Abstract
Introduction
Cervical spondylosis can predispose patients to central canal stenosis. In this setting, myelopathy through further flattening of the cord from extrinsic compression can be precipitated by relatively minor traumas. Arterial dissection is similarly considered a result of high velocity or momentum during trauma, commonly associated with fractures, cervical hyperflexion, or direct blunt force to the neck. Overall, precautions for both arterial dissection and myelopathy are rarely considered in low-velocity, static activities such as yoga.
Case presentation
The authors report the case of a 63-year-old man who suffered concurrent cervical myelopathy from multilevel spondylopathy, right vertebral artery dissection, and left cervical carotid artery dissection following a yoga session. Symptomatology consisted of acute onset neck pain, upper extremity sensory paresthesia, worsening gait and balance, and impaired dexterity for several weeks. Cervical MRI was obtained given myelopathic symptoms and revealed spondylosis with compression and T2 signal change at C3–C4. CT angiography of the neck revealed aforementioned dissections without flow limiting stenosis or occlusion. A therapeutic heparin infusion was started preoperatively until the patient underwent C3–C4 anterior cervical discectomy and fusion. Aspirin and Plavix were then started without incidence and the patient had significant but gradual improvement in myelopathic symptoms at 6-week follow-up.
Discussion
The static yet intensive poses associated with yoga present a rare etiology for arterial dissection and myelopathy, but patients with persistent and progressive symptoms should be screened with the appropriate imaging modality. Cervical decompression should be expedited before initiating an antiplatelet medication.
Similar content being viewed by others
Introduction
Cervical spondylosis, a finding in up to 50% of the population over 40 years of age, can predispose to central canal stenosis [1]. In this setting, myelopathy through further flattening of the cord from extrinsic compression can be precipitated by relatively minor traumas. In high-risk patients, pre-emptive decompression may even be performed prior to the development of myelopathy so as to avoid severe injury. However, such precautions are rarely considered in low-velocity, static activities such as yoga.
Arterial dissection is similarly considered a result of high velocity or momentum during trauma, commonly associated with fractures or with cervical hyperflexion, hyperextension with rotation, or direct blunt force to the neck [2]. While there are reports of yoga-induced dissection, it remains a very rare phenomenon [3]. On further literature review, no cases are reported in the literature of acute myelopathy from yoga with concurrent arterial dissection.
Case presentation
The authors report the case of a 63-year-old man who suffered concurrent cervical myelopathy from multilevel spondylopathy, right vertebral artery dissection, and left cervical carotid artery dissection following a yoga session. Symptomatology consisted of acute onset neck pain, then upper extremity sensory paresthesia, worsening gait and balance, and impaired dexterity for several weeks. Cervical MRI was obtained given myelopathic symptoms and revealed spondylosis with compression and T2 signal change at C3–C4. CT angiography of the neck then revealed aforementioned dissections without flow limiting stenosis or occlusion. A therapeutic heparin infusion was started preoperatively until the patient underwent C3–C4 anterior cervical discectomy and fusion. Aspirin and Plavix were then started without incidence and the patient had significant but gradual improvement in myelopathic symptoms at 6-week follow-up.
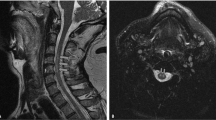
The patient was practicing Vrischikasana, a pose in which the body is balanced on the bilateral forearms with legs initially pointing up. The legs are then slowly lowered by extending at the hips and flexing the knees, with the body finally resting in the shape of the letter “C.” The patient failed to steady the pose and immediately had neck pain after his attempt, which aborted any further yoga that day. The next morning, he noticed numbness and tingling in his bilateral hands. He noted worsening dexterity, and had several episodes of dropping objects. While the patient avoided falls, gait subsequently deteriorated as well with significant trouble balancing. On examination, he was noted to have bilateral Hoffman’s sign and hyperreflexia at the patellae. Subsequent MRI (Fig. 1) demonstrated multilevel spondylosis, severe stenosis, and T2-weighted MRI demonstrating spinal cord signal change. While MRI did not reveal any evidence of stroke, CT angiography (Fig. 1) of the neck was performed given the persistent neck pain. Intimal flaps concerning for dissection were seen in both the left cervical carotid segment and right V2 segment.
