrier codes grouped within 13 broader categories of barriers within the 5 main SEM levels. The full coding manual, including example barriers for each of the 21 barrier codes, is presented in Appendix A. Overall, 152 barriers were extracted from the 123 transcribed sessions and were coded using 21 barrier codes of the coding manual. Across all transcripts, coder agreement was 77% and mean PABAK was 0.97 indicating an “almost perfect” inter-coder reliability.
Dynamic barrier analysis
The total number of barriers mentioned at each session decreased significantly from the introductory session (Mean = 6.9, SD = 3.1) to session 9 (Mean = 1.0, SD = 0.9), t(10) = 5.59, p < 0.01. Barriers also significantly decreased within each SEM level (p < 0.05; see Table 1).
Figure 2 graphically illustrates dynamic changes in barriers across the intervention sessions and across the various SEM levels. Although the number of intrapersonal-level barriers showed the greatest decrease, this category still accounted for the most barriers at session 9. Community- and institutional-level barriers remained consistent until session 7, and then decreased at session 8 and 9. Policy-level barriers peaked during sessions 5 and 7, then diminished at session 9. Interpersonal-level barriers fluctuated across the first 6 sessions, but ultimately reduced to zero by session 9.
Each line represents the average number of barriers that were reported across all participants each week. The black dotted line represents barriers at the intrapersonal level. The orange dashed line represents barriers at the interpersonal level. The grey dashed line represents barriers at the institutional level. The green dashed line represents barriers at the community level, and the blue solid line represents barriers at the policy level.
Discussion
In this study, we developed a systematic coding method to track and evaluate physical activity barrier dynamics over the course of a behavioural intervention for people with SCI. We pilot-tested this method using transcripts from 123 behavioural coaching sessions that were delivered as part of a RCT of a physical activity behaviour-change intervention [10].
Across the intervention, participants reported a total of 152 physical activity barriers. Overall, the number of barriers declined over time across all levels of a SEM. The greatest reductions occurred for the most common barriers; intrapersonal-level factors, particularly psychological barriers (e.g., lack of confidence to perform physical activity, and lack of motivation) and barriers related to body functions/structures (e.g., experiencing pain, feeling too exhausted to exercise). These findings align with our intervention fidelity data [10] which showed that the most frequently-delivered BCT (e.g., problem solving, social support, action planning) were techniques that are used to target intrapersonal-level barriers [12]. These convergent findings attest to the potential value of dynamic barrier tracking and coding methods so that physical activity counsellors can align salient barriers at a particular intervention time-point, with the most appropriate BCT. It is also noteworthy that across the intervention period, the barriers were similar in number, breadth of levels covered in a SEM, and in content to the ~200 barriers identified in meta-reviews of studies involving children and adults with various types of disabilities [3, 14]. Together, these results suggest that our coding method and results may generalize to other settings and impairment groups.
Participants reported relatively more institutional, community, and policy level barriers compared to intrapersonal barriers in later weeks of the intervention than at the start. Perhaps as participants gained confidence to be active, they began looking for more physical activity opportunities in their communities and, unfortunately, encountered more barriers. If a counsellor is aware of changes in the types of barriers, the counsellor can tailor specific techniques and strategies to support changing needs, such as linking and referring clients to community-based resources and programmes that support people with disabilities. These examples illustrate the value of understanding the dynamics of physical activity barriers for improving tailored physical activity behavioural support, including the selection of appropriate BCT [12].
An important innovation within this study was the development and application of methods to measure, categorize, and analyze dynamic changes in physical activity barriers. As noted, these methods can be used to support and improve physical activity behavioural counselling. For instance, continued research can facilitate the development of lists of barriers that become salient as participants transition from the initiation to the maintenance phases of physical activity and appropriate intervention techniques can be aligned and implemented accordingly. These methods could also be used to evaluate the efficacy of physical activity-enhancing interventions by quantifying changes in barriers over time. For example, if a behaviour-change intervention is effective, one would expect to observe a reduction in the number of barriers reported by participants over time. The methods described in this paper could be used to test for such changes. Analyses could also be undertaken to test for associations between a counsellor’s use of specific BCT [12] and changes in barrier dynamics. Testing for such relationships could help identify which BCT are most conducive to reducing specific barriers and when certain strategies are most effective (e.g., earlier versus later in an intervention).
Limitations
While this study provides important direction for further study and analysis of physical activity barrier dynamics within the context of physical activity-enhancing interventions, it has limitations. One study limitation is that given the nature of the data used in our analyses (transcribed physical activity counselling sessions), we have information on the types and number of barriers, but not their perceived impact. In some situations (e.g., when a barrier cannot be removed but merely mitigated), counsellors may find utility in asking their clients about the impact of certain barriers. Dynamic changes in perceived barrier impact could be another important element for understanding change in barrier dynamics in response to participant experiences and counsellor intervention.
A second limitation is that our relatively small sample size precluded repeated measures analyses across all nine sessions. Our pre-post analysis plan involved testing if the barriers decreased across the intervention, rather than when the barriers decreased. With adequately-powered samples, future investigators may find value in testing at which point in an intervention, specific barriers decline significantly.
Another limitation is that our sample consisted of participants involved in a single intervention programme. While the number and types of barriers reported by study participants were consistent with previous findings [1,2,3], the most salient barriers and their pattern of change may differ across samples and interventions. The methods detailed in this paper provide a starting point for investigators to address research questions about dynamic changes in barriers for the purpose of improving physical activity interventions in their own contexts. Our results provide a basis for comparing their results.