Given the progressive neurological decline, associated functional limitation, and cord signal change, surgical intervention was recommended for spinal cord decompression. The patient was admitted and placed on a therapeutic dose heparin drip given the bilateral arterial dissections. Heparin was stopped the night before surgery but was not reversed. On admission 10 mg of IV dexamethasone was given in the setting of cord compression.
Imaging demonstrated focal C3–4 stenosis that was evaluated as the likely symptomatic level. Given single-level pathology with a largely ventral vector of compression, a C3–4 anterior cervical discectomy and fusion was performed. Surgery was uncomplicated and the patient woke from anesthesia without any deterioration in neurological exam. Somatosensory evoked potentials were monitored during the case and were stable throughout.
The patient reported immediate improvement in the character and intensity of his bilateral hand paresthesia. The incision was watched for postoperative hematoma given the short course of heparin infusion prior to the procedure, but remained soft without distention. On postoperative day 2 the patient was started on Aspirin and Plavix, and was subsequently discharged. On short-term follow-up at 6 weeks, he endorsed continued improvement in hand paresthesias and gait. Neurological exam was unchanged throughout the hospital course, and the patient had decreased hyperreflexia but sustained Hoffman’s on the follow-up visit.
Discussion
While yoga has been associated with neck injuries in the literature, this remains the first documented case of yoga-induced acute myelopathy with cervical arterial dissections.
In previous reports, as in this case, the cervical spine is the most common site of traumatic spinal cord injury. Etiology is most frequently related to high-velocity traumas in the young and falls in the elderly [4]. Pathology is often induced by spinal cord compression through mechanical disruption or dislocation of the spinal column, thereby making injuries from low-velocity exercises such as yoga a relative rarity. An extensive literature review revealed one other case of cervical myelopathy precipitated by a yoga. This practitioner held Sirsasana, yet another headstand pose requiring the full weight of the body to be held by the neck [5]. Such axial loading in the setting of prior spondylotic stenosis may be the common mechanism underlying both cases. While cervical SCI in the setting of pre-existing stenosis is frequently reported, data remain limited on the actual risk faced by a stenotic patient. A prospective cohort study by Chang et al. recently described a 0% rate of SCI in ten patients with documented cervical stenosis, prior advice to consider decompression, and subsequent traumatic event [6]. However, this remains a small cohort study, and larger studies would be significantly difficult to design and enroll given the need for nonoperative management of established cervical stenosis and subsequent traumatic event.
In this case, a low-velocity injury also induced bilateral, anterior, and posterior circulation arterial dissections. Cervical arterial dissection remains responsible for 1–2% of all strokes and up to 25% of strokes in young and middle-aged [7]. The pathogenesis of ischemia occurs either directly through thrombosis with occlusion or secondarily through micro-embolic events [8]. Symptoms most frequently consist of head or neck pain, cerebral ischemia, or Horner’s syndrome [9, 10]. The most common etiologies of traumatic dissection are motor vehicle accidents, assaults, falls, and hangings [2]. Treatment depends on morphology, with recent evidence suggesting equivalent outcomes between antiplatelet and anticoagulant agents for minor grade dissections [11, 12]. Yoga is a well-described cause of cervical arterial dissection, with stroke or TIA being the common chief complaint [13, 14]. Our patient remains unique in that cervical arterial dissection was incidentally found without neurologic deficit, but with only the characteristic neck pain associated with dissection. In addition, dissection in the vertebral artery occurred in the V2 segment, which is rare given protected traversal through the foramen transversarium. Carotid dissection occurred in a more common location at the cervical segment, commonly involved as the artery travels from soft tissues to hard bony canal. Definitive treatment followed guidelines with a preoperative heparin infusion for easily reversible coverage followed by postoperative aspirin and Plavix.
Vertebral artery dissection and cervical myelopathy are commonly screened for and found in high-velocity traumas. The static yet intensive poses associated with Yoga present a rare etiology for either injury, but patients with persistent and progressive symptoms should be screened with the appropriate imaging modality. Cervical decompression should be expediated before initiating an antiplatelet medication.
References
Matsumoto M, Fujimura Y, Suzuki N, Nishi Y, Nakamura M, Yabe Y, et al. MRI of cervical intervertebral discs in asymptomatic subjects. J Bone Joint Surg Br. 1998;80:19–24.
Biffl WL, Moore EE, Offner PJ, Brega KE, Franciose RJ, Elliott JP, et al. Optimizing screening for blunt cerebrovascular injuries. Am J Surg. 1999;178:517–21.
Cramer H, Krucoff C, Dobos G. Adverse events associated with yoga: a systematic review of published case reports and case series. PLoS One. 2013;8:e75515.
Chen Y, He Y, DeVivo MJ. Changing demographics and injury profile of new traumatic spinal cord injuries in the United States, 1972–2014. Arch Phys Med Rehabil. 2016;97:1610–9.
Ferreira MA, Galvez-Jimenez N. Sirsasana (Headstand) pose causing compressive myelopathy with myelomalacia. JAMA Neurol. 2013;70:268.
Chang V, Ellingson BM, Salamon N, Holly LT. The risk of acute spinal cord injury after minor trauma in patients with preexisting cervical stenosis. Neurosurgery. 2015;77:561–5.
Debette S, Leys D. Cervical-artery dissections: predisposing factors, diagnosis, and outcome. Lancet Neurol. 2009;8:668–78.
Molina CA, Alvarez-Sabín J, Schonewille W, Montaner J, Rovira A, Abilleira S, et al. Cerebral microembolism in acute spontaneous internal carotid artery dissection. Neurology. 2000;55:1738–40.
Debette S, Grond-Ginsbach C, Bodenant M, Kloss M, Engelter S, Metso T, et al. Differential features of carotid and vertebral artery dissections The CADISP study. Neurology. 2011;77:1174–81.
Lee VH, Brown RD, Mandrekar JN, Mokri B. Incidence and outcome of cervical artery dissection: a population-based study. Neurology. 2006;67:1809–12.
Biffl WL, Moore EE, Offner PJ, Burch JM. Blunt carotid and vertebral arterial injuries. World J Surg. 2001;25:1036–43.
Markus HS, Hayter E, Levi C, Feldman A, Venables G, Norris J, et al. Antiplatelet treatment compared with anticoagulation treatment for cervical artery dissection (CADISS): a randomised trial. Lancet Neurol. 2015;14:361–7.
Hanus SH, Homer TD, Harter DH. Vertebral artery occlusion complicating yoga exercises. Arch Neurol. 1977;34:574–5.
Hilton-Jones D, Warlow CP. Non-penetrating arterial trauma and cerebral infarction in the young. Lancet. 1985;325:1435–8.
Author information
Authors and Affiliations
Contributions
GN developed the project protocol, gathered patient information, and participated in manuscript drafting. AD participated in manuscript drafting and final formatting for submission. N Agarwal helped develop project protocol and gathered patient information. N Alan helped develop project protocol and gathered patient information. JJM supervised and participated in final manuscript editing.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Ethical approval
No formal ethical approval required because no personal patient information shared. Verbal patient consent provided.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
About this article
Cite this article
Nayar, G., Desai, A., Agarwal, N. et al. Cervical arterial dissection and traumatic myelopathy following yoga: surgical case report. Spinal Cord Ser Cases 8, 46 (2022). https://doi.org/10.1038/s41394-021-00458-7
Received:
Revised:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41394-021-00458-7