Conclusion
This paper documents a new, systematic coding method to track and evaluate changes in physical activity barriers. By applying this method in the context of a physical activity behavioural intervention for adults with SCI, we found a significant decrease in the number of barriers reported by participants, over the course of the intervention period. We encourage further research using these methods in other settings and populations. Understanding the dynamics of physical activity barriers can help improve the design of physical activity- enhancing interventions, while barrier tracking can help improve intervention implementation and evaluation.
Data availability
Data are available from the corresponding author on reasonable request.
References
Williams TL, Smith B, Papathomas A. The barriers, benefits and facilitators of leisure time physical activity among people with spinal cord injury: a meta-synthesis of qualitative findings. Health Psychol Rev. 2014;8:404–4025.
Fekete C, Rauch A. Correlates and determinants of physical activity in persons with spinal cord injury: a review using the International Classification of Functioning, Disability and Health as reference framework. Disabil Health J. 2012;5:140–50.
Martin Ginis KA, Ma JK, Latimer-Cheung AE, Rimmer JH. A systematic review of review articles addressing factors related to physical activity participation among children and adults with physical disabilities. Health Psychol Rev. 2016;10:478–94.
McLeroy KR, Bibeau D, Steckler A, Glanz K. An ecological perspective on health promotion programs. Health Educ Q. 1988;15:351–77.
Schwarzer R. Modeling health behavior change: how to predict and modify the adoption and maintenance of health behaviors. Appl Psychol. 2008;57:1–29.
Schwarzer R, Lippke S, Luszczynska A. Mechanisms of health behavior change in persons with chronic illness or disability: the Health Action Process Approach (HAPA). Rehabil Psychol. 2011;56:161–70.
Martin Ginis KA, Tomasone JR, Latimer AE, Arbour-Nicitopoulos KP, Bassett RL, Wolfe DL, et al. Developing physical activity interventions for adults with spinal cord injury. Part 1: a comparison of social cognitions across actors, intenders and non-intenders. Rehabil Psychol. 2013;58:299–306.
Arbour-Nicitopoulos KP, Martin Ginis KA, Latimer AE. Planning, leisure-time physical activity, and coping self-efficacy in persons with spinal cord injury: a randomized controlled trial. Arch Phys Med Rehabil. 2009;90:2003–11.
Michie S, Atkins L, West R. The behaviour change wheel: a guide to designing interventions. London, UK: Silverback Publishing; 2014; www.behaviourchangewheel.com.
Ma JK, West CR, Martin Ginis KA. The effects of a patient and provider co-developed, behavioral physical activity intervention on physical activity, psychosocial predictors, and fitness in individuals with spinal cord injury: a randomized controlled trial. Sports Med. 2019;49:1117–31.
Ma JK, Cheifetz O, Todd KR, Chebaro C, Phang SH, Shaw RB, et al. Co-development of a physiotherapist-delivered physical activity intervention for adults with spinal cord injury. Spinal Cord. 2020;58:778–86.
Michie S, Abraham C, Whittington C, McAteer J, Gupta S. Effective techniques in healthy eating and physical activity interventions: a meta-regression. Health Psychol. 2009;28:690–701.
Martin Ginis KA, van der Scheer JW, Latimer-Cheung AE, Barrow A, Bourne C, Carruthers P, et al. Evidence-based scientific exercise guidelines for adults with spinal cord injury: an update and a new guideline. Spinal Cord. 2018;56:308–21.
Martin Ginis KA, van der Ploeg HP, Foster C, Lai B, McBride CB, Ng K, et al. Participation of people living with disabilities in physical activity: a global perspective. Lancet. 2021;398:443–55.
Todd KR, Martin Ginis KA. Physical activity and spinal cord injury: lessons learned at the lowest end of the physical activity spectrum. Kinesiol Rev. 2019;8:54–62.
Funding
Ontario Neurotrauma Foundation/Rick Hansen Institute grant (2015-RHI-PEPA-998) and a partnership grant from the Social Sciences and Humanities Research Council of Canada (895-201301021) for the Canadian Disability Participation Project (www.cdpp.ca). FH is supported by a Craig H. Neilsen Foundation Postdoctoral Fellowship (#719049) and Michael Smith Foundation for Health Research (MSFHR) Research Trainee Award (#RT-2020-0489). The funding bodies did not contribute to the design of the project, collection, analysis, and interpretation of data or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
MD contributed to study conceptualization, data analysis and writing of the manuscript. FH contributed to study conceptualization (development of coding method), data analysis, writing and review of the manuscript. SS contributed to study conceptualization (development of coding method), data analyses and review of the manuscript. JKM contributed to study conceptualization (ProACTIVE Trial), data collection, and review of the manuscript. KMG contributed to study conceptualization (ProACTIVE trial and coding manual), data analysis, writing and review of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
This study was approved by the Clinical Research Ethics Board of the University of British Columbia (H19-02694).
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Dinwoodie, M., Hoekstra, F., Stelzer, S. et al. A dynamic analysis of physical activity barriers experienced by adults with spinal cord injury. Spinal Cord Ser Cases 8, 37 (2022). https://doi.org/10.1038/s41394-022-00504-y
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-022-00504-y